Nutritional Considerations for Bladder Storage Conditions in Adult Females
Abstract
:1. Introduction
2. Materials and Methods
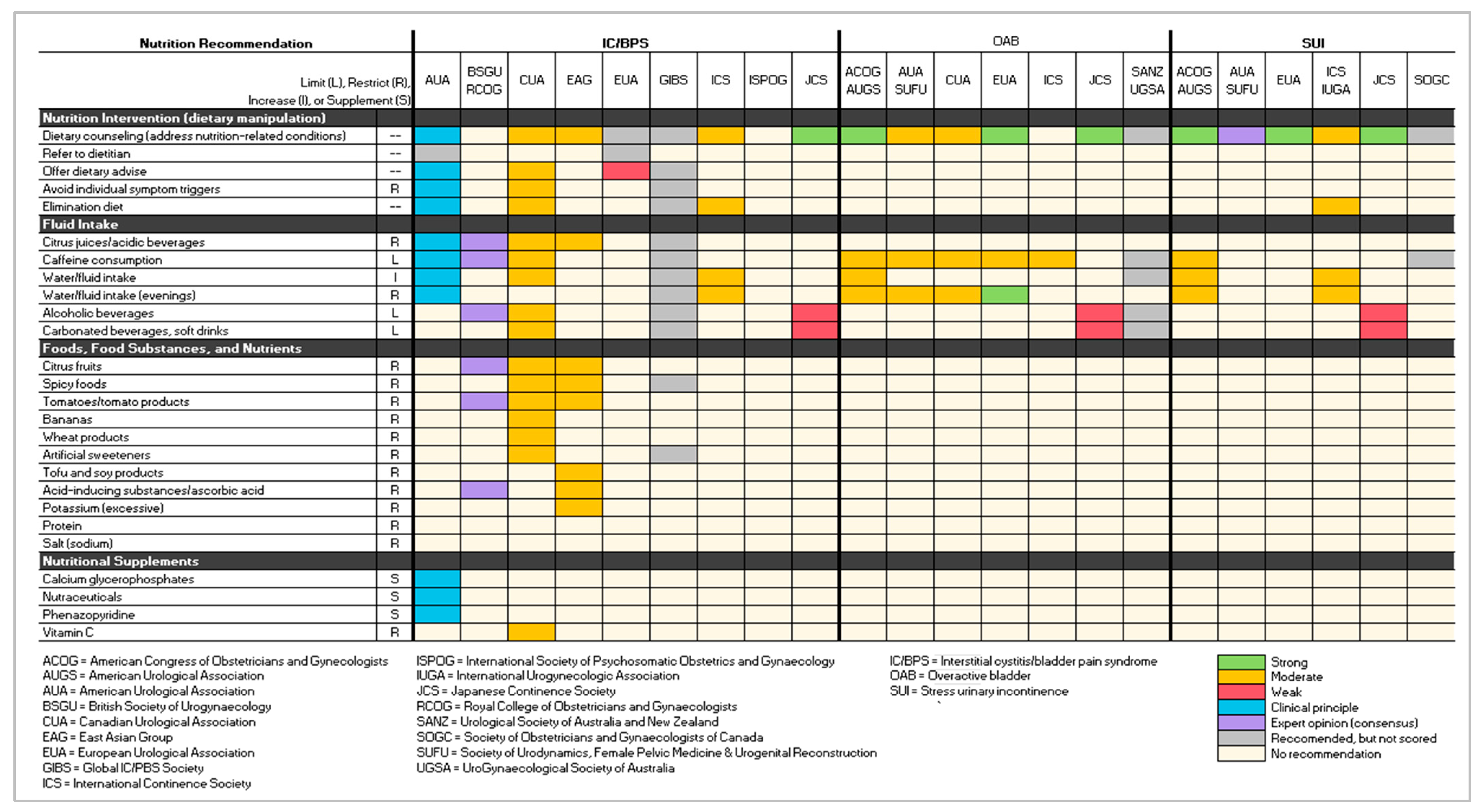
3. Results
- Four were gynecology associations/societies: American College of Obstetricians and Gynecologists, Royal College of Obstetricians and Gynaecologists (RCOG), International Society of Psychosomatic Obstetrics and Gynaecology (ISPOG), and the Society of Obstetricians and Gynaecologists of Canada (SOGC) [11,12,14,15].
- The remaining guideline was developed by the East Asian group of urologists (EAG), an ad hoc group of experts [19].
- AUA/SUFU on OAB and SUI.
- AUGS and ACOG on OAB and SUI.
- BSUG and RCOG on IC/BPS.
- ICS and IUGA on SUI.
- SANZ and UGSA partnered on OAB.
3.1. Interstitial Cystitis/Bladder Pain Syndrome
3.2. Overactive Bladder
3.3. Stress Urinary Incontinence
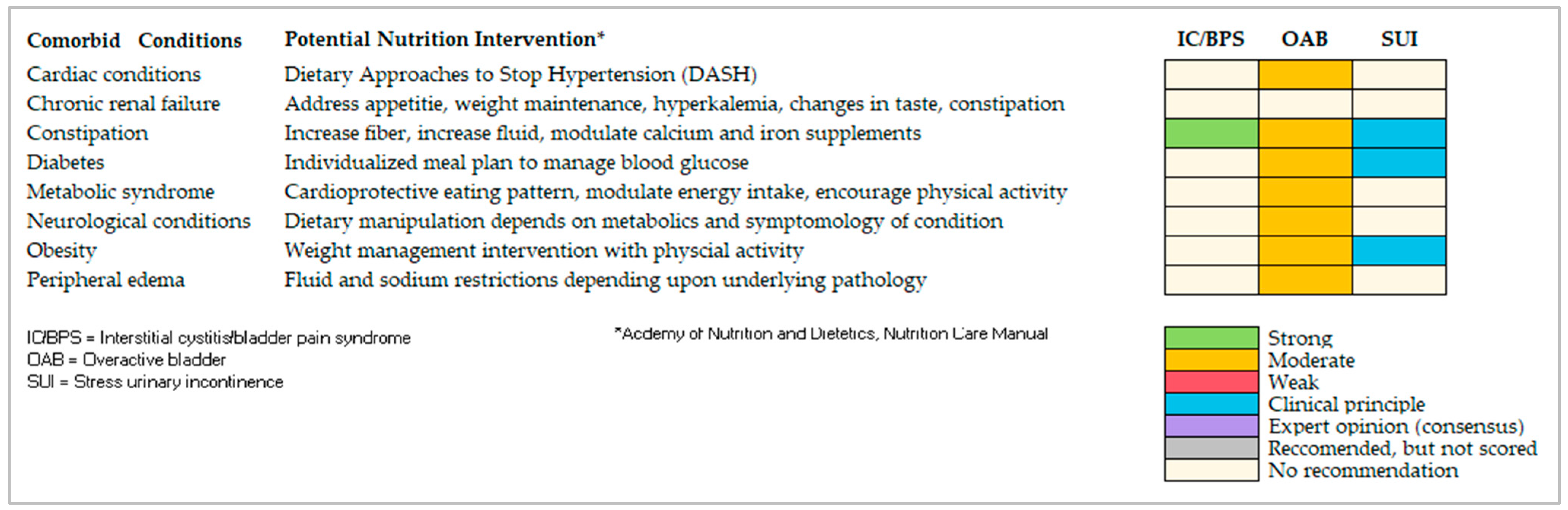
4. Discussion
4.1. Dietary Bladder Irritants
4.2. Translation of Findings into Clinical Practice
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Keathley, J.R.; Arbour, A.; Vohl, M.C. Towards a standardized definition of medical nutrition therapy and regulatory reform in Canada. Can. J. Diet. Pract. Res. 2022, 83, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Van Horn, L.; Lenders, C.M.; Pratt, C.A.; Beech, B.; Carney, P.A.; Dietz, W.; DiMaria-Ghalili, R.; Harlan, T.; Hash, R.; Kohlmeier, M.; et al. Advancing nutrition education, training, and research for medical students, residents, fellows, attending physicians, and other clinicians: Building competencies and interdisciplinary coordination. Adv. Nutr. 2019, 10, 1181–1200. [Google Scholar] [CrossRef] [PubMed]
- Clemens, J.Q.; Erickson, D.R.; Varela, N.P.; Lai, H.H. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J. Urol. 2022, 208, 34–42. [Google Scholar] [CrossRef]
- Lightner, D.J.; Gomelsky, A.; Souter, L.; Vasavada, S.P. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment 2019. J. Urol. 2019, 202, 558–563. [Google Scholar] [CrossRef]
- Kobashi, K.C.; Albo, M.E.; Dmochowski, R.R.; Ginsberg, D.A.; Goldman, H.B.; Gomelsky, A.; Kraus, S.R.; Sandhu, J.S.; Shepler, T.; Treadwell, J.R.; et al. Surgical treatment of female stress urinary incontinence: AUA/SUFU guideline. J. Urol 2017, 198, 875–883. [Google Scholar] [CrossRef] [PubMed]
- Cox, A.; Golda, N.; Nadeau, G. CUA guideline: Diagnosis and treatment of interstitial cystitis/ bladder pain syndrome. Can. Urol. Assoc. J. 2016, 10, E136–E155. [Google Scholar] [CrossRef] [PubMed]
- Corcos, J.; Przydacz, M.; Campeau, L.; Witten, J.; Hickling, D.; Honeine, C.; Radomski, S.B.; Stothers, L.; Wagg, A. CUA guideline on adult overactive bladder. Can. Urol. Assoc. J. 2017, 11, E142–E173. [Google Scholar] [CrossRef]
- EUA Guidelines on Chronic Pelvic Pain. Available online: https://uroweb.org/guidelines/chronic-pelvic-pain/summary-of-changes/2021 (accessed on 26 March 2023).
- Non-Neurogenic Female LUTS. Available online: https://uroweb.org/guidelines/non-neurogenic-female-luts (accessed on 26 March 2023).
- Chung, E.; Lee, D.; Gani, J.; Gillman, M.; Maher, C.; Brennan, J.; Putra, L.J.; Ahmad, L.; Chan, L.L. Position statement: A clinical approach to the management of adult non-neurogenic overactive bladder. Med. J. Aust. 2018, 208, 41–45. [Google Scholar] [CrossRef]
- American Urogynecological Society/American College of Obstetricians and Gynecologists. Urinary Incontinence in Women. Female Pelvic Med. Reconstr. Surg. 2015, 21, 304–314. [Google Scholar] [CrossRef]
- Tirlapur, S.A.; Birch, J.V.; Carberry, C.L.; Khan, K.S.; Latthe, P.M.; Jha, S.; Ward, K.L.; Irving, A. on behalf of the Royal College of Obstetricians and Gynaecologists. Management of bladder pain syndrome. BJOG 2016, 124, e46–e72. [Google Scholar]
- Bo, K.; Frawley, H.C.; Haylen, B.T.; Abramov, Y.; Almeida, F.G.; Berghmans, B.; Bortolini, M.; Dumoulin, C.; Gomes, M.; McClurg, D.; et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Int. Urogynecol. J. 2017, 28, 191–213. [Google Scholar] [CrossRef]
- Siedentopf, F.; Weijenborg, P.; Engman, M.; Maier, B.; Cagnacci, A.; Mimoun, S.; Wenger, A.; Kentenich, H. ISPOG European Consensus Statement—Chronic pelvic pain in women (short version). J. Psychosom. Obstet. Gynaecol. 2015, 36, 161–170. [Google Scholar] [CrossRef]
- Dufour, S.; Wu, M. No. 397—Conservative Care of Urinary Incontinence in Women. J. Obstet. Gynaecol. Can. 2020, 42, 510–522. [Google Scholar] [CrossRef]
- GIBS Clinical Guidelines for IC/BPS. Available online: https://gibsociety.com/wp-content/uploads/2017/11/GIBS-Guidelines.pdf (accessed on 26 March 2023).
- International Continence Society. ICS Standards 2023. Available online: https://www.ics.org/Publications/ICS%20Standards%202023.pdf (accessed on 15 September 2023).
- Takahashi, S.; Takei, M.; Asakura, H.; Gotoh, M.; Ishizuka, O.; Kato, K.; Koyama, M.; Takeyama, M.; Tomoe, H.; Yamanishi, T.; et al. Clinical guidelines for female lower urinary tract symptoms (second edition). Int. J. Urol. 2021, 28, 474–492. [Google Scholar] [CrossRef]
- Homma, Y.; Akiyama, Y.; Tomoe, H.; Furuta, A.; Ueda, T.; Maeda, D.; Lin, A.T.; Kuo, H.-C.; Lee, M.-H.; Oh, S.-J.; et al. Clinical guidelines for interstitial cystitis/bladder pain syndrome. Int. J. Urol. 2020, 27, 578–589. [Google Scholar] [CrossRef]
- Abrams, P.; Cardozo, L.; Fall, M.; Griffiths, D.; Rosier, P.; Ulmsten, U.; Van Kerrebroeck, P.; Victor, A.; Wein, A.; Standardisation Sub-Committee of the International Continence Society. The standardisation of terminology in lower urinary tract function: Report from the Standardisation Sub-committee of the International Continence Society. Urol 2003, 61, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Brouwers, M.C.; Kho, M.E.; Browman, G.P.; Burgers, J.S.; Cluzeau, F.; Feder, G.; Fervers, B.; Graham, I.D.; Grimshaw, J.; Hanna, S.E.; et al. The AGREE Next Steps Consortium. AGREE II: Advancing guideline development, reporting and evaluation in health care. CMAJ 2010, 82, E839–E842. [Google Scholar] [CrossRef] [PubMed]
- Merwe, J.P.; Nordling, J.; Bouchelouche, P.; Bouchelouche, K.; Cervigni, M.; Daha, L.K.; Elneil, S.; Fall, M.; Hohlbrugger, G.; Irwin, P.; et al. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: An ESSIC proposal. Eur. Urol. 2008, 53, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Alwis, U.S.; Monaghan, T.F.; Haddad, R.; Weiss, J.P.; Roggeman, S.; Laecke, E.V.; Walle, J.V.; Wein, A.J.; Everaert, K. Dietary considerations in the evaluation and management of nocturia. F1000Res 2020, 9, 165. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, T.; Miyata, Y.; Sakai, H. Daily salt intake is an independent risk factor for pollakiuria and nocturia. Int. J. Urol. 2017, 24, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Tomohiro, M.; Nakamura, Y.; Yasuda, T.; Ohba, K.; Miyata, Y.; Sakai, H. Effect of restricted salt intake on nocturia. Eur. Urol. Suppl. 2017, 16, e698. [Google Scholar] [CrossRef]
- Monaghan, T.F.; Michelson, K.P.; Wu, Z.D.; Gong, F.; Agudelo, C.W.; George, C.D.; Alwis, U.S.; Epstein, M.R.; Mekki, P.; Flores, V.X.; et al. Sodium restriction improves nocturia in patients at a cardiology clinic. J. Clin. Hypertens. 2020, 22, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Gueds, P.F.; Santana, S.F.; Colpo, E. Consumption of bladder irritant liquids and foods by incontinent women. Discip. Sci. 2019, 20, 15–24. [Google Scholar]
- Geppetti, P.; Nassini, R.; Materazzi, S.; Benemei, S. The concept of neurogenic inflammation. BJU Int. 2008, 101 (Suppl. S3), 2–6. [Google Scholar] [CrossRef]
- Elliott, R.A.; Kapoor, S.; Tincello, D.G. Expression and distribution of the sweet taste receptor isoforms T1R2 and T1R3 in human and rat bladders. J. Urol. 2011, 186, 2455–2462. [Google Scholar] [CrossRef]
- Dasgupta, J.; Elliott, R.A.; Doshani, A.; Tincello, D.G. Enhancement of rat bladder contraction by artificial sweeteners via increased extracellular Ca2+ influx. Toxicol. Appl. Pharmacol. 2006, 217, 216–224. [Google Scholar] [CrossRef]
- Shahid, M.; Kim, M.; Yeon, A.; Andres, A.M.; You, S.; Kim, J. Quantitative proteomic analysis reveals caffeine-perturbed proteomic profiles in normal bladder epithelial cells. Proteomics 2018, 18, e1800190. [Google Scholar] [CrossRef]
- Avelino, A.; Cruz, F. TRPV1 (vanilloid receptor) in the urinary tract: Expression, function and clinical applications. Naunyn. Schmiedebergs. Arch. Pharmacol. 2006, 373, 287–299. [Google Scholar] [CrossRef]
- Dasgupta, J.; Elliott, R.A.; Tincello, D.G. Modification of rat detrusor muscle contraction by ascorbic acid and citric acid involving enhanced neurotransmitter release and Ca2+ influx. Neurourol. Urodyn. 2009, 28, 542–548. [Google Scholar] [CrossRef]
- Jordt, S.E.; Bautista, D.M.; Chuang, H.H.; McKemy, D.D.; Zygmunt, P.M.; Högestätt, E.D.; Meng, I.D.; Julius, D. Mustard oils and cannabinoids excite sensory nerve fibres through the TRP channel ANKTM1. Nature 2004, 427, 260–265. [Google Scholar] [CrossRef]
- Gordon, B.; Shorter, B.; Sarcona, A.; Moldwin, R. Nutritional considerations for interstitial cystitis/bladder pain syndrome. J. Acad. Nutr. Diet. 2015, 115, 1372–1379. [Google Scholar] [CrossRef] [PubMed]
- Imamura, M.; Williams, K.; Wells, M.; McGrother, C. Lifestyle interventions for the treatment of urinary incontinence in adults. Cochrane Database Syst. Rev. 2015, 12, CD003505. [Google Scholar] [CrossRef] [PubMed]
- Bradley, C.S.; Erickson, B.A.; Messersmith, E.E.; Pelletier-Cameron, A.; Lai, H.H.; Kreder, K.J.; Yang, C.C.; Merion, R.M.; Bavendam, T.G.; Kirkali, Z.; et al. Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN). Evidence of the impact of diet, fluid Intake, caffeine, alcohol and tobacco on lower Urinary Tract Symptoms: A systematic review. J. Urol. 2017, 198, 1010–1020. [Google Scholar] [CrossRef]
- Foster, H.E., Jr.; Hanno, P.M.; Nickel, J.C.; Payne, C.K.; Mayer, R.D.; Burks, D.A.; Yang, C.C.; Chai, T.C.; Kreder, K.J.; Peters, K.M.; et al. Interstitial Cystitis Collaborative Research Network. Effect of amitriptyline on symptoms in treatment naïve patients with interstitial cystitis/painful bladder syndrome. J. Urol. 2010, 183, 1853–1858. [Google Scholar] [CrossRef] [PubMed]
- Oh-oka, H. Clinical efficacy of 1-year intensive systematic dietary manipulation as complementary and alternative medicine therapies on female patients with interstitial cystitis/bladder pain syndrome. Urol 2017, 106, 50–54. [Google Scholar] [CrossRef]
- Gordon, B.; Blanton, C.; Ramsey, R.; Jeffery, A.; Richey, L.; Hulse, R. Anti-inflammatory diet for women with interstitial cystitis/bladder pain syndrome: The AID-IC pilot study. Methods Protoc. 2022, 5, 40. [Google Scholar] [CrossRef]
- Matsuo, T.; Miyata, Y.; Otsubo, A.; Mukae, Y.; Mitsunari, K.; Ohba, K.; Sakai, H. Efficacy of salt reduction for managing overactive bladder symptoms: A prospective study in patients with excessive daily salt intake. Sci. Rep. 2021, 18, 4046. [Google Scholar] [CrossRef]
- Hashim, H.; Abrams, P. How should patients with an overactive bladder manipulate their fluid intake? BJU Int. 2008, 102, 62–66. [Google Scholar] [CrossRef]
- Yazdany, T.; Jakus-Waldman, S.; Jeppson, P.C.; Schimpf, M.O.; Yurteri-Kaplan, L.A.; Ferzandi, T.R.; Weber-LeBrun, E.; Knoepp, L.; Mamik, M.; Viswanathan, M.; et al. American Urogynecologic Society. The impact of weight loss intervention on lower urinary tract symptoms and urinary incontinence in overweight and obese women. Female Pelvic Med. Reconstr. Surg. 2020, 26, 16–29. [Google Scholar] [CrossRef]
- Academy of Nutrition and Dietetics Nutrition Care Manual®. Available online: http://www.nutritioncaremanual.org (accessed on 1 July 2023).
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Focused on one or more of the three disorders | Did not provide discrete guidance on specific conditions |
| Included recommendations relevant to adult females | Recommendations were for children or males |
| Published in the last 10 years (December 2012–January 2023) | Published prior to December 2012 |
| Developed by urologic, urogynecologic, and gynecologic association, society, or committee | Developed by other associations, societies, or committees |
| Included relevant treatment interventions | Focused on guidelines for non-treatment issues |
| Published in the English language | English translation of guideline not found |
| Refs. | Acronym | Organizational Developer | IC/BPS | OAB | SUI |
|---|---|---|---|---|---|
| [11] | ACOG | American Urogynecologic Society | 2014 | 2014 | |
| AUGS | American College of Obstetricians and Gynecologists | ||||
| [3] | AUA | American Urological Association | 2022 | ||
| [4] | AUA | American Urological Association | 2022 | ||
| SUFU | Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction | ||||
| [5] | AUA | American Urological Association | 2023 | ||
| SUFU | Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction | ||||
| [12] | BSUG | British Society of Urogynaecology | 2016 | ||
| RCOG | Royal College of Obstetricians and Gynaecologists | ||||
| [6] | CUA | Canadian Urological Association | 2019 | ||
| [7] | CUA | Canadian Urological Association | 2017 | ||
| [19] | EAG | East Asian Group | 2015 | ||
| [8] | EUA | European Urological Association | 2021 | ||
| [9] | EUA | European Urological Association | 2022 | 2022 | |
| [16] | GIBS | Global IC/PBS Society | 2015 | ||
| [17] | ICS | International Continence Society | 2023 | 2023 | |
| [13] | ICS | International Continence Society | 2017 | ||
| IUGA | International Urogynecological Association | ||||
| [14] | ISPOG | International Society of Psychosomatic Obstetrics and Gynecology | 2015 | ||
| [18] | JCS | Japanese Continence Society | 2021 | 2021 | 2021 |
| [15] | SOGC | Society of Obstetricians and Gynaecologists of Canada | 2018 | ||
| [10] | SANZ | Urological Society of Australia and New Zealand | 2018 | ||
| UGSA | Urogynaecological Society of Australia | ||||
| Number of Guidelines per Condition | 9 | 7 | 6 | ||
| Total Number of Guidelines in Review | 22 | ||||
| Schema Org: Condition | Grading Schema Employed for Strength of Evidence Rating | Mapped to Standardized Schema | |||
|---|---|---|---|---|---|
| ACOG/AUGS ACOG/AUGS: OAB, SUI | Level A = Good and consistent scientific evidence Level B = Limited or inconsistent scientific evidence Level C = Clinical practice and expert opinion | Level A = Strong/Moderate Level B = Weak Level C = Clinical principal or Expert Opinion | |||
| AUA AUA: IC/BPS AUA/SUFU: SUI | Grade A/Strong = Rigorous RCT or very strong observational Grade B/Moderate = Weak RCTs or strong observational Grade C/Low = Weak observational Clinical principle (CP) = Widely accepted care practice Expert opinion (EO) = consensus of guidelines panel | Grade A = Strong Grade B = Moderate Grace C = Weak CP = Clinical principle EO = Expert opinion | |||
| BSUG/RCOG BSUG/RCOG: IC/BPS | Grade A = ≥1 Meta-analysis, systematic review or RCT Grade B = High-quality reviews, case-control, cohorts) Grade C = Well-conducted case-control or cohorts Grade D = Case reports, case series, expert opinions √ = Clinical experience | Grade A = Strong Grade B = Moderate Grace C = Weak √ = Clinical principle Grade D = Expert opinion | |||
| EAG EAG: IC/BPS | A = Strongly recommended B = Recommended C = Insufficient evidence for recommendation D = Not recommended | Grade A = Strong Grade B = Moderate Grade C = Weak Grade D = No recommendation | |||
| GRADE AUA/SUFU: OAB EUA: IC/BPS, OAB, SUI SOGC: SUI | High/Strong = Treatment effect confidently same as research findings Moderate = Treatment effect probably close to findings Low/Weak = Treatment effect different from findings Very low = Treatment effect markedly different from findings | High = Strong Moderate = Moderate Low = Weak Very low = Expert opinion | |||
| JCS JCS: IC/PBS, OAB, SUI | A = This action is strongly recommended B = This action is recommended C = There is no clear evidence for recommending this action C1 = Performing the action is not recommended C2 = Not performing this action is recommended D = The action can still be performed Pending = No decision has been made regarding the grade of recommendation | A = Strong B = Moderate C/C1/C2 = Weak D = Expert opinion Pending = No recommendation | |||
| OCEBM CUA: IC/BPS CUA: OAB ICS: IC/BPS, OAB | Grade A (level 1) = Randomized controlled trial Grade B (level 2) = Systematic review of clinical trials, nonrandomized controlled cohort/follow-up study Grade C (level 3) = Case-series, case-control Grade D (level 4) = Expert opinion | Grade A = Strong Grade B = Moderate Grade C = Weak Grade D = Clinical principle/ expert opinion | |||
Grading Schemas:
| Organization (Org) Acronyms: ACOG = American College of Obstetricians and Gynecologists AUGS = American Urogynecologic Society AUA = American Urological Association BSUG = British Society of Urogynaecology CUA = Canadian Urological Association EAG = East Asian group of urologists EUA = European Urological Association GIBS = Global IC/PBS Society ICS = International Continence Society ISPOG = International Society of Psychosomatic Obstetrics and Gynecology IUGA = International Urogynecological Association JCS = Japanese Continence Society RCOG = Royal College of Obstetricians and Gynaecologists SANZ = Urological Society of Australia and New Zealand SOGC = Society of Obstetricians and Gynaecologists of Canada SUFU = Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction UGSA = Urogynaecological Society of Australia | ||||
| Item | LUTS | Mechanism of Action | Source |
|---|---|---|---|
| Artificial sweeteners | Urinary urgency, overactive bladder | Rat and in vitro: Activation of T1R2/3 sweet taste receptors in bladder urothelium may result in bladder contraction | [29] |
| Urinary urgency and frequency, nocturia | In vitro: Artificial sweeteners modulate L-type Ca+2 channels provoke detrusor muscle contraction | [30] | |
| Caffeine | Urinary urgency | In vitro: Increased expression of transient receptor potential vanilloid 1 (TRPV1) mRNA in bladder lining mucosa | [31] |
| Urinary urgency | Rat model: Affects capsaicin-sensitive ion channel which regulates pain perception and bladder contractions | [32] | |
| Urinary frequency | Mouse model: Elevated transcription factor c-Fos and nerve growth factor activate neuronal micturition centers | [31] | |
| Urinary urgency/frequency, incontinence, nocturia | In vitro: Heightened bladder sensory signaling, generating detrusor overactivity | [31] | |
| Urinary urgency, overactive bladder | In vitro: Affects bladder epithelium, causes changes in the biological pathways integral in muscle contraction | [31] | |
| Citrus foods | Urinary urgency and frequency, incontinence | In vitro: Ascorbic acid increases both the frequency and intensity of muscle contractions in the bladder | [33] |
| Soda | Urinary urgency and frequency, incontinence | In vitro: Ascorbic acid, citric acid, phenylalanine, and colorants in carbonated sodas disrupt bladder functioning and enhance bladder muscle contraction | [33] |
| Spicy foods (Wasabi, horseradish, mustard, chili peppers) | Bladder pain | In vitro: Capsaicin and other chemicals found in spicy foods activate sensory nerve endings via TRP channels producing irritation and inflammation | [28,34] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gordon, B. Nutritional Considerations for Bladder Storage Conditions in Adult Females. Int. J. Environ. Res. Public Health 2023, 20, 6879. https://doi.org/10.3390/ijerph20196879
Gordon B. Nutritional Considerations for Bladder Storage Conditions in Adult Females. International Journal of Environmental Research and Public Health. 2023; 20(19):6879. https://doi.org/10.3390/ijerph20196879
Chicago/Turabian StyleGordon, Barbara. 2023. "Nutritional Considerations for Bladder Storage Conditions in Adult Females" International Journal of Environmental Research and Public Health 20, no. 19: 6879. https://doi.org/10.3390/ijerph20196879
APA StyleGordon, B. (2023). Nutritional Considerations for Bladder Storage Conditions in Adult Females. International Journal of Environmental Research and Public Health, 20(19), 6879. https://doi.org/10.3390/ijerph20196879





