Pregnancy Apps for Self-Monitoring: Scoping Review of the Most Popular Global Apps Available in Australia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Step 1: Identification of Smartphone Apps
2.3. Step 2: Screening of Smartphone Apps
2.4. Step 3: Evaluation of Smartphone Apps
2.5. Step 4: Scoring and Analysis of Smartphone Apps
2.6. Statistical Analysis
3. Results
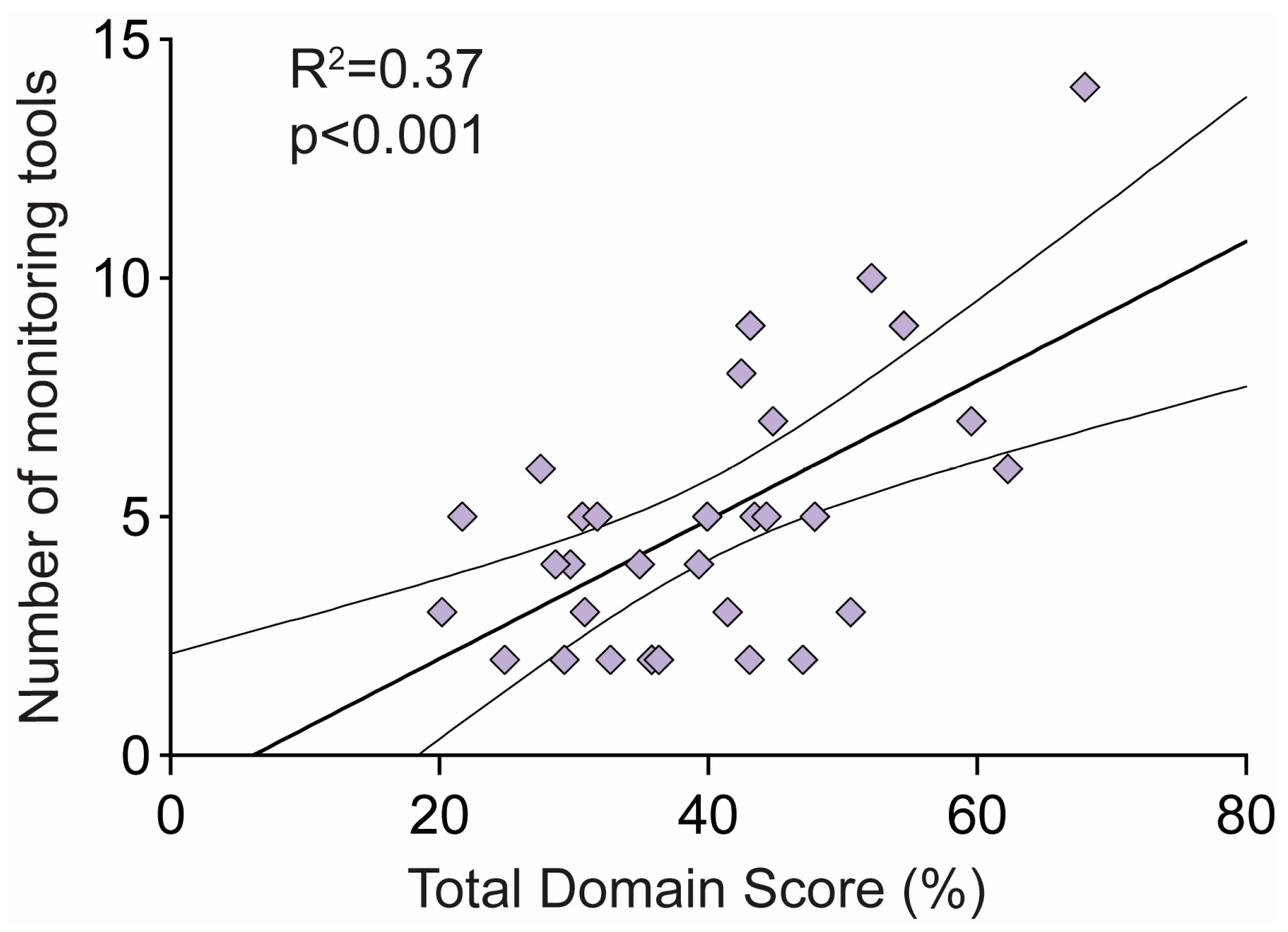
3.1. Self-Monitoring Tools
3.2. Scorecard Approach
3.2.1. Clinical
3.2.2. Technical
3.2.3. Usability—User Experience and Interface
3.2.4. Cost and Time
3.2.5. End-User Requirements
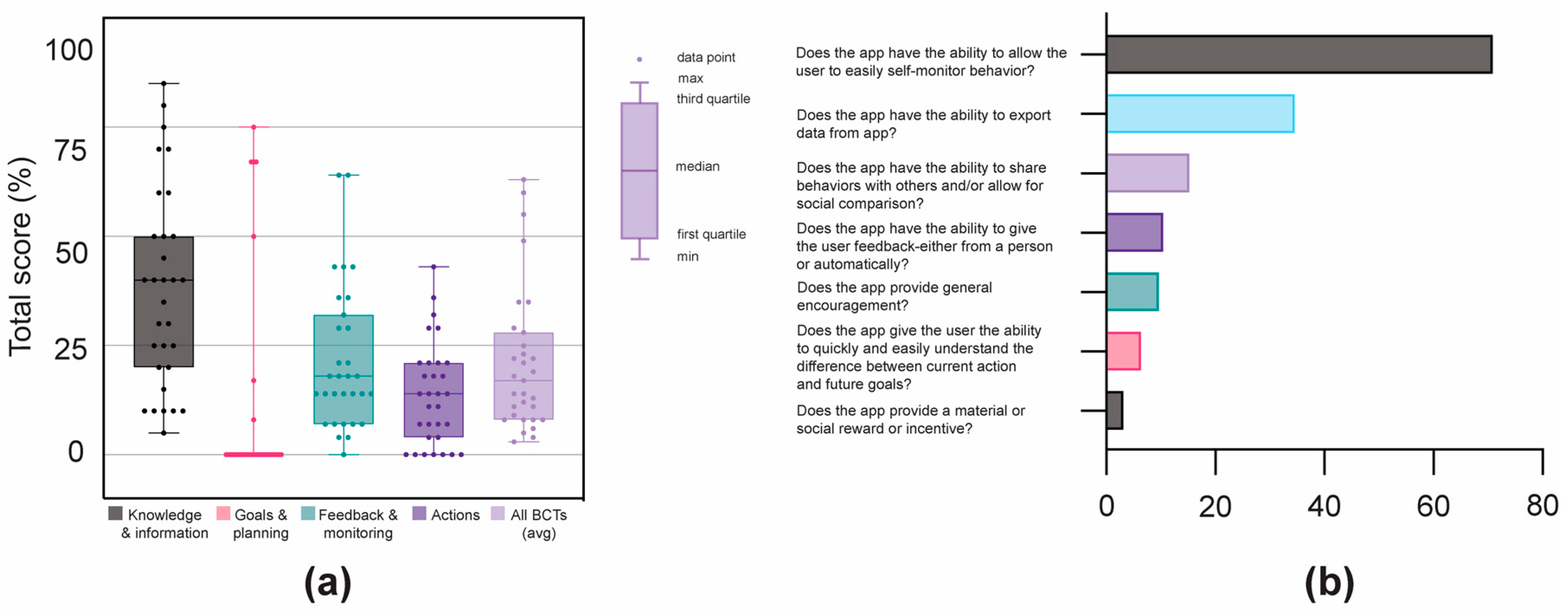
3.3. Behaviour Change Techniques (BCTs)
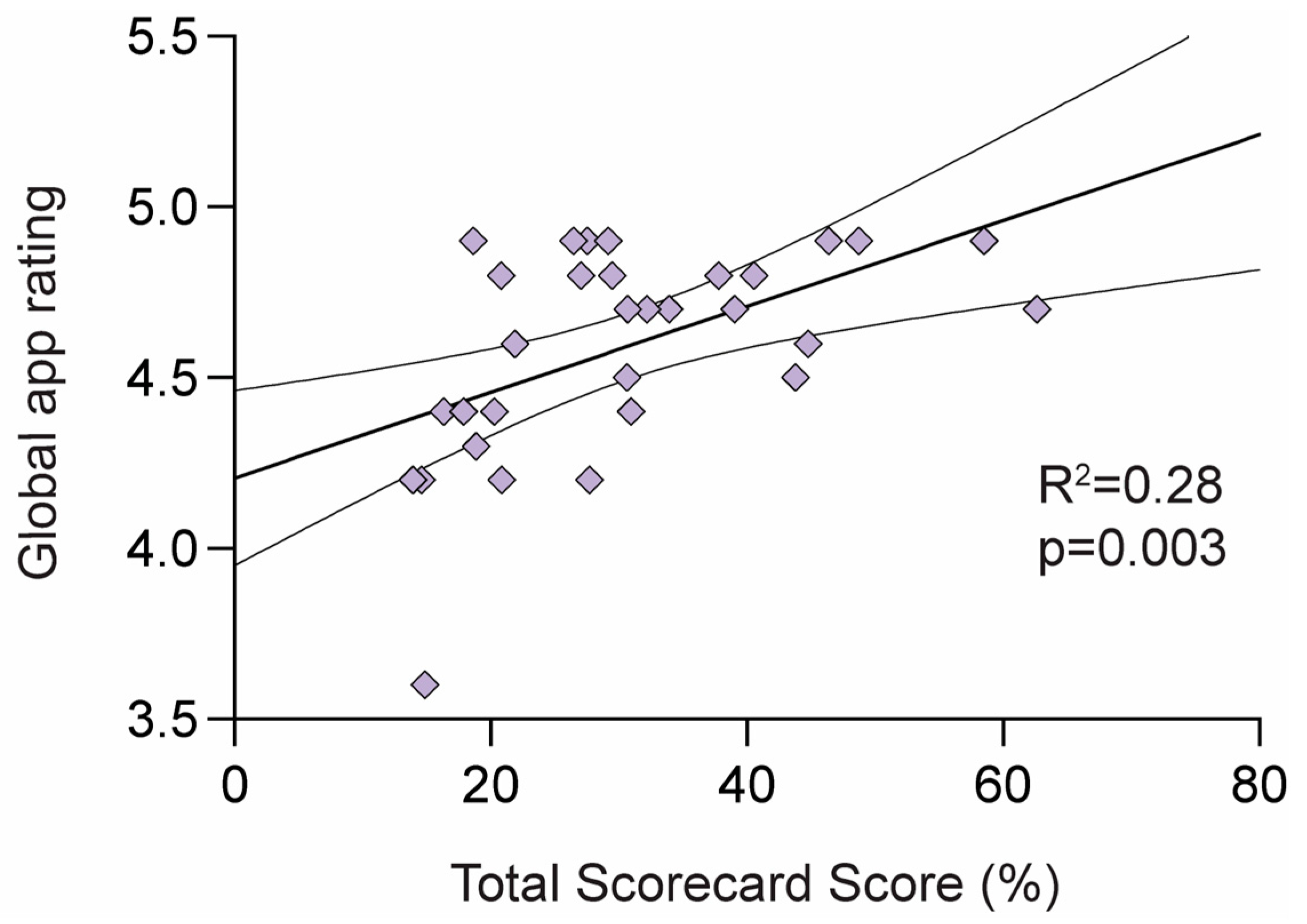
3.4. Overall Quality of Pregnancy Apps
4. Discussion
4.1. Summary of Findings
4.2. What Factors Contribute to the Quality of Pregnancy Apps for Self-Monitoring?
4.3. How Can We Relay These Findings to Users to Inform Their App Choices?
4.4. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- DataReportal. Digital around the World. 2022. Available online: https://datareportal.com/global-digital-overview (accessed on 10 November 2022).
- Marko, K.I.; Ganju, N.; Krapf, J.M.; Gaba, N.D.; Brown, J.A.; Benham, J.J.; Oh, J.; Richards, L.M.; Meltzer, A.C. A Mobile Prenatal Care App to Reduce In-Person Visits: Prospective Controlled Trial. JMIR mHealth uHealth 2019, 7, e10520. [Google Scholar] [CrossRef]
- Lisonkova, S.; Sheps, S.B.; Janssen, P.A.; Lee, S.K.; Dahlgren, L.; Macnab, Y.C. Birth Outcomes Among Older Mothers in Rural Versus Urban Areas: A Residence-Based Approach. J. Rural. Health 2011, 27, 211–219. [Google Scholar] [CrossRef]
- Kent, S.T.; McClure, L.A.; Zaitchik, B.F.; Gohlke, J.M. Area-level risk factors for adverse birth outcomes: Trends in urban and rural settings. BMC Pregnancy Childbirth 2013, 13, 129. [Google Scholar] [CrossRef] [Green Version]
- Dongarwar, D.; Salihu, H.M. Place of Residence and Inequities in Adverse Pregnancy and Birth Outcomes in India. Int. J. Matern. Child Health AIDS 2020, 9, 53–63. [Google Scholar] [CrossRef]
- Kim, M.K.; Lee, S.M.; Bae, S.-H.; Kim, H.J.; Lim, N.G.; Yoon, S.-J.; Lee, J.Y.; Jo, M.-W. Socioeconomic status can affect pregnancy outcomes and complications, even with a universal healthcare system. Int. J. Equity Health 2018, 17, 2. [Google Scholar] [CrossRef] [Green Version]
- Ospina, M.; Osornio-Vargas, R.; Nielsen, C.C.; Crawford, S.; Kumar, M.; Aziz, K.; Serrano-Lomelin, J. Socioeconomic gradients of adverse birth outcomes and related maternal factors in rural and urban Alberta, Canada: A concentration index approach. BMJ Open 2020, 10, e033296. [Google Scholar] [CrossRef] [Green Version]
- Lisonkova, S.; Haslam, M.D.; Dahlgren, L.; Chen, I.; Synnes, A.R.; Lim, K.I. Maternal morbidity and perinatal outcomes among women in rural versus urban areas. Can. Med. Assoc. J. 2016, 188, E456–E465. [Google Scholar] [CrossRef] [Green Version]
- Lupton, D.; Pedersen, S. An Australian survey of women’s use of pregnancy and parenting apps. Women Birth 2016, 29, 368–375. [Google Scholar] [CrossRef] [Green Version]
- Şat, S.Ö.; Sözbir, Ş.Y. Use of mobile applications and blogs by pregnant women in Turkey and the impact on adaptation to pregnancy. Midwifery 2018, 62, 273–277. [Google Scholar]
- Wang, N.; Deng, Z.; Wen, L.M.; Ding, Y.; He, G. Understanding the Use of Smartphone Apps for Health Information Among Pregnant Chinese Women: Mixed Methods Study. JMIR mHealth uHealth 2019, 7, e12631. [Google Scholar] [CrossRef]
- Lupton, D. ‘It Just Gives Me a Bit of Peace of Mind’: Australian Women’s Use of Digital Media for Pregnancy and Early Motherhood. Societies 2017, 7, 25. [Google Scholar] [CrossRef]
- Lanssens, D.; Thijs, I.M.; Dreesen, P.; Van Hecke, A.; Coorevits, P.; Gaethofs, G.; Derycke, J.; Tency, I. Information Resources Among Flemish Pregnant Women: Cross-sectional Study. JMIR Form. Res. 2022, 6, e37866. [Google Scholar] [CrossRef]
- Şat, S.; Sözbir, Y. Use of Mobile Applications by Pregnant Women and Levels of Pregnancy Distress During the COVID-19 (Coronavirus) Pandemic. Matern. Child Health J. 2021, 25, 1057–1068. [Google Scholar]
- Wang, W.; Sun, L.; Liu, T.; Lai, T. The use of E-health during the COVID-19 pandemic: A case study in China’s Hubei province. Health Sociol. Rev. 2021, 31, 215–231. [Google Scholar] [CrossRef]
- Store, A.A. App Store Preview Medical. 2022. Available online: https://apps.apple.com/us/charts/iphone/medical-apps/6020?chart=top-free (accessed on 31 October 2022).
- Hughson, J.-A.P.; Daly, J.O.; Woodward-Kron, R.; Hajek, J.; Story, D. The Rise of Pregnancy Apps and the Implications for Culturally and Linguistically Diverse Women: Narrative Review. JMIR mHealth uHealth 2018, 6, e189. [Google Scholar] [CrossRef] [Green Version]
- Lee, Y.; Moon, M. Utilization and Content Evaluation of Mobile Applications for Pregnancy, Birth and Child Care. Health Inform. Res. 2016, 22, 73–80. [Google Scholar] [CrossRef] [Green Version]
- Musgrave, L.M.; Kizirian, N.V.; Homer, C.S.; Gordon, A. Mobile Phone Apps in Australia for Improving Pregnancy Outcomes: Systematic Search on App Stores. JMIR mHealth uHealth 2020, 8, e22340. [Google Scholar] [CrossRef]
- Simpson, K.R. Birth Settings in America: Outcomes, Quality, Access, and Choice: New Report from the National Academies of Sciences, Engineering and Medicine. MCN Am. J. Matern. Child Nurs. 2020, 45, 137. [Google Scholar] [CrossRef]
- Tucker, K.L.; Taylor, K.S.; Crawford, C.; Hodgkinson, J.A.; Bankhead, C.; Carver, T.; Ewers, E.; Glogowska, M.; Greenfield, S.M.; Ingram, L.; et al. Blood pressure self-monitoring in pregnancy: Examining feasibility in a prospective cohort study. BMC Pregnancy Childbirth 2017, 17, 442. [Google Scholar] [CrossRef] [Green Version]
- Dahl, A.A. Healthy Motivations for Moms-To-Be (Healthy MoM2B) Study: A Mobile Health Intervention Targeting Gestational Weight Gain among U.S. Women. Ph.D. Thesis, University of South Carolina, Columbia, SC, USA, 2018. [Google Scholar]
- Willcox, J.; Wilkinson, S.A.; Lappas, M.; Ball, K.; Crawford, D.; McCarthy, E.A.; Fjeldsoe, B.; Whittaker, R.; Maddison, R.; Campbell, K.J. A mobile health intervention promoting healthy gestational weight gain for women entering pregnancy at a high body mass index: The txt4two pilot randomised controlled trial. Int. J. Obstet. Gynaecol. 2017, 124, 1718–1728. [Google Scholar] [CrossRef] [Green Version]
- Frid, G.; Bogaert, K.; Chen, K.T. Mobile Health Apps for Pregnant Women: Systematic Search, Evaluation, and Analysis of Features. J. Med. Internet Res. 2021, 23, e25667. [Google Scholar] [CrossRef] [PubMed]
- Brunelli, L.; De Vita, C.; Cenedese, F.; Cinello, M.; Paris, M.; Samogizio, F.; Starec, A.; Bava, M.; Cin, M.D.; Zanchiello, S.; et al. Gaps and Future Challenges of Italian Apps for Pregnancy and Postnatal Care: Systematic Search on App Stores. J. Med. Internet Res. 2021, 23, e29151. [Google Scholar] [CrossRef]
- Daly, L.M.; Boyle, F.; Gibbons, K.; Le, H.; Roberts, J.; Flenady, V. Mobile applications providing guidance about decreased fetal movement: Review and content analysis. Women Birth 2019, 32, e289–e296. [Google Scholar] [CrossRef] [PubMed]
- Scott, K.M.; Gome, G.A.; Richards, D.; Caldwell, P.H. How trustworthy are apps for maternal and child health? Health Technol. 2015, 4, 329–336. [Google Scholar] [CrossRef]
- Muñoz-Mancisidor, A.; Martin-Payo, R.; Gonzalez-Mendez, X.; Fernández-Álvarez, M.D.M. Content, Behavior Change Techniques, and Quality of Pregnancy Apps in Spain: Systematic Search on App Stores. JMIR mHealth uHealth 2021, 9, e27995. [Google Scholar] [CrossRef] [PubMed]
- Alicia, A.; Dahl, C.G.D.; Alycia, K. Boutté, Anthony Crimarco & Gabrielle Turner-McGrievy Mobilizing mHealth for Moms: A Review of Mobile Apps for Tracking Gestational Weight Gain. J. Technol. Behav. Sci. 2018, 3, 32–40. [Google Scholar]
- Hayman, M.J.; Alfrey, K.-L.; Waters, K.; Cannon, S.; Mielke, G.I.; Keating, S.E.; Mena, G.P.; Mottola, M.F.; Evenson, K.R.; Davenport, M.H.; et al. Evaluating Evidence-Based Content, Features of Exercise Instruction, and Expert Involvement in Physical Activity Apps for Pregnant Women: Systematic Search and Content Analysis. JMIR mHealth uHealth 2022, 10, e31607. [Google Scholar] [CrossRef]
- Tinius, R.A.; Polston, M.; Bradshaw, H.; Ashley, P.; Greene, A.; Parker, A.N. An Assessment of Mobile Applications Designed to Address Physical Activity During Pregnancy and Postpartum. Int. J. Exerc. Sci. 2021, 14, 382–399. [Google Scholar]
- Brown, H.M.; Bucher, T.; Collins, C.E.; Rollo, M.E. A review of pregnancy apps freely available in the Google Play Store. Health Promot. J. Aust. Off. J. Aust. Assoc. Health Promot. Prof. 2020, 31, 340–342. [Google Scholar] [CrossRef]
- Brown, H.M.; Bucher, T.; Collins, C.E.; Rollo, M.E. A review of pregnancy iPhone apps assessing their quality, inclusion of behaviour change techniques, and nutrition information. Matern. Child Nutr. 2019, 15, e12768. [Google Scholar] [CrossRef] [Green Version]
- Faessen, J.P.; Lucassen, D.A.; Buso, M.E.C.; Camps, G.; Feskens, E.J.M.; Brouwer-Brolsma, E.M. Eating for 2: A Systematic Review of Dutch App Stores for Apps Promoting a Healthy Diet during Pregnancy. Curr. Dev. Nutr. 2022, 6, nzac087. [Google Scholar] [CrossRef] [PubMed]
- Bland, C.; Dalrymple, K.V.; White, S.L.; Moore, A.; Poston, L.; Flynn, A.C. Smartphone applications available to pregnant women in the United Kingdom: An assessment of nutritional information. Matern. Child Nutr. 2020, 16, e12918. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evans, K.; Donelan, J.; Rennick-Egglestone, S.; Cox, S.; Kuipers, Y. A review of Mobile ‘Apps’ for women with anxiety in pregnancy: Maternity care professionals guide to locating and assessing Anxiety Apps. J. Med. Internet Res. 2022, 24, e31831. [Google Scholar] [CrossRef] [PubMed]
- Spadaro, B.; Martin-Key, N.A.; Funnell, E.; Bahn, S. mHealth Solutions for Perinatal Mental Health: Scoping Review and Appraisal Following the mHealth Index and Navigation Database Framework. JMIR mHealth uHealth 2022, 10, e30724. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, A.; Smith, A.D.; Chadwick, P.; Croker, H.; Llewellyn, C.H. Exclusively Digital Health Interventions Targeting Diet, Physical Activity, and Weight Gain in Pregnant Women: Systematic Review and Meta-Analysis. JMIR mHealth uHealth 2020, 8, e18255. [Google Scholar] [CrossRef]
- Griffiths, S.E.; Parsons, J.; Naughton, F.; Fulton, E.A.; Tombor, I.; Brown, K.E. Are digital interventions for smoking cessation in pregnancy effective? A systematic review and meta-analysis. Health Psychol. Rev. 2018, 12, 333–356. [Google Scholar] [CrossRef] [Green Version]
- Truelove, S.; Vanderloo, L.M.; Tucker, P.; Di Sebastiano, K.M.; Faulkner, G. The use of the behaviour change wheel in the development of ParticipACTION’s physical activity app. Prev. Med. Rep. 2020, 20, 101224. [Google Scholar] [CrossRef]
- Mathews, S.C.; McShea, M.J.; Hanley, C.L.; Ravitz, A.; Labrique, A.B.; Cohen, A.B. Digital health: A path to validation. NPJ Digit. Med. 2019, 2, 38. [Google Scholar] [CrossRef] [Green Version]
- Sedhom, R.; McShea, M.J.; Cohen, A.B.; Webster, J.A.; Mathews, S.C. Mobile app validation: A digital health scorecard approach. NPJ Digit. Med. 2021, 4, 111. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Straus, S.E. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- BinDhim, N.F.; Hawkey, A.; Trevena, L. A Systematic Review of Quality Assessment Methods for Smartphone Health Apps. Telemed. e-Health 2015, 21, 97–104. [Google Scholar] [CrossRef]
- Olano, F. Google-Play-Scraper. 2022. Available online: https://github.com/facundoolano/google-play-scraper#pull/557/head (accessed on 2 April 2021).
- Olano, F. App-Store-Scraper. 2022. Available online: https://github.com/facundoolano/app-store-scraper (accessed on 2 April 2021).
- Lupton, D.; Pedersen, S. ‘What Is Happening with Your Body and Your Baby’: Australian Women’s Use of Pregnancy and Parenting Apps; University of Canberra: Canberra, Australia, 2015. [Google Scholar]
- Vickery, M.; van Teijlingen, E.; Hundley, V.; Smith, G.B.; Way, S.; Westwood, G. Midwives’ views towards women using mHealth and eHealth to self-monitor their pregnancy: A systematic review of the literature. Eur. J. Midwifery 2020, 4, 36. [Google Scholar] [CrossRef] [PubMed]
- McKay, F.H.; Slykerman, S.; Dunn, M. The App Behavior Change Scale: Creation of a Scale to Assess the Potential of Apps to Promote Behavior Change. JMIR mHealth uHealth 2019, 7, e11130. [Google Scholar] [CrossRef] [PubMed]
- Alfawzan, N.; Christen, M.; Spitale, G.; Biller-Andorno, N. Privacy, Data Sharing, and Data Security Policies of Women’s mHealth Apps: Scoping Review and Content Analysis. JMIR mHealth uHealth 2022, 10, e33735. [Google Scholar] [CrossRef] [PubMed]
- Holeman, I.; Kane, D. Human-centered design for global health equity. Inf. Technol. Dev. 2019, 26, 477–505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCurdie, T.; Taneva, S.; Casselman, M.; Yeung, M.; McDaniel, C.; Ho, W.; Cafazzo, J. mHealth Consumer Apps: The Case for User-Centered Design. Biomed. Instrum. Technol. 2012, 46, 49–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liddell, K.; Simon, D.A.; Lucassen, A. Patient data ownership: Who owns your health? J. Law Biosci. 2021, 8, lsab023. [Google Scholar] [CrossRef] [PubMed]
- Akbar, S.; Coiera, E.; Magrabi, F. Safety concerns with consumer-facing mobile health applications and their consequences: A scoping review. J. Am. Med. Inform. Assoc. 2019, 27, 330–340. [Google Scholar] [CrossRef] [Green Version]
- Holl, F.; Swoboda, W. Methods to Measure the Impact of mHealth Applications: Preliminary Results of a Scoping Review. Stud. Health Technol. Inform. 2018, 251, 285–288. [Google Scholar]
- Dugas, C.; Slane, V.H. Miscarriage. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Keep, M. The silence around miscarriage hurts healthcare and bereaved parents. Med. J. Aust. 2021, 215, 343–344. [Google Scholar] [CrossRef]
- Lupton, D.; Thomas, G.M. Playing Pregnancy: The Ludification and Gamification of Expectant Motherhood in Smartphone Apps. M/C J. 2015, 18, 1–3. [Google Scholar] [CrossRef]
- Bondaronek, P.; AlKhaldi, G.; Slee, A.; Hamilton, F.L.; Murray, E.; Lumsden, J.; Atherton, H. Quality of Publicly Available Physical Activity Apps: Review and Content Analysis. JMIR mHealth uHealth 2018, 6, e53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biviji, R.; Vest, J.R.; Dixon, B.E.; Cullen, T.; Harle, C.A. Factors Related to User Ratings and User Downloads of Mobile Apps for Maternal and Infant Health: Cross-Sectional Study. JMIR mHealth uHealth 2020, 8, e15663. [Google Scholar] [CrossRef]



| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Cost: free, freemium, and paid Availability: apps available on Apple App Store and/or Google Play Store App popularity: apps with an average user rating of and user ratings of at least 20 App focus: apps designed for pregnancy; monitoring of physical health or wellness during pregnancy App features: includes more than one monitoring tool | Cost: no apps were excluded based on their cost. If an app had a free and paid version, the free version was downloaded and tested first. If the paid version allowed for additional self-monitoring app features, the app account was upgraded. App focus: apps designed to focus essentially on fertility, postpartum, or for baby monitoring; apps that did not include features to monitor physical health or wellness or behaviours during pregnancy. App features: app includes no or only one monitoring tool. Apps including just kick or contraction counters were excluded. |
| App Name | A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | Total /15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ovia Pregnancy Tracker | 14 | |||||||||||||||
| Glow/Nurture Tracker | 10 | |||||||||||||||
| Woman’s Pregnancy | 9 | |||||||||||||||
| Pregnancy Tracker-Wachanga | 9 | |||||||||||||||
| Velmio Pregnancy Tracker | 8 | |||||||||||||||
| AMMA Pregnancy Tracker | 7 | |||||||||||||||
| WebMD Pregnancy | 7 | |||||||||||||||
| myFetalLife | 6 | |||||||||||||||
| Baby2Body Pregnancy | 6 | |||||||||||||||
| Pregnancy-Krishnu | 5 | |||||||||||||||
| 280 days Pregnancy | 5 | |||||||||||||||
| MomDiary | 5 | |||||||||||||||
| Pregnancy Tracker-Momly | 5 | |||||||||||||||
| Pregnancy-Sevenlogics | 5 | |||||||||||||||
| Sprout Pregnancy | 5 | |||||||||||||||
| Stork Pregnancy Tracker | 5 | |||||||||||||||
| Babynote Pregnancy | 4 | |||||||||||||||
| Hello Belly | 4 | |||||||||||||||
| Pregnancy App-Amila Tech | 4 | |||||||||||||||
| Pregnancy Companion | 4 | |||||||||||||||
| Pregnancy+ | 4 | |||||||||||||||
| Happy Pregnancy Ticker | 3 | |||||||||||||||
| Pregnancy Week-Promotube | 3 | |||||||||||||||
| Pregnancy Tracker-Enes | 3 | |||||||||||||||
| BabyCentre | 2 | |||||||||||||||
| My Pregnancy-Aleksei | 2 | |||||||||||||||
| Pregnancy Tracker-Hylal | 2 | |||||||||||||||
| Pregnancy Week-Paydos | 2 | |||||||||||||||
| Pregnancy Tracker-Timskiy | 2 | |||||||||||||||
| Pregnancy Tracker-FitnessLab | 2 | |||||||||||||||
| Pregnancy Tracker-Fittur | 2 |
| App Name | Total Scorecard Score (avg %) | Scorecard Rating /5 | Global App Store Rating /5 | Domain Score (avg %) | Behaviour Change Techniques Score (avg %) |
|---|---|---|---|---|---|
| Baby2Body | 62.6 | 3.1 | 4.7 | 62.3 | 63.0 |
| Ovia Pregnancy Tracker | 58.5 | 2.9 | 4.9 | 68.0 | 49.0 |
| Velmio Pregnancy Tracker | 48.7 | 2.5 | 4.9 | 42.5 | 55.0 |
| Pregnancy Tracker ~Fittur | 46.4 | 2.3 | 4.9 | 32.7 | 60.0 |
| Woman’s Pregnancy | 44.8 | 2.2 | 4.6 | 54.6 | 35.0 |
| WebMD Pregnancy | 43.8 | 2.2 | 4.5 | 59.6 | 28.0 |
| Glow/Nurture Tracker | 40.6 | 2.0 | 4.8 | 52.1 | 29.0 |
| Pregnancy Tracker—Wachanga | 39.1 | 2.0 | 4.7 | 43.1 | 35.0 |
| Pregnancy+ | 37.8 | 1.9 | 4.8 | 50.6 | 25.0 |
| AMMA Pregnancy Tracker | 33.9 | 1.7 | 4.7 | 44.8 | 23.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lazarevic, N.; Lecoq, M.; Bœhm, C.; Caillaud, C. Pregnancy Apps for Self-Monitoring: Scoping Review of the Most Popular Global Apps Available in Australia. Int. J. Environ. Res. Public Health 2023, 20, 1012. https://doi.org/10.3390/ijerph20021012
Lazarevic N, Lecoq M, Bœhm C, Caillaud C. Pregnancy Apps for Self-Monitoring: Scoping Review of the Most Popular Global Apps Available in Australia. International Journal of Environmental Research and Public Health. 2023; 20(2):1012. https://doi.org/10.3390/ijerph20021012
Chicago/Turabian StyleLazarevic, Natasa, Marie Lecoq, Céline Bœhm, and Corinne Caillaud. 2023. "Pregnancy Apps for Self-Monitoring: Scoping Review of the Most Popular Global Apps Available in Australia" International Journal of Environmental Research and Public Health 20, no. 2: 1012. https://doi.org/10.3390/ijerph20021012
APA StyleLazarevic, N., Lecoq, M., Bœhm, C., & Caillaud, C. (2023). Pregnancy Apps for Self-Monitoring: Scoping Review of the Most Popular Global Apps Available in Australia. International Journal of Environmental Research and Public Health, 20(2), 1012. https://doi.org/10.3390/ijerph20021012






