Effect of Lumbar Spine Mobility and Postural Alignment on Menstrual Pain in Young Women
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Study Qualification
2.3. Methods
2.3.1. Anthropometric Measurements
2.3.2. Assessment of Spinal Curvature
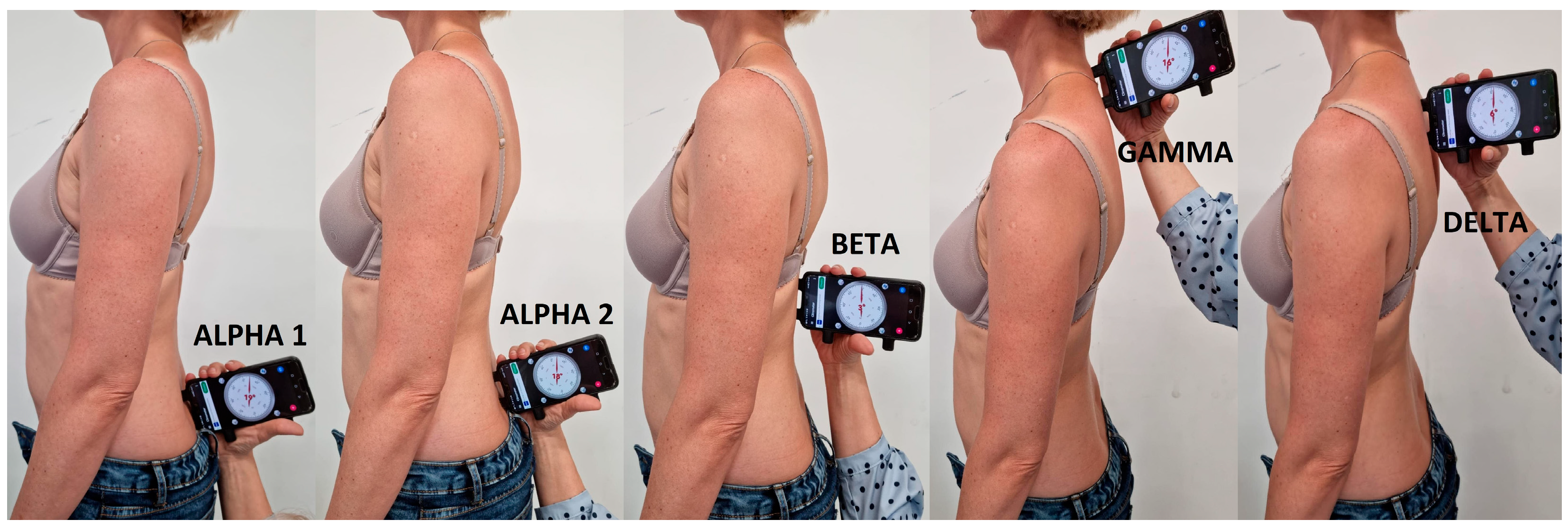
- ALPHA 1 angle—inclination of the sacrum (upper beam of the inclinometer in the middle of the intervertebral space on the line connecting the posterior superior iliac spines).
- ALPHA 2 angle—sacrolumbar junction S/L (centre of the inclinometer on the line connecting the posterior superior iliac spines).
- BETA angle—Th12-L1 thoracolumbar junction (centre of the inclinometer at the thoracolumbar junction).
- GAMMA angle—C7-Th1 (upper beam of the inclinometer on C7).
- DELTA angle—Th3-Th4 (upper beam of the inclinometer at the height of the anglus superior of the scapula). The location of the parameters is presented in Figure 2.
- Lumbosacral angle (ALPHA 2 angle)—15–30°;
- Lumbar lordosis angle—LLA (ALPHA 2 angle + BETA angle)—30–40°;
- Thoracic kyphosis angle –TKA (BETA angle + DELTA angle)—30–40° [23];
2.3.3. Assessment of Spinal Mobility
2.3.4. Questionnaire
2.4. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Belayneh, Z.; Mekuriaw, B. Knowledge and Menstrual Hygiene Practice among Adolescent School Girls in Southern Ethiopia: A Cross-Sectional Study. BMC Public Health 2019, 19, 1595. [Google Scholar] [CrossRef]
- Critchley, H.O.D.; Maybin, J.A.; Armstrong, G.M.; Williams, A.R.W. Physiology of the Endometrium and Regulation of Menstruation. Physiol. Rev. 2020, 100, 1149–1179. [Google Scholar] [CrossRef]
- Iacovides, S.; Avidon, I.; Baker, F.C. What We Know about Primary Dysmenorrhea Today: A Critical Review. Hum. Reprod. Update 2015, 21, 762–778. [Google Scholar] [CrossRef] [Green Version]
- Karout, S.; Soubra, L.; Rahme, D.; Karout, L.; Khojah, H.M.J.; Itani, R. Prevalence, Risk Factors, and Management Practices of Primary Dysmenorrhea among Young Females. BMC Women’s Health 2021, 21, 392. [Google Scholar] [CrossRef]
- Vilšinskaitė, D.S.; Vaidokaitė, G.; Mačys, Ž.; Bumbulienė, Ž. The risk factors of dysmenorrhea in young women. Wiadomości Lek. 2019, 72, 1170–1174. [Google Scholar] [CrossRef]
- McKenna, K.A.; Fogleman, C.D. Dysmenorrhea. Am. Fam. Physician 2021, 104, 164–170. [Google Scholar] [PubMed]
- Ju, H.; Jones, M.; Mishra, G. The Prevalence and Risk Factors of Dysmenorrhea. Epidemiol. Rev. 2014, 36, 104–113. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yacubovich, Y.; Cohen, N.; Tene, L.; Kalichman, L. The Prevalence of Primary Dysmenorrhea among Students and Its Association with Musculoskeletal and Myofascial Pain. J. Bodyw. Mov. Ther. 2019, 23, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Piiroinen, O.; Kaihola, H.-L. Uterine Size Measured by Ultrasound During the Menstrual Cycle. Acta Obstet. Et Gynecol. Scand. 1975, 54, 247–250. [Google Scholar] [CrossRef] [PubMed]
- Marjoribanks, J.; Ayeleke, R.O.; Farquhar, C.; Proctor, M. Nonsteroidal Anti-Inflammatory Drugs for Dysmenorrhoea. Cochrane Database Syst. Rev. 2015, 2015, CD001751. [Google Scholar] [CrossRef] [PubMed]
- Oladosu, F.A.; Tu, F.F.; Farhan, S.; Garrison, E.F.; Steiner, N.D.; Roth, G.E.; Hellman, K.M. Abdominal Skeletal Muscle Activity Precedes Spontaneous Menstrual Cramping Pain in Primary Dysmenorrhea. Am. J. Obstet. Gynecol. 2018, 219, 91.e1–91.e7. [Google Scholar] [CrossRef] [PubMed]
- Bernardi, M.; Lazzeri, L.; Perelli, F.; Reis, F.M.; Petraglia, F. Dysmenorrhea and Related Disorders. F1000Research 2017, 6, 1645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evans, S.; Mikocka-Walus, A.; Olive, L.; Seidman, L.C.; Druitt, M.; Payne, L.A. Phenotypes of Women with and Without Endometriosis and Relationship with Functional Pain Disability. Pain Med. 2020, 22, 1511–1521. [Google Scholar] [CrossRef] [PubMed]
- Bajalan, Z.; Moafi, F.; MoradiBaglooei, M.; Alimoradi, Z. Mental Health and Primary Dysmenorrhea: A Systematic Review. Journal of Psychosom. Obstet. Gynecol. 2019, 40, 185–194. [Google Scholar] [CrossRef]
- Karakus, A.; Balaban, M.; Kaya, D.O.; Celenay, S.T. Lumbopelvic Muscle Endurance, Morphology, Alignment, and Mobility in Women with Primary Dysmenorrhea: A Case-Control Study. Clin. Biomech. 2022, 92, 105582. [Google Scholar] [CrossRef]
- Kim, M.; Baek, I.; Goo, B. The Effect of Lumbar-Pelvic Alignment and Abdominal Muscle Thickness on Primary Dysmenorrhea. J. Phys. Ther. Sci. 2016, 28, 2988–2990. [Google Scholar] [CrossRef] [Green Version]
- Armour, M.; Ee, C.C.; Naidoo, D.; Ayati, Z.; Chalmers, K.J.; Steel, K.A.; de Manincor, M.J.; Delshad, E. Exercise for dysmenorrhoea. Cochrane Database Syst. Rev. 2019, 3, CD004142. [Google Scholar] [CrossRef]
- Naukowiec.org. Available online: https://www.naukowiec.org/dobor.html (accessed on 18 November 2021).
- Budrowska, W.; Paul, M.; Zawałkiewicz, A.; Żynda, M. Library statistics and analysis-new methods and tools. Biuletyn EBIB 2019, 188, 5. [Google Scholar]
- Walicka-Cypruś, K.; Szeliga, E.; Guzik, A.; Mrozkowiak, M.; Niewczas, M.; Ostrowski, P.; Tabaczek-Bejster, I. Evaluation of anterior-posterior spine curvatures and incidence of sagittal defects in children and adolescents practicing traditional karate. Biomed. Res. Int. 2019, 2019, 9868473. [Google Scholar] [CrossRef] [Green Version]
- Yen, Y.R.; Luo, J.F.; Liu, M.L.; Lu, F.J.; Wang, S.R. The Anthropometric Measurement of Schober’s Test in Normal Taiwanese Population. Biomed Res. Int. 2015, 2015, 256365. [Google Scholar] [CrossRef] [Green Version]
- Walicka-Cupryś, K.; Wyszyńska, J.; Podgórska-Bednarz, J.; Drzał-Grabiec, J. Concurrent validity of photogrammetric and inclinometric techniques based on assessment of anteroposterior spinal curvatures. Eur. Spine J. 2018, 27, 497–507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saunders, J. Saunders digital inclinometer. In Instructional Materials; The Saundersa Group Inc.: Shoreview, MN, USA, 1998; Volume 8. [Google Scholar]
- Abd Elmeged, N.A.; Ibrahim, A.H.; Labib, A.M.; Ahmed, A.R.; Mohamed, G.I.; Kamal, H.A. Effect of Mckenzie Exercises on Functional Neck Disability in Females with Dowager’S Hump. Egypt. J. Appl. Sci. 2021, 36, 163–182. [Google Scholar]
- Buckup, K.; Buckup, J. Clinical Tests in the Examination of Bones, Joints and Muscles; PZWL: Warszawa, Poland, 2014. [Google Scholar]
- Escalona-Marfil, C.; Coda, A.; Ruiz-Moreno, J.; Miquel Riu-Gispert, L.; Gironès, X. Validation of an Electronic Visual Analog Scale mHealth Tool for Acute Pain Assessment: Prospective Cross-Sectional Study. J. Med. Internet Res. 2020, 22, e13468. [Google Scholar] [CrossRef]
- Fernández-Martínez, E.; Onieva-Zafra, M.D.; Parra-Fernández, M.L. The Impact of Dysmenorrhea on Quality of Life Among Spanish Female University Students. Int. J. Environ. Res. Public Health 2019, 16, 713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rafique, N.; Al-Sheikh, M.H. Prevalence of Primary Dysmenorrhea and Its Relationship with Body Mass Index. J. Obstet. Gynaecol. Res. 2018, 44, 1773–1778. [Google Scholar] [CrossRef]
- Abadi Bavil, D.; Dolatian, M.; Mahmoodi, Z.; Akbarzadeh Baghban, A. A Comparison of Physical Activity and Nutrition in Young Women with and without Primary Dysmenorrhea. F1000Research 2018, 7, 59. [Google Scholar] [CrossRef] [Green Version]
- Rafique, N.; Al-Sheikh, M.H. Prevalence of Menstrual Problems and Their Association with Psychological Stress in Young Female Students Studying Health Sciences. Saudi Med. J. 2018, 39, 67–73. [Google Scholar] [CrossRef]
- Facchin, F.; Barbara, G.; Saita, E.; Mosconi, P.; Roberto, A.; Fedele, L.; Vercellini, P. Impact of Endometriosis on Quality of Life and Mental Health: Pelvic Pain Makes the Difference. J. Psychosom. Obstet. Gynecol. 2015, 36, 135–141. [Google Scholar] [CrossRef]
- Abd El-Mawgod, M.M.; Alshaibany, A.S.; Al-anazi, A.M. Epidemiology of Dysmenorrhea among Secondary-School Students in Northern Saudi Arabia. J. Egypt. Public Health Assoc. 2016, 91, 115–119. [Google Scholar] [CrossRef]
- Hashim, R.T.; Alkhalifah, S.S.; Alsalman, A.A.; Alfaris, D.M.; Alhussaini, M.A.; Qasim, R.S.; Shaik, S.A. Prevalence of Primary Dysmenorrhea and Its Effect on the Quality of Life amongst Female Medical Students at King Saud University, Riyadh, Saudi Arabia. Saudi Med. J. 2020, 41, 283–289. [Google Scholar] [CrossRef]
- Ibrahim, N.K.R.; AlGhamdi, M.S.; Al-Shaibani, A.N.; Al-Amri, F.A.; Alharbi, H.A.; Al-Jadani, A.K.; Alfaidi, R.A. Dysmenorrhea among Female Medical Students in King Abdulaziz University: Prevalence, Predictors and Outcome. Pak. J. Med. Sci. 2015, 31, 1312–1317. [Google Scholar] [CrossRef]
- Yücel, G.; Kendirci, M.; Gül, Ü. Menstrual Characteristics and Related Problems in 9- to 18-Year-Old Turkish School Girls. J. Pediatr. Adolesc. Gynecol. 2018, 31, 350–355. [Google Scholar] [CrossRef]
- Torkan, B.; Mousavi, M.; Dehghani, S.; Hajipour, L.; Sadeghi, N.; Ziaei Rad, M.; Montazeri, A. The Role of Water Intake in the Severity of Pain and Menstrual Distress among Females Suffering from Primary Dysmenorrhea: A Semi-Experimental Study. BMC Women’s Health 2021, 21, 40. [Google Scholar] [CrossRef]
- Pembe, A.B.; Ndolele, N.T. Dysmenorrhoea and coping strategies among secondary school adolescents in Ilala District, Tanzania. East Afr. J. Public Health 2011, 8, 232–236. [Google Scholar]
- Nimbalkar, S.; Kamat, S.; Nimbalkar, A.; Phatak, A. Premenstrual Syndrome in Anand District, Gujarat: A Cross-Sectional Survey. J. Fam. Med. Prim. Care 2019, 8, 640–647. [Google Scholar] [CrossRef]
- Teul, I.; Kliś, K.; Jarzębak, K.; Wronka, I. Częstość występowania oraz czynniki skorelowane z bólem miesiączkowym u zdrowych studentek. Rocz. Pomor. Akad. Med. W Szczecinie 2014, 60, 89–94. [Google Scholar] [CrossRef]
- Knapik, A.; Grzyb, A.; Horodecki, M.; Hanus, B. Spine Pain among the Secondary School Youth in the Silesia Province of Poland Scale of the Problem and Reasons. Med. Ogólna I Nauk. O Zdrowiu 2018, 24, 19–24. [Google Scholar] [CrossRef] [Green Version]
- Chun, S.-W.; Lim, C.-Y.; Kim, K.; Hwang, J.; Chung, S.G. The Relationships between Low Back Pain and Lumbar Lordosis: A Systematic Review and Meta-Analysis. Spine J. 2017, 17, 1180–1191. [Google Scholar] [CrossRef] [PubMed]
- Molins-Cubero, S.; Rodríguez-Blanco, C.; Oliva-Pascual-Vaca, Á.; Heredia-Rizo, A.M.; Boscá-Gandía, J.J.; Ricard, F. Changes in Pain Perception after Pelvis Manipulation in Women with Primary Dysmenorrhea: A Randomized Controlled Trial. Pain Med. 2014, 15, 1455–1463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rakhshaee, Z. Effect of Three Yoga Poses (Cobra, Cat and Fish Poses) in Women with Primary Dysmenorrhea: A Randomized Clinical Trial. J. Pediatr. Adolesc. Gynecol. 2011, 24, 192–196. [Google Scholar] [CrossRef]
- Yonglitthipagon, P.; Muansiangsai, S.; Wongkhumngern, W.; Donpunha, W.; Chanavirut, R.; Siritaratiwat, W.; Mato, L.; Eungpinichpong, W.; Janyacharoen, T. Effect of Yoga on the Menstrual Pain, Physical Fitness, and Quality of Life of Young Women with Primary Dysmenorrhea. J. Bodyw. Mov. Ther. 2017, 21, 840–846. [Google Scholar] [CrossRef] [PubMed]
- Yang, N.-Y.; Kim, S.-D. Effects of a Yoga Program on Menstrual Cramps and Menstrual Distress in Undergraduate Students with Primary Dysmenorrhea: A Single-Blind, Randomized Controlled Trial. J. Altern. Complement. Med. 2016, 22, 732–738. [Google Scholar] [CrossRef]
- Demirel, A.; Oz, M.; Ozel, Y.A.; Cetin, H.; Ulger, O. Stabilization Exercise versus Yoga Exercise in Non-Specific Low Back Pain: Pain, Disability, Quality of Life, Performance: A Randomized Controlled Trial. Complement. Ther. Clin. Pract. 2019, 35, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Bulun, S.E.; Yilmaz, B.D.; Sison, C.; Miyazaki, K.; Bernardi, L.; Liu, S.; Kohlmeier, A.; Yin, P.; Milad, M.; Wei, J. Endometriosis. Endocr. Rev. 2019, 40, 1048–1079. [Google Scholar] [CrossRef] [PubMed]
- Mehedintu, C.; Plotogea, M.N.; Ionescu, S.; Antonovici, M. Endometriosis still a challenge. J. Med. Life 2014, 7, 349–357. [Google Scholar] [PubMed]
- Sirmans, S.; Pate, K. Epidemiology, Diagnosis, and Management of Polycystic Ovary Syndrome. Clin. Epidemiol. 2013, 2014, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Solomon, C.G. The epidemiology of Polycystic Ovary Syndrome. Endocrinol. Metab. Clin. N. Am. 1999, 28, 247–263. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.Y.; Kim, M.K.; Lee, I.; Yun, J.; Won, Y.B.; Yun, B.H.; Seo, S.K.; Cho, S.; Choi, Y.S.; Lee, B.S. Polycystic Ovarian Morphology Is Associated with Primary Dysmenorrhea in Young Korean Women. Obstet. Gynecol. Sci. 2019, 62, 329–334. [Google Scholar] [CrossRef]
- Ramos-Pichardo, J.D.; Ortega-Galán, Á.M.; Iglesias-López, M.T.; Abreu-Sánchez, A.; Fernández-Martínez, E. Why Do Some Spanish Nursing Students with Menstrual Pain Fail to Consult Healthcare Professionals? Int. J. Environ. Res. Public Health 2020, 17, 8173. [Google Scholar] [CrossRef]

| Control Group | Study Group | |||||
|---|---|---|---|---|---|---|
| Outcome Variable | x | S | x | S | U | p |
| Absence from work/university | 0.03 | 0.16 | 0.16 | 0.37 | −3.08 | 0.088 |
| Lack of concentration | 0.17 | 0.38 | 0.60 | 0.49 | −6.23 | <0.001 |
| Limited physical activity | 0.38 | 0.49 | 0.79 | 0.41 | −6.00 | <0.001 |
| Adverse impact on academic/work performance | 0.13 | 0.34 | 0.45 | 0.50 | −4.78 | <0.001 |
| Increased body temperature | 0.18 | 0.39 | 0.30 | 0.46 | −1.98 | 0.133 |
| Worse feeling compared to the days before menstruation | 0.62 | 0.49 | 0.91 | 0.29 | −5.34 | <0.001 |
| Control Group | Study Group | |||||||
|---|---|---|---|---|---|---|---|---|
| Outcome Variable | x | Me | S | x | Me | S | U | p |
| ALPHA 1 | 21.4 | 22.0 | 5.3 | 20.4 | 20.0 | 5.4 | 1.62 | 0.106 |
| ALPHA 2 | 18.9 | 18.0 | 6.3 | 17.1 | 17.0 | 6.9 | 2.13 | 0.034 |
| BETA | 13.3 | 14.0 | 5.6 | 11.5 | 11.5 | 6.9 | 2.02 | 0.044 |
| GAMMA | 26.1 | 26.0 | 6.4 | 26.1 | 24.0 | 14.1 | 1.29 | 0.197 |
| DELTA | 11.6 | 11.0 | 5.1 | 10.8 | 10.0 | 5.8 | 1.33 | 0.184 |
| LLA | 32.2 | 32.5 | 9.4 | 28.5 | 29.0 | 10.3 | 2.74 | 0.006 |
| MTKA | 24.9 | 25.0 | 7.7 | 22.3 | 22.5 | 9.7 | 2.08 | 0.037 |
| TKA | 39.4 | 39.5 | 9.6 | 37.6 | 35.5 | 16.8 | 1.86 | 0.063 |
| SH | 14.4 | 14.0 | 6.5 | 15.3 | 13.0 | 14.1 | 0.79 | 0.431 |
| Schober Test—flexion | 4.1 | 4.0 | 1.2 | 4.2 | 4.0 | 1.7 | 0.00 | 0.999 |
| Schober Test—extension | 1.9 | 1.5 | 1.0 | 1.9 | 2.0 | 0.9 | −0.70 | 0.497 |
| Control Group | Study Group | |||||||
|---|---|---|---|---|---|---|---|---|
| Outcome Variable | x | Me | S | x | Me | S | U | p |
| Mean length of bleeding (days) | 5.2 | 5.0 | 1.0 | 5.7 | 6.0 | 1.0 | −2.52 | 0.017 |
| Pain before menstruation (days) | 0.8 | 0.0 | 1.4 | 2.0 | 1.0 | 2.2 | −5.26 | <0.001 |
| Duration of menstrual cycle (days) | 28.6 | 28.0 | 1.9 | 29.2 | 29.0 | 2.5 | −1.95 | 0.057 |
| Control Group | Study Group | p | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome Variable | Below Norm | Norm | Above Norm | Below Norm | Norm | Above Norm | |||||||
| n | % | n | % | n | % | N | % | n | % | n | % | ||
| ALPHA 1 | 9 | 11.5 | 66 | 84.6 | 3 | 3.9 | 23 | 15.8 | 117 | 80.1 | 6 | 4.1 | 0.886 |
| LLA | 29 | 37.2 | 34 | 43.6 | 15 | 19.2 | 79 | 54.1 | 54 | 37.0 | 13 | 8.9 | 0.261 |
| MTKA | 55 | 70.5 | 22 | 28.2 | 1 | 1.3 | 114 | 78.1 | 28 | 19.2 | 4 | 2.7 | 0.067 |
| TKA | 11 | 14.2 | 29 | 37.2 | 38 | 48.7 | 32 | 21.9 | 59 | 40.4 | 55 | 37.7 | 0.822 |
| SH | - | - | 69 | 88.5 | 9 | 11.5 | - | - | 125 | 85.6 | 21 | 14.4 | 0.699 |
| Spearman’s Rank-Order Correlation | ||||
|---|---|---|---|---|
| Control Group | Study Group | |||
| A Pair of Variables | R Spearman | p | R Spearman | p |
| ALPHA 1 and medium pain | −0.15 | 0.189 | 0.07 | 0.369 |
| ALPHA 2 and medium pain | −0.13 | 0.239 | −0.11 | 0.206 |
| BETA and medium pain | −0.06 | 0.620 | 0.11 | 0.204 |
| DELTA and medium pain | 0.06 | 0.604 | −0.06 | 0.494 |
| GAMMA and medium pain | 0.17 | 0.127 | −0.02 | 0.827 |
| LLA and medium pain | −0.11 | 0.336 | 0.03 | 0.687 |
| MTKA and medium pain | 0.05 | 0.682 | 0.05 | 0.516 |
| TKA and medium pain | 0.07 | 0.548 | 0.08 | 0.359 |
| SH and medium pain | 0.17 | 0.142 | 0.03 | 0.718 |
| Schober Test—flexion and medium pain | 0.11 | 0.328 | 0.04 | 0.659 |
| Schober Test—extension and medium pain | 0.17 | 0.145 | −0.03 | 0.762 |
| ALPHA 1 and bleeding intensity | 0.08 | 0.472 | 0.04 | 0.651 |
| ALPHA 2 and bleeding intensity | 0.01 | 0.930 | −0.05 | 0.589 |
| BETA and bleeding intensity | 0.12 | 0.284 | 0.25 | 0.002 |
| DELTA and bleeding intensity | 0.10 | 0.401 | −0.00 | 0.974 |
| GAMMA and bleeding intensity | 0.14 | 0.237 | 0.05 | 0.556 |
| LLA and bleeding intensity | 0.07 | 0.517 | 0.14 | 0.102 |
| MTKA and bleeding intensity | 0.16 | 0.153 | 0.17 | 0.046 |
| TKA and bleeding intensity | 0.14 | 0.226 | 0.21 | 0.013 |
| SH and bleeding intensity | 0.06 | 0.582 | 0.08 | 0.311 |
| Schober Test—flexion and bleeding intensity | 0.08 | 0.470 | −0.03 | 0.691 |
| Schober Test—extension and bleeding intensity | 0.10 | 0.394 | 0.05 | 0.574 |
| ALPHA 1 and periods regularity | 0.05 | 0.667 | −0.06 | 0.500 |
| ALPHA 2 and periods regularity | 0.16 | 0.173 | 0.05 | 0.568 |
| BETA and periods regularity | −0.02 | 0.836 | −0.14 | 0.090 |
| DELTA and periods regularity | 0.22 | 0.049 | 0.01 | 0.933 |
| GAMMA and periods regularity | 0.14 | 0.236 | 0.14 | 0.085 |
| LLA and periods regularity | 0.09 | 0.447 | −0.04 | 0.602 |
| MTKA and periods regularity | 0.10 | 0.392 | −0.07 | 0.410 |
| TKA and periods regularity | 0.02 | 0.880 | 0.04 | 0.663 |
| SH and periods regularity | −0.08 | 0.484 | 0.12 | 0.140 |
| Schober Test—flexion and periods regularity | −0.01 | 0.897 | 0.04 | 0.631 |
| Schober Test—extension and periods regularity | 0.04 | 0.731 | 0.00 | 0.978 |
| ALPHA 1 and menstruation related nuisance | −0.03 | 0.770 | 0.11 | 0.176 |
| ALPHA 2 and menstruation related nuisance | −0.17 | 0.138 | −0.03 | 0.741 |
| BETA and menstruation related nuisance | 0.11 | 0.345 | 0.25 | 0.002 |
| DELTA and menstruation related nuisance | −0.08 | 0.487 | 0.00 | 0.978 |
| GAMMA and menstruation related nuisance | −0.09 | 0.411 | 0.04 | 0.630 |
| LLA and menstruation related nuisance | −0.05 | 0.635 | 0.14 | 0.090 |
| MTKA and menstruation related nuisance | 0.06 | 0.574 | 0.17 | 0.040 |
| TKA and menstruation related nuisance | −0.00 | 0.975 | 0.19 | 0.025 |
| SH and menstruation related nuisance | 0.06 | 0.621 | 0.06 | 0.507 |
| Schober Test—flexion and menstruation related nuisance | −0.06 | 0.601 | −0.06 | 0.470 |
| Schober Test—extension and menstruation related nuisance | 0.03 | 0.765 | −0.08 | 0.338 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walicka-Cupryś, K.; Pelc, A.R.; Pasierb, M.; Płonka, S.; Pal, A.; Rosowska, N. Effect of Lumbar Spine Mobility and Postural Alignment on Menstrual Pain in Young Women. Int. J. Environ. Res. Public Health 2023, 20, 6458. https://doi.org/10.3390/ijerph20156458
Walicka-Cupryś K, Pelc AR, Pasierb M, Płonka S, Pal A, Rosowska N. Effect of Lumbar Spine Mobility and Postural Alignment on Menstrual Pain in Young Women. International Journal of Environmental Research and Public Health. 2023; 20(15):6458. https://doi.org/10.3390/ijerph20156458
Chicago/Turabian StyleWalicka-Cupryś, Katarzyna, Agnieszka Renata Pelc, Mirosław Pasierb, Sylwia Płonka, Agnieszka Pal, and Nikola Rosowska. 2023. "Effect of Lumbar Spine Mobility and Postural Alignment on Menstrual Pain in Young Women" International Journal of Environmental Research and Public Health 20, no. 15: 6458. https://doi.org/10.3390/ijerph20156458






