Psychological Reactions during and after a Lockdown: Self-Efficacy as a Protective Factor of Mental Health
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Materials
2.2.1. Psychological Factors
- State-Trait Anxiety Inventory (STAI): The STAI [42,43] measures both the level of anxiety present at the time of assessment (i.e., state anxiety) and the genetic predisposition to be anxious (i.e., trait anxiety). The latter is more of a personal trait. It is a self-reported inventory with a 4-point Likert scale in which 20 items (S scale) measure feelings of worry, nervousness, apprehension, tension, etc. at the moment (i.e., “How do you feel now?”), while another 20 items (T scale) measure relatively stable aspects of “anxiety vulnerability”, such as general calmness, confidence and security. The scores range from 20 to 80, with higher scores corresponding to greater anxiety. To detect significant clinical symptoms on the S-Anxiety scale, a cut-off of 39–40 is indicated [44,45,46]. Some studies suggest a higher cut-off of 54–55 [43]. In general, several studies have shown both acceptable internal consistency (Cronbach’s alpha of 0.91 to 0.95 for the S scale; 0.85 to 0.90 for the T scale) and good test–retest reliability (0.49 for the S scale and 0.82 for the T scale) [47].
- Perceived Stress Scale (PSS): The PSS was used to assess the perceived stress levels [48,49,50]. It measures the extent to which a person perceives that the demands of everyday life situations exceed their ability to cope with them, i.e., how stressful they are. The instrument consists of 10 items rated on a 5-point Likert scale ranging from 0 = ‘never’ to 4 = ‘very often’. Participants are asked to indicate the extent to which they have felt or thought a certain way in response to stressful situations in the past month. Scores range from 0 to 40, with higher scores indicating higher perceived stress (low stress: between 0 and 13; moderate stress: between 14 and 26; high stress: between 27 and 40). A satisfactory internal consistency (overall Cronbach’s alpha was 0.74) and test–retest reliability (i.e., 0.86 after one week, 0.61 after one year) of the PSS has been observed [51,52,53].
- General Self-Efficacy Scale (GSES): The GSES measures how well a person feels able to cope with a range of difficult demands in life [54]. The instrument consists of 10 items scored on a 4-point Likert scale. The items refer explicitly to personal agency, i.e., believing that one’s own actions are responsible for achieving positive outcomes. Scholz and colleagues [55] reported high reliability of the scale (alpha range: 0.75–0.92, across 25 different countries) and its validity has been shown in several works (see: http://userpage.fu-berlin.de/~health/faq_gse.pdf accessed on 21 August 2023).
2.2.2. Situational Factors
2.3. Procedure
2.4. Data Analysis
3. Results
3.1. What Are the Predictors of State Anxiety during Confinement (H1)?
3.2. What Are the Predictors of Perceived Stress during Confinement (H2)?
3.3. Does the End of the Lockdown Lead to Improved Mental Health (H3)?
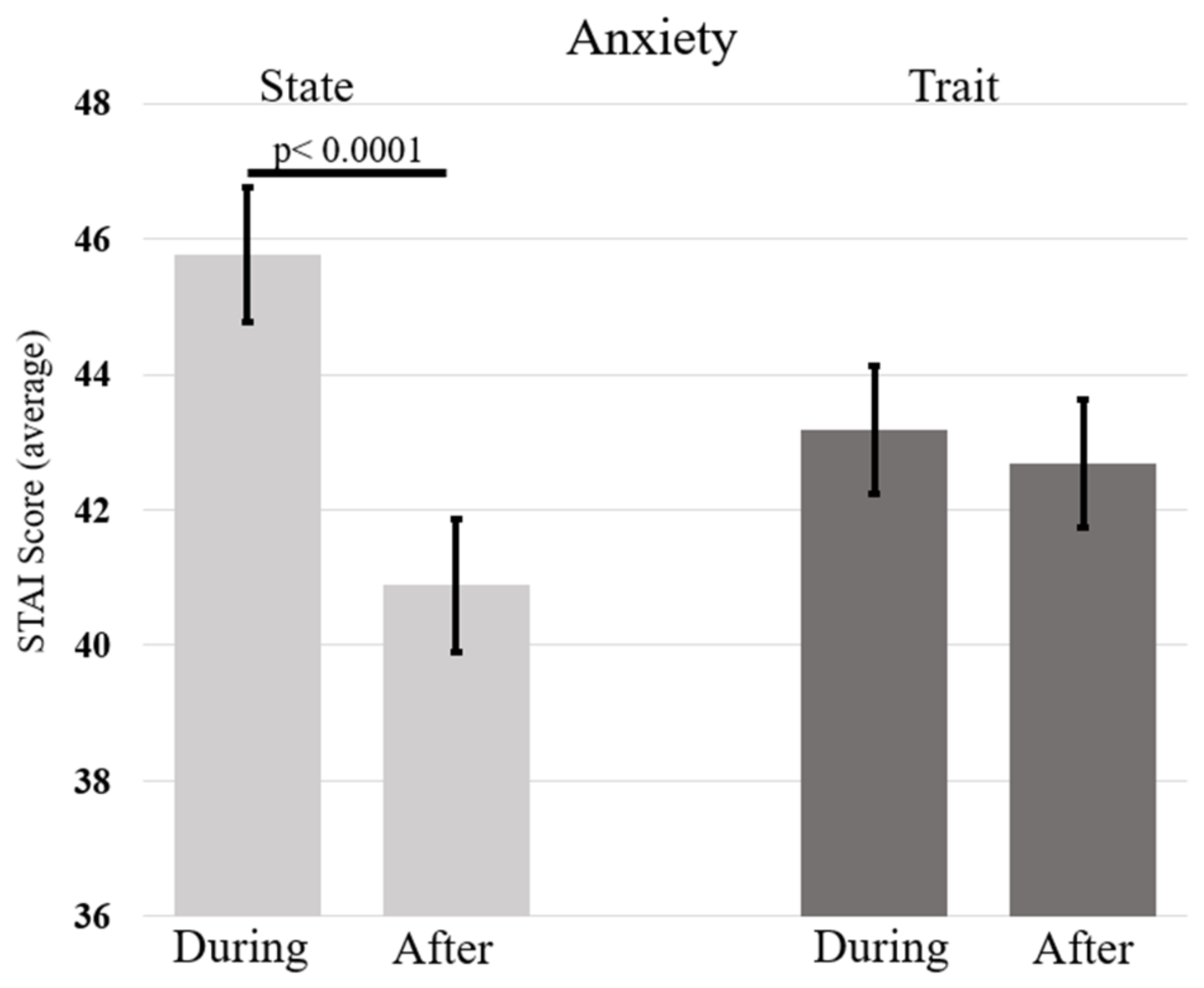
3.3.1. Anxiety Levels during and after Confinement
3.3.2. Perceived Stress during and after Confinement
3.3.3. Feeling of Isolation during and after Confinement
3.3.4. Safety Inside and Outside the Home during and after Confinement
3.4. Does Self-Efficacy Predict the Mental Health of Individuals after Confinement (H4)?
4. Discussion
4.1. Predictors of State Anxiety and Perceived Stress during the COVID-19 Lockdown
4.2. Mental Health before and after Lockdown and Gender Differences
4.3. The Role of Self-Efficacy as a Protective Factor of Mental Health
4.4. Limitations of the Current Study
5. Conclusions
- (i)
- Females showed higher levels of trait anxiety and feelings of isolation, which were associated with higher levels of perceived stress and state anxiety during lockdown. Interestingly, the presence of children at home was associated with higher levels of anxiety but not stress, whereas young age was associated with higher levels of stress but not anxiety.
- (ii)
- More importantly, the novelty of this study lies in having compared the picture that emerged during confinement with that after the end of restrictions. After the lockdown, levels of stress, state anxiety and feelings of isolation had decreased, and the sense of safety outside the home had increased, but this was more true for men than for women.
- (iii)
- Finally, the current study crucially showed that self-efficacy may play a protective role in recovering mental well-being after a lockdown. In fact, higher levels of self-efficacy were associated with lower levels of perceived stress, state anxiety and sense of isolation, and with higher levels of perceived safety outside home.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tang, B.; Xia, F.; Tang, S.; Bragazzi, N.L.; Li, Q.; Sun, X.; Liang, J.; Xiao, Y.; Wu, J. The effectiveness of quarantine and isolation determine the trend of the COVID-19 epidemics in the final phase of the current outbreak in China. Int. J. Infect. Dis. 2020, 95, 288–293. [Google Scholar] [CrossRef] [PubMed]
- Ammar, A.; Trabelsi, K.; Brach, M.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of home confinement on mental health and lifestyle behaviours during the COVID-19 outbreak: Insight from the ECLB-COVID19 multicenter study. Biol. Sport 2021, 38, 9–21. [Google Scholar] [CrossRef]
- Rehman, U.; Shahnawaz, M.G.; Khan, N.H.; Kharshiing, K.D.; Khursheed, M.; Gupta, K.; Kashyap, D.; Uniyal, R. Depression, anxiety and stress among Indians in times of COVID-19 lockdown. Community Ment. Health J. 2021, 57, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Malesza, M.; Kaczmarek, M.C. Predictors of anxiety during the COVID-19 pandemic in Poland. Pers. Individ. Differ. 2021, 170, 110419. [Google Scholar] [CrossRef] [PubMed]
- Creswell, C.; Shum, A.; Pearcey, S.; Skripkauskaite, S.; Patalay, P.; Waite, P. Young people’s mental health during the COVID-19 pandemic. Lancet Child Adolesc. Health 2021, 5, 535–537. [Google Scholar] [CrossRef] [PubMed]
- Knox, L.; Karantzas, G.C.; Romano, D.; Feeney, J.A.; Simpson, J.A. One Year On: What we have learned about the psychological effects of COVID-19 social restrictions—A meta-analysis. Curr. Opin. Psychol. 2022, 46, 101315. [Google Scholar] [CrossRef]
- Bonati, M.; Campi, R.; Segre, G. Psychological impact of the quarantine during the COVID-19 pandemic on the general European adult population: A systematic review of the evidence. Epidemiol. Psych. Sci. 2022, 31, e27. [Google Scholar] [CrossRef]
- García-Prado, A.; González, P.; Rebollo-Sanz, Y.F. Lockdown strictness and mental health effects among older populations in Europe. Econ. Hum. Biol. 2022, 45, 101116. [Google Scholar] [CrossRef]
- Butterworth, P.; Schurer, S.; Trinh, T.A.; Vera-Toscano, E.; Wooden, M. Effect of lockdown on mental health in Australia: Evidence from a natural experiment analysing a longitudinal probability sample survey. Lancet Public Health 2022, 7, e427–e436. [Google Scholar] [CrossRef]
- Adams-Prassl, A.; Boneva, T.; Golin, M.; Rauh, C. The impact of the coronavirus lockdown on mental health: Evidence from the United States. Econ. Policy 2022, 37, 139–155. [Google Scholar] [CrossRef]
- Bower, M.; Smout, S.; Donohoe-Bales, A.; O’dean, S.; Teesson, L.; Boyle, J.; Lim, D.; Nguyen, A.; Calear, A.L.; Batterham, P.J.; et al. A hidden pandemic? An umbrella review of global evidence on mental health in the time of COVID-19. Front. Psychiatry 2023, 14, 1107560. [Google Scholar] [CrossRef] [PubMed]
- Barbisch, D.; Koenig, K.L.; Shih, F.Y. Is there a case for quarantine? Perspectives from SARS to Ebola. Disaster Med. Public 2015, 9, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Miles, S.H. Kaci Hickox: Public health and the politics of fear. Am. J. Bioeth. 2015, 15, 17–19. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef] [PubMed]
- Moghanibashi-Mansourieh, A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatry 2020, 51, 102076. [Google Scholar] [CrossRef]
- Ahmed, R.R.; Streimikiene, D.; Rolle, J.A.; Duc, P.A. The COVID-19 pandemic and the antecedants for the impulse buying behavior of US Citizens. J. Compet. 2020, 12, 5–27. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Shevlin, M.; McBride, O.; Murphy, J.; Miller, J.G.; Hartman, T.K.; Levita, L.; Mason, L.; Martinez, A.P.; McKay, R.; Stocks, T.V.A.; et al. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open 2020, 6, e125. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Özdin, S.; Bayrak Özdin, Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int. J. Soc. Psychiatry 2020, 66, 504–511. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Talevi, D.; Mensi, S.; Niolu, C.; Pacitti, F.; Di Marco, A.; Rossi, A.; Siracusano, A.; Di Lorenzo, G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiatry 2020, 11, 790. [Google Scholar] [CrossRef] [PubMed]
- White, R.G.; Boor, C.V.D. Impact of the COVID-19 pandemic and initial period of lockdown on the mental health and well-being of adults in the UK. BJPsych Open 2020, 6, e90. [Google Scholar] [CrossRef] [PubMed]
- Sigdel, A.; Bista, A.; Bhattarai, N.; Pun, B.C.; Giri, G.; Marqusee, H.; Thapa, S. Depression, Anxiety and Depression-anxiety comorbidity amid COVID-19 Pandemic: An online survey conducted during lockdown in Nepal. medRxiv 2020. [Google Scholar] [CrossRef]
- Verma, S.; Mishra, A. Depression, anxiety, and stress and socio-demographic correlates among general Indian public during COVID-19. Int. J. Soc. Psychiatry 2020, 66, 756–762. [Google Scholar] [CrossRef] [PubMed]
- Hawkley, L.C.; Cacioppo, J.T. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 2010, 40, 218–227. [Google Scholar] [CrossRef]
- Gu, X.; Obrenovic, B.; Fu, W. Empirical Study on Social Media Exposure and Fear as Drivers of Anxiety and Depression during the COVID-19 Pandemic. Sustainability 2023, 15, 5312. [Google Scholar] [CrossRef]
- Khomaeny, E.F.F.; Kusumaputeri, E.S. Parental anxiety and form of parenting during the COVID-19 pandemic. Int. J. Child Care Educ. Policy 2022, 16, 10. [Google Scholar] [CrossRef]
- Leonard, B.E.; Song, C. Stress and the immune system in the etiology of anxiety and depression. Pharmacol. Biochem. Behav. 1996, 54, 299–303. [Google Scholar] [CrossRef]
- Yıldırım, M.; Güler, A. COVID-19 severity, self-efficacy, knowledge, preventive behaviors, and mental health in Turkey. Death Stud. 2022, 46, 979–986. [Google Scholar] [CrossRef] [PubMed]
- Cuadrado, E.; Rich-Ruiz, M.; Gutiérrez-Domingo, T.; Luque, B.; Castillo-Mayén, R.; Villaécija, J.; Farhane-Medina, N.Z. Regulatory emotional self-efficacy and anxiety in times of pandemic: A gender perspective. Health Psychol. Behav. Med. 2023, 11, 2158831. [Google Scholar] [CrossRef] [PubMed]
- Saxena, A.; Jangra, M.K. The level of perceived stress, burnout, self-efficacy, and coping strategies among physiotherapy academicians during the COVID-19 lockdown. Work 2023, 75, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Karademas, E.C.; Thomadakis, C. COVID-19 pandemic-related representations, self-efficacy, and psychological well-being in the general population during lockdown. Curr. Psychol. 2023, 42, 4523–4530. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-efficacy mechanism in psychobiologic functioning. In Self-Efficacy: Thought Control of Action; Schwarzer, R., Ed.; Taylor & Francis: New York, NY, USA, 1992; Volume 2, pp. 355–394. [Google Scholar]
- Bisschop, M.I.; Kriegsman, D.M.; Beekman, A.T.; Deeg, D.J. Chronic diseases and depression: The modifying role of psychosocial resources. Soc. Sci. Med. 2004, 59, 721–733. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zu, X.; Luo, W.; Yang, H.; Luo, G.; Zhang, M.; Tang, S. Social isolation produces anxiety-like behaviors and changes PSD-95 levels in the forebrain. Neurosci. Lett. 2012, 514, 27–30. [Google Scholar] [CrossRef]
- Skelly, M.J.; Chappell, A.E.; Carter, E.; Weiner, J.L. Adolescent social isolation increases anxiety-like behavior and ethanol intake and impairs fear extinction in adulthood: Possible role of disrupted noradrenergic signaling. Neuropharmacology 2015, 97, 149–159. [Google Scholar] [CrossRef]
- Leal, P.C.; Goes, T.C.; da Silva, L.C.F.; Teixeira-Silva, F. Trait vs. state anxiety in different threatening situations. Trends Psychiatry Psychother. 2017, 39, 147–157. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Iachini, T.; Frassinetti, F.; Ruotolo, F.; Sbordone, F.L.; Ferrara, A.; Arioli, M.; Pazzaglia, F.; Bosco, A.; Candini, M.; Lopez, A.; et al. Social distance during the COVID-19 pandemic reflects perceived rather than actual risk. Int. J. Environ. Res. Public Health 2021, 18, 5504. [Google Scholar] [CrossRef]
- Spielberger, C.D. State-Trait anxiety inventory. In The Corsini Encyclopedia of Psychology; Wiley Online Library: Hoboken, NJ, USA, 2010. [Google Scholar]
- Julian, L.J. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res. 2011, 63, S467–S472. [Google Scholar] [CrossRef] [PubMed]
- Addolorato, G.; Ancona, C.; Capristo, E.; Graziosetto, R.; Di Rienzo, L.; Maurizi, M.; Gasbarrini, G. State and trait anxiety in women affected by allergic and vasomotor rhinitis. J. Psychosom. Res. 1999, 46, 283–289. [Google Scholar] [CrossRef]
- Knight, R.G.; Waal-Manning, H.J.; Spears, G.F. Some norms and reliability data for the State-Trait Anxiety Inventory and the Zung Self-Rating Depression scale. Br. J. Clin. Psychol. 1983, 22, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Kvaal, K.; Ulstein, I.; Nordhus, I.H.; Engedal, K. The Spielberger State-Trait Anxiety Inventory (STAI): The state scale in detecting mental disorders in geriatric patients. Int. J. Geriatr. Psych. 2005, 20, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Spielberger, C.D.; Pedrabissi, L.; Santinello, M. STAI State-Trait Anxiety Inventory Forma Y: Manuale; Giunti OS Organizzazioni Speciali: Firenze, Italy, 2012. [Google Scholar]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Cohen, S. Perceived stress in a probability sample of the United States. In The Claremont Symposium on Applied Social Psychology the Social Psychology of Health; Spacapan, S., Oskamp, S., Eds.; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1988; pp. 31–67. [Google Scholar]
- Fossati, A. Traduzione Italiana della Scala per lo Stress Percepito [Italian Translation of the Perceived Stress Scale]; Università Vita-Salute San Raffaele: Milano, Italy, 2010. [Google Scholar]
- Mondo, M.; Sechi, C.; Cabras, C. Psychometric evaluation of three versions of the Italian Perceived Stress Scale. Curr. Psychol. 2021, 40, 1884–1892. [Google Scholar] [CrossRef]
- Remor, E. Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS). Span. J. Psychol. 2006, 9, 86–93. [Google Scholar] [CrossRef]
- Siqueira Reis, R.; Ferreira, H.A.A.; Romélio, R.A.C. Perceived stress scale: Reliability and validity study in Brazil. J. Health Psychol. 2010, 15, 107–114. [Google Scholar] [CrossRef]
- Schwarzer, R.; Jerusalem, M. Generalized self-efficacy scale. In Measures in Health Psychology: A User’s Portfolio. Causal and Control Beliefs; Weinman, J., Wright, S., Johnston, M., Eds.; NFER-Nelson: Windsor, UK, 1995; Volume 35, p. 37. [Google Scholar]
- Scholtz, U.; Doña, B.G.; Sud, S.; Schwarzer, R. Is general self-efficacy a universal construct? Psychometric findings from 25 countries. Eur. J. Psychol. Assess 2002, 18, 242. [Google Scholar] [CrossRef]
- Stoet, G. PsyToolkit: A software package for programming psychological experiments using Linux. Behav. Res. Methods 2010, 42, 1096–1104. [Google Scholar] [CrossRef]
- Stoet, G. PsyToolkit: A novel web-based method for running online questionnaires and reaction-time experiments. Teach. Psychol. 2017, 44, 24–31. [Google Scholar] [CrossRef]
- Adhanom Ghebreyesus, T. Addressing mental health needs: An integral part of COVID-19 response. World Psychiatry 2020, 19, 129–130. [Google Scholar] [CrossRef] [PubMed]
- Van Bavel, J.J.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef]
- Archer, J.; Bower, P.; Gilbody, S.; Lovell, K.; Richards, D.; Gask, L.; Dickens, C.; Coventry, P. Collaborative care for depression and anxiety problems. Cochrane Database Syst. Rev. 2012, 10, CD006525. [Google Scholar] [CrossRef]
- Lauterbach, D.; Vora, R.; Rakow, M. The relationship between posttraumatic stress disorder and self-reported health problems. Psychosom. Med. 2005, 67, 939–947. [Google Scholar] [CrossRef]
- Auerbach, J.; Miller, B.F. COVID-19 exposes the cracks in our already fragile mental health system. Am. J. Public Health 2020, 110, 969–970. [Google Scholar] [CrossRef] [PubMed]
- Endler, N.S.; Kocovski, N.L. State and trait anxiety revisited. J. Anxiety Disord. 2001, 15, 231–245. [Google Scholar] [CrossRef]
- Killgore, W.D.; Cloonan, S.A.; Taylor, E.C.; Dailey, N.S. Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Res. 2020, 290, 113117. [Google Scholar] [CrossRef]
- Ingram, J.; Maciejewski, G.; Hand, C.J. Changes in diet, sleep, and physical activity are associated with differences in negative mood during COVID-19 lockdown. Front. Psychol. 2020, 11, 588604. [Google Scholar] [CrossRef]
- Lenzo, V.; Quattropani, M.C.; Musetti, A.; Zenesini, C.; Freda, M.F.; Lemmo, D.; Vegni, E.; Borghi, L.; Plazzi, G.; Castelnuovo, G.; et al. Resilience contributes to low emotional impact of the COVID-19 outbreak among the general population in Italy. Front. Psychol. 2020, 11, 576485. [Google Scholar] [CrossRef]
- Mazza, M.; Marano, G.; Lai, C.; Janiri, L.; Sani, G. Danger in danger: Interpersonal violence during COVID-19 quarantine. Psychiatry Res. 2020, 289, 113046. [Google Scholar] [CrossRef] [PubMed]
- Moccia, L.; Janiri, D.; Pepe, M.; Dattoli, L.; Molinaro, M.; De Martin, V.; Chieffo, D.; Janiri, L.; Fiorillo, A.; Sani, G.; et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: An early report on the Italian general population. Brain Behav. Immun. 2020, 87, 75–79. [Google Scholar] [CrossRef] [PubMed]
- OECD Policy Responses to Coronavirus (COVID-19): Women at the Core of the Fight against COVID-19 Crisis. Available online: https://www.oecd.org/coronavirus/policy-responses/women-at-the-core-of-the-fight-against-covid-19-crisis-553a8269/ (accessed on 20 August 2023).
- News European Parliament: Understanding COVID-19’s Impact on Women (Infographics). Available online: https://www.europarl.europa.eu/news/en/headlines/society/20210225STO98702/understanding-the-impact-of-covid-19-on-women-infographics (accessed on 20 August 2023).
- Blendon, R.J.; Benson, J.M.; DesRoches, C.M.; Raleigh, E.; Taylor-Clark, K. The public’s response to severe acute respiratory syndrome in Toronto and the United States. Clin. Infect. Dis. 2004, 38, 925–931. [Google Scholar] [CrossRef] [PubMed]
- Desclaux, A.; Badji, D.; Ndione, A.G.; Sow, K. Accepted monitoring or endured quarantine? Ebola contacts’ perceptions in Senegal. Soc. Sci. Med. 2017, 178, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Hall, R.C.W.; Chapman, M.J. The 1995 Kikwit Ebola outbreak: Lessons hospitals and physicians can apply to future viral epidemics. Gen. Hosp. Psychiatry 2008, 30, 446–452. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.R.; Agho, K.E.; Stevens, G.J.; Raphael, B. Factors influencing psychological distress during a disease epidemic: Data from Australia’s first outbreak of equine influenza. BMC Public Health 2008, 8, 347. [Google Scholar] [CrossRef] [PubMed]
- Kendler, K.S.; Thornton, L.M.; Prescott, C.A. Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. Am. J. Psychiatry 2001, 158, 587–593. [Google Scholar] [CrossRef] [PubMed]
- McLean, C.P.; Anderson, E.R. Brave men and timid women? A review of the gender differences in fear and anxiety. Clin. Psychol. Rev. 2009, 29, 496–505. [Google Scholar] [CrossRef]
- Di Giorgio, E.; Di Riso, D.; Mioni, G.; Cellini, N. The interplay between mothers’ and children behavioral and psychological factors during COVID-19: An Italian study. Eur. Child Adolesc. Psychiatry 2021, 30, 1401–1412. [Google Scholar] [CrossRef]
- Benassi, E.; Vallone, M.; Camia, M.; Scorza, M. Women during the COVID-19 lockdown: More anxiety symptoms in women with children than without children and role of the resilience. Mediterr. J. Clin. Psychol. 2020, 8, 1–19. [Google Scholar]
- Sprang, G.; Silman, M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public 2013, 7, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Spinelli, M.; Lionetti, F.; Pastore, M.; Fasolo, M. Parents’ stress and children’s psychological problems in families facing the COVID-19 outbreak in Italy. Front. Psychol. 2020, 11, 1713. [Google Scholar] [CrossRef] [PubMed]
- Nwachukwu, I.; Nkire, N.; Shalaby, R.; Hrabok, M.; Vuong, W.; Gusnowski, A.; Surood, S.; Urichuk, L.; Greenshaw, A.J.; Agyapong, V.I.O. COVID-19 pandemic: Age-related differences in measures of stress, anxiety and depression in Canada. Int. J. Environ. Res. Public Health 2020, 17, 6366. [Google Scholar] [CrossRef] [PubMed]
- Parola, A.; Rossi, A.; Tessitore, F.; Troisi, G.; Mannarini, S. Mental health through the COVID-19 quarantine: A growth curve analysis on Italian young adults. Front. Psychol. 2020, 11, 567484. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Sun, J.; Feng, Y. How have COVID-19 isolation policies affected young people’s mental health?—Evidence from Chinese college students. Front. Psychol. 2020, 11, 1529. [Google Scholar] [CrossRef] [PubMed]
- Gavranidou, M.; Rosner, R. The weaker sex? Gender and post-traumatic stress disorder. Depress. Anxiety 2003, 17, 130–139. [Google Scholar] [CrossRef]
- Frans, Ö.; Rimmö, P.A.; Åberg, L.; Fredrikson, M. Trauma exposure and post-traumatic stress disorder in the general population. Acta Psychiatry Scand. 2005, 111, 291–299. [Google Scholar] [CrossRef]
- Olff, M. Sex and gender differences in post-traumatic stress disorder: An update. Eur. J. Psychotraumatol. 2017, 8 (Suppl. S4), 1351204. [Google Scholar] [CrossRef]
- Bandura, A.; Caprara, G.V.; Barbaranelli, C.; Gerbino, M.; Pastorelli, C. Role of affective self-regulatory efficacy in diverse spheres of psychosocial functioning. Child Dev. 2003, 74, 769–782. [Google Scholar] [CrossRef]
- Sandin, B.; Sánchez-Arribas, C.; Chorot, P.; Valiente, R.M. Anxiety sensitivity, catastrophic misinterpretations and panic self-efficacy in the prediction of panic disorder severity: Towards a tripartite cognitive model of panic disorder. Behav. Res. Ther. 2015, 67, 30–40. [Google Scholar] [CrossRef]
- Maciejewski, P.K.; Prigerson, H.G.; Mazure, C.M. Self-efficacy as a mediator between stressful life events and depressive symptoms: Differences based on history of prior depression. Br. J. Psychiatry 2000, 176, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Schönfeld, P.; Brailovskaia, J.; Bieda, A.; Zhang, X.C.; Margraf, J. The effects of daily stress on positive and negative mental health: Mediation through self-efficacy. Int. J. Clin. Health Psychol. 2016, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Southwick, S.M.; Bonanno, G.A.; Masten, A.S.; Panter-Brick, C.; Yehuda, R. Resilience definitions, theory, and challenges: Interdisciplinary perspectives. Eur. J. Psychotraumatol. 2014, 5, 25338. [Google Scholar] [CrossRef]
- Eakman, A.M.; Schelly, C.; Henry, K.L. Protective and vulnerability factors contributing to resilience in post-9/11 veterans with service-related injuries in postsecondary education. Am. J. Occup. Ther. 2016, 70, 7001260010p1–7001260010p10. [Google Scholar] [CrossRef] [PubMed]
- Lamet, A.; Szuchman, L.; Perkel, L.; Walsh, S. Risk factors, resilience, and psychological distress among holocaust and nonholocaust surviviors in the post-9/11 environment. Educ. Gerontol. 2008, 35, 32–46. [Google Scholar] [CrossRef]
- Poole, J.C.; Dobson, K.S.; Pusch, D. Do adverse childhood experiences predict adult interpersonal difficulties? The role of emotion dysregulation. Child Abuse Negl. 2018, 80, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Fornara, F.; Mosca, O.; Bosco, A.; Caffò, A.O.; Lopez, A.; Iachini, T.; Ruggiero, G.; Ruotolo, F.; Sbordone, F.L.; Ferrara, A.; et al. Space at home and psychological distress during the COVID-19 lockdown in Italy. J. Environ. Psychol. 2022, 79, 101747. [Google Scholar] [CrossRef]

| B (Stand.) | St. Err | B | t | p | |
|---|---|---|---|---|---|
| Gender | −0.09 | 0.02 | −2.11 | −4.57 | * |
| Children | 0.10 | 0.02 | 2.27 | 4.71 | * |
| Safety Out | −0.15 | 0.02 | −2.17 | −7.61 | * |
| Isolation | 0.23 | 0.02 | 2.43 | 10.89 | * |
| Trait Anxiety | 0.60 | 0.02 | 0.63 | 27.21 | * |
| B (Stand.) | St. Err | B | t | p | |
|---|---|---|---|---|---|
| Age | −0.11 | 0.02 | −0.05 | −5.64 | * |
| Gender | −0.08 | 0.02 | −1.22 | −4.34 | * |
| Safety Out | −0.07 | 0.02 | −0.68 | −3.91 | * |
| Isolation | 0.12 | 0.02 | 0.84 | 6.22 | * |
| Trait Anxiety | 0.66 | 0.02 | 0.46 | 32.11 | * |
| Time | Mean (SE) | Sex | Mean (SE) | ||
|---|---|---|---|---|---|
| (a) | State Anxiety | During | 45.77 (1.00) *1 | Male | 41.65 (1.72) |
| Female | 49.88 (1.03) | ||||
| After | 40.89 (0.98) * | Male | 38.50 (1.67) | ||
| Female | 43.27 (1.00) | ||||
| Trait Anxiety | During | 43.18 (0.95) *** | Male | 40.52 (1.63) | |
| Female | 45.84 (0.98) | ||||
| After | 42.68 (0.94) *** | Male | 40.91 (1.61) | ||
| Female | 44.45 (0.97) | ||||
| (b) | Perceived Stress | During | 18.85 (0.64) ** | Male | 16.48 (1.09) |
| Female | 21.22 (0.66) | ||||
| After | 17.64 (0.58) ** | Male | 16.33 (0.99) | ||
| Female | 18.95 (0.59) | ||||
| (c) | Feeling of Isolation | During | 2.90 (0.09) * | Male | 2.63 (0.16) |
| Female | 3.16 (0.09) | ||||
| After | 2.07 (0.09) * | Male | 1.93 (0.15) | ||
| Female | 2.20 (0.09) | ||||
| (d) | Security Inside the Home | During | 4.23 (0.06) *** | Male | 4.28 (0.10) |
| Female | 4.17 (0.06) | ||||
| After | 4.30 (0.06) *** | Male | 4.37 (0.10) | ||
| Female | 4.23 (0.06) | ||||
| Security Outside the Home | During | 2.68 (0.06) * | Male | 2.78 (0.11) | |
| Female | 2.58 (0.07) | ||||
| After | 3.14 (0.06) * | Male | 3.33 (0.09) | ||
| Female | 2.95 (0.06) | ||||
| B (Stand.) | St. Err | B | t | p | ||
|---|---|---|---|---|---|---|
| Self-efficacy | Isolation | −0.03 | 0.01 | −0.21 | −2.87 | * |
| Safety Out | 0.02 | 0.01 | 0.20 | 2.64 | ** | |
| State Anxiety | −0.88 | 0.12 | −0.49 | −7.38 | * | |
| Stress | −0.55 | 0.07 | −0.52 | −8.03 | * | |
| Safety In | 0.01 | 0.01 | 0.08 | 0.99 | 0.32 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruotolo, F.; Ruggiero, G.; Cattaneo, Z.; Arioli, M.; Candini, M.; Frassinetti, F.; Pazzaglia, F.; Fornara, F.; Bosco, A.; Iachini, T. Psychological Reactions during and after a Lockdown: Self-Efficacy as a Protective Factor of Mental Health. Int. J. Environ. Res. Public Health 2023, 20, 6679. https://doi.org/10.3390/ijerph20176679
Ruotolo F, Ruggiero G, Cattaneo Z, Arioli M, Candini M, Frassinetti F, Pazzaglia F, Fornara F, Bosco A, Iachini T. Psychological Reactions during and after a Lockdown: Self-Efficacy as a Protective Factor of Mental Health. International Journal of Environmental Research and Public Health. 2023; 20(17):6679. https://doi.org/10.3390/ijerph20176679
Chicago/Turabian StyleRuotolo, Francesco, Gennaro Ruggiero, Zaira Cattaneo, Maria Arioli, Michela Candini, Francesca Frassinetti, Francesca Pazzaglia, Ferdinando Fornara, Andrea Bosco, and Tina Iachini. 2023. "Psychological Reactions during and after a Lockdown: Self-Efficacy as a Protective Factor of Mental Health" International Journal of Environmental Research and Public Health 20, no. 17: 6679. https://doi.org/10.3390/ijerph20176679
APA StyleRuotolo, F., Ruggiero, G., Cattaneo, Z., Arioli, M., Candini, M., Frassinetti, F., Pazzaglia, F., Fornara, F., Bosco, A., & Iachini, T. (2023). Psychological Reactions during and after a Lockdown: Self-Efficacy as a Protective Factor of Mental Health. International Journal of Environmental Research and Public Health, 20(17), 6679. https://doi.org/10.3390/ijerph20176679









