How and When May Technostress Impact Workers’ Psycho-Physical Health and Work-Family Interface? A Study during the COVID-19 Pandemic in Italy
Abstract
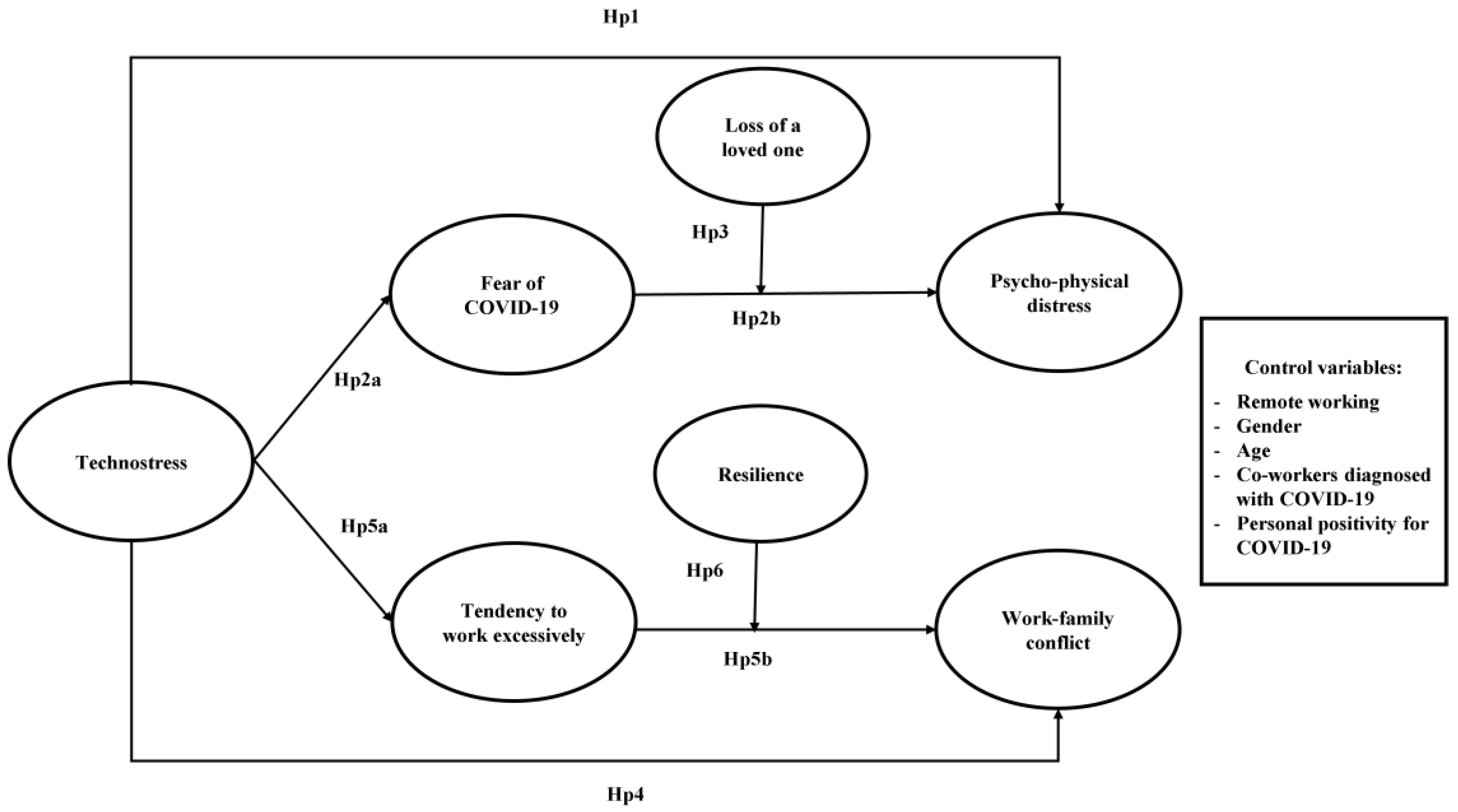
:1. Introduction
1.1. Technostress and Psycho-Physical Distress
1.2. Technostress and Work-Family Conflict
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measurements
3. Results
3.1. Descriptive Analyses
3.2. Independent T-Test Analyses and Analyses of Variance
3.3. Confirmatory Factor Analyses and Assessment of Common Method Bias
3.4. Hypotheses Testing
4. Discussion
Limitations and Future Research Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Maitland, A.; Thomson, P. Future Work: Changing Organizational Culture for the New World of Work, 2nd ed.; Palgrave Macmillan: Basingstoke, UK, 2014; ISBN 978-1-137-36715-0. [Google Scholar]
- International Labour Organization (ILO). Teleworking during the COVID-19 Pandemic and beyond: A Practical Guide; International Labour Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Sostero, M.; Milasi, S.; Hurley, J.; Fernandez-Macías, E.; Bisello, M. Teleworkability and the COVID-19 Crisis: A New Digital Divide? European Commission: Seville, Spain, 2020. [Google Scholar]
- Fukushima, N.; Machida, M.; Kikuchi, H.; Amagasa, S.; Hayashi, T.; Odagiri, Y.; Takamiya, T.; Inoue, S. Associations of working from home with occupational physical activity and sedentary behavior under the COVID-19 pandemic. J. Occup. Health 2021, 63, e12212. [Google Scholar] [CrossRef] [PubMed]
- De’, R.; Pandey, N.; Pal, A. Impact of digital surge during COVID-19 pandemic: A viewpoint on research and practice. Int. J. Inf. Manag. 2020, 55, 102171. [Google Scholar] [CrossRef] [PubMed]
- Javaid, M.; Haleem, A.; Vaishya, R.; Bahl, S.; Suman, R.; Vaish, A. Industry 4.0 technologies and their applications in fighting COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 419–422. [Google Scholar] [CrossRef] [PubMed]
- Eurofound Living, Working and COVID-19 Data. Available online: https://www.eurofound.europa.eu/data/covid-19 (accessed on 27 November 2022).
- Molino, M.; Ingusci, E.; Signore, F.; Manuti, A.; Giancaspro, M.L.; Russo, V.; Zito, M.; Cortese, C.G. Wellbeing Costs of Technology Use during COVID-19 Remote Working: An Investigation Using the Italian Translation of the Technostress Creators Scale. Sustainability 2020, 12, 5911. [Google Scholar] [CrossRef]
- Bloom, N.; Liang, J.; Roberts, J.; Ying, Z.J. Does Working from Home Work? Evidence from a Chinese Experiment. Q. J. Econ. 2014, 130, 165–218. [Google Scholar] [CrossRef] [Green Version]
- Buomprisco, G.; Ricci, S.; Perri, R.; De Sio, S. Health and Telework: New Challenges after COVID-19 Pandemic. Eur. J. Environ. Public Health 2021, 5, em0073. [Google Scholar] [CrossRef]
- Gajendran, R.S.; Harrison, D.A. The good, the bad, and the unknown about telecommuting: Meta-analysis of psychological mediators and individual consequences. J. Appl. Psychol. 2007, 92, 1524–1541. [Google Scholar] [CrossRef] [Green Version]
- Broughton, A.; Battaglini, M. Teleworking during the COVID-19 Pandemic: Risks and Prevention Strategies. 2021. Available online: https://osha.europa.eu/en/publications/teleworking-during-covid-19-pandemic-risks-and-prevention-strategies (accessed on 27 November 2022).
- La Torre, G.; Esposito, A.; Sciarra, I.; Chiappetta, M. Definition, symptoms and risk of techno-stress: A systematic review. Int. Arch. Occup. Environ. Health 2018, 92, 13–35. [Google Scholar] [CrossRef]
- Ragu-Nathan, T.S.; Tarafdar, M.; Ragu-Nathan, B.S.; Tu, Q. The Consequences of Technostress for End Users in Organizations: Conceptual Development and Empirical Validation. Inf. Syst. Res. 2008, 19, 417–433. [Google Scholar] [CrossRef] [Green Version]
- Rey-Merchán, M.D.C.; López-Arquillos, A. Occupational Risk of Technostress Related to the Use of ICT among Teachers in Spain. Sustainability 2022, 14, 8746. [Google Scholar] [CrossRef]
- Brod, C. Technostress: The Human Cost of the Computer Revolution; Addison-Wesley: Reading, MA, USA, 1984; ISBN 978-0-201-11211-5. [Google Scholar]
- Arnetz, B.B.; Wiholm, C. Technological stress: Psychophysiological symptoms in modern offices. J. Psychosom. Res. 1997, 43, 35–42. [Google Scholar] [CrossRef]
- Day, A.; Paquet, S.; Scott, N.; Hambley, L. Perceived information and communication technology (ICT) demands on employee outcomes: The moderating effect of organizational ICT support. J. Occup. Health Psychol. 2012, 17, 473–491. [Google Scholar] [CrossRef]
- Salanova, M.; Llorens, S.; Cifre, E. The dark side of technologies: Technostress among users of information and communication technologies. Int. J. Psychol. 2013, 48, 422–436. [Google Scholar] [CrossRef] [Green Version]
- International Labour Organization (ILO). The Impact of Technology on the Quality and Quantity of Jobs; International Labour Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Day, A.; Scott, N.; Kelloway, E.K. Information and communication technology: Implications for job stress and employee well-being. New Dev. Theor. Concept. Approaches Job Stress 2010, 8, 317–350. [Google Scholar] [CrossRef]
- Oklar, A.N.; Sahin, Y.L. Technostress Levels of Social Network Users Based on ICTs in Turkey. Eur. J. Soc. Sci. 2011, 23, 171–182. [Google Scholar]
- Tarafdar, M.; Tu, Q.; Ragu-Nathan, B.S.; Ragu-Nathan, T.S. The Impact of Technostress on Role Stress and Productivity. J. Manag. Inf. Syst. 2007, 24, 301–328. [Google Scholar] [CrossRef] [Green Version]
- Nam, T. Technology Use and Work-Life Balance. Appl. Res. Qual. Life 2014, 9, 1017–1040. [Google Scholar] [CrossRef]
- Mahapatra, M.; Pati, S.P. Technostress Creators and Burnout: A Job Demands-Resources Perspective. In Proceedings of the 2018 ACM SIGMIS Conference on Computers and People Research, Buffalo-Niagara Falls, NY, USA, 18–20 June 2018; pp. 70–77. [Google Scholar]
- Borle, P.; Reichel, K.; Niebuhr, F.; Voelter-Mahlknecht, S. How Are Techno-Stressors Associated with Mental Health and Work Outcomes? A Systematic Review of Occupational Exposure to Information and Communication Technologies within the Technostress Model. Int. J. Environ. Res. Public Health 2021, 18, 8673. [Google Scholar] [CrossRef]
- Finstad, G.L.; Giorgi, G. The technostress questionnaire: A pilot study. J. Adv. Health Care 2021, 3, 1–11. [Google Scholar] [CrossRef]
- Brown, R.; Duck, J.; Jimmieson, N. E-mail in the workplace: The role of stress appraisals and normative response pressure in the relationship between e-mail stressors and employee strain. Int. J. Stress Manag. 2014, 21, 325–347. [Google Scholar] [CrossRef]
- Brillhart, P.E. Technostress in the workplace: Managing stress in the electronic workplace. J. Am. Acad. Bus. 2004, 5, 302–330. [Google Scholar]
- Salo, M.; Pirkkalainen, H.; Koskelainen, T. Technostress and social networking services: Explaining users’ concentration, sleep, identity, and social relation problems. Inf. Syst. J. 2018, 29, 408–435. [Google Scholar] [CrossRef]
- Harper, S. Managing technostress in UK libraries: A realistic guide. Ariadne 2000, 25, 18–21. [Google Scholar]
- Galluch, P.S.; Grover, V.; Thatcher, J.B. Interrupting the workplace: Examining stressors in an information technology context. J. Assoc. Inf. Syst. 2015, 16, 1–47. [Google Scholar] [CrossRef]
- Riedl, R. On the biology of technostress. ACM SIGMIS Database Database Adv. Inf. Syst. 2012, 44, 18–55. [Google Scholar] [CrossRef]
- Giorgi, G.; Lecca, L.I.; Alessio, F.; Finstad, G.L.; Bondanini, G.; Lulli, L.G.; Arcangeli, G.; Mucci, N. COVID-19-Related Mental Health Effects in the Workplace: A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 7857. [Google Scholar] [CrossRef]
- Yuen, K.F.; Wang, X.; Ma, F.; Li, K.X. The Psychological Causes of Panic Buying Following a Health Crisis. Int. J. Environ. Res. Public Health 2020, 17, 3513. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2022, 20, 1537–1545. [Google Scholar] [CrossRef] [Green Version]
- Harper, C.A.; Satchell, L.P.; Fido, D.; Latzman, R.D. Functional Fear Predicts Public Health Compliance in the COVID-19 Pandemic. Int. J. Ment. Health Addict. 2020, 19, 1875–1888. [Google Scholar] [CrossRef]
- Coelho, C.M.; Suttiwan, P.; Arato, N.; Zsido, A.N. On the Nature of Fear and Anxiety Triggered by COVID-19. Front. Psychol. 2020, 11, 581314. [Google Scholar] [CrossRef]
- Şimşir, Z.; Koç, H.; Seki, T.; Griffiths, M.D. The relationship between fear of COVID-19 and mental health problems: A meta-analysis. Death Stud. 2021, 46, 515–523. [Google Scholar] [CrossRef]
- Bukhari, E.E.; Temsah, M.H.; A Aleyadhy, A.; A Alrabiaa, A.; Alhboob, A.A.; Jamal, A.; A BinSaeed, A. Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak perceptions of risk and stress evaluation in nurses. J. Infect. Dev. Ctries. 2016, 10, 845–850. [Google Scholar] [CrossRef] [Green Version]
- Mertens, G.; Gerritsen, L.; Duijndam, S.; Salemink, E.; Engelhard, I.M. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. J. Anxiety Disord. 2020, 74, 102258. [Google Scholar] [CrossRef]
- Dymecka, J.; Filipkowski, J.; Machnik-Czerwik, A. Fear of COVID-19: Stress and job satisfaction among Polish doctors during the pandemic. Adv. Psychiatry Neurol. 2021, 30, 243–250. [Google Scholar] [CrossRef]
- Satici, S.A.; Kayis, A.R.; Satici, B.; Griffiths, M.D.; Can, G. Resilience, Hope, and Subjective Happiness among the Turkish Population: Fear of COVID-19 as a Mediator. Int. J. Ment. Health Addict. 2020, 1–16. [Google Scholar] [CrossRef]
- Morales-Rodríguez, F.M. Fear, Stress, Resilience and Coping Strategies during COVID-19 in Spanish University Students. Sustainability 2021, 13, 5824. [Google Scholar] [CrossRef]
- Savolainen, I.; Oksa, R.; Savela, N.; Celuch, M.; Oksanen, A. COVID-19 Anxiety—A Longitudinal Survey Study of Psychological and Situational Risks among Finnish Workers. Int. J. Environ. Res. Public Health 2021, 18, 794. [Google Scholar] [CrossRef]
- Raio, C.M.; Orederu, T.A.; Palazzolo, L.; Shurick, A.A.; Phelps, E.A. Cognitive emotion regulation fails the stress test. Proc. Natl. Acad. Sci. USA 2013, 110, 15139–15144. [Google Scholar] [CrossRef] [Green Version]
- Golkar, A.; Johansson, E.; Kasahara, M.; Osika, W.; Perski, A.; Savic, I. The Influence of Work-Related Chronic Stress on the Regulation of Emotion and on Functional Connectivity in the Brain. PLoS ONE 2014, 9, e104550. [Google Scholar] [CrossRef] [Green Version]
- Lazarus, R.S. Relational Meaning and Discrete Emotions. In Appraisal Processes in Emotion: Theory, Methods, Research; Series in Affective Science; Oxford University Press: New York, NY, USA, 2001; pp. 37–67. ISBN 0-19-513007-3. [Google Scholar]
- Galanti, T.; Guidetti, G.; Mazzei, E.; Zappalà, S.; Toscano, F. Work from Home during the COVID-19 Outbreak. J. Occup. Environ. Med. 2021, 63, e426–e432. [Google Scholar] [CrossRef]
- Gordillo, F.; Mestas, L.; Arana, J.M.; Pérez, M.; Escotto, E.A. The effect of mortality salience and type of life on personality evaluation. Eur. J. Psychol. 2017, 13, 286–299. [Google Scholar] [CrossRef] [PubMed]
- Cavanaugh, M.A.; Boswell, W.R.; Roehling, M.V.; Boudreau, J.W. An empirical examination of self-reported work stress among US man-agers. J. Appl. Psychol. 2000, 85, 65–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: Berlin/Heidelberg, Germany, 1984. [Google Scholar]
- Mawritz, M.B.; Folger, R.; Latham, G.P. Supervisors’ exceedingly difficult goals and abusive supervision: The mediating effects of hindrance stress, anger, and anxiety. J. Organ. Behav. 2013, 35, 358–372. [Google Scholar] [CrossRef]
- Searle, B.J.; Auton, J. The merits of measuring challenge and hindrance appraisals. Anxiety Stress. Coping 2014, 28, 121–143. [Google Scholar] [CrossRef] [PubMed]
- Webster, J.R.; Beehr, T.A.; Love, K. Extending the challenge-hindrance model of occupational stress: The role of appraisal. J. Vocat. Behav. 2011, 79, 505–516. [Google Scholar] [CrossRef]
- Mahmud, S.; Talukder, M.U.; Rahman, S.M. Does ‘Fear of COVID-19’ trigger future career anxiety? An empirical investigation considering depression from COVID-19 as a mediator. Int. J. Soc. Psychiatry 2020, 67, 35–45. [Google Scholar] [CrossRef]
- Satici, B.; Saricali, M.; Satici, S.A.; Griffiths, M.D. Intolerance of uncertainty and mental wellbeing: Serial mediation by rumi-nation and fear of COVID-19. Int. J. Ment. Health Addict. 2022, 20, 2731–2742. [Google Scholar] [CrossRef]
- Sun, J.; Wu, T.; Chen, B. Fear of Virus or of Competitors? The Decision Rationales of Financial Managers under COVID-19. Front. Psychol. 2020, 11, 556139. [Google Scholar] [CrossRef]
- Pyszczynski, T.; Lockett, M.; Greenberg, J.; Solomon, S. Terror Management Theory and the COVID-19 Pandemic. J. Humanist. Psychol. 2020, 61, 173–189. [Google Scholar] [CrossRef]
- Eisma, M.C.; Tamminga, A.; Smid, G.E.; Boelen, P.A. Acute grief after deaths due to COVID-19, natural causes and unnatural causes: An empirical comparison. J. Affect. Disord. 2020, 278, 54–56. [Google Scholar] [CrossRef]
- Joaquim, R.M.; Pinto, A.L.; Guatimosim, R.F.; de Paula, J.J.; Costa, D.S.; Diaz, A.P.; da Silva, A.G.; Pinheiro, M.I.; Serpa, A.L.; Miranda, D.M.; et al. Bereavement and psychological distress during COVID-19 pandemics: The impact of death experience on mental health. Curr. Res. Behav. Sci. 2021, 2, 100019. [Google Scholar] [CrossRef]
- Mousavi, S.A.-M.; Hooshyari, Z.; Ahmadi, A. The Most Stressful Events during the COVID-19 Epidemic. Iran. J. Psychiatry 2020, 15, 220–227. [Google Scholar] [CrossRef]
- Gersons, B.P.R.; Smid, G.E.; Smit, A.S.; Kazlauskas, E.; McFarlane, A. Can a ‘second disaster’ during and after the COVID-19 pandemic be mitigated? Eur. J. Psychotraumatol. 2020, 11, 1–5. [Google Scholar] [CrossRef]
- Kahn, R.; Wolfe, D.; Quinn, R.; Snoek, J.; Rosenthai, R. Organizational Stress: Studies in Role Conflict and Ambiguity; Wiley: New York, NY, USA, 1964. [Google Scholar]
- Greenhaus, J.H.; Beutell, N.J. Sources of Conflict between Work and Family Roles. Acad. Manag. Rev. 1985, 10, 76. [Google Scholar] [CrossRef]
- Bernuzzi, C.; Sommovigo, V.; Setti, I. The role of resilience in the work-life interface: A systematic review. Work 2022, 73, 1147–1165. [Google Scholar] [CrossRef]
- Loscalzo, Y.; Raffagnino, R.; Gonnelli, C.; Giannini, M. Work–Family Conflict Scale: Psychometric Properties of the Italian Version. SAGE Open 2019, 9, 1–12. [Google Scholar] [CrossRef]
- Leung, L.; Zhang, R. Mapping ICT use at home and telecommuting practices: A perspective from work/family border theory. Telemat. Inform. 2017, 34, 385–396. [Google Scholar] [CrossRef]
- Vaziri, H.; Casper, W.J.; Wayne, J.H.; Matthews, R.A. Changes to the work–family interface during the COVID-19 pandemic: Examining predictors and implications using latent transition analysis. J. Appl. Psychol. 2020, 105, 1073–1087. [Google Scholar] [CrossRef]
- Harris, K.J.; Harris, R.B.; Valle, M.; Carlson, J.; Carlson, D.S.; Zivnuska, S.; Wiley, B. Technostress and the entitled employee: Impacts on work and family. Inf. Technol. People 2021, 35, 1073–1095. [Google Scholar] [CrossRef]
- Harris, K.J.; Harris, R.B.; Carlson, J.R.; Carlson, D.S. Resource loss from technology overload and its impact on work-family conflict: Can leaders help? Comput. Hum. Behav. 2015, 50, 411–417. [Google Scholar] [CrossRef]
- Hobfoll, S.E.; Freedy, J. Conservation of Resources: A General Stress Theory Applied to Burnout. In Professional Burnout; Routledge: London, UK, 2017; pp. 115–129. [Google Scholar]
- Ayyagari, R.; Grover, V.; Purvis, R. Technostress: Technological Antecedents and Implications. MIS Q. 2011, 35, 831–858. [Google Scholar] [CrossRef] [Green Version]
- Derks, D.; Van Duin, D.; Tims, M.; Bakker, A.B. Smartphone use and work-home interference: The moderating role of social norms and employee work engagement. J. Occup. Organ. Psychol. 2014, 88, 155–177. [Google Scholar] [CrossRef]
- Dragano, N.; Lunau, T. Technostress at work and mental health: Concepts and research results. Curr. Opin. Psychiatry 2020, 33, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Dierdorff, E.C.; Ellington, J.K. It’s the nature of the work: Examining behavior-based sources of work-family conflict across occupations. J. Appl. Psychol. 2008, 93, 883. [Google Scholar] [CrossRef] [PubMed]
- Robinson, B.E. The Psychosocial and Familial Dimensions of Work Addiction: Preliminary Perspectives and Hypotheses. J. Couns. Dev. 1996, 74, 447–452. [Google Scholar] [CrossRef]
- Spagnoli, P.; Balducci, C.; Fabbri, M.; Molinaro, D.; Barbato, G. Workaholism, intensive smartphone use, and the sleep-wake cycle: A multiple mediation analysis. Int. J. Environ. Res. Public Health 2019, 16, 3517. [Google Scholar] [CrossRef] [Green Version]
- Porter, G.; Kakabadse, N.K. HRM perspectives on addiction to technology and work. J. Manag. Dev. 2006, 25, 535–560. [Google Scholar] [CrossRef]
- Spagnoli, P.; Molino, M.; Molinaro, D.; Giancaspro, M.L.; Manuti, A.; Ghislieri, C. Workaholism and technostress during the COVID-19 emergency: The crucial role of the leaders on remote working. Front. Psychol. 2020, 11, 620310. [Google Scholar] [CrossRef]
- Di Stefano, G.; Gaudiino, M. Workaholism and work engagement: How are they similar? How are they different? A systematic review and meta-analysis. Eur. J. Work. Organ. Psychol. 2019, 28, 329–347. [Google Scholar] [CrossRef]
- Krumov, K.D.; Larsen, K.S.; Liu, J.; Schneider, J.F.; Kemmelmeier, M.; Krumova, A.K.; Widodo, E.; Gungov, A.L.; Juhasz, M.; Garvanova, M.Z.; et al. Workaholism across European and Asian cultures during the COVID-19 pandemic. PsyCh J. 2022, 11, 85–96. [Google Scholar] [CrossRef]
- Huyghebaert, T.; Fouquereau, E.; Lahiani, F.-J.; Beltou, N.; Gimenes, G.; Gillet, N. Examining the longitudinal effects of workload on ill-being through each dimension of workaholism. Int. J. Stress Manag. 2018, 25, 144–162. [Google Scholar] [CrossRef]
- Braun, A.C.; Machado, W.D.L.; De Andrade, A.L.; De Oliveira, M.Z. Why work-family conflict can drive your executives away? Rev. De Psicol. 2019, 37, 251–278. [Google Scholar] [CrossRef] [Green Version]
- Bernuzzi, C.; Setti, I.; Maffoni, M.; Sommovigo, V. From moral distress to burnout through work-family conflict: The protective role of resilience and positive refocusing. Ethic.-Behav. 2022, 32, 578–600. [Google Scholar] [CrossRef]
- Grandey, A.A.; Cropanzano, R. The Conservation of Resources Model Applied to Work–Family Conflict and Strain. J. Vocat. Behav. 1999, 54, 350–370. [Google Scholar] [CrossRef] [Green Version]
- Di Fabio, A.; Palazzeschi, L. Connor-Davidson Resilience Scale: Proprietà Psicometriche Della Versione Italiana [Connor-Davidson Resilience Scale: Psychometric Properties of the Italian Version]. G. Ital. Ric. Appl. 2012, 5, 101–110. [Google Scholar]
- Balducci, C.; Avanzi, L.; Consiglio, C.; Fraccaroli, F.; Schaufeli, W. A Cross-National Study on the Psychometric Quality of the Italian Version of the Dutch Work Addiction Scale (DUWAS). Eur. J. Psychol. Assess. 2017, 33, 422–428. [Google Scholar] [CrossRef]
- Colombo, L.; Ghisleri, C. The Work-to-Family Conflict: Theories and Measures. TPM-Test. Psychom. Methodol. Appl. Psychol. 2008, 15, 35–55. [Google Scholar]
- Fraccaroli, F.; Depolo, M.; Sarchielli, G. L’uso Del General Health Questionnaire Di Goldberg in Una Ricerca Su Giovani Disoccupati. [The Use of Goldberg’s General Health Questionnaire in a Study of Unemployed Young People.]. Giunti Organ. Spec. 1991, 197, 13–19. [Google Scholar]
- Soraci, P.; Ferrari, A.; Abbiati, F.A.; Del Fante, E.; De Pace, R.; Urso, A.; Griffiths, M.D. Validation and Psychometric Evaluation of the Italian Version of the Fear of COVID-19 Scale. Int. J. Ment. Health Addict. 2022, 20, 1913–1922. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedics sciences. Behav. Res. Methods. 2007, 39, 175–191. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows, Version 25.0; IBM Corp: Armonk, NY, USA, 2017. [Google Scholar]
- Podsakoff, P.M.; MacKenzie, S.B.; Podsakoff, N.P. Sources of method bias in social science research and recommendations on how to control it. Annu. Rev. Psychol. 2012, 63, 539–569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hughes, D.; Fairley, A. The COVID chronicles: An Employee Assistance Program’s observations and responses to the pandemic. J. Work. Behav. Health 2021, 36, 177–196. [Google Scholar] [CrossRef]
- Keyes, K.M.; Pratt, C.; Galea, S.; McLaughlin, K.; Koenen, K.C.; Shear, M.K. The Burden of Loss: Unexpected Death of a Loved One and Psychiatric Disorders Across the Life Course in a National Study. Am. J. Psychiatry 2014, 171, 864–871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohammadi, F.; Oshvandi, K.; Shamsaei, F.; Cheraghi, F.; Khodaveisi, M.; Bijani, M. The mental health crises of the families of COVID-19 victims: A qualitative study. BMC Fam. Pract. 2021, 22, 94. [Google Scholar] [CrossRef] [PubMed]
- Ghislieri, C.; Molino, M.; Dolce, V.; Sanseverino, D.; Presutti, M. Work-family conflict during the COVID-19 pandemic: Teleworking of administrative and technical staff in healthcare. An Italian study: Work-family conflict during the COVID-19 pandemic in healthcare. La Med. del Lav. 2021, 112, 229–240. [Google Scholar] [CrossRef]
- Signore, F.; Cortese, C.G.; Parisi, S.; Russo, V.; Zito, M.; Ingusci, E. Job crafting e benessere lavorativo: Un’indagine esplorativa nel periodo dell’emergenza sanitaria. Med. Lav. 2020, 111, 478–492. [Google Scholar] [CrossRef]
- Srivastava, S.C.; Chandra, S.; Shirish, A. Technostress creators and job outcomes: Theorising the moderating influence of personality traits. Inf. Syst. J. 2015, 25, 355–401. [Google Scholar] [CrossRef]
- Suh, A.; Lee, J. Understanding teleworkers’ technostress and its influence on job satisfaction. Internet Res. 2017, 27, 140–159. [Google Scholar] [CrossRef]
- Cramton, C.D. The Mutual Knowledge Problem and Its Consequences for Dispersed Collaboration. Organ. Sci. 2001, 12, 346–371. [Google Scholar] [CrossRef] [Green Version]
- Kanawattanachai, P.; Yoo, Y. The impact of knowledge coordination on virtual team performance over time. MIS Q. 2007, 31, 783–808. [Google Scholar] [CrossRef] [Green Version]
- Toscano, F.; Zappalà, S. Social Isolation and Stress as Predictors of Productivity Perception and Remote Work Satisfaction during the COVID-19 Pandemic: The Role of Concern about the Virus in a Moderated Double Mediation. Sustainability 2020, 12, 9804. [Google Scholar] [CrossRef]
- Borelli, J.L.; Nelson, S.K.; River, L.M.; Birken, S.A.; Moss-Racusin, C. Gender Differences in Work-Family Guilt in Parents of Young Children. Sex Roles 2016, 76, 356–368. [Google Scholar] [CrossRef]
- Del Boca, D.; Oggero, N.; Profeta, P.; Rossi, M. Women’s and Men’s Work, Housework and Childcare, before and during COVID-19. Rev. Econ. Househ. 2020, 18, 1001–1017. [Google Scholar] [CrossRef]
- Risi, E.; Pronzato, R. Smart working is not so smart: Always-on lives and the dark side o platformisation. Work. Organ. Labour Glob. 2021, 15, 107–125. [Google Scholar] [CrossRef]
- Sommovigo, V.; Bernuzzi, C.; Setti, I. Investigating the association between patient verbal aggression and emotional exhaustion among Italian health care professionals during the COVID-19 pandemic. J. Nurs. Manag. 2022, 30, 1713–1723. [Google Scholar] [CrossRef]
- Chen, C.Y.-C.; Byrne, E.; Vélez, T. A Preliminary Study of COVID-19-related Stressors, Parenting Stress, and Parental Psychological Well-being Among Parents of School-age Children. J. Child Fam. Stud. 2022, 31, 1558–1569. [Google Scholar] [CrossRef]
- Miller, K.E.; Riley, J. Changed Landscape, Unchanged Norms: Work-Family Conflict and the Persistence of the Academic Mother Ideal. Innov. High. Educ. 2022, 47, 471–492. [Google Scholar] [CrossRef]
- Sasaki, R.; Ota, A.; Yatsuya, H.; Tabuchi, T. Gender Difference in Fear and Anxiety about and Perceived Susceptibility to COVID-19 in the Third Wave of Pandemic among the Japanese General Population: A Nationwide Web-Based Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2022, 19, 16239. [Google Scholar] [CrossRef]
- Mazzucchelli, O.; Manzi, C.; Lamastra, C.R. Women’s Working Conditions during COVID-19: A Review of the Literature and a Research Agenda. Soc. Sci. 2022, 11, 539. [Google Scholar] [CrossRef]
- Alsharawy, A.; Spoon, R.; Smith, A.; Ball, S. Gender differences in fear and risk perception during the COVID-19 pandemic. Front. Psychol. 2021, 12, 699467. [Google Scholar] [CrossRef]
- Shaukat, S.; Bendixen, L.D.; Ayub, N. The Impact of Technostress on Teacher Educators’ Work–Family Conflict and Life Satisfaction While Working Remotely during COVID-19 in Pakistan. Educ. Sci. 2022, 12, 616. [Google Scholar] [CrossRef]
- Salthouse, T.A. Individual differences in working memory and aging. In Working Memory and Ageing; Logie, R.H., Morris, R.G., Eds.; Psychology Press: London, UK, 2014; pp. 17–36. [Google Scholar]
- Prensky, M. Digital Natives, Digital Immigrants Part 2: Do They Really Think Differently? Horizon 2001, 9, 1–6. [Google Scholar] [CrossRef]
- Daoust, J.-F. Elderly people and responses to COVID-19 in 27 Countries. PLoS ONE 2020, 15, e0235590. [Google Scholar] [CrossRef] [PubMed]
- Pearman, A.; Hughes, M.L.; Smith, E.L.; Neupert, S.D. Age Differences in Risk and Resilience Factors in COVID-19-Related Stress. J. Gerontol. Ser. B 2021, 76, e38–e44. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Bala, H.; Dey, B.L.; Filieri, R. Enforced remote working: The impact of digital platform-induced stress and remote working ex-perience on technology exhaustion and subjective wellbeing. J. Bus. Res. 2022, 151, 269–286. [Google Scholar] [CrossRef]
- Oksanen, A.; Oksa, R.; Savela, N.; Mantere, E.; Savolainen, I.; Kaakinen, M. COVID-19 crisis and digital stressors at work: A longitudinal study on the Finnish working population. Comput. Hum. Behav. 2021, 122, 106853. [Google Scholar] [CrossRef]
- Morkevičiūtė, M.; Endriulaitienė, A.; Poškus, M.S. Understanding the etiology of workaholism: The results of the systematic review and meta-analysis. J. Work. Behav. Health 2021, 36, 351–372. [Google Scholar] [CrossRef]
- Maffoni, M.; Fiabane, E.; Setti, I.; Martelli, S.; Pistarini, C.; Sommovigo, V. Moral Distress among Frontline Physicians and Nurses in the Early Phase of COVID-19 Pandemic in Italy. Int. J. Environ. Res. Public Health 2022, 19, 9682. [Google Scholar] [CrossRef]
- Chowdhury, R.; Shah, D.; Payal, A.R. Healthy worker effect phenomenon: Revisited with emphasis on statistical methods—A review. Indian J. Occup. Environ. Med. 2017, 21, 2–8. [Google Scholar] [CrossRef]
- Sommovigo, V.; Bernuzzi, C.; Setti, I. Helping others not always helps ourselves: The relationship between victim incivility and emergency workers’ burnout through work-to-family conflict. Int. J. Work. Health Manag. 2022, 15, 467–492. [Google Scholar] [CrossRef]
- Rego, F.; Sommovigo, V.; Setti, I.; Giardini, A.; Alves, E.; Morgado, J.; Maffoni, M. How Supportive Ethical Relationships Are Negatively Related to Palliative Care Professionals’ Negative Affectivity and Moral Distress: A Portuguese Sample. Int. J. Environ. Res. Public Health 2022, 19, 3863. [Google Scholar] [CrossRef]


| M | SD | Skewness | Kurtosis | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Remote working | - | - | - | - | - | |||||||||||||
| 2. Technostress | 2.31 | 0.90 | 0.52 | −0.46 | 0.25 ** | 0.88 | ||||||||||||
| 3. Fear of COVID-19 | 2.10 | 1.02 | 0.85 | 0.01 | 0.18 ** | 0.28 * | 0.91 | |||||||||||
| 4. Working excessively | 2.83 | 0.71 | −0.34 | −0.45 | 0.05 | 0.30 ** | 0.16 ** | 0.72 | ||||||||||
| 5. Psycho-physical distress | 1.14 | 0.67 | 0.71 | −0.06 | 0.10 | 0.27 ** | 0.42 ** | 0.20 ** | 0.89 | |||||||||
| 6. Work-family conflict | 3.49 | 1.61 | 0.23 | −0.82 | 0.09 | 0.50 ** | 0.27 ** | 0.46 ** | 0.35 ** | 0.89 | ||||||||
| 7. Resilience | 2.93 | 0.53 | −0.34 | −0.11 | −0.05 | 0.01 | −0.08 | 0.12 * | −0.35 ** | −0.03 | 0.80 | |||||||
| 8. Gender | - | - | - | - | 0.14 * | 0.05 | 0.23 ** | 0.15 * | 0.21 ** | 0.12 * | −0.21 ** | - | ||||||
| 9. Age | 39.40 | 12.26 | - | - | 0.17 * | 0.26 ** | 0.18 ** | −0.08 | −0.11 | 0.06 | 0.03 | 0.13 * | - | |||||
| 10. Being tested for COVID-19 | - | - | - | - | −0.06 | −0.01 | −0.07 | 0.07 | −0.01 | 0.06 | −0.04 | 0.09 | −0.03 | - | ||||
| 11. Personal positivity | - | - | - | - | −0.09 | 0.08 | 0.01 | 0.01 | 0.02 | 0.13 * | 0.11 | 0.03 | −0.12 | 0.25 ** | - | |||
| 12. Colleague’s positivity | - | - | - | - | 0.13 * | 0.14 * | 0.08 | −0.06 | 0.07 | 0.07 | 0.01 | 0.07 | 0.10 | 0.10 | 0.13 * | - | ||
| 13. Family/friends’ positivity | - | - | - | - | 0.09 | 0.09 | 0.09 | 0.08 | 0.09 | 0.08 | 0.04 | 0.08 | −0.06 | 0.08 | 0.19 ** | 0.25 ** | - | |
| 14. Loss of a loved one | - | - | - | - | −0.03 | 0.06 | 0.26 ** | 0.08 | 0.06 | 0.15 | 0.10 | 0.12 * | 0.10 | −0.06 | 0.10 | 0.20 ** | 0.18 ** | - |
| 15. Family working in healthcare | - | - | - | - | 0.01 | −0.01 | 0.04 | 0.07 | 0.07 | 0.11 | 0.07 | 0.03 | 0.03 | 0.17 ** | 0.13 * | 0.15 * | 0.29 ** | 0.03 |
| Model | χ2 | df | p | RMSEA | 90% RMSEA | SRMR | CFI | TLI |
|---|---|---|---|---|---|---|---|---|
| Six-factor model_meth n | 1781.860 | 1099 | 0.00 | 0.04 | [0.04, 0.05] | 0.05 | 0.90 | 0.90 |
| Six-factor model_mo m | 1970.061 | 1149 | 0.00 | 0.05 | [0.04, 0.06] | 0.07 | 0.90 | 0.90 |
| Six-factor model l | 2411.325 | 1160 | 0.00 | 0.06 | [0.06, 0.07] | 0.07 | 0.89 | 0.88 |
| Five-factor model2 i | 2538.719 | 1165 | 0.00 | 0.07 | [0.06, 0.07] | 0.07 | 0.78 | 0.77 |
| Five-factor model1 h | 3067.571 | 1165 | 0.00 | 0.08 | [0.07, 0.08] | 0.09 | 0.69 | 0.68 |
| Four-factor model2 g | 3241.569 | 1169 | 0.00 | 0.08 | [0.07, 0.08] | 0.09 | 0.67 | 0.65 |
| Four-factor model1 f | 3284.148 | 1169 | 0.00 | 0.08 | [0.08, 0.09] | 0.10 | 0.66 | 0.64 |
| Three-factor model2 e | 4138.958 | 1172 | 0.00 | 0.09 | [0.09, 0.10] | 0.12 | 0.52 | 0.50 |
| Three-factor model1 d | 4154.705 | 1172 | 0.00 | 0.10 | [0.09, 0.10] | 0.12 | 0.52 | 0.50 |
| Two-factor model 2 c | 4561.390 | 1174 | 0.00 | 0.10 | [0.10, 0.11] | 0.13 | 0.45 | 0.43 |
| Two-factor model 1 b | 4668.066 | 1174 | 0.00 | 0.11 | [0.10, 0.11] | 0.12 | 0.44 | 0.42 |
| One-factor model a | 5148.710 | 1175 | 0.00 | 0.11 | [0.10, 0.12] | 0.13 | 0.36 | 0.33 |
| Model (Outcome) | χ2 | df | p | RMSEA | SRMR | CFI | TLI |
|---|---|---|---|---|---|---|---|
| Model 1 | 1693.076 | 948 | 0.000 | 0.05 [0.05,0.06] | 0.07 | 0.90 | 0.90 |
| Standardized direct and indirect effects | |||||||
| Effects—Model 1 | Estimate | S.E. | 95% CI | ||||
| Remote working → Technostress | 0.23 ** | 0.07 | [0.09,0.39] | ||||
| Age → Technostress | 0.22 ** | 0.07 | [0.09,0.36] | ||||
| Colleagues positive for COVID-19 → Technostress | 0.06 | 0.07 | [−0.07,0.19] | ||||
| Age → Working excessively | −0.21 ** | 0.07 | [−0.36, −0.11] | ||||
| Gender → Working excessively | 0.17 * | 0.08 | [0.05,0.27] | ||||
| Working excessively → Work-family conflict | 0.45 *** | 0.07 | [0.31,0.58] | ||||
| Gender → Work-family conflict | 0.02 | 0.05 | [−0.09,0.13] | ||||
| COVID-19 positivity → Work-family conflict | 0.08 | 0.05 | [−0.01,0.18] | ||||
| Technostress → Work-family conflict | 0.36 *** | 0.07 | [0.23,0.50] | ||||
| Technostress → Working excessively | 0.43 *** | 0.07 | [0.13,0.64] | ||||
| Technostress → Working excessively → Work-family conflict | 0.17 * | 0.04 | [0.10,0.28] | ||||
| Total effects on work-family conflict | 0.56 *** | 0.06 | [0.44,0.68] | ||||
| Remote working → Fear of COVID-19 | 0.08 | 0.06 | [−0.03,0.20] | ||||
| Gender → Fear of COVID-19 | 0.17 ** | 0.06 | [0.05,0.29] | ||||
| Loss of loved ones → Psycho-physical distress | 0.59 *** | 0.19 | [0.36,0.66] | ||||
| Ag e→ Fear of COVID-19 | 0.07 | 0.06 | [−0.05,0.19] | ||||
| Fear of COVID-19 → Psycho-physical distress | 0.38 *** | 0.07 | [0.24,0.56] | ||||
| Gender → Psycho-physical distress | 0.16 ** | 0.06 | [0.05,0.27] | ||||
| Age → Psycho-physical distress | −0.23 *** | 0.06 | [−0.36, −0.11] | ||||
| Technostress → Psycho-physical distress | 0.26 ** | 0.08 | [0.10,0.41] | ||||
| Technostress → Fear of COVID-19 | 0.27 * | 0.07 | [0.13,0.44] | ||||
| Technostress → Fear of COVID-19 → Psycho-physical distress | 0.09 ** | 0.03 | [0.02,0.16] | ||||
| Total effects on psycho-physical distress | 0.35 *** | 0.08 | [0.19,0.51] | ||||
| Paths | Effects | |
|---|---|---|
| Estimate | S.E. | |
| Remote working→ Technostress | 0.23 *** | 0.06 |
| Age→ Technostress | 0.22 *** | 0.06 |
| Colleagues’ positivity for COVID-19→ Technostress | 0.06 | 0.06 |
| Age→ Working excessively | −0.21 ** | 0.07 |
| Gender→ Working excessively | 0.12 * | 0.05 |
| Technostress→ Working excessively | 0.43 *** | 0.07 |
| Working excessively → Work-family conflict | 0.39 *** | 0.07 |
| Gender→ Work-family conflict | −0.01 | 0.05 |
| Personal positivity for COVID-19→ Work-family conflict | 0.10 | 0.05 |
| Gender→ Resilience | −0.15 * | 0.02 |
| Resilience→ Work-family conflict | −0.11 | 0.09 |
| Working excessively × Resilience→ Work-family conflict | −0.20 ** | 0.07 |
| Technostress→ Work-family conflict | 0.36 *** | 0.06 |
| Remote working→ Fear of COVID-19 | 0.06 | 0.06 |
| Gender→ Fear of COVID-19 | 0.20 ** | 0.06 |
| Age→ Fear of COVID-19 | 0.08 | 0.06 |
| Technostress→ Fear of COVID-19 | 0.27 *** | 0.07 |
| Fear of COVID-19→ Psycho-physical distress | 0.29 *** | 0.07 |
| Fear of COVID-19 × Loss→ Psycho-physical distress | 0.32 ** | 0.12 |
| Loss→ Psycho-physical distress | 0.59 ** | 0.19 |
| Gender→ Psycho-physical distress | 0.16 ** | 0.05 |
| Age→ Psycho-physical distress | −0.20 *** | 0.06 |
| Techno-distress→ Psycho-physical distress | 0.21 *** | 0.06 |
| Technostress→ Working excessively × Low Resilience →Work-family conflict | 0.46 *** | 0.11 |
| Technostress→ Working excessively × Moderate Resilience → Work-family conflict | 0.31 *** | 0.08 |
| Technostress→ Working excessively × High Resilience→ Work-family conflict | 0.15 | 0.09 |
| Total effects for Low Resilience | 1.12 *** | 0.07 |
| Total effects for Moderate Resilience | 0.97 *** | 0.13 |
| Total effects for High Resilience | 0.81 *** | 0.13 |
| Technostress→ Fear of COVID-19 × No loss of a loved one→ Psycho-physical distress | −0.04 | 0.02 |
| Technostress→ Fear of COVID-19 × Loss of a loved one→ Psycho-physical distress | 0.08 ** | 0.02 |
| Total effects for no loss of a loved one | 0.11 *** | 0.04 |
| Total effects for loss of a loved one | 0.20 *** | 0.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sommovigo, V.; Bernuzzi, C.; Finstad, G.L.; Setti, I.; Gabanelli, P.; Giorgi, G.; Fiabane, E. How and When May Technostress Impact Workers’ Psycho-Physical Health and Work-Family Interface? A Study during the COVID-19 Pandemic in Italy. Int. J. Environ. Res. Public Health 2023, 20, 1266. https://doi.org/10.3390/ijerph20021266
Sommovigo V, Bernuzzi C, Finstad GL, Setti I, Gabanelli P, Giorgi G, Fiabane E. How and When May Technostress Impact Workers’ Psycho-Physical Health and Work-Family Interface? A Study during the COVID-19 Pandemic in Italy. International Journal of Environmental Research and Public Health. 2023; 20(2):1266. https://doi.org/10.3390/ijerph20021266
Chicago/Turabian StyleSommovigo, Valentina, Chiara Bernuzzi, Georgia Libera Finstad, Ilaria Setti, Paola Gabanelli, Gabriele Giorgi, and Elena Fiabane. 2023. "How and When May Technostress Impact Workers’ Psycho-Physical Health and Work-Family Interface? A Study during the COVID-19 Pandemic in Italy" International Journal of Environmental Research and Public Health 20, no. 2: 1266. https://doi.org/10.3390/ijerph20021266
APA StyleSommovigo, V., Bernuzzi, C., Finstad, G. L., Setti, I., Gabanelli, P., Giorgi, G., & Fiabane, E. (2023). How and When May Technostress Impact Workers’ Psycho-Physical Health and Work-Family Interface? A Study during the COVID-19 Pandemic in Italy. International Journal of Environmental Research and Public Health, 20(2), 1266. https://doi.org/10.3390/ijerph20021266








