Cervical Spine Instability Screening Tool Thai Version: Assessment of Convergent Validity and Rater Reliability
Abstract
1. Introduction
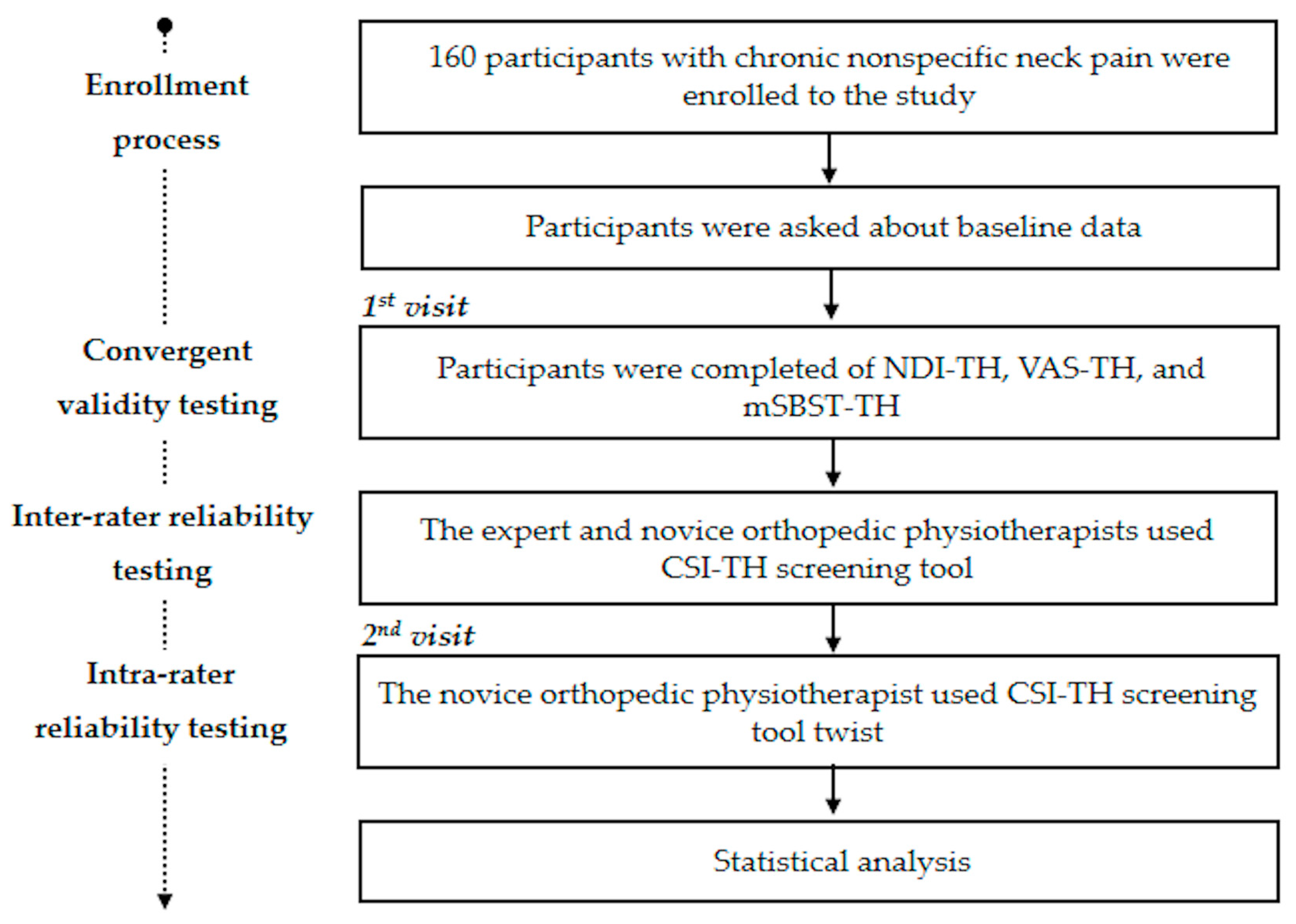
2. Materials and Methods
2.1. Ethics Statement
2.2. Study Population Recruitment
2.3. Procedure
2.4. Questionnaires
2.4.1. The Cervical Spine Instability Thai Version (CSI-TH)
2.4.2. Neck Disability Index Thai Version (NDI-TH)
2.4.3. Visual Analog Scale Thai Version (VAS-TH)
2.4.4. The Modified STarT Back Screening Tool Thai Version (mSBST-TH)
2.4.5. The Global Rating of Change (GRC)
2.5. Statistical Analysis
3. Results
3.1. The Score of Each Questionnaire
3.2. Rater Reliability Consideration
3.3. Convergent Validity Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Theodore, N. Degenerative Cervical Spondylosis. N. Engl. J. Med. 2020, 383, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Binder, A.I. Cervical spondylosis and neck pain. Br. Med. J. 2007, 334, 527–531. [Google Scholar] [CrossRef] [PubMed]
- Rahman, S.; Das, J.M. Anatomy, Head and Neck: Cervical Spine; StatPearls: Treasure Island, FL, USA, 2022. [Google Scholar]
- Webb, R.; Brammah, T.; Lunt, M.; Urwin, M.; Allison, T.; Symmons, D. Prevalence and predictors of intense, chronic, and disabling neck and back pain in the UK general population. Spine 2003, 28, 1195–1202. [Google Scholar] [CrossRef]
- Fejer, R.; Kyvik, K.O.; Hartvigsen, J. The prevalence of neck pain in the world population: A systematic critical review of the literature. Eur. Spine J. 2006, 15, 834–848. [Google Scholar] [CrossRef]
- Shin, D.W.; Shin, J.I.; Koyanagi, A.; Jacob, L.; Smith, L.; Lee, H.; Chang, Y.; Song, T.J. Global, regional, and national neck pain burden in the general population, 1990–2019: An analysis of the global burden of disease study 2019. Front. Neurol. 2022, 13, 955367. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, H.; Yukawa, Y.; Suda, K.; Yamagata, M.; Ueta, T.; Kato, F. Abnormal findings on magnetic resonance images of the cervical spines in 1211 asymptomatic subjects. Spine 2015, 40, 392–398. [Google Scholar] [CrossRef]
- Fakhoury, J.; Dowling, T.J. Cervical Degenerative Disc Disease; StatPearls: Treasure Island, FL, USA, 2022. [Google Scholar]
- Macovei, L.; Rezuş, E. Cervical Spine Lesions in Rheumatoid Arthritis Patients. Rev. Med. Chir. Soc. Med. Nat. Iasi 2016, 120, 70–76. [Google Scholar]
- Mysliwiec, A.; Posłuszny, A.; Saulicz, E.; Doroniewicz, I.; Linek, P.; Wolny, T.; Knapik, A.; Rottermund, J.; Zmijewski, P.; Cieszczyk, P. Atlanto-Axial Instability in People with Down’s Syndrome and its Impact on the Ability to Perform Sports Activities—A Review. J. Hum. Kinet. 2015, 48, 17–24. [Google Scholar] [CrossRef]
- Yeo, C.G.; Jeon, I.; Kim, S.W. Delayed or Missed Diagnosis of Cervical Instability after Traumatic Injury: Usefulness of Dynamic Flexion and Extension Radiographs. Korean J. Spine 2015, 12, 146. [Google Scholar] [CrossRef]
- Panjabi, M.M. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J. Spinal Disord. 1992, 5, 390–396, discussion 397. [Google Scholar] [CrossRef]
- Panjabi, M.M. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J. Spinal Disord. 1992, 5, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Steilen, D.; Hauser, R.; Woldin, B.; Sawyer, S. Chronic Neck Pain: Making the Connection Between Capsular Ligament Laxity and Cervical Instability. Open Orthop. J. 2014, 8, 326–345. [Google Scholar] [CrossRef] [PubMed]
- Dai, L. Disc degeneration and cervical instability. Zhonghua Wai Ke Za Zhi 1999, 37, 180–182. [Google Scholar] [CrossRef]
- Bifulco, P.; Cesarelli, M.; Romano, M.; Fratini, A.; Sansone, M. Measurement of Intervertebral Cervical Motion by Means of Dynamic X-ray Image Processing and Data Interpolation. Int. J. Biomed. Imaging 2013, 2013, 152920. [Google Scholar] [CrossRef] [PubMed]
- Liao, S.; Jung, M.K.; Hörnig, L.; Grützner, P.A.; Kreinest, M. Injuries of the upper cervical spine-how can instability be identified? Int. Orthop. 2020, 44, 1239–1253. [Google Scholar] [CrossRef]
- White, A.A.; Johnson, R.M.; Panjabi, M.M.; Southwick, W.O. Biomechanical analysis of clinical stability in the cervical spine. Clin. Orthop. Relat. Res. 1975, 109, 85–96. [Google Scholar] [CrossRef]
- Karavas, E.; Ece, B.; Aydın, S.; Kocak, M.; Cosgun, Z.; Bostanci, I.E.; Kantarci, M. Are we aware of radiation: A study about necessity of diagnostic X-ray exposure. World J. Methodol. 2022, 12, 264. [Google Scholar] [CrossRef]
- Shi, H.-M.; Sun, Z.-C.; Ju, F.-H. Recommendations for reducing exposure to medical X-ray irradiation (Review). Med. Int. 2022, 2, 22. [Google Scholar] [CrossRef]
- Cook, C.; Brismée, J.M.; Fleming, R.; Sizer, P.S. Identifiers suggestive of clinical cervical spine instability: A Delphi study of physical therapists. Phys. Ther. 2005, 85, 895–906. [Google Scholar] [CrossRef]
- Derrick, L.J.; Chesworth, B.M. Post-motor vehicle accident alar ligament laxity. J. Orthop. Sports Phys. Ther. 1992, 16, 6–11. [Google Scholar] [CrossRef]
- Henderson, F.C.; Francomano, C.A.; Koby, M.; Tuchman, K.; Adcock, J.; Patel, S. Cervical medullary syndrome secondary to craniocervical instability and ventral brainstem compression in hereditary hypermobility connective tissue disorders: 5-year follow-up after craniocervical reduction, fusion, and stabilization. Neurosurg. Rev. 2019, 42, 915. [Google Scholar] [CrossRef] [PubMed]
- Herkowitz, H.N.; Rothman, R.H. Subacute instability of the cervical spine. Spine 1984, 9, 348–357. [Google Scholar] [CrossRef] [PubMed]
- Niere, K.R.; Torney, S.K. Clinicians’ perceptions of minor cervical instability. Man. Ther. 2004, 9, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Olson, K.A.; Joder, D. Diagnosis and treatment of cervical spine clinical instability. J. Orthop. Sports Phys. Ther. 2001, 31, 194–206. [Google Scholar] [CrossRef]
- Paley, D.; Gillespie, R. Chronic repetitive unrecognized flexion injury of the cervical spine (high jumper’s neck). Am. J. Sports Med. 1986, 14, 92–95. [Google Scholar] [CrossRef]
- Rueangsri, C.; Puntumetakul, R.; Sae-jung, S.; Phadungkit, S. Content Validity of Thai Version Screening Tool for Cervical Spine Instability. In Proceedings of the 2nd International Conference on Integrative Medicine, Chiang Rai, Thailand, 20–21 July 2022; pp. 143–146. [Google Scholar]
- Cleland, J.A.; Childs, J.D.; Whitman, J.M. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch. Phys. Med. Rehabil. 2008, 89, 69–74. [Google Scholar] [CrossRef]
- Guzman, J.; Haldeman, S.; Carroll, L.J.; Carragee, E.J.; Hurwitz, E.L.; Peloso, P.; Nordin, M.; Cassidy, J.D.; Holm, L.W.; Côté, P.; et al. Clinical practice implications of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders: From concepts and findings to recommendations. Spine 2008, 33, S199–S213. [Google Scholar] [CrossRef]
- Sousa, V.D.; Rojjanasrirat, W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. J. Eval. Clin. Pract. 2011, 17, 268–274. [Google Scholar] [CrossRef]
- Lim, H.H.R.; Tang, Z.Y.; Hashim, M.A.B.M.; Yang, M.; Koh, E.Y.L.; Koh, K.H. Cross-cultural adaptation, reliability, validity, and responsiveness of the Simplified-Chinese Version of Neck Disability Index. Spine 2020, 45, 541–548. [Google Scholar] [CrossRef]
- Rovinelli, R.; Hambleton, R. On the Use of Content Specialists in the Assessment of Criterion-Referenced Test Item Validity. In Proceedings of the Presented at the Annual Meeting of the American Educational Research Association, San Francisco, CA, USA, 19–23 April 1976. [Google Scholar]
- Uthaikhup, S.; Paungmali, A.; Pirunsan, U. Validation of thai versions of the neck disability index and neck pain and disability scale in patients with neck pain. Spine 2011, 36, 1415–1421. [Google Scholar] [CrossRef]
- Luksanapruksa, P.; Wathana-Apisit Md, T.; Wanasinthop, S.; Sanpakit, S.; Chavasiri, C. Reliability and Validity Study of a Thai Version of the Neck Disability Index in Patients with Neck Pain. J. Med. Assoc. Thai 2012, 95, 681–688. [Google Scholar] [PubMed]
- Macdelilld, J.C.; Walton, D.M.; Avery, S.; Blanchard, A.; Etruw, E.; Mcalpine, C.; Goldsmith, C.H. Measurement properties of the neck disability index: A systematic review. J. Orthop. Sports Phys. Ther. 2009, 39, 400–416. [Google Scholar] [CrossRef]
- Carlsson, A.M. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 1983, 16, 87–101. [Google Scholar] [CrossRef] [PubMed]
- Bijur, P.E.; Silver, W.; Gallagher, E.J. Reliability of the visual analog scale for measurement of acute pain. Acad. Emerg. Med. 2001, 8, 1153–1157. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, A.M.; Schiphorst Preuper, H.R.; Reneman, M.F.; Posthumus, J.B.; Stewart, R.E. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int. J. Rehabil. Res. 2008, 31, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Crossley, K.M.; Bennell, K.L.; Cowan, S.M.; Green, S. Analysis of outcome measures for persons with patellofemoral pain: Which are reliable and valid? Arch. Phys. Med. Rehabil. 2004, 85, 815–822. [Google Scholar] [CrossRef]
- Bier, J.D.; Ostelo, R.W.J.G.; Koes, B.W.; Verhagen, A.P. Validity and reproducibility of the modified STarT Back Tool (Dutch version) for patients with neck pain in primary care. Musculoskelet. Sci. Pract. 2017, 31, 22–29. [Google Scholar] [CrossRef]
- Bier, J.D.; Ostelo, R.W.J.G.; Van Hooff, M.L.; Koes, B.W.; Verhagen, A.P. Validity and Reproducibility of the STarT Back Tool (Dutch Version) in Patients with Low Back Pain in Primary Care Settings. Phys. Ther. 2017, 97, 561–570. [Google Scholar] [CrossRef]
- Hill, J.C.; Dunn, K.M.; Lewis, M.; Mullis, R.; Main, C.J.; Foster, N.E.; Hay, E.M. A primary care back pain screening tool: Identifying patient subgroups for initial treatment. Arthritis Rheum. 2008, 59, 632–641. [Google Scholar] [CrossRef]
- Phungwattanakul, N.; Boonyapo, U.; Wiangkham, T. Adaptation and psychometric evaluation of the Thai version of the modified STarT Back Screening Tool in individuals with neck pain. Physiother. Theory Pract. 2022, 1–10. [Google Scholar] [CrossRef]
- Kamper, S.J.; Maher, C.G.; Mackay, G. Global rating of change scales: A review of strengths and weaknesses and considerations for design. J. Man. Manip. Ther. 2009, 17, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Wright, A.A.; Abbott, J.H.; Baxter, D.; Cook, C. The ability of a sustained within-session finding of pain reduction during traction to dictate improved outcomes from a manual therapy approach on patients with osteoarthritis of the hip. J. Man. Manip. Ther. 2020, 18, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research Applications to Practice, 3rd ed.; Julie, L.A., Ed.; Pearson/Prentice Hall: Upper Saddle River, NJ, USA, 2009; p. 525. [Google Scholar]
- Chatprem, T.; Puntumetakul, R.; Boucaut, R.; Wanpen, S.; Chatchawan, U. A Screening Tool for Patients with Lumbar Instability: A Criteria-related Validity of Thai Version. Spine 2020, 45, E1431–E1438. [Google Scholar] [CrossRef]
- Hwang, S.; Mun, M.-H. Relationship of neck disability index, shoulder pain and disability index, and visual analogue scale in individuals with chronic neck pain. Phys. Ther. Rehabil. Sci. 2013, 2, 111–114. [Google Scholar] [CrossRef][Green Version]
- Lazaridou, A.; Elbaridi, N.; Edwards, R.R.; Berde, C.B. Pain Assessment. In Essentials of Pain Medicine; Elsevier: Amsterdam, The Netherlands, 2018; pp. 39–46.e1. [Google Scholar] [CrossRef]
- Sterling, M.; Rebbeck, T. The Neck Disability Index (NDI). Aust. J. Physiother. 2005, 51, 271. [Google Scholar] [CrossRef]
- Kääriä, S.; Laaksonen, M.; Rahkonen, O.; Lahelma, E.; Leino-Arjas, P. Risk factors of chronic neck pain: A prospective study among middle-aged employees. Eur. J. Pain 2012, 16, 911–920. [Google Scholar] [CrossRef] [PubMed]
- Safiri, S.; Kolahi, A.-A.; Hoy, D.; Buchbinder, R.; Mansournia, M.A.; Bettampadi, D.; Ashrafi-Asgarabad, A.; Almasi-Hashiani, A.; Smith, E.; Sepidarkish, M.; et al. Global, regional, and national burden of neck pain in the general population, 1990–2017: Systematic analysis of the global burden of disease study 2017. BMJ 2020, 368, m791. [Google Scholar] [CrossRef]
- Côté, P.; Cassidy, D.J.; Carroll, L.J.; Kristman, V. The annual incidence and course of neck pain in the general population: A population-based cohort study. Pain 2004, 112, 267–273. [Google Scholar] [CrossRef]
- McLean, S.M.; May, S.; Klaber-Moffett, J.; Sharp, D.M.; Gardiner, E. Risk factors for the onset of non-specific neck pain: A systematic review. J. Epidemiol. Community Health 2010, 64, 565–572. [Google Scholar] [CrossRef]
- Fillingim, R.B.; King, C.D.; Ribeiro-Dasilva, M.C.; Rahim-Williams, B.; Riley, J.L., III. Sex, gender, and pain: A review of recent clinical and experimental findings. J. Pain 2009, 10, 447–485. [Google Scholar] [CrossRef]

| Items | Patients Respond | |
|---|---|---|
| Yes | No | |
| 1. Intolerance to prolonged static postures | ||
| 2. Fatigue and inability to hold the head up | ||
| 3. Better with external support, including hands or a collar | ||
| 4. Frequent need for self-manipulation | ||
| 5. Feeling of instability, shaking, or lack of control | ||
| 6. Frequent episodes of acute attacks | ||
| 7. Sharp pain, possibly with sudden movements | ||
| 8. The head feels heavy | ||
| 9. The neck gets stuck, or locks, with movement | ||
| 10. Better in an unloaded position, such as lying down | ||
| 11. Catching, clicking, clunking, and popping sensations | ||
| 12. Past history of neck dysfunction or trauma | ||
| 13. Trivial movements provoke symptoms | ||
| 14. Muscles feel tight or stiff | ||
| 15. Unwillingness, apprehension, or fear as regards movement | ||
| 16. Temporary improvement with clinical manipulation | ||
| Total | ||
| n (%) | Mean ± SD | Range | |
|---|---|---|---|
| Age (years) | 44.6 ± 6.5 | 35–55 | |
| Gender | |||
| Male | 32 (20.0) | ||
| Female | 128 (80.0) | ||
| Underlying disease | |||
| Yes | 25 (15.63) | ||
| No | 135 (84.37) | ||
| Education level | |||
| Primary school | 32 (20.0) | ||
| High school | 45 (28.13) | ||
| University | 83 (51.87) | ||
| Pain duration (months) | 15.48 ± 19.26 | 3 to 120 | |
| 3–12 | 126 (78.75) | ||
| >12 | 34 (21.25) | ||
| GRC score | 0.01 ± 0.45 | −2 to 3 |
| Min | Q1 | Median | Mean | Q3 | Max | |
|---|---|---|---|---|---|---|
| CSI-TH (score) | 2 | 6 | 8 | 7.7 | 9 | 14 |
| VAS-TH (score) | 0.3 | 3.2 | 4.5 | 4.4 | 5.8 | 9.3 |
| mSBST-TH (score) | 0 | 3 | 4 | 4.3 | 5 | 9 |
| NDI-TH (score) | 0 | 6 | 11 | 10.9 | 16 | 30 |
| Mean ± SD | ICC | 95% CI | ||
|---|---|---|---|---|
| Expert | Novice | |||
| Inter-rater reliability | 7.70 ± 2.56 | 7.72 ± 2.60 | 0.987 | 0.983–0.991 |
| Intra-rater reliability | 7.68 ± 2.52 | 0.992 | 0.989–0.994 | |
| Correlation | CSI-TH | VAS-TH | mSBST-TH | NDI-TH |
|---|---|---|---|---|
| CSI-TH | 1.00 | 0.5446 * | 0.5136 * | 0.5545 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rueangsri, C.; Puntumetakul, R.; Leungbootnak, A.; Sae-Jung, S.; Chatprem, T. Cervical Spine Instability Screening Tool Thai Version: Assessment of Convergent Validity and Rater Reliability. Int. J. Environ. Res. Public Health 2023, 20, 6645. https://doi.org/10.3390/ijerph20176645
Rueangsri C, Puntumetakul R, Leungbootnak A, Sae-Jung S, Chatprem T. Cervical Spine Instability Screening Tool Thai Version: Assessment of Convergent Validity and Rater Reliability. International Journal of Environmental Research and Public Health. 2023; 20(17):6645. https://doi.org/10.3390/ijerph20176645
Chicago/Turabian StyleRueangsri, Chanyawat, Rungthip Puntumetakul, Arisa Leungbootnak, Surachai Sae-Jung, and Thiwaphon Chatprem. 2023. "Cervical Spine Instability Screening Tool Thai Version: Assessment of Convergent Validity and Rater Reliability" International Journal of Environmental Research and Public Health 20, no. 17: 6645. https://doi.org/10.3390/ijerph20176645
APA StyleRueangsri, C., Puntumetakul, R., Leungbootnak, A., Sae-Jung, S., & Chatprem, T. (2023). Cervical Spine Instability Screening Tool Thai Version: Assessment of Convergent Validity and Rater Reliability. International Journal of Environmental Research and Public Health, 20(17), 6645. https://doi.org/10.3390/ijerph20176645






