Physical Activity in Long COVID: A Comparative Study of Exercise Rehabilitation Benefits in Patients with Long COVID, Coronary Artery Disease and Fibromyalgia
Abstract
1. Introduction
2. Materials and Methods
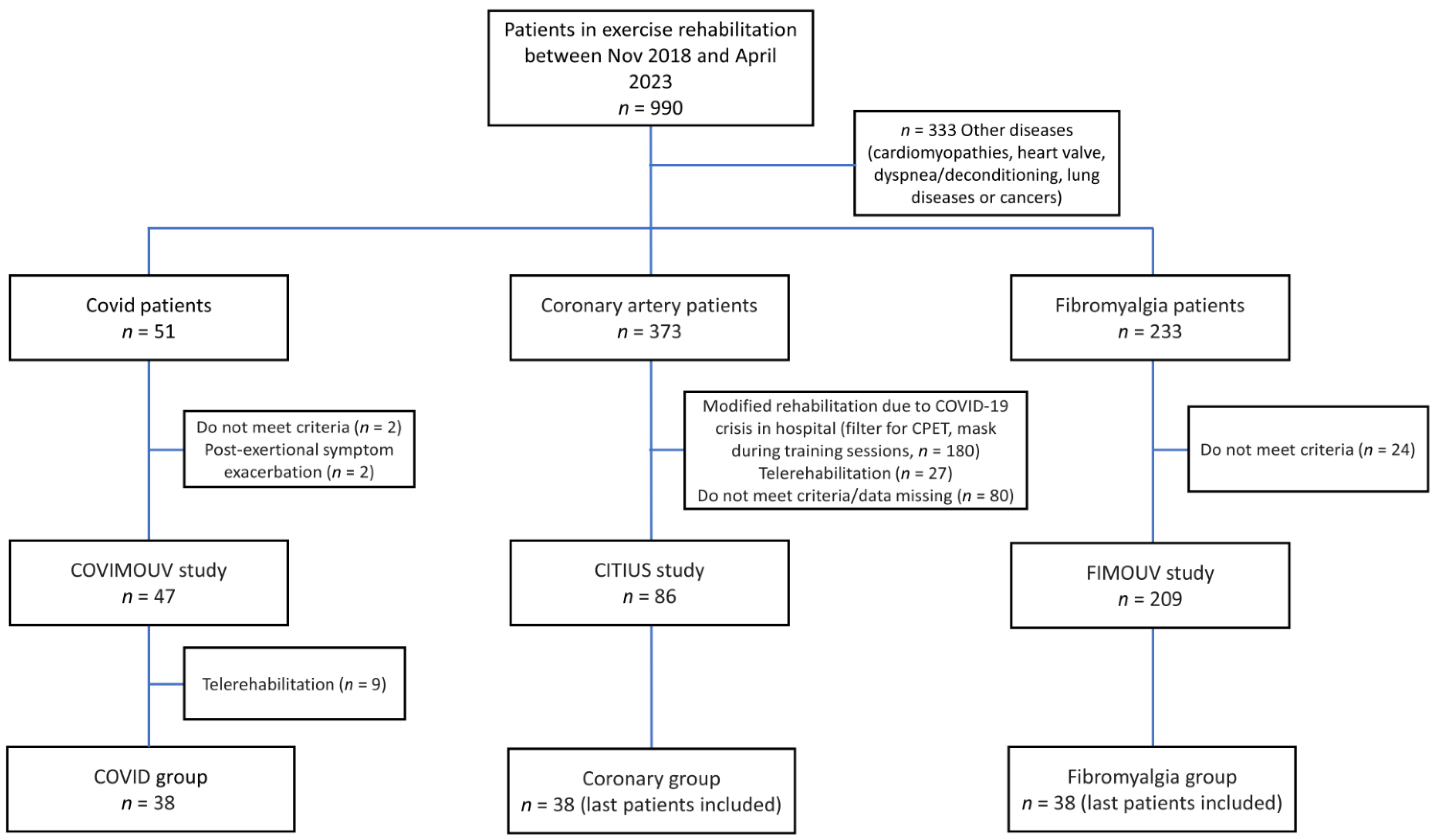
2.1. Study Design
2.2. Exercise Rehabilitation Program
2.3. Assessment Measures
- Aerobic performances: improvement in VO2 peak, VO2 at the first ventilatory threshold (VT1) and maximal aerobic power (MAP) were assessed by a CPET (Vyntus CPX, CareFusion, San Diego, CA, USA);
- Anaerobic performances: improvement in upper limb muscular strength was assessed by a handgrip test (in kg) with a Jamar hydraulic hand dynamometer (JLW instruments, Chicago, IL, USA);
- Cardiac autonomic nervous system (ANS) performances: improvement in resting heart rate (HR), baroreflex sensitivity (BRS) and HRV throughout RMSSD, LF and HF indexes and LF/HF ratio were assessed from a 15′ resting heart recording in the supine position (Finapres Medical Systems BV, Enschede, The Netherlands). BRS assesses the ability to regulate fluctuations in blood pressure and HR through the activation of the sympathetic and orthosympathetic branches of the ANS. Impaired BRS is associated with numerous pathologies, notably cardiovascular, and its reduction is a predictive factor for cardiac mortality [41]. Physiological values of HRV for short-term recording in healthy population have been described by Nunan et al. [42]. Altered ANS in patients is generally characterized by lower parasympathetic activity (mainly measured by RMSSD and HF) and higher sympathetic activity (mainly measured by LF) compared to healthy controls; the LF/HF ratio is therefore higher overall and indicating sympathetic predominance [43,44]. These values were expressed as the natural logarithm to correct the skewed distribution [40].
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Living Guidance for Clinical Management of COVID-19. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2 (accessed on 16 October 2022).
- Santé Publique France. L’affection Post-COVID-19 (Aussi Appelée COVID Long) en France. Résultats de L’enquête Affection Post-COVID, 22 Mars–8 Avril 2022; Santé Publique France: Paris, France, 2022. [Google Scholar]
- Haute Autorité de Santé. Symptômes Prolongés suite à une COVID-19 de L’adulte—Diagnostic et Prise en Charge. Mise à Jour du 19 Novembre 2021. Available online: https://www.has-sante.fr/jcms/p_3237041/fr/symptomes-prolonges-suite-a-une-covid-19-de-l-adulte-diagnostic-et-prise-en-charge (accessed on 16 November 2022).
- Jimeno-Almazán, A.; Pallarés, J.G.; Buendía-Romero, Á.; Martínez-Cava, A.; Franco-López, F.; Sánchez-Alcaraz Martínez, B.J.; Bernal-Morel, E.; Courel-Ibáñez, J. Post-COVID-19 Syndrome and the Potential Benefits of Exercise. Int. J. Environ. Res. Public Health 2021, 18, 5329. [Google Scholar] [CrossRef]
- Mendelson, M.; Nel, J.; Blumberg, L.; Madhi, S.A.; Dryden, M.; Stevens, W.; Venter, F.W.D. Long-COVID: An Evolving Problem with an Extensive Impact. S. Afr. Med. J. 2020, 111, 10–12. [Google Scholar] [CrossRef]
- Vehar, S.; Boushra, M.; Ntiamoah, P.; Biehl, M. Post-Acute Sequelae of SARS-CoV-2 Infection: Caring for the “Long-Haulers”. Cleve Clin. J. Med. 2021, 88, 267–272. [Google Scholar] [CrossRef]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major Findings, Mechanisms and Recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Taquet, M.; Dercon, Q.; Luciano, S.; Geddes, J.R.; Husain, M.; Harrison, P.J. Incidence, Co-Occurrence, and Evolution of Long-COVID Features: A 6-Month Retrospective Cohort Study of 273,618 Survivors of COVID-19. PLoS Med. 2021, 18, e1003773. [Google Scholar] [CrossRef] [PubMed]
- Matheson, G.O.; Klügl, M.; Dvorak, J.; Engebretsen, L.; Meeuwisse, W.H.; Schwellnus, M.; Blair, S.N.; van Mechelen, W.; Derman, W.; Börjesson, M.; et al. Responsibility of Sport and Exercise Medicine in Preventing and Managing Chronic Disease: Applying Our Knowledge and Skill Is Overdue. Br. J. Sports Med. 2011, 45, 1272–1282. [Google Scholar] [CrossRef]
- Bricca, A.; Harris, L.K.; Jäger, M.; Smith, S.M.; Juhl, C.B.; Skou, S.T. Benefits and Harms of Exercise Therapy in People with Multimorbidity: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Ageing Res. Rev. 2020, 63, 101166. [Google Scholar] [CrossRef] [PubMed]
- Steenkamp, L.; Saggers, R.T.; Bandini, R.; Stranges, S.; Choi, Y.-H.; Thornton, J.S.; Hendrie, S.; Patel, D.; Rabinowitz, S.; Patricios, J. Small Steps, Strong Shield: Directly Measured, Moderate Physical Activity in 65,361 Adults Is Associated with Significant Protective Effects from Severe COVID-19 Outcomes. Br. J. Sports Med. 2022, 56, 568–576. [Google Scholar] [CrossRef] [PubMed]
- Prado, A.K.G.; de Almeida Alves, J.C.; Gurginski, R.N.M.; Mikuni, T.; Zata, D.; da Silva Albuquerque, P.L.M.; de Oliveira, J.R.G. Recomendações de exercício físico após adoecimento por COVID-19: Revisão de escopo. Rev. Bras. Atividade Física Saúde 2022, 27, 1–12. [Google Scholar] [CrossRef]
- Cattadori, G.; Di Marco, S.; Baravelli, M.; Picozzi, A.; Ambrosio, G. Exercise Training in Post-COVID-19 Patients: The Need for a Multifactorial Protocol for a Multifactorial Pathophysiology. J. Clin. Med. 2022, 11, 2228. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi Hekmatikar, A.H.; Ferreira Júnior, J.B.; Shahrbanian, S.; Suzuki, K. Functional and Psychological Changes after Exercise Training in Post-COVID-19 Patients Discharged from the Hospital: A PRISMA-Compliant Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 2290. [Google Scholar] [CrossRef]
- de Sire, A.; Moggio, L.; Marotta, N.; Agostini, F.; Tasselli, A.; Drago Ferrante, V.; Curci, C.; Calafiore, D.; Ferraro, F.; Bernetti, A.; et al. Impact of Rehabilitation on Fatigue in Post-COVID-19 Patients: A Systematic Review and Meta-Analysis. Appl. Sci. 2022, 12, 8593. [Google Scholar] [CrossRef]
- Stavrou, V.T.; Vavougios, G.D.; Kalogiannis, P.; Tachoulas, K.; Touloudi, E.; Astara, K.; Mysiris, D.S.; Tsirimona, G.; Papayianni, E.; Boutlas, S.; et al. Breathlessness and Exercise with Virtual Reality System in Long-Post-Coronavirus Disease 2019 Patients. Front. Public Health 2023, 11, 1115393. [Google Scholar] [CrossRef]
- Aparisi, Á.; Ladrón, R.; Ybarra-Falcón, C.; Tobar, J.; San Román, J.A. Exercise Intolerance in Post-Acute Sequelae of COVID-19 and the Value of Cardiopulmonary Exercise Testing—A Mini-Review. Front. Med. 2022, 9, 924819. [Google Scholar] [CrossRef] [PubMed]
- Wichi, R.B.; De Angelis, K.; Jones, L.; Irigoyen, M.C. A Brief Review of Chronic Exercise Intervention to Prevent Autonomic Nervous System Changes during the Aging Process. Clinics 2009, 64, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Blitshteyn, S.; Whiteson, J.H.; Abramoff, B.; Azola, A.; Bartels, M.N.; Bhavaraju-Sanka, R.; Chung, T.; Fleming, T.K.; Henning, E.; Miglis, M.G.; et al. Multi-Disciplinary Collaborative Consensus Guidance Statement on the Assessment and Treatment of Autonomic Dysfunction in Patients with Post-Acute Sequelae of SARS-CoV-2 Infection (PASC). PM R 2022, 14, 1270–1291. [Google Scholar] [CrossRef] [PubMed]
- Décary, S.; Gaboury, I.; Poirier, S.; Garcia, C.; Simpson, S.; Bull, M.; Brown, D.; Daigle, F. Humility and Acceptance: Working Within Our Limits With Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. J. Orthop. Sports Phys. Ther. 2021, 51, 197–200. [Google Scholar] [CrossRef]
- Torjesen, I. NICE Backtracks on Graded Exercise Therapy and CBT in Draft Revision to CFS Guidance. BMJ 2020, 371, m4356. [Google Scholar] [CrossRef] [PubMed]
- Pavy, B.; Iliou, M.-C.; Vergès-Patois, B.; Brion, R.; Monpère, C.; Carré, F.; Aeberhard, P.; Argouach, C.; Borgne, A.; Consoli, S.; et al. French Society of Cardiology Guidelines for Cardiac Rehabilitation in Adults. Arch. Cardiovasc. Dis. 2012, 105, 309–328. [Google Scholar] [CrossRef]
- Pelliccia, A.; Sharma, S.; Gati, S.; Bäck, M.; Börjesson, M.; Caselli, S.; Collet, J.-P.; Corrado, D.; Drezner, J.A.; Halle, M.; et al. 2020 ESC Guidelines on Sports Cardiology and Exercise in Patients with Cardiovascular Disease: The Task Force on Sports Cardiology and Exercise in Patients with Cardiovascular Disease of the European Society of Cardiology (ESC). Eur. Heart J. 2021, 42, 17–96. [Google Scholar] [CrossRef]
- Cathébras, P.; Goutte, J.; Gramont, B.; Killian, M. «COVID long»: Une opportunité pour approcher la complexité des syndromes fonctionnels post-infectieux. Rev. Médecine Interne 2021, 42, 492–497. [Google Scholar] [CrossRef] [PubMed]
- Ranque, B. Appeler Un Chat Un Chat. Rev. Med. Interne 2021, 42, 449–451. [Google Scholar] [CrossRef] [PubMed]
- Dotan, A.; David, P.; Arnheim, D.; Shoenfeld, Y. The Autonomic Aspects of the Post-COVID19 Syndrome. Autoimmun. Rev. 2022, 21, 103071. [Google Scholar] [CrossRef] [PubMed]
- Macfarlane, G.J.; Kronisch, C.; Dean, L.E.; Atzeni, F.; Häuser, W.; Fluß, E.; Choy, E.; Kosek, E.; Amris, K.; Branco, J.; et al. EULAR Revised Recommendations for the Management of Fibromyalgia. Ann. Rheum. Dis. 2017, 76, 318–328. [Google Scholar] [CrossRef] [PubMed]
- Bidonde, J.; Busch, A.J.; Schachter, C.L.; Webber, S.C.; Musselman, K.E.; Overend, T.J.; Góes, S.M.; Dal Bello-Haas, V.; Boden, C. Mixed Exercise Training for Adults with Fibromyalgia. Cochrane Database Syst. Rev. 2019, 5, CD013340. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, C.W.; While, A.E. Cardiac Rehabilitation and Quality of Life: A Systematic Review. Int. J. Nurs. Stud. 2012, 49, 755–771. [Google Scholar] [CrossRef] [PubMed]
- Candelaria, D.; Randall, S.; Ladak, L.; Gallagher, R. Health-Related Quality of Life and Exercise-Based Cardiac Rehabilitation in Contemporary Acute Coronary Syndrome Patients: A Systematic Review and Meta-Analysis. Qual. Life Res. 2020, 29, 579–592. [Google Scholar] [CrossRef]
- da Silva, J.M.; de Barros, B.S.; Almeida, G.J.; O’Neil, J.; Imoto, A.M. Dosage of Resistance Exercises in Fibromyalgia: Evidence Synthesis for a Systematic Literature Review up-Date and Meta-Analysis. Rheumatol. Int. 2021, 42, 413–429. [Google Scholar] [CrossRef]
- Clavario, P.; De Marzo, V.; Lotti, R.; Barbara, C.; Porcile, A.; Russo, C.; Beccaria, F.; Bonavia, M.; Bottaro, L.C.; Caltabellotta, M.; et al. Cardiopulmonary Exercise Testing in COVID-19 Patients at 3 Months Follow-Up. Int. J. Cardiol. 2021, 340, 113–118. [Google Scholar] [CrossRef]
- Chaves-García, M.; Sandoval-Cuellar, C.; Calero-Saa, P. Association between aerobic capacity and quality of life in older adults in Colombia. Rev. Peru. Med. Exp. Salud Publica 2017, 34, 672–676. [Google Scholar] [CrossRef]
- Hager, A.; Hess, J. Comparison of Health Related Quality of Life with Cardiopulmonary Exercise Testing in Adolescents and Adults with Congenital Heart Disease. Heart 2005, 91, 517–520. [Google Scholar] [CrossRef] [PubMed]
- Valim, V.; Oliveira, L.M.; Suda, A.L.; Silva, L.E.; Faro, M.; Neto, T.L.B.; Feldman, D.; Natour, J. Peak Oxygen Uptake and Ventilatory Anaerobic Threshold in Fibromyalgia. J. Rheumatol. 2002, 29, 353–357. [Google Scholar] [PubMed]
- American College of Sports Medicine, G. Acsm’s Guidelines for Exercise Testing and Prescription, 11th ed.; Wolters Kluwer Health: Philadelphia, PA, USA, 2021; ISBN 978-1-975150-18-1. [Google Scholar]
- Togo, F.; Takahashi, M. Heart Rate Variability in Occupational Health—A Systematic Review. Ind. Health 2009, 47, 589–602. [Google Scholar] [CrossRef] [PubMed]
- Marsac, J. Variabilité de la fréquence cardiaque: Un marqueur de risque cardiométabolique en santé publique. Bull. L’académie Natl. Médecine 2013, 197, 175–186. [Google Scholar] [CrossRef]
- Besson, C.; Saubade, M.; Gremeaux, V.; Millet, G.P.; Schmitt, L. Analyse de la variabilité de la fréquence cardiaque: Méthodes, limites et exemples cliniques. Rev. Med. Suisse 2020, 701, 1432–1437. [Google Scholar] [CrossRef]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef]
- La Rovere, M.T.; Bigger, J.T.; Marcus, F.I.; Mortara, A.; Schwartz, P.J. Baroreflex Sensitivity and Heart-Rate Variability in Prediction of Total Cardiac Mortality after Myocardial Infarction. ATRAMI (Autonomic Tone and Reflexes After Myocardial Infarction) Investigators. Lancet 1998, 351, 478–484. [Google Scholar] [CrossRef]
- Nunan, D.; Sandercock, G.R.H.; Brodie, D.A. A Quantitative Systematic Review of Normal Values for Short-Term Heart Rate Variability in Healthy Adults. Pacing Clin. Electrophysiol. 2010, 33, 1407–1417. [Google Scholar] [CrossRef]
- Venkatesh, D.; Anahita, R.S.; Prakash, V.S. Alteration of Heart Rate Variability in Patients with Coronary Artery Disease. Natl. J. Physiol. Pharm. Pharmacol. 2018, 8, 820–823. [Google Scholar] [CrossRef]
- Tracy, L.M.; Ioannou, L.; Baker, K.S.; Gibson, S.J.; Georgiou-Karistianis, N.; Giummarra, M.J. Meta-Analytic Evidence for Decreased Heart Rate Variability in Chronic Pain Implicating Parasympathetic Nervous System Dysregulation. Pain 2016, 157, 7–29. [Google Scholar] [CrossRef]
- Alba, G.A.; Ziehr, D.R.; Rouvina, J.N.; Hariri, L.P.; Knipe, R.S.; Medoff, B.D.; Hibbert, K.A.; Kowal, A.; Hoenstine, C.; Ginns, L.C.; et al. Exercise Performance in Patients with Post-Acute Sequelae of SARS-CoV-2 Infection Compared to Patients with Unexplained Dyspnea. eClinicalMedicine 2021, 39, 101066. [Google Scholar] [CrossRef] [PubMed]
- Cassar, M.P.; Tunnicliffe, E.M.; Petousi, N.; Lewandowski, A.J.; Xie, C.; Mahmod, M.; Samat, A.H.A.; Evans, R.A.; Brightling, C.E.; Ho, L.-P.; et al. Symptom Persistence Despite Improvement in Cardiopulmonary Health—Insights from Longitudinal CMR, CPET and Lung Function Testing Post-COVID-19. eClinicalMedicine 2021, 41, 101159. [Google Scholar] [CrossRef] [PubMed]
- Ladlow, P.; O’Sullivan, O.; Houston, A.; Barker-Davies, R.; May, S.; Mills, D.; Dewson, D.; Chamley, R.; Naylor, J.; Mulae, J.; et al. Dysautonomia Following COVID-19 Is Not Associated with Subjective Limitations or Symptoms but Is Associated with Objective Functional Limitations. Heart Rhythm. 2022, 19, 613–620. [Google Scholar] [CrossRef]
- Haunhorst, S.; Bloch, W.; Wagner, H.; Ellert, C.; Krüger, K.; Vilser, D.C.; Finke, K.; Reuken, P.; Pletz, M.W.; Stallmach, A.; et al. Long COVID: A Narrative Review of the Clinical Aftermaths of COVID-19 with a Focus on the Putative Pathophysiology and Aspects of Physical Activity. Oxf. Open Immunol. 2022, 3, iqac006. [Google Scholar] [CrossRef] [PubMed]
- Durstenfeld, M.S.; Sun, K.; Tahir, P.; Peluso, M.J.; Deeks, S.G.; Aras, M.A.; Grandis, D.J.; Long, C.S.; Beatty, A.; Hsue, P.Y. Use of Cardiopulmonary Exercise Testing to Evaluate Long COVID-19 Symptoms in Adults: A Systematic Review and Meta-Analysis. JAMA Netw. Open 2022, 5, e2236057. [Google Scholar] [CrossRef]
- Barbagelata, L.; Masson, W.; Iglesias, D.; Lillo, E.; Migone, J.F.; Orazi, M.L.; Maritano Furcada, J. Cardiopulmonary Exercise Testing in Patients with Post-COVID-19 Syndrome. Med. Clín. (Engl. Ed.) 2021, 159, 6–11. [Google Scholar] [CrossRef]
- Contreras, A.M.; Newman, D.B.; Cappelloni, L.; Niven, A.S.; Mueller, M.R.; Ganesh, R.; Squires, R.W.; Bonikowske, A.R.; Allison, T.G. Cardiopulmonary Testing in Long COVID-19 versus Non–COVID-19 Patients with Undifferentiated Dyspnea on Exertion. Prog. Cardiovasc. Dis. 2023. [Google Scholar] [CrossRef]
- Rinaldo, R.F.; Mondoni, M.; Parazzini, E.M.; Pitari, F.; Brambilla, E.; Luraschi, S.; Balbi, M.; Sferrazza Papa, G.F.; Sotgiu, G.; Guazzi, M.; et al. Deconditioning as Main Mechanism of Impaired Exercise Response in COVID-19 Survivors. Eur. Respir. J. 2021, 58, 2100870. [Google Scholar] [CrossRef]
- Vannini, L.; Quijada-Fumero, A.; Martín, M.P.R.; Pina, N.C.; Afonso, J.S.H. Cardiopulmonary Exercise Test with Stress Echocardiography in COVID-19 Survivors at 6 Months Follow-Up. Eur. J. Intern. Med. 2021, 94, 101–104. [Google Scholar] [CrossRef]
- Townsend, L.; Dyer, A.H.; Jones, K.; Dunne, J.; Mooney, A.; Gaffney, F.; O’Connor, L.; Leavy, D.; O’Brien, K.; Dowds, J.; et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS ONE 2020, 15, e0240784. [Google Scholar] [CrossRef]
- O’Sullivan, O.; Barker-Davies, R.M.; Thompson, K.; Bahadur, S.; Gough, M.; Lewis, S.; Martin, M.; Segalini, A.; Wallace, G.; Phillip, R.; et al. Rehabilitation Post-COVID-19: Cross-Sectional Observations Using the Stanford Hall Remote Assessment Tool. BMJ Mil. Health 2021, 169, 243–248. [Google Scholar] [CrossRef]
- Maquet, D.; Demoulin, C.; Croisier, J.-L.; Crielaard, J.-M. Benefits of Physical Training in Fibromyalgia and Related Syndromes. Ann. Réadapt. Méd. Phys. 2007, 50, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Lorenzen, I. Fibromyalgia: A Clinical Challenge. J. Intern. Med. 1994, 235, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Cathebras, P. Troubles Fonctionnels et Somatisation: Comment Aborder les Symptômes Médicalement Inexpliqués; Elsevier Masson: Paris, France, 2006; ISBN 978-2-294-01652-3. [Google Scholar]
- de Sire, A.; Andrenelli, E.; Negrini, F.; Lazzarini, S.G.; Cordani, C.; Ceravolo, M.G.; International Multiprofessional Steering Committee of Cochrane Rehabilitation REH-COVER Action. Rehabilitation and COVID-19: Update of the Rapid Living Systematic Review by Cochrane Rehabilitation Field as of February 28th, 2022. Eur. J. Phys. Rehabil. Med. 2022, 58, 498–501. [Google Scholar] [CrossRef] [PubMed]
- Araújo, B.T.S.; Barros, A.E.V.R.; Nunes, D.T.X.; Remígio de Aguiar, M.I.; Mastroianni, V.W.; de Souza, J.A.F.; Fernades, J.; Campos, S.L.; Brandão, D.C.; Dornelas de Andrade, A. Effects of Continuous Aerobic Training Associated with Resistance Training on Maximal and Submaximal Exercise Tolerance, Fatigue, and Quality of Life of Patients Post-COVID-19. Physiother. Res. Int. 2022, 28, e1972. [Google Scholar] [CrossRef]
- Barbara, C.; Clavario, P.; De Marzo, V.; Lotti, R.; Guglielmi, G.; Porcile, A.; Russo, C.; Griffo, R.; Mäkikallio, T.; Hautala, A.J.; et al. Effects of Exercise Rehabilitation in Patients with Long COVID-19. Eur. J. Prev. Cardiol. 2022, 29, e258–e260. [Google Scholar] [CrossRef]
- Stavrou, V.T.; Vavougios, G.D.; Boutlas, S.; Tourlakopoulos, K.N.; Papayianni, E.; Astara, K.; Stavrou, I.T.; Daniil, Z.; Gourgoulianis, K.I. Physical Fitness Differences, Amenable to Hypoxia-Driven and Sarcopenia Pathophysiology, between Sleep Apnea and COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 669. [Google Scholar] [CrossRef]
- Halaweh, H. Correlation between Health-Related Quality of Life and Hand Grip Strength among Older Adults. Exp. Aging Res. 2020, 46, 178–191. [Google Scholar] [CrossRef]
- de Sevilla, G.G.P.; Sánchez-Pinto, B. Associations between Muscle Strength, Dyspnea and Quality of Life in Post-COVID-19 Patients. Rev. Assoc. Med. Bras. 2022, 68, 1753–1758. [Google Scholar] [CrossRef]
- Dani, M.; Dirksen, A.; Taraborrelli, P.; Torocastro, M.; Panagopoulos, D.; Sutton, R.; Lim, P.B. Autonomic Dysfunction in “Long COVID”: Rationale, Physiology and Management Strategies. Clin. Med. 2021, 21, e63–e67. [Google Scholar] [CrossRef]
- Jamoulle, M.; Kazeneza-Mugisha, G.; Zayane, A. Follow-Up of a Cohort of Patients with Post-Acute COVID-19 Syndrome in a Belgian Family Practice. Viruses 2022, 14, 2000. [Google Scholar] [CrossRef] [PubMed]
- Szekely, Y.; Lichter, Y.; Sadon, S.; Lupu, L.; Taieb, P.; Banai, A.; Sapir, O.; Granot, Y.; Hochstadt, A.; Friedman, S.; et al. Cardiorespiratory Abnormalities in Patients Recovering from Coronavirus Disease 2019. J. Am. Soc. Echocardiogr. 2021, 34, 1273–1284.e9. [Google Scholar] [CrossRef] [PubMed]
- Barizien, N.; Le Guen, M.; Russel, S.; Touche, P.; Huang, F.; Vallée, A. Clinical Characterization of Dysautonomia in Long COVID-19 Patients. Sci. Rep. 2021, 11, 14042. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, L.d.F.; Pianowski, G.; Gonçalves, A.P.; Carvalho, L.d.F.; Pianowski, G.; Gonçalves, A.P. Personality Differences and COVID-19: Are Extroversion and Conscientiousness Personality Traits Associated with Engagement with Containment Measures? Trends Psychiatry Psychother. 2020, 42, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Suh, H.-W.; Kwon, C.-Y.; Lee, B. Long-Term Impact of COVID-19 on Heart Rate Variability: A Systematic Review of Observational Studies. Healthcare 2023, 11, 1095. [Google Scholar] [CrossRef]
- Barthelemy, J.-C.; Pichot, V.; Hupin, D.; Berger, M.; Celle, S.; Mouhli, L.; Bäck, M.; Lacour, J.-R.; Roche, F. Targeting Autonomic Nervous System as a Biomarker of Well-Ageing in the Prevention of Stroke. Front. Aging Neurosci. 2022, 14, 969352. [Google Scholar] [CrossRef]
- Manresa-Rocamora, A.; Ribeiro, F.; Sarabia, J.M.; Íbias, J.; Oliveira, N.L.; Vera-García, F.J.; Moya-Ramón, M. Exercise-Based Cardiac Rehabilitation and Parasympathetic Function in Patients with Coronary Artery Disease: A Systematic Review and Meta-Analysis. Clin. Auton. Res. 2021, 31, 187–203. [Google Scholar] [CrossRef]
- Kulshreshtha, P.; Deepak, K.K. Autonomic Nervous System Profile in Fibromyalgia Patients and Its Modulation by Exercise: A Mini Review. Clin. Physiol. Funct. Imaging 2013, 33, 83–91. [Google Scholar] [CrossRef]
- Fritz, C.; Hock, J.; Oberhoffer, R.; Hager, A.; Ewert, P.; Müller, J. Reduced Parasympathetic Activity in Patients With Different Types of Congenital Heart Disease and Associations to Exercise Capacity. J. Cardiopulm. Rehabil. Prev. 2021, 41, 35–39. [Google Scholar] [CrossRef]
- Kaliyaperumal, D.; Rk, K.; Alagesan, M.; Ramalingam, S. Characterization of Cardiac Autonomic Function in COVID-19 Using Heart Rate Variability: A Hospital Based Preliminary Observational Study. J. Basic Clin. Physiol. Pharmacol. 2021, 32, 247–253. [Google Scholar] [CrossRef]
- Menezes Junior, A.d.S.; Schröder, A.A.; Botelho, S.M.; Resende, A.L. Cardiac Autonomic Function in Long COVID-19 Using Heart Rate Variability: An Observational Cross-Sectional Study. J. Clin. Med. 2022, 12, 100. [Google Scholar] [CrossRef] [PubMed]
- Asarcikli, L.D.; Hayiroglu, M.İ.; Osken, A.; Keskin, K.; Kolak, Z.; Aksu, T. Heart Rate Variability and Cardiac Autonomic Functions in Post-COVID Period. J. Interv. Card. Electrophysiol. 2022, 63, 715–721. [Google Scholar] [CrossRef] [PubMed]
- Garavaglia, L.; Gulich, D.; Defeo, M.M.; Thomas Mailland, J.; Irurzun, I.M. The Effect of Age on the Heart Rate Variability of Healthy Subjects. PLoS ONE 2021, 16, e0255894. [Google Scholar] [CrossRef] [PubMed]
- Antelmi, I.; de Paula, R.S.; Shinzato, A.R.; Peres, C.A.; Mansur, A.J.; Grupi, C.J. Influence of Age, Gender, Body Mass Index, and Functional Capacity on Heart Rate Variability in a Cohort of Subjects without Heart Disease. Am. J. Cardiol. 2004, 93, 381–385. [Google Scholar] [CrossRef]
- Tiwari, R.; Kumar, R.; Malik, S.; Raj, T.; Kumar, P. Analysis of Heart Rate Variability and Implication of Different Factors on Heart Rate Variability. Curr. Cardiol. Rev. 2021, 17, e160721189770. [Google Scholar] [CrossRef]
- Fu, Q.; Levine, B.D. Exercise and the Autonomic Nervous System. Handb. Clin. Neurol. 2013, 117, 147–160. [Google Scholar] [CrossRef]
- Besnier, F.; Labrunée, M.; Pathak, A.; Pavy-Le Traon, A.; Galès, C.; Sénard, J.-M.; Guiraud, T. Exercise Training-Induced Modification in Autonomic Nervous System: An Update for Cardiac Patients. Ann. Phys. Rehabil. Med. 2017, 60, 27–35. [Google Scholar] [CrossRef]
- Kingsley, J.D.; Figueroa, A. Acute and Training Effects of Resistance Exercise on Heart Rate Variability. Clin. Physiol. Funct. Imaging 2016, 36, 179–187. [Google Scholar] [CrossRef]
- Duru, F.; Candinas, R.; Dziekan, G.; Goebbels, U.; Myers, J.; Dubach, P. Effect of Exercise Training on Heart Rate Variability in Patients with New-Onset Left Ventricular Dysfunction after Myocardial Infarction. Am. Heart J. 2000, 140, 157–161. [Google Scholar] [CrossRef]
- Kingsley, J.D.; McMillan, V.; Figueroa, A. The Effects of 12 Weeks of Resistance Exercise Training on Disease Severity and Autonomic Modulation at Rest and after Acute Leg Resistance Exercise in Women with Fibromyalgia. Arch. Phys. Med. Rehabil. 2010, 91, 1551–1557. [Google Scholar] [CrossRef]
- Bardal, E.M.; Roeleveld, K.; Mork, P.J. Aerobic and Cardiovascular Autonomic Adaptations to Moderate Intensity Endurance Exercise in Patients with Fibromyalgia. J. Rehabil. Med. 2015, 47, 639–646. [Google Scholar] [CrossRef] [PubMed]
- Murad, K.; Brubaker, P.H.; Fitzgerald, D.M.; Morgan, T.M.; Goff, D.C.; Soliman, E.Z.; Eggebeen, J.D.; Kitzman, D.W. Exercise Training Improves Heart Rate Variability in Older Patients with Heart Failure: A Randomized, Controlled, Single-Blinded Trial. Congest. Heart Fail. 2012, 18, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Villafaina, S.; Collado-Mateo, D.; Domínguez-Muñoz, F.J.; Gusi, N.; Fuentes-Garcia, J.P. Effects of Exergames on Heart Rate Variability of Women with Fibromyalgia: A Randomized Controlled Trial. Sci. Rep. 2020, 10, 5168. [Google Scholar] [CrossRef]
- Sañudo, B.; Carrasco, L.; de Hoyo, M.; Figueroa, A.; Saxton, J.M. Vagal Modulation and Symptomatology Following a 6-Month Aerobic Exercise Program for Women with Fibromyalgia. Clin. Exp. Rheumatol. 2015, 33, S41–S45. [Google Scholar] [PubMed]
- Del Valle, M.F.; Valenzuela, J.; Marzuca-Nassr, G.N.; Cabrera-Inostroza, C.; Del Sol, M.; Lizana, P.A.; Escobar-Cabello, M.; Muñoz-Cofre, R. Eight Weeks of Supervised Pulmonary Rehabilitation Are Effective in Improving Resting Heart Rate and Heart Rate Recovery in Severe COVID-19 Patient Survivors of Mechanical Ventilation. Medicina 2022, 58, 514. [Google Scholar] [CrossRef]
- Udina, C.; Ars, J.; Morandi, A.; Vilaró, J.; Cáceres, C.; Inzitari, M. Rehabilitation in Adult Post-COVID-19 Patients in Post-Acute Care with Therapeutic Exercise. J. Frailty Aging 2021, 10, 297–300. [Google Scholar] [CrossRef]
- Daynes, E.; Baldwin, M.; Greening, N.J.; Yates, T.; Bishop, N.C.; Mills, G.; Roberts, M.; Hamrouni, M.; Plekhanova, T.; Vogiatzis, I.; et al. The Effect of COVID Rehabilitation for Ongoing Symptoms Post HOSPitalisation with COVID-19 (PHOSP-R): Protocol for a Randomised Parallel Group Controlled Trial on Behalf of the PHOSP Consortium. Trials 2023, 24, 61. [Google Scholar] [CrossRef]
- Del Corral, T.; Fabero-Garrido, R.; Plaza-Manzano, G.; Fernández-de-Las-Peñas, C.; Navarro-Santana, M.; López-de-Uralde-Villanueva, I. Home-Based Respiratory Muscle Training on Quality of Life and Exercise Tolerance in Long-Term Post-COVID-19: Randomized Controlled Trial. Ann. Phys. Rehabil. Med. 2023, 66, 101709. [Google Scholar] [CrossRef]
- Cahalan, R.M.; Meade, C.; Mockler, S. SingStrong-A Singing and Breathing Retraining Intervention for Respiratory and Other Common Symptoms of Long COVID: A Pilot Study. Can. J. Respir. Ther. 2022, 58, 20–27. [Google Scholar] [CrossRef]
- Groenveld, T.; Achttien, R.; Smits, M.; de Vries, M.; van Heerde, R.; Staal, B.; van Goor, H.; COVID Rehab Group. Feasibility of Virtual Reality Exercises at Home for Post-COVID-19 Condition: Cohort Study. JMIR Rehabil. Assist. Technol. 2022, 9, e36836. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Sivan, M.; Delaney, B.; Evans, R.; Milne, R. Long Covid—An Update for Primary Care. BMJ 2022, 378, e072117. [Google Scholar] [CrossRef] [PubMed]
- Wahlgren, C.; Divanoglou, A.; Larsson, M.; Nilsson, E.; Östholm Balkhed, Å.; Niward, K.; Birberg Thornberg, U.; Lilliecreutz Gudmundsson, E.; Levi, R. Rehabilitation Needs Following COVID-19: Five-Month Post-Discharge Clinical Follow-up of Individuals with Concerning Self-Reported Symptoms. eClinicalMedicine 2022, 43, 101219. [Google Scholar] [CrossRef] [PubMed]
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re’em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing Long COVID in an International Cohort: 7 Months of Symptoms and Their Impact. eClinicalMedicine 2021, 38, 101019. [Google Scholar] [CrossRef]
- Twomey, R.; DeMars, J.; Franklin, K.; Culos-Reed, S.N.; Weatherald, J.; Wrightson, J.G. Chronic Fatigue and Postexertional Malaise in People Living With Long COVID: An Observational Study. Phys. Ther. 2022, 102, pzac005. [Google Scholar] [CrossRef]
- Coscia, F.; Mancinelli, R.; Gigliotti, P.V.; Checcaglini, F.; Fanò-Illic, G. Physical Activity Effects on Muscle Fatigue in Sport in Active Adults with Long COVID-19: An Observational Study. Diagnostics 2023, 13, 1336. [Google Scholar] [CrossRef]
- Fairbank, R. Long COVID Exercise Trials Proposed by NIH Raise Alarm. Nature 2023, 616, 228–229. [Google Scholar] [CrossRef]
- Wright, J.; Astill, S.L.; Sivan, M. The Relationship between Physical Activity and Long COVID: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 5093. [Google Scholar] [CrossRef]
- Parker, M.; Sawant, H.B.; Flannery, T.; Tarrant, R.; Shardha, J.; Bannister, R.; Ross, D.; Halpin, S.; Greenwood, D.C.; Sivan, M. Effect of Using a Structured Pacing Protocol on Post-Exertional Symptom Exacerbation and Health Status in a Longitudinal Cohort with the Post-COVID-19 Syndrome. J. Med. Virol. 2023, 95, e28373. [Google Scholar] [CrossRef]
- World Health Organization. Support for Rehabilitation: Self-Management after COVID-19-Related Illness, 2nd ed.; World Health Organization. Regional Office for Europe: Copenhagen, Denmark, 2021.
- Cotler, J.; Holtzman, C.; Dudun, C.; Jason, L.A. A Brief Questionnaire to Assess Post-Exertional Malaise. Diagnostics 2018, 8, 66. [Google Scholar] [CrossRef] [PubMed]
| Variable | COVID Group (n = 38) | Coronary Group (n = 38) | Fibromyalgia Group (n = 38) | p-Value |
|---|---|---|---|---|
| Age (y) | 46.9 ± 12.7 | 61.4 ± 9.45 | 47.4 ± 9.93 | <0.001 * |
| Females | 21 (55) | 9 (24) | 35 (92) | <0.001 * |
| BMI (kg.m−2) | 25.4 ± 5.44 | 26.3 ± 4.45 | 28.1 ± 6.57 | 0.175 |
| Physical activity | 25 (66) | 20 (53) | 17 (45) | 0.131 |
| Tobacco | 14 (37) | 29 (76) | 11 (29) | <0.001 * |
| Variable | COVID Group | Coronary Group | Fibromyalgia Group | Time Effect p-Value | Effect Size | Group Effect p-Value | Time-by-Group Interaction p-Value | |||
|---|---|---|---|---|---|---|---|---|---|---|
| PRE | POST | PRE | POST | PRE | POST | |||||
| Cardiorespiratory | ||||||||||
| VO2 at VT1 (mL·min−1·kg−1) | 15.6 ± 5.03 | 17.3 ± 4.74 | 12.4 ± 3.49 | 13.3 ± 4.10 | 13.5 ± 3.49 | 15.2 ± 3.96 | <0.001 | 1.5013 | 0.020 | 0.517 |
| VO2 peak (mL·min−1·kg−1) | 23.0 ± 5.92 | 27.0 ± 7.22 * | 19.0 ± 4.52 | 20.4 ± 5.25 * | 19.7 ± 4.83 | 22.8 ± 6.18 | <0.001 | 2.928 | 0.039 | 0.019 |
| MAP (W) | 133 ± 50.9 | 154 ± 55.7 | 105 ± 29.9 | 124 ± 33.8 | 95 ± 36.4 | 112 ± 40.4 | <0.001 | 18.711 | 0.031 | 0.756 |
| Muscular | ||||||||||
| Handgrip force (kg) | 31.3 ± 10.1 | 35.7 ± 10.0 | 34.4 ± 9.08 | 36.6 ± 10.5 | 21.9 ± 10.6 | 28.7 ± 11.3 * | <0.001 | 4.636 | 0.121 | 0.059 |
| Autonomic | ||||||||||
| Resting HR (bpm) | 88.8 ± 13.7 | 85.4 ± 11.9 | 69.8 ± 9.52 | 68.0 ± 12.8 | 78.6 ± 14.6 | 77.3 ± 10.9 | 0.059 | −2.0925 | <0.001 | 0.634 |
| BRS (ms·mmHg−1) | 6.06 ± 3.02 | 7.29 ± 3.02 | 7.03 ± 5.54 | 8.95 ± 12.3 | 6.78 ± 5.48 | 7.31 ± 4.48 | 0.580 | 1.1809 | 0.276 | 0.821 |
| RMSSD (ms) | 27.7 ± 12.5 | 31.0 ± 13.3 | 36.4 ± 27.9 | 41.8 ± 41.0 | 20.9 ± 16.8 | 23.5 ± 19.2 | 0.082 | 3.231 | 0.045 | 0.994 |
| LF (ms2) a | 5.30 ± 1.06 | 5.30 ± 1.34 | 4.70 ± 1.54 | 5.07 ± 1.62 | 5.45 ± 2.05 | 5.44 ± 1.05 | 0.430 | 0.1367 | 0.231 | 0.510 |
| HF (ms2) a | 4.43 ± 1.17 | 4.39 ± 1.32 | 4.20 ± 1.49 | 4.39 ± 1.55 | 4.81 ± 1.67 | 4.84 ± 1.03 | 0.630 | 0.0781 | 0.419 | 0.863 |
| LF/HF a | 0.868 ± 0.965 | 1.08 ± 1.31 | 0.506 ± 0.749 | 0.679 ± 0.660 | 0.633 ± 0.964 | 0.598 ± 0.912 | 0.246 | 0.1198 | 0.224 | 0.482 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Colas, C.; Le Berre, Y.; Fanget, M.; Savall, A.; Killian, M.; Goujon, I.; Labeix, P.; Bayle, M.; Féasson, L.; Roche, F.; et al. Physical Activity in Long COVID: A Comparative Study of Exercise Rehabilitation Benefits in Patients with Long COVID, Coronary Artery Disease and Fibromyalgia. Int. J. Environ. Res. Public Health 2023, 20, 6513. https://doi.org/10.3390/ijerph20156513
Colas C, Le Berre Y, Fanget M, Savall A, Killian M, Goujon I, Labeix P, Bayle M, Féasson L, Roche F, et al. Physical Activity in Long COVID: A Comparative Study of Exercise Rehabilitation Benefits in Patients with Long COVID, Coronary Artery Disease and Fibromyalgia. International Journal of Environmental Research and Public Health. 2023; 20(15):6513. https://doi.org/10.3390/ijerph20156513
Chicago/Turabian StyleColas, Claire, Yann Le Berre, Marie Fanget, Angélique Savall, Martin Killian, Ivan Goujon, Pierre Labeix, Manon Bayle, Léonard Féasson, Frederic Roche, and et al. 2023. "Physical Activity in Long COVID: A Comparative Study of Exercise Rehabilitation Benefits in Patients with Long COVID, Coronary Artery Disease and Fibromyalgia" International Journal of Environmental Research and Public Health 20, no. 15: 6513. https://doi.org/10.3390/ijerph20156513
APA StyleColas, C., Le Berre, Y., Fanget, M., Savall, A., Killian, M., Goujon, I., Labeix, P., Bayle, M., Féasson, L., Roche, F., & Hupin, D. (2023). Physical Activity in Long COVID: A Comparative Study of Exercise Rehabilitation Benefits in Patients with Long COVID, Coronary Artery Disease and Fibromyalgia. International Journal of Environmental Research and Public Health, 20(15), 6513. https://doi.org/10.3390/ijerph20156513






