Nutritional Care for Institutionalized Persons with Dementia: An Integrative Review
Abstract
:1. Introduction
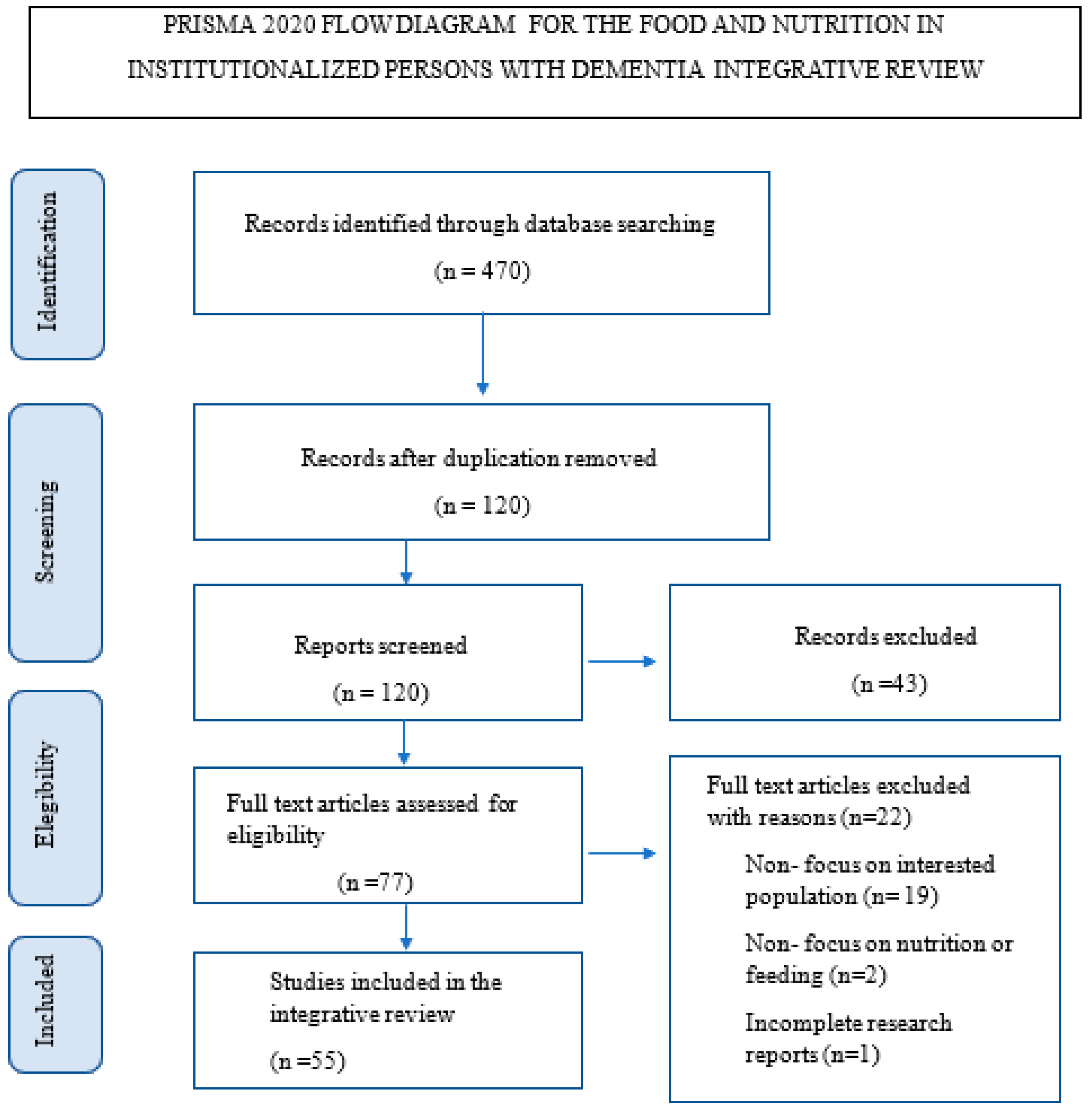
2. Materials and Methods
3. Results
3.1. Caring Assessment for Feeding and Nutrition of the Institutionalized Individuals with Dementia
3.2. Caring Interventions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Dementia. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 16 May 2022).
- Ngabirano, L.; Samieri, C.; Feart, C.; Gabelle, A.; Artero, S.; Duflos, C.; Berr, C.; Mura, T. Intake of Meat, Fish, Fruits, and Vegetables and Long-Term Risk of Dementia and Alzheimer’s Disease. J. Alzheimer’s Dis. 2019, 68, 711–722. [Google Scholar] [CrossRef] [PubMed]
- van den Brink, A.C.; Brouwer-Brolsma, E.M.; Berendsen, A.A.M.; van de Rest, O. The Mediterranean, Dietary Approaches to Stop Hypertension (DASH), and Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) Diets Are Associated with Less Cognitive Decline and a Lower Risk of Alzheimer’s Disease—A Review. Adv. Nutr. 2019, 10, 1040–1065. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Galik, E.; Boltz, M.; Nahm, E.S.; Lerner, N.; Resnick, B. Factors associated with eating performance for long-term care residents with moderate-to-severe cognitive impairment. J. Adv. Nurs. 2016, 72, 348–360. [Google Scholar] [CrossRef]
- Nell, D.; Neville, S.; Bellew, R.; O’Leary, C.; Beck, K.L. Factors affecting optimal nutrition and hydration for people living in specialised dementia care units: A qualitative study of staff caregivers’ perceptions. Australas. J. Ageing 2016, 35, E1–E6. [Google Scholar] [CrossRef] [PubMed]
- Cipriani, G.; Carlesi, C.; Lucetti, C.; Danti, S.; Nuti, A. Eating Behaviors and Dietary Changes in Patients with Dementia. Am. J. Alzheimer’s Dis. Other Dement. 2016, 31, 706–716. [Google Scholar] [CrossRef]
- Soysal, P.; Dokuzlar, O.; Erken, N.; Dost Günay, F.S.; Isik, A.T. The Relationship Between Dementia Subtypes and Nutritional Parameters in Older Adults. J. Am. Med. Dir. Assoc. 2020, 21, 1430–1435. [Google Scholar] [CrossRef]
- Martín, I.S.M.; Barato, V.P.; Oliva, S.L.; Rodríguez, M.; Yurrita, L.C.; Cabañas, M.J.C.; Rojo, S.S.; De La Calle, L.; Díaz, E.Á.; Santos, Y.Q.; et al. Body Composition, Dietary, and Gustatory Function Assessment in People with Alzheimer’s Disease. Am. J. Alzheimer’s Dis. Other Dement. 2018, 33, 508–515. [Google Scholar] [CrossRef]
- Chen, L.-L.; Li, H.; Lin, R.; Zheng, J.-H.; Wei, Y.-P.; Li, J.; Chen, P.; Chen, H.-Y. Effects of a feeding intervention in patients with Alzheimer’s disease and dysphagia. J. Clin. Nurs. 2016, 25, 699–707. [Google Scholar] [CrossRef]
- Chang, C.-C.; Lin, Y.-F.; Chiu, C.-H.; Liao, Y.-M.; Ho, M.-H.; Lin, Y.-K.; Chou, K.-R.; Liu, M.F. Prevalence and factors associated with food intake difficulties among residents with dementia. PLoS ONE 2017, 12, e0171770. [Google Scholar] [CrossRef]
- Faraday, J.; Salis, C.; Barrett, A. Equipping Nurses and Care Staff to Manage Mealtime Difficulties in People with Dementia: A Systematic Scoping Review of Training Needs and Interventions. Am. J. Speech-Lang. Pathol. 2019, 28, 717–742. [Google Scholar] [CrossRef]
- Featherstone, K.; Northcott, A.; Bridges, J. Routines of resistance: An ethnography of the care of people living with dementia in acute hospital wards and its consequences. Int. J. Nurs. Stud. 2019, 96, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Keller, H.H.; Chaudhury, H.; Pfisterer, K.J.; Slaughter, S.E. Development and Inter-Rater Reliability of the Mealtime Scan for Long-Term Care. Gerontologist 2018, 58, e160–e167. [Google Scholar] [CrossRef] [PubMed]
- Guerchet, M.; Albanese, E.; Prina, M.; Prince, M.; Siervo, M.; Acosta, D. Nutrition and Dementia: A Review of Available Research. Ph.D. Thesis, Alzheimer’s Disease International, London, UK, 2014. [Google Scholar]
- Cronin, M.A.; George, E. The Why and How of the Integrative Review. Organ. Res. Methods 2020, 26, 168–192. [Google Scholar] [CrossRef]
- Hong, Q.N.; Gonzalez-Reyes, A.; Pluye, P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). J. Eval. Clin. Pract. 2018, 24, 459–467. [Google Scholar] [CrossRef]
- Page, M.J.; E McKenzie, J.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Moher, D. Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. J. Clin. Epidemiol. 2021, 134, 103–112. [Google Scholar] [CrossRef]
- Sattar, R.; Lawton, R.; Panagioti, M.; Johnson, J. Meta-ethnography in healthcare research: A guide to using a meta-ethnographic approach for literature synthesis. BMC Health Serv. Res. 2021, 21, 50. [Google Scholar] [CrossRef]
- dos Santos, W.M.; Secoli, S.R.; de Araújo Püschel, V.A. The Joanna Briggs Institute approach for systematic reviews. Rev. Lat.-Am. Enferm. 2018, 26, e3074. [Google Scholar] [CrossRef]
- Lobiondo-Wood, G.; Haber, J. Nursing Research Methods and Critical Appraisal for Evidence-Based Practice, 9th ed.; Elsevier: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Abdelhamid, A.; Bunn, D.; Copley, M.; Cowap, V.; Dickinson, A.; Gray, L.; Howe, A.; Killett, A.; Lee, J.; Li, F.; et al. Effectiveness of interventions to directly support food and drink intake in people with dementia: Systematic review and meta-analysis. BMC Geriatr. 2016, 16, 26. [Google Scholar] [CrossRef]
- Anantapong, K.; Davies, N.; Chan, J.; McInnerney, D.; Sampson, E.L. Mapping and understanding the decision-making process for providing nutrition and hydration to people living with dementia: A systematic review. BMC Geriatr. 2020, 20, 520. [Google Scholar] [CrossRef]
- Arahata, M.; Oura, M.; Tomiyama, Y.; Morikawa, N.; Fujii, H.; Minani, S.; Shimizu, Y. A comprehensive intervention following the clinical pathway of eating and swallowing disorder in the elderly with dementia: Historically controlled study. BMC Geriatr. 2017, 17, 146. [Google Scholar] [CrossRef]
- Batchelor-Murphy, M.K.; McConnell, E.S.; Amella, E.J.; Anderson, R.A.; Bales, C.W.; Silva, S.; Barnes, A.; Beck, C.; Colon-Emeric, C.S. Experimental Comparison of Efficacy for Three Handfeeding Techniques in Dementia. J. Am. Geriatr. Soc. 2017, 65, e89–e94. [Google Scholar] [CrossRef] [PubMed]
- Batchelor-Murphy, M.; Kennerly, S.M.; Horn, S.D.; Barrett, R.; Bergstrom, N.; Boss, L.; Yap, T.L. Impact of Cognition and Handfeeding Assistance on Nutritional Intake for Nursing Home Residents. J. Nutr. Gerontol. Geriatr. 2019, 38, 262–276. [Google Scholar] [CrossRef] [PubMed]
- Benigas, J.E.; Bourgeois, M. Using Spaced Retrieval with External Aids to Improve Use of Compensatory Strategies During Eating for Persons with Dementia. Am. J. Speech-Lang. Pathol. 2016, 25, 321–334. [Google Scholar] [CrossRef] [PubMed]
- Bunn, D.K.; Abdelhamid, A.; Copley, M.; Cowap, V.; Dickinson, A.; Howe, A.; Killett, A.; Poland, F.; Potter, J.F.; Richardson, K.; et al. Effectiveness of interventions to indirectly support food and drink intake in people with dementia: Eating and Drinking Well IN dementiA (EDWINA) systematic review. BMC Geriatr. 2016, 16, 89. [Google Scholar] [CrossRef] [PubMed]
- Herke, M.; Fink, A.; Langer, G.; Wustmann, T.; Watzke, S.; Hanff, A.-M.; Burckhardt, M. Environmental and behavioural modifications for improving food and fluid intake in people with dementia. Cochrane Database Syst. Rev. 2018, 2018, CD011542. [Google Scholar] [CrossRef] [PubMed]
- Johansson, L.; Björklund, A.; Sidenvall, B.; Christensson, L. Staff views on how to improve mealtimes for elderly people with dementia living at home. Dementia 2017, 16, 835–852. [Google Scholar] [CrossRef]
- Jung, D.; De Gagne, J.C.; Lee, M.; Lee, H.; Lee, K.; Choi, E.; Chung, J. Feasibility of a Mobile Meal Assistance Program for Direct Care Workers in Long-Term Care Facilities in South Korea. Clin. Interv. Aging 2020, 15, 2019–2029. [Google Scholar] [CrossRef]
- Kawaharada, R.; Sugimoto, T.; Matsuda, N.; Tsuboi, Y.; Sakurai, T.; Ono, R. Impact of loss of independence in basic activities of daily living on caregiver burden in patients with Alzheimer’s disease: A retrospective cohort study. Geriatr. Gerontol. Int. 2019, 19, 1243–1247. [Google Scholar] [CrossRef]
- Keller, H.H. Improving food intake in persons living with dementia. Ann. N. Y. Acad. Sci. 2016, 1367, 3–11. [Google Scholar] [CrossRef]
- Kobayashi, N.; Soga, Y.; Maekawa, K.; Kanda, Y.; Kobayashi, E.; Inoue, H.; Kanao, A.; Himuro, Y.; Fujiwara, Y. Prevalence of oral health-related conditions that could trigger accidents for patients with moderate-to-severe dementia. Gerodontology 2017, 34, 129–134. [Google Scholar] [CrossRef]
- Leah, V. Supporting people with dementia to eat. Nurs. Older People 2016, 28, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Zhao, Y.; Wang, Y.; Wang, Z. Overview of systematic reviews: Effectiveness of non-pharmacological interventions for eating difficulties in people with dementia. J. Adv. Nurs. 2020, 76, 2830–2848. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Sun, D.; Zhang, X.; Li, H.; Zhao, Y.; Ma, D.; Li, Z.; Sun, J. Informal dementia caregivers’ experiences and perceptions about mealtime care: A qualitative evidence synthesis. J. Adv. Nurs. 2020, 76, 3317–3328. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Jao, Y.L.; Williams, K. The association of eating performance and environmental stimulation among older adults with dementia in nursing homes: A secondary analysis. Int. J. Nurs. Stud. 2017, 71, 70–79. [Google Scholar] [CrossRef]
- Liu, W.; Jao, Y.; Williams, K. Factors influencing the pace of food intake for nursing home residents with dementia: Resident characteristics, staff mealtime assistance and environmental stimulation. Nurs. Open 2019, 6, 772–782. [Google Scholar] [CrossRef]
- Liu, Q.; Guo, J.; Hu, L.; Veronese, N.; Smith, L.; Yang, L.; Cao, C. Association between Intake of Energy and Macronutrients and Memory Impairment Severity in US Older Adults, National Health and Nutrition Examination Survey 2011–2014. Nutrients 2020, 12, 3559. [Google Scholar] [CrossRef]
- Liu, W.; Tripp-Reimer, T.; Williams, K.; Shaw, C. Facilitators and barriers to optimizing eating performance among cognitively impaired older adults: A qualitative study of nursing assistants’ perspectives. Dementia 2020, 19, 2090–2113. [Google Scholar] [CrossRef]
- Liu, W.; Batchelor, M.; Williams, K. Ease of use, feasibility and inter-rater reliability of the refined Cue Utilization and Engagement in Dementia (CUED) mealtime video-coding scheme. J. Adv. Nurs. 2020, 76, 3609–3622. [Google Scholar] [CrossRef]
- Liu, T.; Li, N.; Hou, Z.; Liu, L.; Gao, L.; Wang, L.; Tan, J. Nutrition and exercise interventions could ameliorate age-related cognitive decline: A meta-analysis of randomized controlled trials. Aging Clin. Exp. Res. 2021, 33, 1799–1809. [Google Scholar] [CrossRef]
- Marples, O.; Baldwin, C.; Weekes, C.E. The effect of nutrition training for health care staff on learner and patient outcomes in adults: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2017, 106, 284–310. [Google Scholar] [CrossRef]
- McGrattan, A.M.; McEvoy, C.T.; Vijayakumar, A.; Moore, S.E.; Neville, C.E.; McGuinness, B.; McKinley, M.C.; Woodside, J.V. A mixed methods pilot randomised controlled trial to develop and evaluate the feasibility of a Mediterranean diet and lifestyle education intervention ‘THINK-MED’ among people with cognitive impairment. Pilot Feasibility Stud. 2021, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.L.; Holmes, J.; Brooks, C. Nutrition and dementia care: Developing an evidence-based model for nutritional care in nursing homes. BMC Geriatr. 2017, 17, 55. [Google Scholar] [CrossRef] [PubMed]
- Palese, A.; Bressan, V.; Kasa, T.; Meri, M.; Hayter, M.; Watson, R. Interventions maintaining eating Independence in nursing home residents: A multicentre qualitative study. BMC Geriatr. 2018, 18, 292. [Google Scholar] [CrossRef]
- Palese, A.; Bressan, V.; Hayter, M.; Watson, R. Enhancing independent eating among older adults with dementia: A scoping review of the state of the conceptual and research literature. BMC Nurs. 2020, 19, 32. [Google Scholar] [CrossRef] [PubMed]
- Painter, V.; le Couteur, D.; Waite, L. Texture-modified food and fluids in dementia and residential aged care facilities. Clin. Interv. Aging 2017, 12, 1193–1203. [Google Scholar] [CrossRef]
- Park, M.; Song, J.-A.; Lee, M.; Jeong, H.; Lim, S.; Lee, H.; Kim, C.-G.; Kim, J.S.; Kim, K.S.; Lee, Y.W.; et al. National study of the nutritional status of Korean older adults with dementia who are living in long-term care settings. Jpn. J. Nurs. Sci. 2018, 15, 318–329. [Google Scholar] [CrossRef]
- Poscia, A.; Milovanovic, S.; La Milia, D.I.; Duplaga, M.; Grysztar, M.; Landi, F.; Moscato, U.; Magnavita, N.; Collamati, A.; Ricciardi, W. Effectiveness of nutritional interventions addressed to elderly persons: Umbrella systematic review with meta-analysis. Eur. J. Public Health 2018, 28, 275–283. [Google Scholar] [CrossRef]
- Prizer, L.P.; Zimmerman, S. Progressive Support for Activities of Daily Living for Persons Living with Dementia. Gerontologist 2018, 58 (Suppl. S1), S74–S87. [Google Scholar] [CrossRef]
- Quinn, C.; Toms, G. Influence of Positive Aspects of Dementia Caregiving on Caregivers’ Well-Being: A Systematic Review. Gerontologist 2018, 59, e584–e596. [Google Scholar] [CrossRef]
- Saarela, R.K.T.; Muurinen, S.; Suominen, M.H.; Savikko, N.N.; Soini, H.; Pitkälä, K.H. Changes in malnutrition and quality of nutritional care among aged residents in all nursing homes and assisted living facilities in Helsinki 2003–2011. Arch. Gerontol. Geriatr. 2017, 72, 169–173. [Google Scholar] [CrossRef]
- Salminen, K.S.; Suominen, M.H.; Kautiainen, H.; Roitto, H.M.; Pitkala, K.H. Energy Intake and Severity of Dementia Are Both Associated with Health-Related Quality of Life among Older Long-Term Care Residents. Nutrients 2019, 11, 2261. [Google Scholar] [CrossRef]
- Shatenstein, B.; Kergoat, M.J.; Reid, I. Outcome of a Targeted Nutritional Intervention Among Older Adults with Early-Stage Alzheimer’s Disease: The Nutrition Intervention Study. J. Appl. Gerontol. 2017, 36, 782–807. [Google Scholar] [CrossRef]
- Sheppard, C.L.; McArthur, C.; Hitzig, S.L. A Systematic Review of Montessori-Based Activities for Persons with Dementia. J. Am. Med. Dir. Assoc. 2016, 17, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Simmons, S.F.; Coelho, C.S.; Sandler, A.; Schnelle, J.F. A Quality Improvement System to Manage Feeding Assistance Care in Assisted-Living. J. Am. Med. Dir. Assoc. 2018, 19, 262–269. [Google Scholar] [CrossRef]
- Snyder, S.A.; Vitaliano, P.P. Caregiver Psychological Distress: Longitudinal Relationships with Physical Activity and Diet. Am. J. Alzheimer’s Dis. Other Dement. 2020, 35, 153331752090455. [Google Scholar] [CrossRef] [PubMed]
- Soininen, H.; Solomon, A.; Visser, P.J.; Hendrix, S.B.; Blennow, K.; Kivipelto, M.; Hartmann, T.; Hallikainen, I.; Hallikainen, M.; Helisalmi, S.; et al. 24-month intervention with a specific multinutrient in people with prodromal Alzheimer’s disease (LipiDiDiet): A randomised, double-blind, controlled trial. Lancet Neurol. 2017, 16, 965–975. [Google Scholar] [CrossRef] [PubMed]
- Soininen, H.; Solomon, A.; Visser, P.J.; Hendrix, S.B.; Blennow, K.; Kivipelto, M.; Hartmann, T.; The LipiDiDiet Clinical Study Group. 36-month LipiDiDiet multinutrient clinical trial in prodromal Alzheimer’s disease. Alzheimer’s Dement. 2021, 17, 29–40. [Google Scholar] [CrossRef]
- Takada, K.; Tanaka, K.; Hasegawa, M.; Sugiyama, M.; Yoshiike, N. Grouped factors of the ‘SSADE: Signs and symptoms accompanying dementia while eating’ and nutritional status-An analysis of older people receiving nutritional care in long-term care facilities in Japan. Int. J. Older People Nurs. 2017, 12, e12149. [Google Scholar] [CrossRef]
- Tangvik, R.J.; Bruvik, F.K.; Drageset, J.; Kyte, K.; Hunskår, I. Effects of oral nutrition supplements in persons with dementia: A systematic review. Geriatr. Nurs. 2021, 42, 117–123. [Google Scholar] [CrossRef]
- Tombini, M.; Sicari, M.; Pellegrino, G.; Ursini, F.; Insardá, P.; di Lazzaro, V. Nutritional Status of Patients with Alzheimer’s Disease and Their Caregivers. J. Alzheimer’s Dis. 2016, 54, 1619–1627. [Google Scholar] [CrossRef]
- Watanabe, K.; Umegaki, H.; Huang, C.; Martins, B.A.; Asai, A.; Kanda, S.; Nomura, H.; Kuzuya, M. Association between dysphagia risk and unplanned hospitalization in older patients receiving home medical care. Geriatr. Gerontol. Int. 2019, 19, 977–981. [Google Scholar] [CrossRef] [PubMed]
- Whitelock, E.; Ensaff, H. On Your Own: Older Adults’ Food Choice and Dietary Habits. Nutrients 2018, 10, 413. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Morrison, J.M.; Dunn-Ridgeway, H.; Vucea, V.; Iuglio, S.; Keller, H. Mixed methods developmental evaluation of the CHOICE program: A relationship-centred mealtime intervention for long-term care. BMC Geriatr. 2018, 18, 277. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, A. (Ed.) Oxford Dictionary of English; Oxford University Press: New York, NY, USA, 2010. [Google Scholar]
- Bronfenbrenner, U. Toward an experimental ecology of human development. Am. Psychol. 1977, 32, 513. [Google Scholar] [CrossRef]
- Crist, J.D.; Lacasse, C.; Phillips, L.R.; Liu, J. Lawton’s theory of Person-Environment Fit: Theoretical foundations for detecting tipping points. Innov. Aging 2019, 3 (Suppl. S1), S597. [Google Scholar] [CrossRef]

| Author | Year | Title | Country | Method | Evidence | Main Results |
|---|---|---|---|---|---|---|
| Abdelhamid et al. [21] | 2016 | Effectiveness of interventions to directly support food and drink intake in people with dementia: systematic review and meta-analysis. | UK | Systematic review: n = 43. | 1 | They did not find definitive evidence of effectiveness, or lack of it on specific interventions. There is a need for more robust research. |
| Anantapong et al. [22] | 2020 | Mapping and understanding the decision-making process for providing nutrition and hydration to people living with dementia: a systematic review. | UK | Systematic review: n = 45. | 1 | Making decisions regarding nutrition and hydration for people living with dementia is not a linear process and demands a shared and stepwise manner support. |
| Arahata et al. [23] | 2017 | A comprehensive intervention following the clinical pathway of eating and swallowing disorder in the elderly with dementia: historically controlled study. | Japan | This is a single-arm, non-randomized trial: n = 90 patients. | 3 | The comprehensive geriatric assessment with multidisciplinary interventions enhanced dementia patients’ eating functional status. |
| Batchelor et al. [24] | 2017 | Experimental Comparison of Efficacy for Three Handfeeding Techniques in Dementia. | USA | Prospective pilot study with subjects’ experimental Latin square design and randomization to one of three handfeeding techniques: n = 30. | 2 | The 3 direct-, over-, and under-hand techniques were time neutral. Under- and direct-hand techniques helped to better diminish meal intake, feeding problematic behaviors. |
| Batchelor-M. et al. [25] | 2019 | Impact of Cognition and Handfeeding Assistance on Nutritional Intake for Nursing Home Residents. | USA | Secondary analysis research: n = 786 residents with and without dementia. | 6 | People with dementia that need assistance have a significantly lower food intake and therefore a higher risk of malnutrition. Snacks helped them increase their caloric intake. |
| Benigas, et. al. [26] | 2016 | Using Spaced Retrieval with External Aids to Improve Use of Compensatory Strategies During Eating for Persons with Dementia. | USA | Evaluative study on the effects of teaching from a baseline of compensatory swallowing behaviors (i.e., chin retraction): n = 5 patients. | 4 | Visual aid training strategies applied within an adapted context helped balancing 2–3 compensatory swallowing behaviors in each participant. |
| Bunn, et. al. [27] | 2016 | Effectiveness of interventions to indirectly support food and drink intake in people with dementia: Eating and Drinking Well IN dementia (EDWINA) systematic review. BMC geriatrics, 16(1), 1–21. | UK | Systematic review: n = 51 studies including 56 interventions. | 1 | There are several indirect interventions that may have a promising future to improve, maintain, or facilitate food and drink intake in people with cognitive impairment. |
| Chang et al. [10] | 2017 | Prevalence and factors associated with food intake difficulties among residents with dementia. | Taiwan | Correlational study: n = 213 residents with dementia. | 4 | The physical function and dining environment may be associated with food intake difficulties in people with dementia. |
| Chen et al. [9] | 2016 | Effects of a feeding intervention in patients with Alzheimer’s disease and dysphagia. | China | Prospective study: n = 30 Alzheimer’s patients with dysphagia. | 4 | Eating and feeding in patients with Alzheimer’s improved with a feeding intervention model that included patient, environment, food, and utensils preparation, as well as appropriate assistance, patient monitoring, psychological care, and nursing care after eating. |
| Cipriani et al. [6] | 2016 | Eating Behaviors and Dietary Changes in Patients with Dementia. | Italy | Literature review: n = 89. | 5 | Most dementia patients have several feeding and eating problems associated with their cognitive impairment, metabolic or neurochemical condition, or available care. |
| Faraday et al. [11] | 2019 | Equipping nurses and care staff to manage mealtime difficulties in people with dementia: A systematic scoping review of training needs and interventions. | UK | Systematic scoping review: n = 76. | 5 | Training needs are especially necessary to manage uncertainty. Training interventions on dysphagia management and communication are necessary. |
| Featherstone et al. [12] | 2019 | Routines of resistance: an ethnography of the care of people living with dementia in acute hospital wards and its consequences. | UK | Ethnography within 5 hospitals. | 6 | Cycles of resistance in response to organizationally imposed care schedules can result in poor care experiences for patients and lead to emotional and physical exhaustion for staff. More research is needed on how institutional goals can be better aligned to dementia patients’ needs. |
| Herke, M. [28] | 2018 | Environmental and behavioral modifications for improving food and fluid intake in people with dementia. | Germany | Systematic review: n = 9 studies (1502 patients with dementia). | 1 | Verbal and tactile communication from the caregiver can affect the nutrition of dementia patients by encouraging food intake. Objective measures of nutrition are indispensable to assess the effect of clinical trials. The environment is relevant as an external stimulus for the nutrition of the elderly person with dementia. The evidence on environmental interventions is weak. |
| Johansson et.al. [29] | 2017 | Staff views on how to improve mealtimes for elderly people with dementia living at home. | Sweden | Descriptive qualitative study with 4 focal groups. Participants included 22 workers that care for people with dementia. | 6 | The quality of meals for dementia patients can be improved with a person-centered approach. It is necessary to promote autonomy and maintain a family environment at mealtimes. It is also necessary to share staff experiences. |
| Jung et al. [30] | 2020 | Feasibility of a Mobile Meal Assistance Program for Direct Care Workers in Long-Term Care Facilities in South Korea. | S. Korea | Mixed study that follows 23 dyads of older adults with dementia and their attendants from a long-term care facility in South Korea. | 4 | The APP intervention may be useful in the long-term care of people with dementia, especially for formal caregivers who need training in meal attendant skills. |
| Kawaharada et al. [31] | 2019 | Impact of loss of independence in basic activities of daily living on caregiver burden in patients with Alzheimer’s disease: A retrospective cohort study. | Japan | Retrospective cohort study of people with Alzheimer’s disease: n = 117. | 4 | The turndown in functionality in activities of daily living related to bathing and feeding people with dementia are risk factors for the caregiver burden. |
| Keller et al. [13] | 2018 | Development and Inter-Rater Reliability of the Mealtime Scan for Long-Term Care. | Canada | Methodological study: n = 82 (in different dining rooms in 32 long-term care facilities). | 6 | The MTS scale showed facial validity and reliability to assess the physical and psychosocial environments in shared dining rooms during meals. It is necessary to test its constructs. |
| Keller, H. [32] | 2016 | Improving food intake in persons living with dementia. | Canada | Narrative review of the literature: n = 74 studies. | 5 | Malnutrition in people with dementia is associated with poor food intake. Modifying the psychosocial aspects during mealtimes may improve food intake and quality of life. |
| Kobayashi et al. [33] | 2017 | Prevalence of oral health-related conditions that could trigger accidents for patients with moderate-to-severe dementia. | Japan | Descriptive quantitative study: n = 92 dementia patients with oral problems. | 5 | Patients with moderate-to-severe dementia have a high prevalence of oral health conditions that increase the risk of accidents during mealtimes. |
| Leah, V. [34] | 2016 | Supporting people with dementia to eat. | UK | Systematic review: n = 22 studies. | 1 | Recommended interventions focused on education, environmental changes, routine management, and feeding support. There is a need to ensure that staff carry out individual assessments to identify people who are having difficulty eating and to guarantee that they have enough time to eat. |
| Li et al. [35] | 2020 | Overview of systematic reviews: Effectiveness of non-pharmacological interventions for eating difficulties in people with dementia. | China | Umbrella review: n = 18 systematic reviews. | 1 | A review of non-pharmacological interventions provides weak evidence that could help caregivers select the most effective strategies for coping with feeding difficulties and preventing adverse events. |
| Li et al. [36] | 2020 | Informal dementia caregivers’ experiences and perceptions about mealtime care: A qualitative evidence synthesis. | China | Metasynthesis: n = 10 articles. | 5 | Caregivers need to be knowledgeable and informed about services related to the feeding of people with dementia to care for them appropriately. The experiences and clinical skills of informal caregivers are relevant to improve the quality of mealtime care. |
| Liu et al. [4] | 2016 | Factors associated with eating performance for long-term care residents with moderate-to-severe cognitive impairment. | USA | Secondary analysis of data from 192 residents in 8 institutions. | 6 | Interventions aimed at reducing the impact of cognitive impairment and improving the physical capacity of residents are required to optimize feeding performance. |
| Liu et al. [37] | 2017 | The association of eating performance and environmental stimulation among older adults with dementia in nursing homes: A secondary analysis. | USA | Secondary analysis of videos taken from residents at lunchtime. There are 36 videos, 15 residents with dementia, and 19 nursing assistants. | 6 | An association was found between the dietary performance of elderly people with advanced dementia and associated comorbidities. Environmental stimulation should be personalized to respond to their unique conditions and preferences. |
| Liu et al. [38] | 2019 | Factors influencing the pace of food intake for nursing home residents with dementia: Resident characteristics, staff mealtime assistance and environmental stimulation. | USA | A secondary analysis: n = 36 videos. | 6 | Factors influencing mealtime pace include being male, having more interactions, having physical and visual assistance, and a better performance during feeding. |
| Liu et al. [39] | 2020 | Association between Intake of Energy and Macronutrients and Memory Impairment Severity in US Older Adults, National Health and Nutrition Examination Survey 2011–2014. | USA China Italy UK Canada | Survey research: n = 3623 participants older than 60 years. | 4 | The authors related the intake of a healthy diet with better cognitive capacity, pointing out that people who consume more carbohydrates and sugars have a higher risk of having memory impairment than those who consume more protein-based energy. |
| Liu et al. [40] | 2020 | Facilitators and barriers to optimizing eating performance among cognitively impaired older adults: A qualitative study of nursing assistants’ perspectives. | USA | Descriptive qualitative study in 2 hospitals with 6 focal groups that included 23 nurses. | 6 | The main barriers and facilitators of feeding performance are related to caregivers. According to them, these are related to physical, social, and cultural aspects of the environment, as well as to the norms of the institution. Barriers include lack of preparation and training, competing work demands, time pressure, and frustration. Facilitators involve preparation, motivational, technical, informational, and instrumental assistance. It is recommended that programs include staff training emphasizing individualized care. |
| Liu et al. [41] | 2020 | Ease of use, feasibility and inter-rater reliability of the refined Cued Utilization and Engagement in Dementia (CUED) mealtime video-coding scheme. | USA | Methodological study with a secondary analysis of 110 observations of video recordings: n = 25 residents and 29 assistants. | 6 | The CUED scheme for analyzing videos of food intake in interaction with the person and the dementia patient–caregiver dyad was preliminarily valid, reliable, and useful. |
| Liu et al. [42] | 2021 | Nutrition and exercise interventions could ameliorate age-related cognitive decline: a meta-analysis of randomized controlled trials. | USA | Systematic review and meta-analysis: n = 6 clinical randomized control trials with 1039 participants. | 1 | There is a beneficial effect of proper nutrition combined with exercise on the overall cognitive function of individuals. |
| Marples et al. [43] | 2017 | The effect of nutrition training for health care staff on learner and patient outcomes in adults: a systematic review and meta-analysis. | UK | Systematic review and meta-analysis of clinical trials of staff training: n = 24 studies. | 1 | Despite the weak evidence, it can be stated that nutrition training can benefit the knowledge, attitude, and behavior of caregivers of the vulnerable elderly with effects on the nutritional intake of patients with dementia. |
| Martin et al. [8] | 2018 | Body composition, dietary, and gustatory function assessment in people with Alzheimer’s disease. | Spain | Descriptive comparative, cross-sectional cohort study: n = 75 people with Alzheimer’s disease compared with 267 healthy older adults. | 4 | People with Alzheimer’s disease had significant differences. They had lower body mass indexes, more hours of sleep, greater alteration in the perception of sweet and salty tastes, and less adherence to exercise and to the Mediterranean diet. These differential factors increase the risk of malnutrition in those with Alzheimer’s disease. |
| McGrattan et al. [44] | 2021 | A mixed methods pilot randomized controlled trial to develop and evaluate the feasibility of a Mediterranean diet and lifestyle education intervention ‘THINK-MED’ among people with cognitive impairment. | UK | A mixed methods pilot randomized controlled trial: n = 20 participants. | 2 | The authors present the development and preliminary evaluation of the Think-MED intervention, which strives for adherence to a Mediterranean diet. The results are not conclusive. |
| Murphy et al. [45] | 2017 | Nutrition and dementia care: developing an evidence-based model for nutritional care in nursing homes. | UK | Qualitative study with 9 focus groups. | 6 | The authors present an empirical model with an overall theme of person-centered nutritional care and a collaborative approach. They add to this view the availability of food and drink, tools, resources, contact, interaction when eating and drinking, participation in activities, and consistency of care and information. |
| Nell et al. [5] | 2016 | Factors affecting optimal nutrition and hydration for people living in specialized dementia care units: A qualitative study of staff caregivers’ perception. | New Zealand | Descriptive qualitative study: n = 11 caregivers. | 6 | The factors that affect nutrition and hydration in people living with dementia are complex, inter-related, and include both personal and environmental aspects. Therefore, both aspects included must be considered within the care given to these people. |
| Palese et al. [46] | 2018 | Interventions maintaining eating Independence in nursing home residents: a multicenter qualitative study. | Italy | Qualitative descriptive multicenter study. Participants included 54 health professionals interviewed in 13 focus groups. | 6 | The experience of caring for people with dementia of the study participants adds new interventions at mealtime in addition to those already described. Documented interventions include individualized care, environmental, and social interaction. |
| Palese et al. [47] | 2020 | Enhancing independent eating among older adults with dementia: a scoping review of the state of the conceptual and research literature. | Italy UK | Scoping review with 17 documents included. | 5 | Recommended interventions to improve the diet of people with dementia must have an explicit conceptual framework and integrate individual, social, cultural, and environmental factors. When evaluating the effectiveness of these interventions, dietary performance, clinical outcomes, and adverse events should be considered. |
| Painter et al. [48] | 2017 | Texture-modified food and fluids in dementia and residential aged care facilities. | Australia | Literature review with 22 studies. | 5 | Fluoroscopy showed that texture-modified food reduced the risk of aspiration in people with dementia. These meals did not reduce clinical aspiration or pneumonia incidence and were associated with lower daily energy and fluid intake. Their adherence was variable. |
| Park et al. [49] | 2018 | National study of the nutritional status of Korean older adults with dementia who are living in long-term care settings. | Korea | Secondary analysis of data from the Nationwide Survey on Dementia Care in Korea: n = 3474 participants. | 6 | The nutritional status of older adults with dementia living in long-term care facilities in South Korea was found to be poor and associated with multiple factors. The malnutrition rate was 38% and the risk of this was 55%. Most of the malnourished older adult population with dementia was institutionalized and suffered from cognitive impairment, with functional dependence and associated comorbidities. |
| Poscia et al. [50] | 2018 | Effectiveness of nutritional interventions addressed to elderly persons: umbrella systematic review with meta-analysis. | Italy Poland | Umbrella systematic review with meta-analysis: 28 articles. | 2 | The nutrition of the elderly requires a preventive approach to improve their quality of life. Personalized nutritional interventions are suggested that consider functional conditions and cognitive status and are supported by solid evidence, such as vitamin D supplementation that helps prevent falls and fractures. In the same way, they suggest oral supplements and protein-based formulas that reduce the risk of malnutrition and improve weight. |
| Prizer et al. [51] | 2018 | Progressive Support for Activities of Daily Living for Persons Living with Dementia. | USA | Review of the gray literature: n = 59 references. | 6 | Person-centered care is recommended in which dementia is considered to require progressive support as functionality is lost. Care should consider the tastes and preferences of the person. Simple instructions are easier to follow. It is necessary to keep in mind the respect for dignity, try to preserve autonomy, respect customs, know the personal health situation, monitor the environment considering the necessary adaptations, and the characteristics of food and drinks and interaction at mealtime. |
| Quinn et al. [52] | 2019 | Influence of Positive Aspects of Dementia Caregiving on Caregivers’ Well-Being: A Systematic Review. | UK | Systematic review: n = 53 studies. | 5 | Identification of positive aspects of dementia care is associated with better caregiver well-being. Therefore, it is necessary to develop approaches and measures to promote them. Longitudinal studies are also required, as these experiences may change over time. |
| Saarela et al. [53] | 2017 | Changes in malnutrition and quality of nutritional care among aged residents in all nursing homes and assisted living facilities in Helsinki 2003–2011. | Finland | Retrospective observational study 2003 (n = 1987), in 2007 (n = 1377), in 2011 (n = 1576), and (4) in 2011 (n = 1585). | 4 | Institutionalized residents are at a higher risk of presenting nutritional problems. Institutions must improve their efforts to provide better nutritional care to the elderly. |
| Salminen et al. [54] | 2019 | Energy Intake and Severity of Dementia Are Both Associated with Health-Related Quality of Life among Older Long-Term Care Residents. | Finland | Descriptive correlational: n = 583 residents. | 4 | Energy intake has a correlation with HRQL in people with dementia. There is a positive correlation between these two variables, especially in the dimensions of mobility and daily activities in people with mild and moderate dementia, but not with those who have severe dementia. |
| Shatenstein et al. [55] | 2017 | Outcome of a Targeted Nutritional Intervention Among Older Adults with Early-Stage Alzheimer’s Disease: The Nutrition Intervention Study. | Canada | Intervention study: n = 67 dyads. Intervention group: n = 34 dyads and control group: n = 33. | 3 | The results show a higher intake of fat, energy, protein, and calcium in the intervention group, which improves body weight and muscle strength compared with the control group. Long-term follow-up is required to verify that these results are maintained over time. |
| Sheppard et al. [56] | 2016 | A Systematic Review of Montessori-Based Activities for Persons with Dementia. | Canada | Systematic review: n = 14 articles. | 5 | The results show the benefits of Montessori-based activities on eating behaviors but not on cognitive processes in people with dementia. Given the variety of the characteristics of the interventions, it is necessary to standardize the approach in future studies in order to analyze their benefits in the long term. |
| Simmons et al. [57] | 2018 | A Quality Improvement System to Manage Feeding Assistance Care in Assisted-Living. | USA | Observational study with n = 53 residents. | 6 | The implementation of the system to improve the quality of assistance during and between meals to institutionalized people with dementia showed positive results, evidenced in a reduction in weight loss. |
| Snyder et al. [58] | 2020 | Caregiver Psychological Distress: Longitudinal Relationships with Physical Activity and Diet. | USA | Correlational study: n = 122 caregivers of spouses with Alzheimer’s disease, 117 non-caregivers. | 4 | The results of this study highlight the effect of hours of care for people with Alzheimer’s and the psychological distress related to the health behaviors of caregivers. |
| Soininen et al. [59] | 2017 | 24-month intervention with a specific multinutrient in people with prodromal Alzheimer’s disease (LipiDiDiet): a randomized, double-blind, controlled trial. | Finland Sweden Netherlands USA Germany | RCT n = 311 with individuals with prodromal Alzheimer’s disease. | 2 | The Fortasyn Connect intervention did not show a significant effect on the neurocognitive functions of the intervention group when compared to the control group. These researchers found group differences related to disease progression in cognitive and hippocampal function and cortical atrophy. Studies with larger sample sizes and the determination of a more sensitive endpoint in people with predementia are required. |
| Soininen, et al. [60] | 2021 | 36-month LipiDiDiet multinutrient clinical trial in prodromal Alzheimer’s disease. | RCT: n = 311 with individuals with prodromal Alzheimer’s disease. | 2 | A period of 36 months’ follow-up showed the benefits of the Fortasyn Connect multinutrient intervention. The results show that the process of cognitive deterioration, functionality, and brain atrophy in people with Alzheimer’s disease slowed down. These results indicate that the benefits of the intervention increased with long-term use. | |
| Takada et al. [61] | 2017 | Grouped factors of the ‘SSADE: signs and symptoms accompanying dementia while eating and nutritional status—An analysis of older people receiving nutritional care in long-term care facilities in Japan. | Japan | Methodological research: n = 259. | 6 | The results show that the four factors measured by the SSADE (hypoactivity, hyperactivity, obsession, aberrant behaviors) are related to nutritional status and have acceptable factorial validity. The first three factors are negatively correlated with BMI, and aberrant behaviors are positively correlated with dietary intake. |
| Tangvik et al. [62] | 2021 | Effects of oral nutrition supplements in persons with dementia: A systematic review. | Norway | Systematic review: n = 10 studies. | 5 | The intake of Oral Nutritional Supplements improves the nutritional status of people with dementia, which translates to an increase in body weight, muscle mass, and nutritional biomarkers. Studies do not show the impact of these supplements on the cognitive and functional level. |
| Tombini et al. [63] | 2016 | Nutritional Status of Patients with Alzheimer’s Disease and Their Caregivers. | Italy Canada | Descriptive: n = 90. | 6 | The results show a high prevalence of malnutrition in patients with Alzheimer’s disease associated with impaired functionality. In the caregivers group, 23% had malnutrition and 41.1% were at risk. This situation is associated with age, functionality, educational level, and cognitive status. It is imperative to establish nutrition education programs and policies to promote the nutrition of patients and caregivers. |
| Watanabe et al. [64] | 2019 | Association between dysphagia risk and unplanned hospitalization in older patients receiving home medical care. | Japan Taiwan Australia | Secondary analysis: n = 128. | 6 | The results of this study show that it is possible to predict the risk of unexpected hospitalization in older adults when they are at risk of dysphagia, hence, the importance of determining this risk in all home-care patients. |
| Whitelock et al. [65] | 2018 | On your own: older adults’ food choice and dietary habits. | UK | Qualitative focus groups: n = 30. | 6 | The authors identified changes associated with age, access to food, feeding on their own, and relationship with food, with 12 subthemes, which affect the acquisition and preparation of food and eating habits. Loneliness is an aspect that affects eating habits. It is important to develop policies and programs that favor the acquisition of food and opportunities for eating in the company of others. |
| Wu et al. [66] | 2018 | Mixed methods developmental evaluation of the CHOICE program: a relationship-centered mealtime intervention for long-term care. | Canada | Mixed methods research: n = 64 residents, 25 care staff/home management. | 6 | Participants in this study consider that the CHOICE (Connecting, Honoring dignity, Offering support, supporting Identity, Creating opportunities, and Enjoyment) multicomponent intervention is an appropriate strategy for managing mealtime challenges. The experiences with its application during meals were satisfactory. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreno-Fergusson, M.E.; Caez-Ramírez, G.R.; Sotelo-Díaz, L.I.; Sánchez-Herrera, B. Nutritional Care for Institutionalized Persons with Dementia: An Integrative Review. Int. J. Environ. Res. Public Health 2023, 20, 6763. https://doi.org/10.3390/ijerph20186763
Moreno-Fergusson ME, Caez-Ramírez GR, Sotelo-Díaz LI, Sánchez-Herrera B. Nutritional Care for Institutionalized Persons with Dementia: An Integrative Review. International Journal of Environmental Research and Public Health. 2023; 20(18):6763. https://doi.org/10.3390/ijerph20186763
Chicago/Turabian StyleMoreno-Fergusson, María Elisa, Gabriela Rabe Caez-Ramírez, Luz Indira Sotelo-Díaz, and Beatriz Sánchez-Herrera. 2023. "Nutritional Care for Institutionalized Persons with Dementia: An Integrative Review" International Journal of Environmental Research and Public Health 20, no. 18: 6763. https://doi.org/10.3390/ijerph20186763
APA StyleMoreno-Fergusson, M. E., Caez-Ramírez, G. R., Sotelo-Díaz, L. I., & Sánchez-Herrera, B. (2023). Nutritional Care for Institutionalized Persons with Dementia: An Integrative Review. International Journal of Environmental Research and Public Health, 20(18), 6763. https://doi.org/10.3390/ijerph20186763





