Socio-Economic Factors Associated with Ethnic Disparities in SARS-CoV-2 Infection and Hospitalization
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Socio-Demographic Characteristics
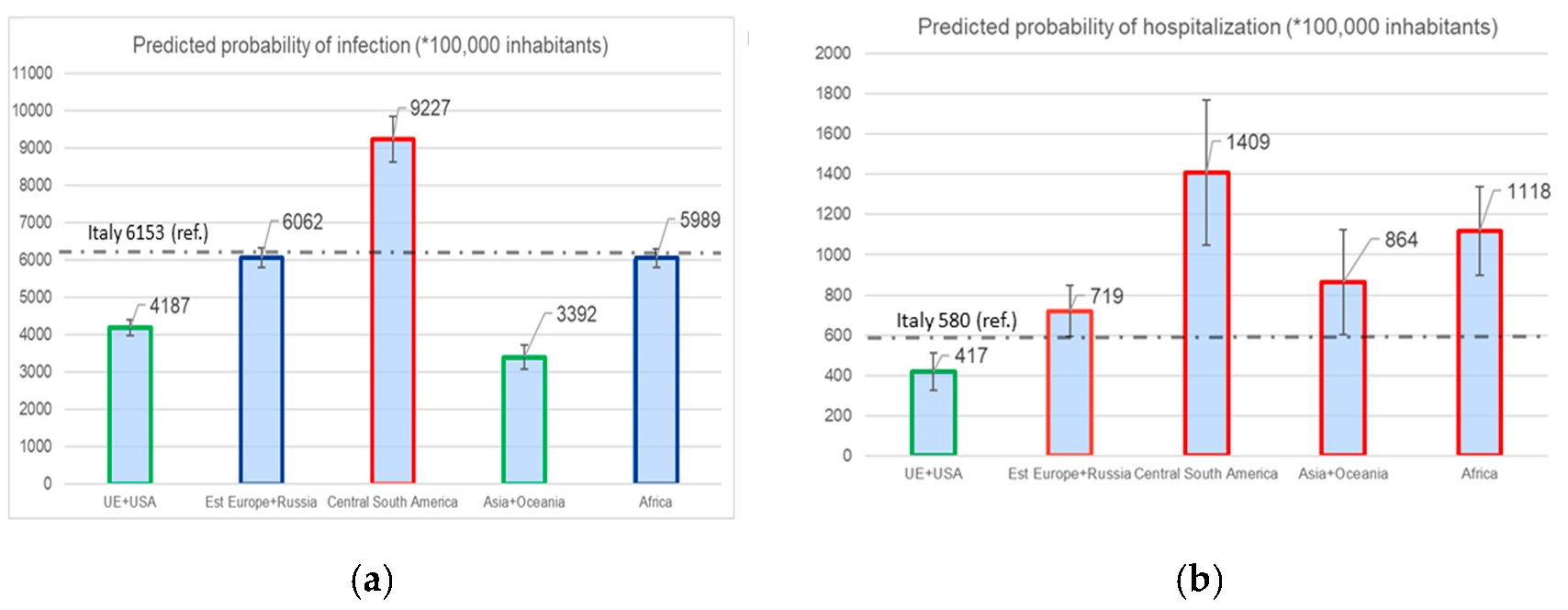
3.2. Association of Nationality and Socio-Economic Factors with SARS-CoV-2 Test Positivity
3.3. Association of Nationality and Socio-Economic Factors with COVID-19 Hospitalization
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 25 February 2023).
- Indseth, T.; Grøsland, M.; Arnesen, T.; Skyrud, K.; Kløvstad, H.; Lamprini, V.; Telle, K.; Kjøllesdal, M. COVID-19 among immigrants in Norway, notified infections, related hospitalizations and associated mortality: A register-based study. Scand. J. Public Health 2021, 49, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, T.; Caldwell, D.; Gomez-Aguinaga, B.; Doña-Reveco, C. Race, Ethnicity, Nativity and Perceptions of Health Risk during the COVID-19 Pandemic in the US. Int. J. Environ. Res. Public Health 2021, 18, 11113. [Google Scholar] [CrossRef]
- Mackey, K.; Ayers, C.K.; Kondo, K.K.; Saha, S.; Advani, S.M.; Young, S.; Spencer, H.; Rusek, M.; Anderson, J.; Veazie, S.; et al. Racial and ethnic disparities in covid-19-related infections, hospitalizations, and deaths a systematic review. Ann. Intern. Med. 2021, 174, 362–373. [Google Scholar] [CrossRef]
- Kelly, M. The relation between the social and the biological and COVID-19. Public Health 2021, 196, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Courtin, E.; Vineis, P. COVID-19 as a Syndemic. Front. Public Health 2021, 9, 763830. [Google Scholar] [CrossRef]
- Caron, R.M.; Adegboye, A.R.A. COVID-19: A Syndemic Requiring an Integrated Approach for Marginalized Populations. Front. Public Health 2021, 9, 675280. [Google Scholar] [CrossRef] [PubMed]
- Egede, L.E.; Walker, R.J.; Garacci, E. Racial/Ethnic Differences In COVID-19 Screening, Hospitalization, And Mortality In Southeast Wisconsin. Health Aff. 2020, 39, 1926–1934. [Google Scholar] [CrossRef] [PubMed]
- Gershengorn, H.B.; Patel, S.; Shukla, B.; Warde, P.R.; Bhatia, M.; Parekh, D.; Ferreira, T. Association of Race and Ethnicity with COVID-19 Test Positivity and Hospitalization Is Mediated by Socioeconomic Factors. Ann. Am. Thorac. Soc. 2021, 18, 1326–1334. [Google Scholar] [CrossRef] [PubMed]
- Galiatsatos, P.; Page, K.R.; Chatterjee, S.; Maygers, J.; Sarker, S.; Jones, V.; Lugo, A.; Tolson, T.; Hill-Briggs, F.; Chen, E.S.; et al. Comparing Critical Care Admissions among Urban Populations before and during the COVID-19 Pandemic. Health Secur. 2021, 19, S-34–S-40. [Google Scholar] [CrossRef]
- Mathur, R.; Rentsch, C.T.; Morton, C.E.; Hulme, W.J.; Schultze, A.; MacKenna, B.; Eggo, R.M.; Bhaskaran, K.; Wong, A.Y.S.; Williamson, E.J.; et al. Ethnic differences in SARS-CoV-2 infection and COVID-19-related hospitalisation, intensive care unit admission, and death in 17 million adults in England: An observational cohort study using the OpenSAFELY platform. Lancet 2021, 397, 1711–1724. [Google Scholar] [CrossRef]
- Pan, A.P.; Khan, O.; Meeks, J.R.; Boom, M.L.; Masud, F.N.; Andrieni, J.D.; Phillips, R.A.; Tiruneh, Y.M.; Kash, B.A.; Vahidy, F.S. Disparities in COVID-19 hospitalizations and mortality among black and Hispanic patients: Cross-sectional analysis from the greater Houston metropolitan area. BMC Public Health 2021, 21, 1330. [Google Scholar] [CrossRef] [PubMed]
- Podewils, L.J.; Burket, T.L.; Mettenbrink, C.; Steiner, A.; Seidel, A.; Scott, K.; Cervantes, L.; Hasnain-Wynia, R. Disproportionate Incidence of COVID-19 Infection, Hospitalizations, and Deaths among Persons Identifying as Hispanic or Latino—Denver, Colorado March–October 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 1812–1816. [Google Scholar] [CrossRef]
- Poulson, M.; Neufeld, M.; Geary, A.; Kenzik, K.; Sanchez, S.E.; Dechert, T.; Kimball, S. Intersectional Disparities Among Hispanic Groups in COVID-19 Outcomes. J. Immigr. Minor. Health 2020, 23, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Renelus, B.D.; Khoury, N.C.; Chandrasekaran, K.; Bekele, E.; Briggs, W.M.; Ivanov, A.; Mohanty, S.R.; Jamorabo, D.S. Racial Disparities in COVID-19 Hospitalization and In-hospital Mortality at the Height of the New York City Pandemic. J. Racial Ethn. Health Disparities 2020, 8, 1161–1167. [Google Scholar] [CrossRef] [PubMed]
- Rentsch, C.T.; Kidwai-Khan, F.; Tate, J.P.; Park, L.S.; King, J.T., Jr.; Skanderson, M.; Hauser, R.G.; Schultze, A.; Jarvis, C.I.; Holodniy, M.; et al. Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: A nationwide cohort study. PLOS Med. 2020, 17, e1003379. [Google Scholar] [CrossRef]
- Fabiani, M.; Mateo-Urdiales, A.; Andrianou, X.; Bella, A.; Del Manso, M.; Bellino, S.; Rota, M.C.; Boros, S.; Vescio, M.F.; D'Ancona, F.P.; et al. Epidemiological characteristics of COVID-19 cases in non-Italian nationals notified to the Italian surveillance system. Eur. J. Public Health 2021, 31, 37–44. [Google Scholar] [CrossRef]
- Rossi, P.G.; Marino, M.; Formisano, D.; Venturelli, F.; Vicentini, M.; Grilli, R.; The Reggio Emilia COVID-19 Working Group. Characteristics and outcomes of a cohort of COVID-19 patients in the Province of Reggio Emilia, Italy. PLoS ONE 2020, 15, e0238281. [Google Scholar] [CrossRef]
- Fabiani, M.; Vescio, M.F.; Bressi, M.; Mateo-Urdiales, A.; Petrone, D.; Spuri, M.; Sacco, C.; Del Manso, M.; Bella, A.; D’Ancona, F.; et al. Differences in the incidence and clinical outcomes of SARS-CoV-2 infection between Italian and non-Italian nationals using routine data. Public Health 2022, 211, 136–143. [Google Scholar] [CrossRef]
- Giacomelli, A.; Ridolfo, A.L.; Bonazzetti, C.; Oreni, L.; Conti, F.; Pezzati, L.; Siano, M.; Bassoli, C.; Casalini, G.; Schiuma, M.; et al. Mortality among Italians and immigrants with COVID-19 hospitalised in Milan, Italy: Data from the Luigi Sacco Hospital registry. BMC Infect. Dis. 2022, 22, 63. [Google Scholar] [CrossRef]
- Canevelli, M.; Palmieri, L.; Raparelli, V.; Punzo, O.; Donfrancesco, C.; Lo Noce, C.; Vanacore, N.; Brusaferro, S.; Onder, G.; Italian National Institute of Health COVID-19 Mortality Group. COVID-19 mortality among migrants living in Italy. Ann. Ist. Super. Sanita 2020, 56, 373–377. [Google Scholar]
- Drefahl, S.; Wallace, M.; Mussino, E.; Aradhya, S.; Kolk, M.; Brandén, M.; Malmberg, B.; Andersson, G. A population-based cohort study of socio-demographic risk factors for COVID-19 deaths in Sweden. Nat. Commun. 2020, 11, 5097. [Google Scholar] [CrossRef] [PubMed]
- Allan-Blitz, L.T.; Goldbeck, C.; Hertlein, F.; Turner, I.; Klausner, J.D. Association of lower socioeconomic status and sars-cov-2 positivity in los angeles, california. J. Prev. Med. Public Health 2021, 54, 161–165. [Google Scholar] [CrossRef]
- Amengual-Moreno, M.; Calafat-Caules, M.; Carot, A.; Rosa Correia, A.R.; Río-Bergé, C.; Rovira Plujà, J.; Valenzuela Pascual, C.; Ventura-Gabarró, C. Determinantes sociales de la incidencia de la COVID-19 en Barcelona: Un estudio ecológico preliminar usando datos públicos [Social determinants of the incidence of Covid-19 in Barcelona: A preliminary ecological study using public data.]. Rev. Esp. Salud Publica 2020, 94, e202009101. [Google Scholar] [PubMed]
- Lieberman-Cribbin, W.; Tuminello, S.; Flores, R.M.; Taioli, E. Disparities in COVID-19 Testing and Positivity in New York City. Am. J. Prev. Med. 2020, 59, 326–332. [Google Scholar] [CrossRef]
- Grigsby-Toussaint, D.S.; Shin, J.C.; Jones, A. Disparities in the distribution of COVID-19 testing sites in black and Latino areas in new York City. Prev. Med. 2021, 147, 106463. [Google Scholar] [CrossRef]
- Khanna, N.; Klyushnenkova, E.N.; Kaysin, A. Association of COVID-19 With Race and Socioeconomic Factors in Family Medicine. J. Am. Board Fam. Med. 2021, 34, S40–S47. [Google Scholar] [CrossRef]
- Priebe Rocha, L.; Rose, R.; Hoch, A.; Soares, C.; Fernandes, A.; Galvão, H.; Allen, J.D. The impact of the covid-19 pandemic on the brazilian immigrant community in the U.S: Results from a qualitative study. Int. J. Environ. Res. Public Health, 2021; 18, 3355. [Google Scholar]
- Stockman, J.K.; Wood, B.A.; Anderson, K.M. Racial and ethnic differences in COVID-19 outcomes, stressors, fear, and prevention behaviors among US women: Web-based cross-sectional study. J. Med. Internet Res. 2021, 23, e26296. [Google Scholar] [CrossRef]
- Cervantes, L.; Martin, M.; Frank, M.G.; Farfan, J.F.; Kearns, M.; Rubio, L.A. Experiences of Latinx Individuals Hospitalized for COVID-19: A Qualitative Study. JAMA Netw. Open 2021, 4, e210684. [Google Scholar] [CrossRef]
- Alsan, M.; Stantcheva, S.; Yang, D.; Cutler, D. Disparities in coronavirus 2019 reported incidence, knowledge, and behavior among us adults. JAMA Netw. Open 2020, 3, e2012403. [Google Scholar] [CrossRef]
- Velasco, F.; Yang, D.M.; Zhang, M.; Nelson, T.; Sheffield, T.; Keller, T.; Wang, Y.; Walker, C.; Katterapalli, C.; Zimmerman, K.; et al. Association of Healthcare Access With Intensive Care Unit Utilization and Mortality in Patients of Hispanic Ethnicity Hospitalized With COVID-19. J. Hosp. Med. 2021, 16, 659–666. [Google Scholar] [CrossRef]
- Kim, L.; Garg, S.; O’Halloran, A.; Whitaker, M.; Pham, H.; Anderson, E.J.; Armistead, I.; Bennett, N.M.; Billing, L.; Como-Sabetti, K.; et al. Risk Factors for Intensive Care Unit Admission and In-hospital Mortality among Hospitalized Adults Identified through the US Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET). Clin. Infect. Dis. 2021, 72, E206–E214. [Google Scholar] [CrossRef]
- Palaiodimos, L.; Kokkinidis, D.G.; Li, W.; Karamanis, D.; Ognibene, J.; Arora, S.; Southern, W.N.; Mantzoros, C.S. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism 2020, 108, 154262. [Google Scholar] [CrossRef]
- Dessie, Z.G.; Zewotir, T. Mortality-related risk factors of COVID-19: A systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect. Dis. 2021, 21, 855. [Google Scholar] [CrossRef] [PubMed]
- United Nation Development Program. Available online: https://hdr.undp.org/data-center/human-development-index#/indicies/HDI (accessed on 1 March 2023).
- Mazzalai, E.; Giannini, D.; Tosti, M.E.; D’angelo, F.; Declich, S.; Jaljaa, A.; Caminada, S.; Turatto, F.; De Marchi, C.; Gatta, A.; et al. Risk of Covid-19 Severe Outcomes and Mortality in Migrants and Ethnic Minorities Compared to the General Population in the European WHO Region: A Systematic Review. J. Int. Migr. Integr. 2023, 1–31. [Google Scholar] [CrossRef] [PubMed]
- WHO. Apart Together Survey. Prelımınary Overvıew of Refugees and Migrants Self-Reported İmpact of Covid-19. Available online: https://reliefweb.int/sites/reliefweb.int/files/resources/9789240017924-eng.pdf (accessed on 1 March 2023).
- Trick, W.E.; Badri, S.; Doshi, K.; Zhang, H.; Rezai, K.; Hoffman, M.J.; Weinstein, R.A. Epidemiology of COVID-19 vs. influenza: Differential failure of COVID-19 mitigation among Hispanics, Cook County Health, Illinois. PLoS ONE 2021, 16, e0240202. [Google Scholar] [CrossRef]
- Cuadros, D.F.; Branscum, A.J.; Mukandavire, Z.; Miller, F.D.; MacKinnon, N. Dynamics of the COVID-19 epidemic in urban and rural areas in the United States. Ann. Epidemiol. 2021, 59, 16–20. [Google Scholar] [CrossRef]
- Mateo-Urdiales, A.; Fabiani, M.; Rosano, A.; Vescio, M.F.; Del Manso, M.; Bella, A.; Riccardo, F.; Pezzotti, P.; Regidor, E.; Andrianou, X. Socioeconomic patterns and COVID-19 outcomes before, during and after the lockdown in Italy (2020). Health Place 2021, 71, 102642. [Google Scholar] [CrossRef] [PubMed]
- Meurisse, M.; Lajot, A.; Devleesschauwer, B.; Van Cauteren, D.; Van Oyen, H.; Borre, L.V.D.; Brondeel, R. The association between area deprivation and COVID-19 incidence: A municipality-level spatio-temporal study in Belgium, 2020–2021. Arch. Public Health 2022, 80, 109. [Google Scholar] [CrossRef]
- Azar, K.M.; Shen, Z.; Romanelli, R.J.; Lockhart, S.H.; Smits, K.; Robinson, S.; Brown, S.; Pressman, A.R. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff. 2020, 39, 1253–1262. [Google Scholar] [CrossRef]
- Patel, A.P.; Paranjpe, M.D.; Kathiresan, N.P.; Rivas, M.A.; Khera, A.V. Race, socioeconomic deprivation, and hospitalization for COVID-19 in English participants of a national biobank. Int. J. Equity Health 2020, 19, 114. [Google Scholar] [CrossRef]
- Lassale, C.; Gaye, B.; Hamer, M.; Gale, C.R.; Batty, G.D. Ethnic disparities in hospitalisation for COVID-19 in England: The role of socioeconomic factors, mental health, and inflammatory and pro-inflammatory factors in a community-based cohort study. Brain Behav Immun. 2020, 88, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Vandentorren, S.; Smaïli, S.; Chatignoux, E.; Maurel, M.; Alleaume, C.; Neufcourt, L.; Kelly-Irving, M.; Delpierre, C. The effect of social deprivation on the dynamic of SARS-CoV-2 infection in France: A population-based analysis. Lancet Public Health 2022, 7, e240–e249. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.J.; Tang, K.; Zhao, F.J.; Yu, B.Y.; Liu, T.T.; Zhang, L.L. Impact of Social Deprivation on Hospitalization and Intensive Care Unit Admission among COVID-19 Patients: A Systematic Review and Meta-Analysis. Iran. J. Public Health 2022, 51, 2458–2471. [Google Scholar] [CrossRef]
- Kragholm, K.; Andersen, M.P.; Gerds, T.A.; Butt, J.H.; Østergaard, L.; Polcwiartek, C.; Phelps, M.; Andersson, C.; Gislason, G.H.; Torp-Pedersen, C. Association between Male Sex and Outcomes of Coronavirus Disease 2019 (COVID-19)-A Danish Nationwide, Register-based Study. Clin. Infect. Dis. 2021, 73, E4025–E4030. [Google Scholar] [CrossRef]
- Peckham, H.; De Gruijter, N.M.; Raine, C.; Radziszewska, A.; Ciurtin, C.; Wedderburn, L.R.; Rosser, E.C.; Webb, K.; Deakin, C.T. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat. Commun. 2020, 11, 6317. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, I.; Hou, X. Immigrants and the utilization of hospital emergency departments. World J. Emerg. Med. 2012, 3, 245. [Google Scholar] [CrossRef] [Green Version]
- Bannaga, A.S.; Tabuso, M.; Farrugia, A.; Chandrapalan, S.; Somal, K.; Lim, V.K.; Mohamed, S.; Nia, G.J.; Mannath, J.; Wong, J.L.; et al. C-reactive protein and albumin association with mortality of hospitalised SARS-CoV-2 patients: A tertiary hospital experience. Clin. Med. 2020, 20, 463–468. [Google Scholar] [CrossRef]
- Rao, G.G.; Allen, A.; Papineni, P.; Wang, L.; Anderson, C.; McGregor, A.; Whittington, A.; John, L.; Harris, M.; Hiles, S.; et al. sectional observational study of epidemiology of COVID-19 and clinical outcomes of hospitalised patients in North West London during March and April 2020. BMJ Open 2021, 11, e044384. [Google Scholar]
- Papageorgiou, N.; Providencia, R.; Saberwal, B.; Sohrabi, C.; Tyrlis, A.; Atieh, A.E.; Lim, W.-Y.; Creta, A.; Khanji, M.; Rusinova, R.; et al. Ethnicity and COVID-19 cardiovascular complications: A multi-center UK cohort. Am. J. Cardiovasc. Dis. 2020, 10, 455–462. [Google Scholar]
- Di Napoli, A.; Rossi, A.; Alicandro, G.; Ventura, M.; Frova, L.; Petrelli, A. Salmon bias effect as hypothesis of the lower mortality rates among immigrants in Italy. Sci. Rep. 2021, 11, 8033. [Google Scholar] [CrossRef]
| Variables | General Population | COVID-19 Cases | Hospitalization | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Italian | Non-Italian | Total | Italian | Non-Italian | Total | p-Value | Italian | Non-Italian | Total | p-Value | |
| N (Column%) | N (Column%) | N (Column%) | N (Column%) | N (Column%) | N (Column%) | N (Column%) | N (Column%) | N (Column%) | |||
| Sex | |||||||||||
| Male | 381,131 (47.4) | 42,402 (41.6) | 423,533 (46.7) | 23,843 (49.2) | 2572 (43.3) | 26,415 (48.5) | <0.001 | 2755 (56.3) | 183 (45.6) | 2938 (55.5) | <0.001 |
| Females | 423,296 (52.6) | 59,634 (58.4) | 482,930 (53.3) | 24,663 (50.8) | 3370 (56.7) | 28,033 (51.5) | 2139 (43.7) | 218 (54.4) | 2357 (44.5) | ||
| Age (years) | |||||||||||
| <50 | 384,645 (47.8) | 74,308 (72.8) | 458,953 (50.6) | 26,687 (55.1) | 4597 (77.4) | 31,284 (57.4) | <0.001 | 566 (11.6) | 192 (47.9) | 758 (14.3) | <0.001 |
| 50–59 | 124,723 (15.5) | 15,320 (15) | 140,043 (15.4) | 8111 (16.7) | 817 (13.7) | 8928 (16.4) | 648 (13.2) | 96 (23.9) | 744 (14) | ||
| 60–69 | 107,223 (13.3) | 8433 (8.3) | 115,656 (12.8) | 5548 (11.4) | 379 (6.4) | 5927 (10.9) | 932 (19) | 62 (15.5) | 994 (18.8) | ||
| 70+ | 187,836 (23.4) | 3975 (3.9) | 191,811 (21.2) | 8160 (16.8) | 149 (2.5) | 8309 (15.3) | 2748 (56.2) | 51 (12.7) | 2799 (52.9) | ||
| Geographical areas | |||||||||||
| Italy | 804,427 (100) | - | 804,427 (88.7) | 48,506 (100) | - | 48,506 (89.1) | <0.05 | 4894 (100) | - | 4894 (92.4) | <0.05 |
| EU and North America | - | 31,905 (31.3) | 31,905 (3.5) | - | 1389 (23.4) | 1389 (2.6) | - | 78 (19.5) | 78 (1.5) | ||
| Central–Eastern Europe | - | 29,780 (29.2) | 29,780 (3.3) | - | 1919 (32.3) | 1919 (3.5) | - | 122 (30.4) | 122 (2.3) | ||
| Central–South America | - | 8001 (7.8) | 8001 (0.9) | - | 811 (13.6) | 811 (1.5) | - | 57 (14.2) | 57 (1.1) | ||
| Asia and Oceania | - | 10,904 (10.7) | 10,904 (1.2) | - | 408 (6.9) | 408 (0.7) | - | 43 (10.7) | 43 (0.8) | ||
| Africa | - | 21,446 (21) | 21,446 (2.4) | - | 1415 (23.8) | 1415 (2.6) | - | 101 (25.2) | 101 (1.9) | ||
| HDI | |||||||||||
| Very high | - | 5309 (5.2) | 5309 (0.6) | - | 138 (2.3) | 138 (0.3) | <0.001 | - | 14 (3.5) | 14 (0.3) | <0.001 |
| Italy | 804,427 (100) | - | 804,427 (88.8) | 48,506 (100) | - | 48,506 (89.1) | 4894 (100) | - | 4894 (92.4) | ||
| High | - | 73,898 (72.4) | 73,898 (8.1) | - | 4310 (72.6) | 4310 (7.9) | - | 281 (70.1) | 281 (5.3) | ||
| Medium | - | 16,561 (16.2) | 16,561 (1.8) | - | 1113 (18.7) | 1113 (2) | - | 70 (17.4) | 70 (1.3) | ||
| Low | - | 6252 (6.2) | 6252 (0.7) | - | 380 (6.4) | 380 (0.7) | - | 36 (9) | 36 (0.7) | ||
| Missing | - | 16 (0.0) | 16 (0.0) | - | 1 (0.0) | 1 (0.0) | - | - | - | ||
| Deprivation Index | |||||||||||
| Quintile 1 | 163,933 (2.4) | 15,995 (15.7) | 179,928 (19.8) | 9039 (18.6) | 789 (13.3) | 9828 (18.1) | <0.001 | 891 (18.2) | 54 (13.5) | 945 (17.8) | <0.001 |
| Quintile 2 | 157,314 (19.6) | 16,368 (16) | 173,682 (19.2) | 8829 (18.2) | 748 (12.6) | 9577 (17.6) | 865 (17.7) | 41 (10.2) | 906 (17.1) | ||
| Quintile 3 | 177,664 (22.1) | 22,205 (21.8) | 199,869 (22.1) | 11,629 (24) | 1385 (23.3) | 13,014 (23.9) | 1206 (24.6) | 97 (24.2) | 1303 (24.6) | ||
| Quintile 4 | 46,539 (18.2) | 23,233 (22.8) | 169,772 (18.7) | 9204 (19) | 1856 (31.2) | 11,060 (20.3) | 934 (19.1) | 129 (32.2) | 1063 (20.1) | ||
| Quintile 5 | 151,600 (18.8) | 21,336 (20.9) | 172,936 (19.1) | 9750 (20.1) | 1140 (19.2) | 10,890 (20) | 992 (20.3) | 77 (19.2) | 1069 (20.2) | ||
| Missing | 7377 (0.9) | 2899 (2.8) | 10,276 (1.1) | 55 (0.1) | 24 (0.4) | 79 (0.1) | 6 (0.1) | 3 (0.7) | 9 (0.2) | ||
| Urban–Rural Index | |||||||||||
| A-pole | 366,608 (45.6) | 51,798 (50.8) | 418,406 (46.2) | 23,148 (47.7) | 24 (0.4) | 23,172 (42.6) | <0.001 | 2386 (48.8) | 242 (60.4) | 2628 (49.6) | <0.001 |
| A1-urban | 39,676 (4.9) | 4619 (4.6) | 44,295 (4.9) | 3009 (6.2) | 3459 (58.2) | 6468 (11.9) | 274 (5.6) | 27 (6.7) | 301 (5.7) | ||
| A2-rural | 125,119 (15.6) | 13,687 (13.4) | 138,806 (15.3) | 7977 (16.5) | 350 (5.9) | 8327 (15.3) | 776 (15.8) | 47 (11.7) | 823 (15.5) | ||
| B2-rural | 157,942 (19.6) | 19,115 (18.7) | 177,057 (19.5) | 8778 (18.1) | 806 (13.6) | 9584 (17.6) | 881 (18) | 52 (13) | 933 (17.6) | ||
| C2-rural | 107,705 (13.4) | 9918 (9.7) | 117,623 (13) | 5539 (11.4) | 893 (15) | 6432 (11.8) | 571 (11.7) | 30 (7.5) | 601 (11.4) | ||
| Missing | 7377 (0.9) | 2899 (2.8) | 10,276 (1.1) | 55 (0.1) | 410 (6.9) | 465 (0.8) | 6 (0.1) | 3 (0.7) | 9 (0.2) | ||
| Total | 804,427 (100) | 102,036 (100) | 906,463 (100) | 48,506 (100) | 5942 (100) | 54,448 (100) | 4894 (100) | 401 (100) | 5295 (100) | ||
| Variables | Covid-19 Cases | Hospitalization | ||||
|---|---|---|---|---|---|---|
| Model I1 Univariate | Model I2 HDI | Model I3 Area | Model H1 Univariate | Model H2 HDI | Model H3 Area | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Sex | ||||||
| Male | 1.08 *** | 1.05 *** | 1.05 *** | 1.43 *** | 1.58 *** | 1.58 *** |
| (1.06–1.10) | (1.03–1.07) | (1.04–1.07) | (1.35–1.51) | (1.50–1.67) | (1.50–1.67) | |
| Females | ref. | ref. | ref. | ref. | ref. | ref. |
| Age (years) | ||||||
| <50 | ref. | ref. | ref. | ref. | ref. | ref. |
| 50–59 | 0.93 *** | 0.93 *** | 0.93 *** | 3.25 *** | 3.40 *** | 3.39 *** |
| (0.91–0.95) | (0.91–0.95) | (0.91–0.95) | 2.93–3.59 | (3.07–3.77) | (3.06–3.76) | |
| 60–69 | 0.74 *** | 0.74 *** | 0.74 *** | 5.30 *** | 5.69 *** | 5.66 *** |
| (0.72–0.76) | (0.72–0.76) | (0.72–0.76) | (4.82–5.82) | (5.16–6.26) | (5.14–6.23) | |
| 70+ | 0.62 *** | 0.62 *** | 0.61 *** | 9.06 *** | 9.98 *** | 9.90 *** |
| (0.61–0.64) | (0.60–0.63) | (0.60–0.63) | (8.35–9.82) | (9.18–10.86) | (9.11–10.76) | |
| Nationality | ||||||
| Italian | ref. | ref. | ||||
| Non-Italian | 0.97 ** | 0.64 *** | ||||
| (0.94–0.99) | (0.58–0.71) | |||||
| Geographical areas | ||||||
| Italy | ref. | ref. | ref. | ref. | ||
| EU and North America | 0.73 *** | 0.68 *** | 0.41 *** | 0.73 *** | ||
| (0.69–0.78) | (0.64–0.72) | (0.33–0.51) | (0.58–0.91) | |||
| Central–Eastern Europe | 1.07 *** | 1.39 | 0.67 *** | 1.23 ** | ||
| (1.02–1.13) | (0.94–1.03) | (0.56–0.80) | (1.03–1.48) | |||
| Central–South America | 1.70 *** | 1.54 *** | 1.14 | 2.44 *** | ||
| (1.58–1.83) | (1.43–1.65) | (0.88–1.48) | (1.87–3.18) | |||
| Asia and Oceania | 0.62 *** | 0.55 *** | 0.63 *** | 1.53 *** | ||
| (0.56–0.68) | (0.50–0.61) | (0.46–0.86) | (1.12–2.09) | |||
| Africa | 1.08 *** | 0.96 | 0.76 *** | 1.91 *** | ||
| (1.02–1.14) | (0.91–1.01) | (0.62–0.92) | (1.56–2.34) | |||
| Urban–Rural Index | ||||||
| A-pole | 1.67 *** | 1.45 ** | 1.45 ** | 1.33 ** | 1.33 | 1.32 |
| (1.29–2.16) | (1.08–1.94) | (1.09–1.93) | (1.05–1.68) | (0.98–1.79) | (0.98–1.79) | |
| A2-rural | 1.53 *** | 1.44 *** | 1.45 *** | 1.18 | 1.25 ** | 1.25 ** |
| (1.28–1.84) | (1.21–1.72) | (1.21–1.72) | (0.97–1.43) | (1.01–1.53) | (1.01–1.53) | |
| B2-rural | 1.21 ** | 1.15 | 1.15 | 0.98 | 0.99 | 0.99 |
| (1.03–1.43) | (0.98–1.35) | (0.98–1.35) | (0.82–1.19) | (0.81–1.21) | (0.81–1.21) | |
| C2-rural | ref. | ref. | ref. | ref | ref. | ref. |
| Deprivation Index | ||||||
| Quintile 1 | ref. | ref. | ref. | ref. | ref. | ref. |
| Quintile 2 | 1.14 | 1.11 | 1.11 | 1.11 | 1.17 | 1.17 |
| (0.96–1.36) | (0.95–1.30) | (0.95–1.30) | (0.92–1.34) | (0.97–1.42) | (0.97–1.42) | |
| Quintile 3 | 1.35 *** | 1.18 | 1.18 | 1.22 | 1.19 | 1.20 |
| (1.09–1.67) | (0.97–1.44) | (0.97–1.45) | (0.99–1.49) | (0.95–1.50) | (0.96–1.50) | |
| Quintile 4 | 1.48 | 1.14 | 1.14 | 1.34 | 1.19 | 1.19 |
| (0.76–2.87) | (0.60–2.17) | (0.60–2.15) | (0.80–2.24) | (0.65–2.18) | (0.65–2.16) | |
| Quintile 5 | 1.40 *** | 1.27 ** | 1.27 ** | 1.34 ** | 1.37 ** | 1.38 *** |
| (1.11–1.78) | (1.02–1.59) | (1.02–1.59) | (1.07–1.69) | (1.07–1.77) | (1.07–1.78) | |
| HDI | ||||||
| very high | 0.44 *** | 0.45 *** | 0.46 *** | 0.47 *** | ||
| (0.37–0.53) | (0.38–0.53) | (0.27–0.79) | (0.28–0.79) | |||
| Italy | ref. | ref. | ref. | ref. | ||
| high | 1.37 | 0.88 *** | 0.62 *** | 1.25 *** | ||
| (0.94–1.00) | (0.85–0.91) | (0.55–0.70) | (1.10–1.41) | |||
| medium | 1.11 *** | 0.99 | 0.68 *** | 1.65 *** | ||
| (1.04–1.18) | (0.93–1.05) | (0.53–0.86) | (1.30–2.10) | |||
| low | 1.20 | 0.89 ** | 0.94 | 3.05 *** | ||
| (0.92–1.13) | (0.80–0.89) | (0.67–1.31) | (2.17–4.28) | |||
| σ2u | 0.086 | 0.085 | 0.07 | 0.07 | ||
| Variables | Hospitalization within 48 Hours from the Diagnosis | |
|---|---|---|
| Model H4 | Model H5 | |
| OR (95% CI) | OR (95% CI) | |
| Age (years) | ||
| <50 | ref. | ref. |
| 50–59 | 0.94 | 0.94 |
| (0.76–1.17) | (0.76–1.16) | |
| 60–69 | 1.36 | 0.96 |
| (0.78–1.17) | (0.78–1.17) | |
| 70+ | 1.8 *** | 1.80 *** |
| (1.51–2.14) | (1.51–2.14) | |
| Geographical areas | ||
| Italy | ref. | |
| EU (North America) | 2.12 *** | |
| (1.34–3.45) | ||
| Central–Eastern Europe | 1.89 *** | |
| (1.31–2.72) | ||
| Central–South America | 1.93 ** | |
| (1.14–3.28) | ||
| Asia and Oceania | 4.5 *** | |
| (2.28–8.87) | ||
| Africa | 4.58 *** | |
| (2.94–7.12) | ||
| HDI | ||
| very high | 1.8 | |
| (0.61–5.25) | ||
| Italy | ref. | |
| high | 2.05 *** | |
| (1.6–2.64) | ||
| medium | 4.52 *** | |
| (2.67–7.66) | ||
| low | 10.9 *** | |
| (4.19–28.28) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gili, A.; Caminiti, M.; Lupi, C.; Zichichi, S.; Minicucci, I.; Pezzotti, P.; Primieri, C.; Bietta, C.; Stracci, F. Socio-Economic Factors Associated with Ethnic Disparities in SARS-CoV-2 Infection and Hospitalization. Int. J. Environ. Res. Public Health 2023, 20, 6521. https://doi.org/10.3390/ijerph20156521
Gili A, Caminiti M, Lupi C, Zichichi S, Minicucci I, Pezzotti P, Primieri C, Bietta C, Stracci F. Socio-Economic Factors Associated with Ethnic Disparities in SARS-CoV-2 Infection and Hospitalization. International Journal of Environmental Research and Public Health. 2023; 20(15):6521. https://doi.org/10.3390/ijerph20156521
Chicago/Turabian StyleGili, Alessio, Marta Caminiti, Chiara Lupi, Salvatore Zichichi, Ilaria Minicucci, Patrizio Pezzotti, Chiara Primieri, Carla Bietta, and Fabrizio Stracci. 2023. "Socio-Economic Factors Associated with Ethnic Disparities in SARS-CoV-2 Infection and Hospitalization" International Journal of Environmental Research and Public Health 20, no. 15: 6521. https://doi.org/10.3390/ijerph20156521







