Unveiling Spatial Associations between COVID-19 Severe Health Index, Racial/Ethnic Composition, and Community Factors in the United States
Abstract
:1. Introduction
2. Materials and Methods
2.1. Dependent Variable
2.2. Independent Variable
2.3. Covariates
2.4. Data Analysis
| Variable Name | Variable Description | Analytical Role | Variable Type | Source |
|---|---|---|---|---|
| COVID-19 SHRI | Severe COVID-19 health risk index in 2020 | Dependent Variable | Continuous | [16] |
| Majority Racial/Ethnic Group | County’s predominant racial or ethnic group | Predictor | Categorical 1 = Majority Non-Hispanic White 2 = Majority Non-Hispanic Black 3 = Majority Hispanic 4 = Majority Non-Hispanic Other | Calculated from census row data. American Community Surveys 5-year estimates (ACS) 2020 [37] |
| Men/Women Ratio | Estimated ratio of men to women (number of males per hundred females), between 2015 and 2019 by county in United States | Covariate | Continuous | American Community Surveys 5-year estimates (ACS) 2020 [37] |
| Rural | % Rural: census population estimates | Covariate | Continuous | County health ranking [38] |
| Completed High School | Estimated percent of people with at least a high school diploma, between 2015 and 2019 by County in United States | Covariate | Continuous | American Community Surveys 5 years estimates (ACS) 2020 [37] |
| Age | Estimated median age of all people, between 2015 and 2019 by county in United States | Covariate | Continuous | American Community Surveys 5 years estimates (ACS) 2020 [37] |
| Smoking | Estimated percent of adults reporting to have ever smoked cigarettes in 2018 by county in United States | Covariate | Continuous | PolicyMap [44] 2017 and 2018 CDC Behavioral Risk Factor Surveillance System |
| Insufficient Sleep | Percentage of adults who reported fewer than 7 h of sleep on average (age-adjusted) | Covariate | Continuous | County Health Ranking [38] |
| ICU Beds | Number of Intensive Care Unit (ICU) beds in 2019 by county in United States | Covariate | Continuous | PolicyMap [44] Kaiser Health News |
| Primary Care Physicians (PCP) | Number of primary care doctors per 10,000 residents | Covariate | Continuous | Health Resources & Services Administration. Area health resource files [50] |
| Uninsured Population | Estimated percent of all people without health insurance, between 2015 and 2019 by county in United States | Covariate | Continuous | American Community Surveys 5-year estimates (ACS) 2020 [37] |
| Preventable Hospitalization | Rate of hospital stays for ambulatory-care-sensitive conditions per 100,000 Medicare enrollees | Covariate | Continuous | County health ranking [38] |
| HH with Internet Access | Estimated percent of households with internet access, between 2015 and 2019 by county in United States | Covariate | Continuous | American Community Surveys 5-year estimates (ACS) 2020 [37] |
| Food Insecurity | Estimated food insecurity rate in 2017 by county in United States | Covariate | Continuous | PolicyMap [44] Feeding America |
| PM2.5 | Levels of PM2.5 per county | Covariate | Continuous | EPA [51] |
3. Results
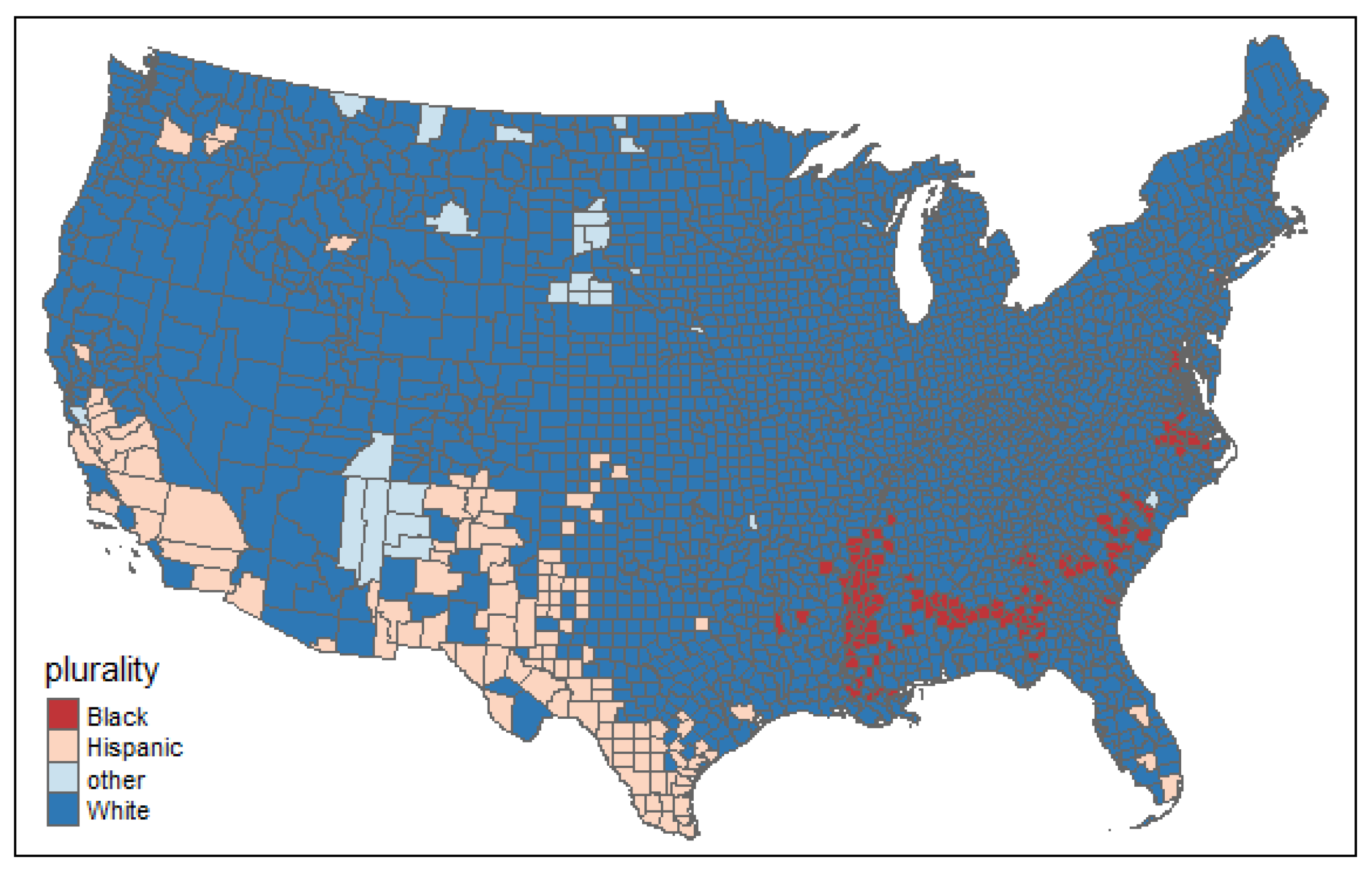
3.1. Descriptive Analysis
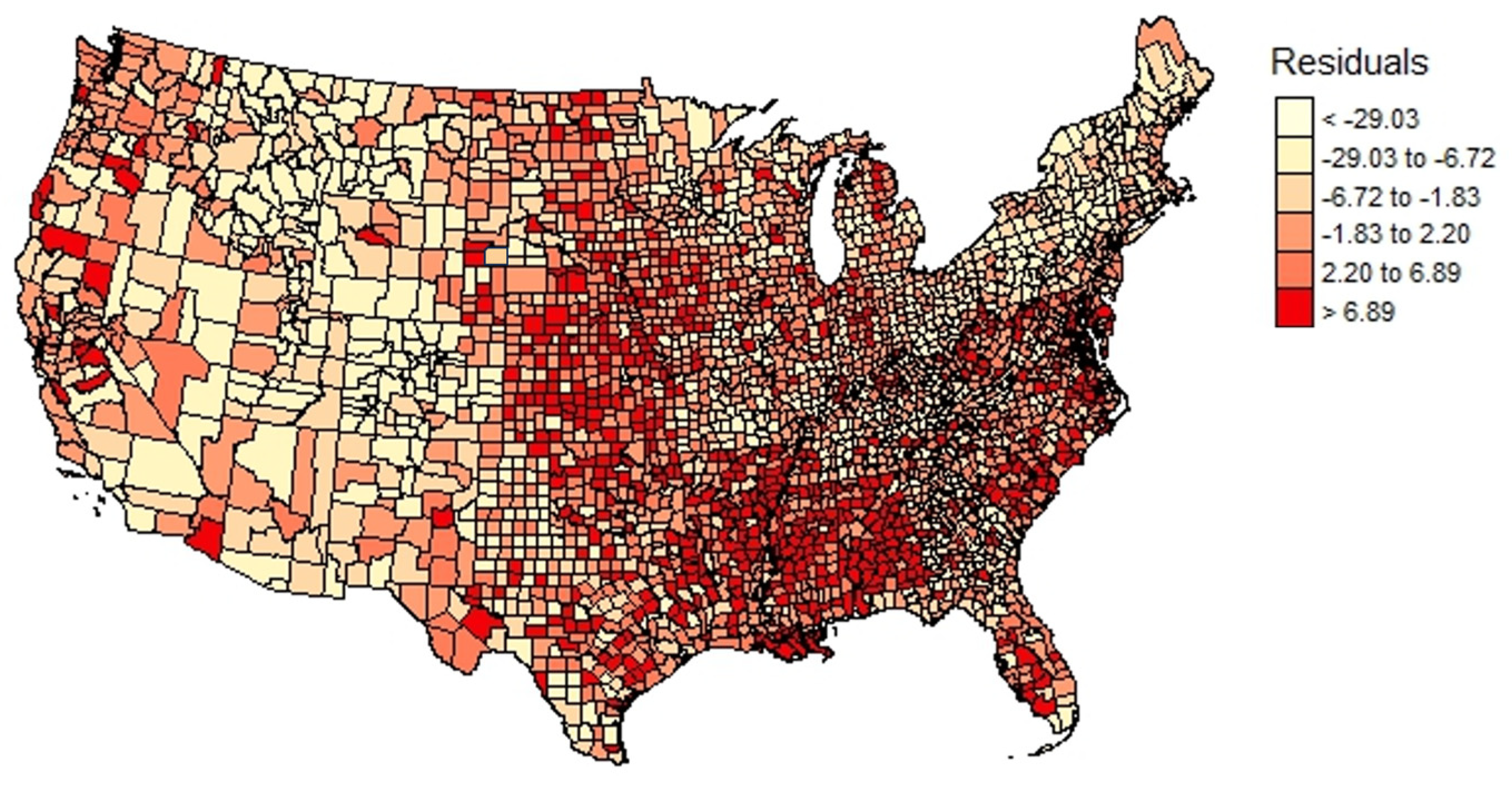
3.2. Regression Analyses Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Model 1 | Model 2 | Model 3 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | β | 95% CI | VIF | β | 95% CI | VIF | β | 95% CI | VIF | |||
| Lower | Upper | Lower | Upper | Lower | Upper | |||||||
| Major Racial/Ethnic Group (Ref = Majority Black | 1.72 | 2.21 | 3.14 | |||||||||
| Majority Hispanic | −9.80 *** | −2.18 | −17.41 | −7.82 *** | −9.97 | −5.68 | −6.45 *** | −8.82 | −4.07 | |||
| Majority Other | −6.82 *** | −10.81 | −2.84 | −7.40 *** | −11.29 | −3.50 | −5.85 ** | −9.74 | −1.97 | |||
| Majority White | −6.41 *** | −8.12 | −4.69 | −5.78 *** | −7.27 | −4.29 | −4.53 *** | −6.14 | −2.92 | |||
| Rural | 0.05 *** | 0.03 | 0.06 | 1.62 | 0.04 *** | 0.02 | 0.05 | 2.45 | 0.03 *** | 0.02 | 0.05 | 2.42 |
| Log Household Income | −22.56 ** | −24.40 | −20.71 | 1.58 | −7.91 *** | −9.83 | −6.00 | 2.01 | −4.71 *** | −7.16 | −2.26 | 3.58 |
| Age | 0.44 *** | 0.36 | 0.51 | 1.48 | 0.50 *** | 0.43 | 0.56 | 2.20 | 0.52 *** | 0.45 | 0.59 | 2.20 |
| Completed High School | −0.65 | −0.72 | −0.58 | 1.77 | −0.11 * | −0.19 | −0.03 | 2.92 | −0.04 | −0.12 | 0.04 | 3.17 |
| Men to Women Ratio | −0.18 *** | −0.21 | −0.15 | 1.07 | −0.16 *** | −0.19 | −0.13 | 1.11 | −0.15 *** | −0.18 | −0.12 | 1.12 |
| Smokers | 0.89 *** | 0.75 | 1.03 | 4.74 | 0.82 *** | 0.68 | 0.97 | 4.80 | ||||
| Insufficient Sleep | 0.79 *** | 0.67 | 0.90 | 3.30 | 0.78 *** | 0.67 | 0.90 | 3.36 | ||||
| Log ICU Beds | −0.01 *** | −0.01 | −0.01 | 1.28 | −0.01 *** | −0.02 | −0.01 | 1.32 | ||||
| Uninsured | 0.03 | −0.04 | 0.10 | 1.70 | 0.01 | −0.06 | 0.08 | 1.76 | ||||
| PCP | −0.03 *** | −0.04 | −0.02 | 1.38 | −0.02 *** | −0.03 | −0.02 | 1.41 | ||||
| Log Preventable Hospitalization | 4.50 *** | 3.67 | 5.34 | 1.48 | 4.17 *** | 3.35 | 4.99 | 1.49 | ||||
| PM2.5 | 0.75 *** | 0.56 | 0.94 | 1.31 | ||||||||
| Broadband | −0.13 *** | −0.19 | −0.07 | 2.96 | ||||||||
| Food Insecurity | 0.16 ** | 0.03 | 0.28 | 3.30 | ||||||||
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristics | β | 95% CI | β | 95% CI | β | 95% CI | |||
| Lower | Upper | Lower | Upper | Lower | Upper | ||||
| Major Racial/Ethnic Group (Ref = Majority Black | |||||||||
| Majority Hispanic | −9.69 *** | −11.59 | −7.78 | −5.17 *** | −7.07 | −3.28 | −4.76 *** | −6.86 | −2.66 |
| Majority Other | 2.68 | −0.46 | 5.83 | −0.36 | −3.81 | 3.09 | −0.13 | −3.59 | 3.33 |
| Majority White | −4.96 *** | −6.32 | −3.61 | −5.15 *** | −6.46 | −3.84 | −4.62 *** | −6.04 | −3.19 |
| Rural | 0.04 *** | 0.02 | 0.05 | 0.02 *** | 0.01 | 0.03 | 0.02 *** | 0.01 | 0.03 |
| Log Household income | −9.68 *** | −11.28 | −8.07 | −3.52 *** | −5.23 | −1.81 | −2.57 ** | −4.74 | −0.41 |
| Age | 0.52 *** | 0.46 | 0.58 | 0.55 *** | 0.49 | 0.61 | 0.56 *** | 0.50 | 0.62 |
| Completed High School | −0.41 *** | −0.47 | −0.35 | −0.13 *** | −0.20 | −0.06 | −0.07 | −0.14 | 0.00 |
| Men to Women Ratio | −0.11 *** | −0.13 | −0.08 | −0.12 *** | −0.14 | −0.09 | −0.11 *** | −0.14 | −0.09 |
| Smokers | 0.58 *** | 0.45 | 0.71 | 0.56 *** | 0.43 | 0.69 | |||
| Insufficient Sleep | 0.46 *** | 0.35 | 0.56 | 0.46 *** | 0.35 | 0.56 | |||
| Log ICU Beds | −0.01 *** | −0.01 | 0.00 | −0.01 *** | −0.01 | −0.01 | |||
| Uninsured | 0.05 | −0.01 | 0.11 | 0.05 | −0.02 | 0.12 | |||
| PCP | −0.03 *** | −0.04 | −0.02 | −0.03 *** | −0.04 | −0.02 | |||
| Log Preventable Hospitalization | 2.94 *** | 2.20 | 3.68 | 2.78 *** | 2.04 | 3.51 | |||
| PM2.5 | 0.46 *** | 0.29 | 0.63 | ||||||
| Broadband | −0.09 *** | −0.15 | −0.04 | ||||||
| Food Insecurity | 0.03 | −0.08 | 0.14 | ||||||
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristics | B | 95% CI | B | 95% CI | B | 95% CI | |||
| Lower | Upper | Lower | Upper | Lower | Upper | ||||
| Major Racial/Ethnic Group (Ref = Majority Black | |||||||||
| Majority Hispanic | −5.53 *** | −7.83 | −3.23 | −2.59 ** | −4.77 | −0.41 | −3.08 ** | −5.43 | −0.73 |
| Majority Other | 7.55 *** | 4.16 | 10.95 | −1.69 | −5.27 | 1.89 | −1.92 | −5.51 | 1.66 |
| Majority White | −4.42 *** | −5.96 | −2.87 | −3.53 *** | −4.98 | −2.09 | −3.65 *** | −5.18 | −2.11 |
| Rural | 0.04 *** | 0.02 | 0.05 | 0.01 | 0.00 | 0.03 | 0.01 | 0.00 | 0.02 |
| Log Household Income | −15.53 *** | −17.41 | −13.65 | −3.20 ** | −5.25 | −1.14 | −3.49 ** | −5.93 | −1.06 |
| Age | 0.70 *** | 0.64 | 0.77 | 0.72 *** | 0.66 | 0.79 | 0.71 *** | 0.65 | 0.78 |
| Completed High School | −0.34 *** | −0.42 | −0.27 | −0.09 | −0.17 | −0.01 | −0.04 | −0.13 | 0.04 |
| Men to Women Ratio | −0.07 *** | −0.10 | −0.05 | −0.11 *** | −0.13 | −0.08 | −0.10 *** | −0.13 | −0.08 |
| Smokers | −7.83 | −3.23 | 0.98 *** | 0.82 | 1.15 | 0.96 *** | 0.80 | 1.13 | |
| Insufficient Sleep | 0.83 *** | 0.69 | 0.98 | 0.83 *** | 0.68 | 0.97 | |||
| Log ICU Beds | −0.01 *** | −0.01 | −0.01 | −0.01 *** | −0.01 | −0.01 | |||
| Uninsured | 0.05 | −0.04 | 0.13 | 0.05 | −0.03 | 0.14 | |||
| PCP | −0.02 *** | −0.02 | −0.01 | −0.01 *** | −0.02 | −0.01 | |||
| Log Preventable Hospitalization | 2.76 *** | 1.95 | 3.58 | 2.66 *** | 1.85 | 3.48 | |||
| PM2.5 | 0.53 *** | 0.28 | 0.78 | ||||||
| Broadband | −0.07 ** | −0.13 | −0.02 | ||||||
| Food Insecurity | −0.07 | −0.21 | 0.08 | ||||||
References
- Noonan, A.S.; Velasco-Mondragon, H.E.; Wagner, F.A. Improving the health of African Americans in the USA: An overdue opportunity for social justice. Public Health Rev. 2016, 37, 12. [Google Scholar] [CrossRef] [PubMed]
- Centers for Medicare & Medicaid Services. State by State Enrollment in the Pre-Existing Condition Insurance Plan. 2020. Available online: https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/pcip-enrollment (accessed on 24 January 2023).
- Wang, Q.; Berger, N.A.; Xu, R. Analyses of Risk, Racial Disparity, and Outcomes among US Patients with Cancer and COVID-19 Infection. JAMA Oncol. 2021, 7, 220–227. [Google Scholar] [CrossRef]
- Guan, W.j.; Liang, W.h.; Zhao, Y.; Liang, H.r.; Chen, Z.s.; Li, Y.m.; Liu, X.q.; Chen, R.-c.; Tang, C.-l.; Wang, T.; et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: A nationwide analysis. Eur. Respir. J. 2020, 55, 2000547. [Google Scholar] [CrossRef] [PubMed]
- Fadini, G.P.; Morieri, M.L.; Longato, E.; Avogaro, A. Prevalence and impact of diabetes among people infected with SARS-CoV-2. J. Endocrinol. Investig. 2020, 43, 867–869. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zheng, Y.; Gou, X.; Pu, K.; Chen, Z.; Guo, Q.; Ji, R.; Wang, H.; Wang, Y.; Zhou, Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis. Int. J. Infect. Dis. 2020, 94, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Henry, B.M. Chronic obstructive pulmonary disease is associated with severe coronavirus disease 2019 (COVID-19). Respir. Med. 2020, 167, 105941. [Google Scholar] [CrossRef] [PubMed]
- Saini, K.S.; Tagliamento, M.; Lambertini, M.; McNally, R.; Romano, M.; Leone, M.; Curigliano, G.; de Azambuja, E. Mortality in patients with cancer and coronavirus disease 2019: A systematic review and pooled analysis of 52 studies. Eur. J. Cancer 2020, 139, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Hu, J.; Zhu, C. Obesity aggravates COVID-19: A systematic review and meta-analysis. J. Med. Virol. 2021, 93, 257–261. [Google Scholar] [CrossRef]
- Földi, M.; Farkas, N.; Kiss, S.; Zádori, N.; Váncsa, S.; Szakó, L.; Dembrovszky, F.; Solymár, M.; Bartalis, E.; Szakács, Z.; et al. Obesity is a risk factor for developing critical condition in COVID-19 patients: A systematic review and meta-analysis. Obes. Rev. 2020, 21, e13095. [Google Scholar] [CrossRef]
- Pranata, R.; Huang, I.; Lim, M.A.; Wahjoepramono, E.J.; July, J. Impact of cerebrovascular and cardiovascular diseases on mortality and severity of COVID-19–systematic review, meta-analysis, and meta-regression. J. Stroke Cerebrovasc. Dis. 2020, 29, 104949. [Google Scholar] [CrossRef]
- Ssentongo, P.; Ssentongo, A.E.; Heilbrunn, E.S.; Ba, D.M.; Chinchilli, V.M. Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0238215. [Google Scholar] [CrossRef] [PubMed]
- Del Sole, F.; Farcomeni, A.; Loffredo, L.; Carnevale, R.; Menichelli, D.; Vicario, T.; Pignatelli, P.; Pastori, D. Features of severe COVID-19: A systematic review and meta-analysis. Eur. J. Clin. Investig. 2020, 50, e13378. [Google Scholar] [CrossRef]
- Bambra, C.; Riordan, R.; Ford, J.; Matthews, F. The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health 2020, 74, 964–968. [Google Scholar] [CrossRef]
- Collaboration, G.B.o.C.D. The Burden of Cardiovascular Diseases among US States, 1990–2016. JAMA Cardiol. 2018, 3, 375–389. [Google Scholar] [CrossRef]
- PolicyMap. Severe COVID-19 Health Risk Index. 2020. Available online: https://slu-policymap-com.ezp.slu.edu/data/our-data-dictionary/#PolicyMap%20Severe%20COVID-19%20Risk%20Index (accessed on 1 February 2022).
- Centers for Disease Control and Prevention. Underlying Medical Conditions Associated with Higher Risk for Severe COVID-19: Information for Healthcare Providers. 2019. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html (accessed on 1 February 2023).
- Boersma, P.; Black, L.; Ward, B.W. Prevalence of Multiple Chronic Conditions among US Adults. Prev. Chronic Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Shaw, K.M.; Theis, K.A.; Self-Brown, S.; Roblin, D.W.; Barker, L. Chronic Disease Disparities by County Economic Status and Metropolitan Classification, Behavioral Risk Factor Surveillance System, 2013. Prev. Chronic Dis. 2016, 13, E119. [Google Scholar] [CrossRef]
- Weissman, G.E.; Kerlin, M.P.; Yuan, Y.; Kohn, R.; Anesi, G.L.; Groeneveld, P.W.; Werner, R.M.; Halpern, S.D. Potentially Preventable Intensive Care Unit Admissions in the United States, 2006–2015. Ann. Am. Thorac. Soc. 2020, 17, 81–88. [Google Scholar] [CrossRef]
- Stelfox, H.T.; Hemmelgarn, B.R.; Bagshaw, S.M.; Gao, S.; Doig, C.J.; Nijssen-Jordan, C.; Manns, B. Intensive Care Unit Bed Availability and Outcomes for Hospitalized Patients with Sudden Clinical Deterioration. Arch. Intern. Med. 2012, 172, 467–474. [Google Scholar] [CrossRef]
- Bindman, A.B.; Grumbach, K.; Osmond, D.; Komaromy, M.; Vranizan, K.; Lurie, N.; Billings, J.; Stewart, A. Preventable hospitalizations and access to health care. JAMA 1995, 274, 305–311. [Google Scholar] [CrossRef]
- Ansah, J.P.; Chiu, C.T. Projecting the chronic disease burden among the adult population in the United States using a multi-state population model. Front. Public Health 2022, 10, 1082183. [Google Scholar] [CrossRef]
- Benda, N.C.; Veinot, T.C.; Sieck, C.J.; Ancker, J.S. Broadband Internet Access Is a Social Determinant of Health! Am. J. Public Health 2020, 110, 1123–1125. [Google Scholar] [CrossRef] [PubMed]
- Fox, S.; Purcell, K. Chronic Disease and the Internet; Pew Internet & American Life Project: Washington, DC, USA, 2010. [Google Scholar]
- Polsky, J.Y.; Gilmour, H. Food insecurity and mental health during the COVID-19 pandemic. Health Rep. 2020, 31, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Coleman-Jensen, A.; Rabbitt, M.P.; Gregory, C.A.; Singh, A. Household Food Security in the United States in 2018. Available online: https://www.ers.usda.gov/webdocs/publications/94849/err-270.pdf (accessed on 8 February 2023).
- Coleman-Jensen, A.; Rabbitt, M.; Singh, A. Household Food Security in the United States in 2019. Available online: https://www.ers.usda.gov/webdocs/publications/99282/err-275.pdf (accessed on 15 February 2023).
- Silverman, J.; Krieger, J.; Kiefer, M.; Hebert, P.; Robinson, J.; Nelson, K. The Relationship between Food Insecurity and Depression, Diabetes Distress and Medication Adherence among Low-Income Patients with Poorly-Controlled Diabetes. J. Gen. Intern. Med. 2015, 30, 1476–1480. [Google Scholar] [CrossRef] [PubMed]
- Texas Commission on Environmental Quality, T. Air Pollution from Particulate Matter. 2020. Available online: https://www.tceq.texas.gov/airquality/sip/criteria-pollutants/sip-pm (accessed on 15 February 2023).
- World Health Organization. WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide. 2023. Available online: https://www.who.int/publications/i/item/9789240034228 (accessed on 8 February 2023).
- Lee, B.J.; Kim, B.; Lee, K. Air pollution exposure and cardiovascular disease. Toxicol. Res. 2014, 30, 71–75. [Google Scholar] [CrossRef]
- Wang, L.; Xie, J.; Hu, Y.; Tian, Y. Air pollution and risk of chronic obstructed pulmonary disease: The modifying effect of genetic susceptibility and lifestyle. eBioMedicine 2022, 79, 103994. [Google Scholar] [CrossRef]
- Keto, J.; Ventola, H.; Jokelainen, J.; Linden, K.; Keinänen-Kiukaanniemi, S.; Timonen, M.; Ylisaukko-oja, T.; Auvinen, J. Cardiovascular disease risk factors in relation to smoking behaviour and history: A population-based cohort study. Open Heart 2016, 3, e000358. [Google Scholar] [CrossRef]
- Reis, C.; Dias, S.; Rodrigues, A.M.; Sousa, R.D.; Gregório, M.J.; Branco, J.; Canhão, H.; Paiva, T. Sleep duration, lifestyles and chronic diseases: A cross-sectional population-based study. Sleep Sci. 2018, 11, 217–230. [Google Scholar] [CrossRef]
- Census. Measuring Racial and Ethnic Diversity for the 2020 Census. 2021. Available online: https://www.census.gov/newsroom/blogs/random-samplings/2021/08/measuring-racial-ethnic-diversity-2020-census.html (accessed on 2 February 2023).
- Socialexplorer. American Community Surveys 5-Years Estimates. 2020. Available online: https://www.socialexplorer.com/explore-tables (accessed on 1 February 2023).
- Explore Health Rankings. 2022 Measures. 2022. Available online: https://www.countyhealthrankings.org/explore-health-rankings/county-health-rankings-measures (accessed on 8 February 2023).
- Yu, L.; Sabatino, S.A.; White, M.C. Rural–Urban and Racial/Ethnic Disparities in Invasive Cervical Cancer Incidence in the United States, 2010–2014. Prev. Chronic Dis. 2019, 16, 180447. [Google Scholar] [CrossRef]
- Henley, S.J.; Anderson, R.N.; Thomas, C.C.; Massetti, G.M.; Peaker, B.; Richardson, L.C. Invasive Cancer Incidence, 2004–2013, and Deaths, 2006–2015, in Nonmetropolitan and Metropolitan Counties—United States. MMWR Surveill. Summ. 2017, 66, 1. [Google Scholar] [CrossRef]
- Kaufman, B.G.; Whitaker, R.; Pink, G.; Holmes, G.M. Half of Rural Residents at High Risk of Serious Illness Due to COVID-19, Creating Stress on Rural Hospitals. J. Rural Health 2020, 36, 584–590. [Google Scholar] [CrossRef]
- Karim, S.A.; Chen, H.F. Deaths from COVID-19 in Rural, Micropolitan, and Metropolitan Areas: A County-Level Comparison. J. Rural Health 2021, 37, 124–132. [Google Scholar] [CrossRef] [PubMed]
- County Health Rankings and Roadmaps. Rankings Data & Documentation. 2021. Available online: https://www.countyhealthrankings.org/explore-health-rankings/rankings-data-documentation (accessed on 1 February 2023).
- PolicyMap. 2021. Available online: https://www.policymap.com/ (accessed on 15 February 2023).
- Github. Urbanmap. 2021. Available online: https://github.com/UrbanInstitute/urbnmapr (accessed on 15 February 2023).
- Sung, B. A spatial analysis of the effect of neighborhood contexts on cumulative number of confirmed cases of COVID-19 in U.S. Counties through 20 October 2020. Prev. Med. 2021, 147, 106457. [Google Scholar] [CrossRef]
- Anselin, L.; Bera, A.K.; Florax, R.; Yoon, M.J. Simple diagnostic tests for spatial dependence. Reg. Sci. Urban Econ. 1996, 26, 77–104. [Google Scholar] [CrossRef]
- Conway, D.; Li, C.Q.; Wolch, J.; Kahle, C.; Jerrett, M. A Spatial Autocorrelation Approach for Examining the Effects of Urban Greenspace on Residential Property Values. J. Real Estate Financ. Econ. 2010, 41, 150–169. [Google Scholar] [CrossRef]
- Kuha, J. AIC and BIC:Comparisons of Assumptions and Performance. Sociol. Methods Res. 2004, 33, 188–229. [Google Scholar] [CrossRef]
- U.S. Department of Health & Human Services. Area Health Resources Files. 2020. Available online: https://data.hrsa.gov/topics/health-workforce/ahrf (accessed on 15 February 2023).
- EPA. Air Quality—Cities and Counties. 2021. Available online: https://www.epa.gov/air-trends/air-quality-cities-and-counties (accessed on 15 February 2023).
- Jensen, L.; Monnat, S.M.; Green, J.J.; Hunter, L.M.; Sliwinski, M.J. Rural Population Health and Aging: Toward a Multilevel and Multidimensional Research Agenda for the 2020s. Am. J. Public Health 2020, 110, 1328–1331. [Google Scholar] [CrossRef] [PubMed]
- The Effects of Violence on Health. Health Aff. 2019, 38, 1622–1629. [CrossRef]
- Vlassoff, C. Gender differences in determinants and consequences of health and illness. J. Health Popul. Nutr. 2007, 25, 47–61. [Google Scholar]
- Extent and Health Consequences of Chronic Sleep Loss and Sleep Disorders. In Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem; Altevogt, B.M.; Institute of Medicine (US) Committee on Sleep Medicine and Research (Eds.) National Academies Press: Washington, DC, USA, 2006; Chapter 3. Available online: https://www.ncbi.nlm.nih.gov/books/NBK19961/ (accessed on 15 February 2023).
- Healthy People 2030. Increase the Proportion of Adults Who Get Enough Sleep—SH-03. 2020. Available online: https://health.gov/healthypeople/objectives-and-data/browse-objectives/sleep/increase-proportion-adults-who-get-enough-sleep-sh-03 (accessed on 20 January 2023).
- Centers for Disease Control and Prevention. Emergency Department Visits. 2022. Available online: https://www.cdc.gov/nchs/fastats/emergency-department.htm (accessed on 20 January 2023).
- Falster, M.O.; Jorm, L.R.; Douglas, K.A.; Blyth, F.M.; Elliott, R.F.; Leyland, A.H. Sociodemographic and health characteristics, rather than primary care supply, are major drivers of geographic variation in preventable hospitalizations in Australia. Med. Care 2015, 53, 436–445. [Google Scholar] [CrossRef]
- Bennett, J.E.; Tamura-Wicks, H.; Parks, R.M.; Burnett, R.T.; Pope, C.A., 3rd; Bechle, M.J.; Marshall, J.D.; Danaei, G.; Ezzati, M. Particulate matter air pollution and national and county life expectancy loss in the USA: A spatiotemporal analysis. PLoS Med. 2019, 16, e1002856. [Google Scholar] [CrossRef]
- Sun, F.; Matthews, S.A.; Yang, T.-C.; Hu, M.-H. A spatial analysis of the COVID-19 period prevalence in U.S. counties through 28 June 2020: Where geography matters? Ann. Epidemiol. 2020, 52, 54–59.e1. [Google Scholar] [CrossRef] [PubMed]
- Mollalo, A.; Vahedi, B.; Rivera, K.M. GIS-based spatial modeling of COVID-19 incidence rate in the continental United States. Sci. Total Environ. 2020, 728, 138884. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Majority White 2826 | Majority Black 130 | Majority Hispanic 125 | Majority Other 27 | Overall Sample | p-Value |
|---|---|---|---|---|---|---|
| COVID-19 SHRI | 92.59 ± 12.96 | 108.65 ± 12.90 | 83.70 ± 9.60 | 98.23 ± 11.54 | 92.85 ± 13.37 | <0.01 |
| % Rural | 59.68 ± 30.89 | 52.59 ± 34.40 | 35.09 ± 30.70 | 76.64 ± 27.06 | 58.06 ± 31.55 | <0.01 |
| Household Income | 58,169.34 ± 14,246.66 | 43,411.35 ± 11,550.58 | 54,951.38 ± 12,075.17 | 43,555.07 ± 20,318.78 | 57,610.36 ± 14,586.42 | <0.01 |
| Age | 41.95 ± 5.21 | 39.25 ± 3.91 | 35.83 ± 5.29 | 31.89 ± 3.64 | 41.47 ± 5.36 | <0.01 |
| Completed High School | 88.36 ± 5.21 | 81.92 ± 5.28 | 76.08 ± 8.97 | 84.44 ± 4.46 | 87.64 ± 6.01 | <0.01 |
| Men to Women Ratio | 100.62 ± 10.45 | 98.65 ± 18.79 | 105.35 ± 13.60 | 98.66 ± 2.76 | 100.67 ± 11.17 | <0.01 |
| Smoking | 20.31 ± 4.02 | 23.39 ± 3.33 | 16.5449 ± 2.2915 | 28.4630 ± 6.4718 | 20.3097 ± 4.2103 | <0.01 |
| Insufficient Sleep | 36.57 ± 3.88 | 42.76 ± 2.28 | 36.2595 ± 2.1045 | 37.8013 ± 2.7749 | 36.7958 ± 3.9591 | <0.01 |
| Log ICU Beds | 0.67 ± 0.52 | 0.64 ± 0.58 | 0.74 ± 0.69 | 0.30 ± 0.28 | 0.61 ± 0.43 | <0.01 |
| % Uninsured | 9.01 ± 4.42 | 12.02 ± 3.11 | 16.13 ± 6.97 | 23.57 ± 8.84 | 9.55 ± 5.09 | <0.01 |
| % PCP | 54.88 ± 36.44 | 48.01 ± 31.51 | 42.75 ± 22.71 | 49.99 ± 24.80 | 54.91 ± 36.48 | <0.01 |
| Preventable Hospitalizations | 4000.22 ± 1531.34 | 5082.67 ± 1412.71 | 3996.67 ± 1454.46 | 4605.11 ± 2099.23 | 4037.70 ± 1542.14 | <0.01 |
| PM2.5 | 7.98 ± 1.56 | 8.61 ± 0.89 | 8.76 ± 3.05 | 6.24 ± 1.96 | 8.01 ± 1.65 | <0.01 |
| Internet Access | 79.27 ± 7.47 | 69.21 ± 11.04 | 75.06 ± 10.06 | 63.10 ± 11.64 | 78.64 ± 8.23 | <0.01 |
| Food Insecurity | 12.83 ± 3.33 | 22.47 ± 4.61 | 11.28 ± 2.76 | 19.51 ± 3.55 | 13.24 ± 3.95 | <0.01 |
| Characteristics | MLR | SLM | SEM | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | 95% CI | |||||||
| β | Lower | Upper | β | Lower | Upper | β | Lower | Upper | |
| Major Racial/Ethnic Group (Ref = Majority Black) | |||||||||
| Majority Hispanic | −6.45 *** | −8.82 | −4.07 | −4.76 *** | −6.86 | −2.66 | −3.08 ** | −5.43 | −0.73 |
| Majority Other | −5.85 ** | −9.74 | −1.97 | −0.13 | −3.59 | 3.33 | −1.92 | −5.51 | 1.66 |
| Majority White | −4.53 *** | −6.14 | −2.92 | −4.62 *** | −6.04 | −3.19 | −3.65 *** | −5.18 | −2.11 |
| Rural | 0.03 *** | 0.02 | 0.05 | 0.02 *** | 0.01 | 0.03 | 0.01 ** | 0.00 | 0.02 |
| Log Household Income | −4.71 *** | −7.16 | −2.26 | −2.57 ** | −4.74 | −0.41 | −3.49 ** | −5.93 | −1.06 |
| Age | 0.52 *** | 0.45 | 0.59 | 0.56 *** | 0.50 | 0.62 | 0.71 *** | 0.65 | 0.78 |
| Completed High School | −0.04 | −0.12 | 0.04 | −0.07 | −0.14 | 0.00 | −0.04 | −0.13 | 0.04 |
| Men to Women Ratio | −0.15 *** | −0.18 | −0.12 | −0.11 *** | −0.14 | −0.09 | −0.10 *** | −0.13 | −0.08 |
| Smokers | 0.82 *** | 0.68 | 0.97 | 0.56 *** | 0.43 | 0.69 | 0.96 *** | 0.80 | 1.13 |
| Insufficient Sleep | 0.78 *** | 0.67 | 0.90 | 0.46 *** | 0.35 | 0.56 | 0.83 *** | 0.68 | 0.97 |
| Log ICU Beds | −0.01 *** | −0.02 | −0.01 | −0.01 *** | −0.01 | −0.01 | −0.01 *** | −0.01 | −0.01 |
| Uninsured | 0.01 | −0.06 | 0.08 | 0.05 | −0.02 | 0.12 | 0.05 | −0.03 | 0.14 |
| PCP | −0.02 *** | −0.03 | −0.02 | −0.03 *** | −0.04 | −0.02 | −0.01 *** | −0.02 | −0.01 |
| Log Preventable Hospitalization | 4.17 *** | 3.35 | 4.99 | 2.78 *** | 2.04 | 3.51 | 2.66 *** | 1.85 | 3.48 |
| PM2.5 | 0.75 *** | 0.56 | 0.94 | 0.46 *** | 0.29 | 0.63 | 0.53 *** | 0.28 | 0.78 |
| Broadband | −0.13 *** | −0.19 | −0.07 | −0.09 *** | −0.15 | −0.04 | −0.07 ** | −0.13 | −0.02 |
| Food Insecurity | 0.16 ** | 0.03 | 0.28 | 0.03 | −0.08 | 0.14 | −0.07 | −0.21 | 0.08 |
| Goodness of Fit | |||||||||
| Rho | 0.41 | 0.38 | 0.44 | ||||||
| Lambda | 0.60 | 0.57 | 0.64 | ||||||
| AIC | 20,039.82 | 19,453 | 19,377 | ||||||
| Log Likelihood | −10,000.91 | −9706.53 | −9668.26 | ||||||
| BIC | 20,153.46 | 19,203.51 | 19,496.11 | ||||||
| Moran’s I of the Residuals | 0.22 ** | 0.08 | −0.022 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Juboori, R.; Subramaniam, D.S.; Hinyard, L.; Sandoval, J.S.O. Unveiling Spatial Associations between COVID-19 Severe Health Index, Racial/Ethnic Composition, and Community Factors in the United States. Int. J. Environ. Res. Public Health 2023, 20, 6643. https://doi.org/10.3390/ijerph20176643
Al Juboori R, Subramaniam DS, Hinyard L, Sandoval JSO. Unveiling Spatial Associations between COVID-19 Severe Health Index, Racial/Ethnic Composition, and Community Factors in the United States. International Journal of Environmental Research and Public Health. 2023; 20(17):6643. https://doi.org/10.3390/ijerph20176643
Chicago/Turabian StyleAl Juboori, Ruaa, Divya S. Subramaniam, Leslie Hinyard, and J. S. Onésimo Sandoval. 2023. "Unveiling Spatial Associations between COVID-19 Severe Health Index, Racial/Ethnic Composition, and Community Factors in the United States" International Journal of Environmental Research and Public Health 20, no. 17: 6643. https://doi.org/10.3390/ijerph20176643
APA StyleAl Juboori, R., Subramaniam, D. S., Hinyard, L., & Sandoval, J. S. O. (2023). Unveiling Spatial Associations between COVID-19 Severe Health Index, Racial/Ethnic Composition, and Community Factors in the United States. International Journal of Environmental Research and Public Health, 20(17), 6643. https://doi.org/10.3390/ijerph20176643







