Ghana’s Adherence to PASCAR’s 10-Point Action Plan towards Hypertension Control: A Scoping Review
Abstract
1. Introduction
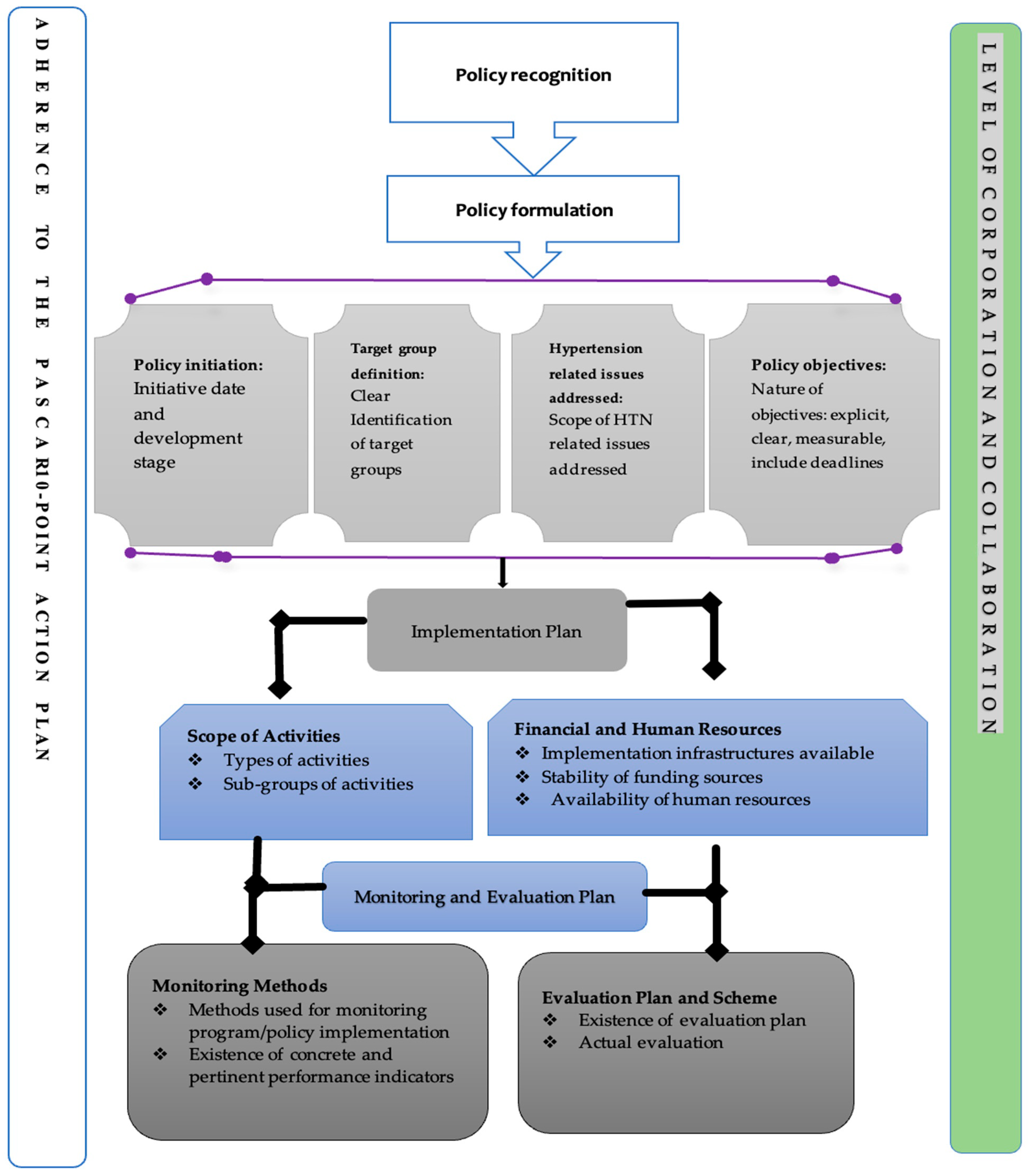
2. Materials and Methods
2.1. Stage 1: The Review Questions
- What are the characteristics of health policies developed from 2017 to 2022 for the control/reduction of hypertension in Ghana?
- To what extent do the current health policies adhere to the 10-point action plan for hypertension control/reduction in Ghana?
2.2. Stage 2: Identifying Relevant Policies
2.3. Stage 3: Study Selection
2.4. Stage 4: Charting the Data
2.5. Stage 5: Collating, Summarising, and Reporting the Results
3. Results
3.1. Part One: Evaluation of Programme and Policy Design of Included Studies
3.1.1. Political Recognition
3.1.2. Policy Initiation
3.1.3. Target Group Definition
3.1.4. Composition of the People Who Developed the Policy/Advisory Panel
3.1.5. Hypertension Issues Discussed
3.1.6. Policy Objectives
“To ensure that medicines selected for incorporation in the Essential Medicines List are suitable for the appropriate treatment of prevailing diseases, and that people’s medicines needs at different levels of the health care system are met in the most scientifically sound and cost-effective manner” [41] (pp. 14, 53).
“…to attain at least 80% coverage of Ghanaians having access to essential health services”, “Reduce by one-third pre-mature mortality from non-communicable diseases…” [37] (p. 19).
3.1.7. Scope of Activities
3.1.8. Financial and Human Resources
“…efforts will be made to produce and equitably distribute motivated human resource needed for NCDs prevention and control. Capacity building of staff that exists under the various levels will include the application of task shifting and task strengthening strategies” [25] (p. 30).
3.1.9. Monitoring and Evaluation (M&E) Plan
“…monitoring and evaluation of the policy will be the responsibility of the Ministry of Health, in collaboration with the Food and Drugs Authority and the National Food Safety Intersectoral Committee. As part of the process an effective M&E system will be built into the strategic framework from the onset. The system will monitor programme implementation and performance against a set of pre-determined indicators at all levels” [41] (p.31).
“Monitoring of the progress and achievement of the health outcomes will be routine and continuous (quarterly, half-yearly and annual)” [37] (pp. 34–35,37).
3.1.10. Level of Coordination and Collaboration
3.1.11. Level of HTN Patients Involvement
“There is observed increase in noncommunicable diseases particularly for hypertension…among the general population” [38] (p. 4).
“NCDs such as hypertension…and related conditions are increasing in prevalence” [37] (p. 13).
3.2. Part Two: Evaluation of Included Policies on the PASCAR Guidelines
3.2.1. Population-Level Interventions for Preventing Hypertension
“The population will be empowered and supported to proactively take measures to adopt healthy lifestyles. The policy shall ensure that the individual is encouraged to enjoy and enjoys adequate rest and shall support the development of recreational and physical activity facilities for regular use of the population towards the achievement of long-term individual and population health benefits. In addition, abstinence from alcohol or moderation in alcohol consumption will be encouraged and promoted through the strengthening of regulations on the production, marketing, and sale of alcoholic beverages” [37] (pp. 23–25).
“… promotive services, control of use of alcohol, tobacco and harmful substances; awareness on: regular medical check-ups…healthy eating, physical activity and wellbeing…” [37] (p. 6).
3.2.2. Additional Plan for the Detection of Hypertension
“…early detection targets persons with NCDs symptoms and persons with no NCDs symptoms but who are at risk of NCDs. This policy seeks to establish screening services to contribute to the reduction of NCDs morbidity and mortality through the implementation of national guidelines for screening, the establishment of wellness clinics and the strengthening of the capacity of the community-based Health Planning and Services (CHPS) to provide screening services” [25] (p. 19).
3.2.3. Funding and Resources for the Early Detection, Efficient Treatment, and Control of Hypertension
“…in line with the Government’s “Ghana beyond aid” agenda there is the need to explore innovative ways for funding NCDs prevention and control activities. This will be done in line with domestic, bilateral and multilateral funding mechanisms and within the current health financing arrangements. The policy will advocate for earmarked funds and increased budgetary allocations for NCDs” [25] (p. 31).
3.2.4. Adopt Simple and Practical Clinical Evidence-Based Hypertension Management Guidelines
3.2.5. Support High-Quality Research to Produce Evidence That will Guide Interventions
“A national health research agenda will also be developed and funded by various partners. Academia, expert consultant, and research institutions will play a key role in its implementation” [38] (p. 36).
3.2.6. Monitoring and Evaluation
3.2.7. Integrate Hypertension Detection, Treatment, and Control within Existing Health Services
“Integrate NCDs policy into all sector planning, budgeting and financial management systems for efficiency and sustainability of services” [25] (p. 24).
3.2.8. Promote a Task-Sharing Approach with Adequately Trained Community Health Workers
3.2.9. Ensure Availability of Essential Equipment and Medicines for Managing Hypertension at All Levels of Care
“Government will focus on the modernization/re-tooling of existing facilities, rationalize the construction and siting of additional purpose-built facilities, promote the availability and use of high-quality assistive devices and technologies (including prostheses, orthoses etc.) at an affordable cost. Comprehensive Health Technology Assessments (HTA) will be institutionalized and inform the selection and procurement of all medical technologies required. In addition, the availability, affordability, efficacy and overall quality of medicines and medical products for all recognized forms of medical practice, will be pursued” [37] (pp. 20–21).
“All primary health care levels will be re-stocked with essential tracer drugs equivalent to three months of their medicine and non-drug consumables requirement. This will also serve as a re-capitalization process following years of indebtedness and stockouts. The aim is to improve the visibility of stocks and consumption at facility level” [38] (pp. 11–12).
“This policy seeks to improve access to essential medicines and supplies for NCDs through the implementation of clearly outlined strategies” [25] (p. 30).
Further, the NMP also envisioned to ensure the availability of essential medicines at affordable and accessible to all Ghanaians [39]. An excerpt from the policy document states, “Government shall exempt selected essential medicines from Value Added Tax (VAT) and other forms of taxation. Such exempted drugs shall be reviewed periodically, but not beyond two years” [39] (p. 24).
“To improve the medicines pricing governance mechanisms and promote affordability of medicines in Ghana” [39] (p. 22).
3.2.10. Provide Universal Access and Coverage for Detecting, Treating, and Controlling HTN
“…promotion of prevention and routine screening for diagnoses for NCDs. Increase access to care for NCDs at all levels. Health education in schools on all NCDs” [25] (p. 19, 23).
“This roadmap recognizes the importance of all services. It however places greater emphasis on interventions that needed to be consolidated, scaled up and to attain universal health coverage” [37] (p. 6).
“The healthcare delivery system will be strengthened to achieve Universal Health Coverage meaning: all persons living in Ghana will have the opportunity to access quality healthcare services they require, wherever they are, with cost of care not being a barrier” [37] (p. 18).
“The policy will seek to strengthen surveillance and response systems to prevent, detect, investigate, protect against, control, and provide a public health response to the spread of diseases….” “The system shall operate across all levels (community, district, metropolitan, regional, and national) and recognize the animal-human interface as well (one-health)” [37] (p. 18).
4. Discussion
Strength and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Hypertension. Geneva, World Health Organisation. 2021. Available online: https://www.who.int/health-topics/hypertension#tab=tab_1 (accessed on 9 July 2022).
- Murray, C.J.L.; Vos, T.; Lozano, R.; Naghavi, M.; Flaxman, A.D.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2197–2223. [Google Scholar] [CrossRef] [PubMed]
- WHO. High Blood Pressure: Public Health Problem; World Health Organisation: Geneva, Switzerland, 2018. [Google Scholar]
- WHO. Blood Pressure/Hypertension; World Health Organisation: Geneva, Switzerland, 2022; Available online: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3155 (accessed on 9 July 2022).
- Kearney, P.M.; Whelton, M.; Reynolds, K.; Muntner, P.; Whelton, P.K.; He, J. Global burden of hypertension: Analysis of worldwide data. Lancet 2005, 365, 217–223. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Noncommunicable Diseases Country Profiles 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Bosu, W.K.; Reilly, S.T.; Aheto, J.M.; Zucchelli, E. Hypertension in older adults in Africa: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0214934. [Google Scholar] [CrossRef] [PubMed]
- Nyirenda, M.J. Non-communicable diseases in sub-Saharan Africa: Understanding the drivers of the epidemic to inform intervention strategies. Int. Health 2016, 8, 157–158. [Google Scholar] [CrossRef]
- Gómez-Olivé, F.X.; Ali, S.A.; Made, F.; Kyobutungi, C.; Nonterah, E.; Micklesfield, L.; Alberts, M.; Boua, R.; Hazelhurst, S.; Debpuur, C.; et al. Regional and sex differences in the prevalence and awareness of hypertension across six sites in sub-Saharan Africa: An H3Africa AWI-Gen study. Glob. Heart 2017, 12, 81. [Google Scholar] [CrossRef]
- Ibrahim, M.M.; Damasceno, A. Hypertension in developing countries. Lancet 2012, 380, 611–619. [Google Scholar] [CrossRef]
- Odili, A.N.; Chori, B.S.; Danladi, B.; Nwakile, P.C.; Okoye, I.C.; Abdullahi, U.; Nwegbu, M.N.; Zawaya, K.; Essien, I.; Sada, K.; et al. Prevalence, awareness, treatment and control of hypertension in Nigeria: Data from a nationwide survey 2017. Glob. Heart 2020, 15, 47. [Google Scholar] [CrossRef]
- Mohamed, S.F.; Mutua, M.K.; Wamai, R.; Wekesah, F.; Haregu, T.; Juma, P.; Nyanjau, L.; Kyobutungi, C.; Ogola, E. Prevalence, awareness, treatment and control of hypertension and their determinants: Results from a national survey in Kenya. BMC Public Health 2018, 18, 1219. [Google Scholar] [CrossRef]
- Awuah, R.B.; Anarfi, J.K.; Agyemang, C.; Ogedegbe, G.; Aikins, A.D. Prevalence, awareness, treatment and control of hypertension in urban poor communities in Accra, Ghana. J. Hypertens. 2014, 32, 1203–1210. [Google Scholar] [CrossRef]
- Okeahialam, B.N.; Ogbonna, C.; Otokwula, A.E.; Joseph, D.E.; Chuhwak, E.K.; Isiguzoro, I.O. Cardiovascular epidemiological transition in a rural habitat of Nigeria: The case of Mangu local government area. West Afr. J. Med. 2012, 31, 14–18. [Google Scholar]
- Atibila, F.; Hoor, G.T.; Donkoh, E.T.; Wahab, A.I.; Kok, G. Prevalence of hypertension in Ghanaian society: A systematic review, meta-analysis, and GRADE assessment. Syst. Rev. 2021, 10, 220. [Google Scholar] [CrossRef]
- Ghana Health Service. The Health Sector in Ghana: Facts and Figures 2018; Ministry of Health of Ghana: Accra, Ghana, 2018; pp. 1–50. [Google Scholar]
- Appiah, F.; Ameyaw, E.K.; Oduro, J.K.; Baatiema, L.; Sambah, F.; Seidu, A.-A.; Ahinkorah, B.O.; Budu, E. Rural-urban variation in hypertension among women in Ghana: Insights from a national survey. BMC Public Health 2021, 21, 2150. [Google Scholar] [CrossRef]
- Miranda, J.J.; Kinra, S.; Casas, J.P.; Davey Smith, G.; Ebrahim, S. Non-communicable diseases in low-and middle-income countries: Context, determinants and health policy. Trop. Med. Int. Health 2008, 13, 1225–1234. [Google Scholar] [CrossRef]
- van de Vijver, S.; Akinyi, H.; Oti, S.; Olajide, A.; Agyemang, C.; Aboderin, I.; Kyobutungi, C. Status report on hypertension in Africa-Consultative review for the 6th Session of the African Union Conference of Ministers of Health on NCD’s. Pan Afr. Med. J. 2014, 16, 3100. [Google Scholar]
- Gay, H.C.; Rao, S.G.; Vaccarino, V.; Ali, M.K. Effects of different dietary interventions on blood pressure: Systematic review and meta-analysis of randomized controlled trials. Hypertension 2016, 67, 733–739. [Google Scholar] [CrossRef]
- Maruf, F.A.; Akinpelu, A.O.; Salako, B.L.; Akinyemi, J. Effects of aerobic dance training on blood pressure in individuals with uncontrolled hypertension on two antihypertensive drugs: A randomized clinical trial. J. Am. Soc. Hypertens. 2016, 10, 336–345. [Google Scholar] [CrossRef]
- Tetteh, J.; Entsua-Mensah, K.; Doku, A.; Mohammed, S.; Swaray, S.M.; Ayanore, M.A.; Yawson, A.E. Self-reported hypertension as a predictor of chronic health conditions among older adults in Ghana: Analysis of the WHO Study on global Ageing and adult health (SAGE) Wave 2. Pan Afr. Med. J. 2020, 36, 21489. [Google Scholar] [CrossRef]
- Dzudie, A.; Twagirumukiza, M.; Cornick, R.; Abdou Ba, S.; Damasceno, A.; Rayner, B.; Kane, A.; Sliwa, K.; Anzouan Kacou, J.B.; Mocumbi, A.O.; et al. Roadmap to achieve 25% hypertension control in Africa by 2025. Cardiovasc. J. Afr. 2017, 28, 262–273. [Google Scholar] [CrossRef]
- Ministry of Health, Kenya. National Strategic Plan for the Prevention and Control of Non-Communicable Diseases 2021/22–2025/26. 2021. Available online: www.health.go.ke/wp-content/uploads/2021/07/Kenya-pdf (accessed on 9 July 2022).
- Ministry of Health. National Policy: Non-Communicable Diseases, 2nd ed.; MoH: Accra, Ghana, 2022. [Google Scholar]
- Ministry of Health. National Policy: Non-Communicable Diseases, 1st ed.; MoH: Accra, Ghana, 2012. [Google Scholar]
- Bosu, W.K.; Bosu, D.K. Prevalence, awareness and control of hypertension in Ghana: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0248137. [Google Scholar] [CrossRef]
- Nyawornota, V.K.; Tay, D.A.; Adu, E.; Ocansey, R.T. A scoping review of 2018–2020 research on NCDs and physical activity in Ghana: Groundwork for a monitoring system and action plan. FASEB BioAdv. 2022, 4, 162–169. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Ahinkorah, B.O.; Kang, M.; Perry, L.; Brooks, F. Prevention of Adolescent Pregnancy in Anglophone Sub-Saharan Africa: A Scoping Review of National Policies. Int. J. Health Policy Manag. 2020, x, 1–14. [Google Scholar] [CrossRef]
- Seidu, A.-A.; Malau-Aduli, B.S.; McBain-Rigg, K.; Malau-Aduli, A.E.O.; Emeto, T.I. Level of inclusiveness of people with disabilities in Ghanaian health policies and reports: A scoping review. Disabilities 2021, 1, 257–277. [Google Scholar] [CrossRef]
- Jones, C.M.; Gautier, L.; Ridde, V. A scoping review of theories and conceptual frameworks used to analyse health financing policy processes in sub-Saharan Africa. Health Policy Plan. 2021, 36, 1197–1214. [Google Scholar] [CrossRef]
- Calves, A. Assessing adolescent reproductive health policies and programs. Policy Working Paper Series, 8 July 2002. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Int. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Mayring, P. Qualitative content analysis: Theoretical background and procedures. In Approaches to Qualitative Research in Mathematics Education; Springer: Dordrecht, The Netherlands, 2015; pp. 365–380. [Google Scholar]
- Vaismoradi, M.; Turunen, H.; Bondas, T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013, 15, 398–405. [Google Scholar] [CrossRef]
- Ministry of Health. National Health Policy: Ensuring Healthy Lives for All, revised ed.; MoH: Accra, Ghana, 2020. [Google Scholar]
- Ministry of Health. Ghana’s Roadmap for Attaining Universal Health Coverage 2020–2030; MoH: Accra, Ghana, 2020. [Google Scholar]
- Ministry of Health. Health Commodity Supply Chain Master Plan; MoH: Accra, Ghana, 2021. [Google Scholar]
- Ministry of Health. National Medicines Policy; MoH: Accra, Ghana, 2017. [Google Scholar]
- Ministry of Health. Health Sector Medium Term Development Plan; MoH: Accra, Ghana, 2022. [Google Scholar]
- Ministry of Health. National Food Safety Policy; MoH: Accra, Ghana, 2022. [Google Scholar]
- Ministry of Health. Ministry of Health Client Service Charter; MoH: Accra, Ghana, 2020. [Google Scholar]
- Owusu, M.F. Effective Management of Non-Communicable Diseases in Ghana: The Case of Hypertension and Diabetes Mellitus. Ph.D. Thesis, University of Canterbury, Christchurch, New Zealand, 2019. [Google Scholar]
- Nyaaba, G.N.; Stronks, K.; Aikins, A.D.-G.; Kengne, A.P.; Agyemang, C. Tracing Africa’s progress towards implementing the Non-Communicable Diseases Global action plan 2013–2020: A synthesis of WHO country profile reports. BMC Public Health 2017, 17, 297. [Google Scholar] [CrossRef]
- JJuma, P.A.; Mapa-Tassou, C.; Mohamed, S.F.; Mwagomba, B.L.M.; Ndinda, C.; Oluwasanu, M.; Mbanya, J.-C.; Nkhata, M.J.; Asiki, G.; Kyobutungi, C. Multi-sectoral action in non-communicable disease prevention policy development in five African countries. BMC Public Health 2018, 18, 953. [Google Scholar] [CrossRef]
- South Africa National NCD. National Strategic Plan for the Prevention and Control of Non-Communicable Diseases 2020–2025; South Africa National NCD: Johannesburg, South Africa, 2020. [Google Scholar]
- Nigeria Federal Ministry of Health. National Multi-Sectoral Action Plan for the Prevention and Control of Non-Communicable Diseases (2019–2025); Nigeria Federal Ministry of Health: Abuja, Nigeria, 2019. [Google Scholar]
- Pollock, A.; Campbell, P.; Struthers, C.; Synnot, A.; Nunn, J.; Hill, S.; Goodare, H.; Morris, J.; Watts, C.; Morley, R. Stakeholder involvement in systematic reviews: A scoping review. Syst. Rev. 2018, 7, 208. [Google Scholar] [CrossRef]
- Amu, H.; Darteh, E.K.; Tarkang, E.E.; Kumi-Kyereme, A. Management of chronic non-communicable diseases in Ghana: A qualitative study using the chronic care model. BMC Public Health 2021, 21, 1120. [Google Scholar] [CrossRef]
- Maher, D.; Ford, N.; Unwin, N. Priorities for developing countries in the global response to non-communicable diseases. Glob. Health 2012, 8, 14. [Google Scholar] [CrossRef]
- WHO. Action Plan for the Global Strategy for the Prevention and Control of Non-Communicable Diseases 2008–2013; World Health Organisation: Geneva, Switzerland, 2008. [Google Scholar]
- Nyaaba, G.N.; Stronks, K.; Masana, L.; Killinger, C.L.; Agyemang, C. Implementing a national non-communicable disease policy in sub-Saharan Africa: Experiences of key stakeholders in Ghana. Health Policy Open 2020, 1, 100009. [Google Scholar] [CrossRef]
- Juma, P.A.; Mohamed, S.F.; Mwagomba, B.L.M.; Ndinda, C.; Mapa-Tassou, C.; Oluwasanu, M.; Oladepo, O.; Abiona, O.; Nkhata, M.J.; Wisdom, J.P.; et al. Non-communicable disease prevention policy process in five African countries authors. BMC Public Health 2018, 18, 961. [Google Scholar] [CrossRef]
- Fang, J.; Zhao, G.; Wang, G.; Ayala, C.; Loustalot, F. Insurance status among adults with hypertension—The impact of underinsurance. J. Am. Heart Assoc. 2016, 5, e004313. [Google Scholar] [CrossRef]
- Ogedegbe, G.; Plange-Rhule, J.; Gyamfi, J.; Chaplin, W.; Ntim, M.; Apusiga, K.; Iwelunmor, J.; Awudzi, K.Y.; Quakyi, K.N.; Mogaverro, J.; et al. Health insurance coverage with or without a nurse-led task shifting strategy for hypertension control: A pragmatic cluster randomized trial in Ghana. PLoS Med. 2018, 15, e1002561. [Google Scholar] [CrossRef]
- Oso, A.A.; Adefurin, A.; Benneman, M.M.; Oso, O.O.; Taiwo, M.A.; Adebiyi, O.O.; Oluwole, O. Health insurance status affects hypertension control in a hospital based internal medicine clinic. Int. J. Cardiol. Hypertens. 2019, 1, 100003. [Google Scholar] [CrossRef]
- Carey, R.M.; Muntner, P.; Bosworth, H.B.; Whelton, P.K. Prevention and control of hypertension: JACC health promotion series. J. Am. Coll. Cardiol. 2018, 72, 1278–1293. [Google Scholar] [CrossRef]
- Asmah, E.E.; Andoh, F.K.; Razvi, S.; Wong, B. Cost-Benefit Analysis of Community Health Worker Led Screening and Treatment for Hypertension in Ghana. Ghana Priorities, Copenhagen Consensus Center. 2020. Available online: https://www.copenhagenconsensus.com/sites (accessed on 9 July 2022).
- Blackstone, S.R. Task-Shifting and Hypertension Management in Ghana. Ph.D. Theis, University of Illinois at Urbana-Champaign, Champaign, IL, USA, 2017. [Google Scholar]
- World Health Organization. Task Shifting: Rational Redistribution of Tasks among Health Workforce Teams: Global Recommendations and Guidelines; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Adler, A.J.; Laar, A.K.; Kotoh, A.M.; Legido-Quigley, H.; Perel, P.; Lamptey, P.; Lange, I.L. Barriers and facilitators to the implementation of a community-based hypertension improvement project in Ghana: A qualitative study of ComHIP. BMC Health Serv. Res. 2020, 20, 67. [Google Scholar] [CrossRef]
- Tindana, P.; Ramsay, M.; Klipstein-Grobusch, K.; Amoakoh-Coleman, M. Advancing non-communicable diseases research in Ghana: Key stakeholders’ recommendations from a symposium. Ghana Med. J. 2020, 54, 121–125. [Google Scholar] [CrossRef]
- Jeemon, P.; Séverin, T.; Amodeo, C.; Balabanova, D.; Campbell, N.R.C.; Gaita, D.; Kario, K.; Khan, T.; Melifonwu, R.; Moran, A.; et al. World heart federation roadmap for hypertension–a 2021 update. Glob. Heart 2021, 16, 63. [Google Scholar] [CrossRef]
- O’Connor, P.J.; Vazquez-Benitez, G.; Schmittdiel, J.A.; Parker, E.D.; Trower, N.K.; Desai, J.R.; Margolis, K.L.; Magid, D.J. Benefits of early hypertension control on cardiovascular outcomes in patients with diabetes. Diabetes Care 2013, 36, 322–327. [Google Scholar] [CrossRef] [PubMed]
- Boudreaux, C.; Noble, C.; Coates, M.M.; Kelley, J.; Abanda, M.; Kintu, A.; McLaughlin, A.; Marx, A.; Bukhman, G. Noncommunicable Disease (NCD) strategic plans in low-and lower-middle income Sub-Saharan Africa: Framing and policy response. Glob. Health Action 2020, 13, 1805165. [Google Scholar] [CrossRef] [PubMed]

| Policy/Report Title | Political Recognition | Issues Addressed Concerning HTN | Target Group Definition | Composition of the People Who Developed It | Policy Objectives (Quantitative or Qualitative) | Scope of Activities or Strategies Targeting HTN | Resources: Financial and Human | M & E Plan/Performance Indicators | Cooperation and Collaboration (Number of Partners Involved) | Involvement of Persons with HTN | Accessible Online? | Mention of HTN | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | National health policy (2020) | √ | √ | General population | Multidisciplinary group without inputs from HTN association or group | Qualitative | √ | √ | √ | √ | X | √ | √ |
| 2 | Ghana’s roadmap for attaining universal health coverage 2020–2030 (2020) | √ | √ | General population | Multidisciplinary group without inputs from HTN association or group | Qualitative | √ | √ | X | √ | X | √ | √ |
| 3 | National policy: non-communicable diseases (2022) | √ | √ | People with non-communicable diseases | Multidisciplinary group including members of HTN Association | Qualitative | √ | √ | √ | √ | √ | √ | √ |
| 4 | Health commodity supply chain master plan (2021) | √ | √ | General population | Multidisciplinary group without inputs from HTN association or group | Qualitative | X | √ | √ | √ | X | √ | X |
| 5 | Health Sector Medium Term Development Plan (2021) | √ | √ | General population | Multidisciplinary group without inputs from HTN association or group | Qualitative | √ | √ | √ | √ | X | √ | √ |
| 6 | National Medicines Policy (2017) | √ | √ | General population | Multidisciplinary group without inputs from HTN association or group | Qualitative | X | √ | √ | √ | X | √ | X |
| 7 | National food safety policy (2022) | √ | X | General population | Multidisciplinary group without inputs from HTN association or group | Qualitative | X | √ | √ | √ | X | √ | X |
| 8 | Ministry of health client service charter (2020) | √ | √ | General population | Multidisciplinary group without inputs from HTN association or group | Qualitative | X | √ | X | √ | X | √ | X |
| Policy/Report Title | Population-Level Interventions for Preventing Hypertension | Additional Plan for the Detection of Hypertension | Funding and Resources for the Early Detection, Efficient Treatment, and Control of Hypertension | Adopt Simple and Practical Clinical Evidence-Based Hypertension Management Guidelines | Support High-Quality Research to Produce Evidence That will Guide Interventions | Annually Monitor and Report the Detection, Treatment and Control Rates of Hypertension, with a Clear Target of Improvement by 2025, Using the WHO STEP Wise Surveillance in All Countries | Integrate Hypertension Detection, Treatment, and Control within Existing Health Services | Promote a Task-Sharing Approach with Adequately Trained Community Health Workers | Ensure Availability of Essential Equipment and Medicines for Managing Hypertension at all Levels of Care | Provide Universal Access and Coverage for Detecting, Treating, and Controlling Hypertension |
|---|---|---|---|---|---|---|---|---|---|---|
| √ | X | X | X | √ | √ | X | X | √ | √ |
| √ | √ | X | X | √ | √ | X | X | √ | X |
| √ | √ | √ | X | √ | √ | √ | √ | √ | √ |
| √ | X | X | X | X | X | X | X | X | X |
| √ | √ | √ | X | X | X | X | X | √ | X |
| √ | X | X | X | √ | X | X | X | √ | X |
| X | X | X | X | √ | X | X | X | X | X |
| √ | X | X | X | X | X | X | X | X | X |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sambah, F.; Malau-Aduli, B.S.; Seidu, A.-A.; Malau-Aduli, A.E.O.; Emeto, T.I. Ghana’s Adherence to PASCAR’s 10-Point Action Plan towards Hypertension Control: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 1425. https://doi.org/10.3390/ijerph20021425
Sambah F, Malau-Aduli BS, Seidu A-A, Malau-Aduli AEO, Emeto TI. Ghana’s Adherence to PASCAR’s 10-Point Action Plan towards Hypertension Control: A Scoping Review. International Journal of Environmental Research and Public Health. 2023; 20(2):1425. https://doi.org/10.3390/ijerph20021425
Chicago/Turabian StyleSambah, Francis, Bunmi S. Malau-Aduli, Abdul-Aziz Seidu, Aduli E. O. Malau-Aduli, and Theophilus I. Emeto. 2023. "Ghana’s Adherence to PASCAR’s 10-Point Action Plan towards Hypertension Control: A Scoping Review" International Journal of Environmental Research and Public Health 20, no. 2: 1425. https://doi.org/10.3390/ijerph20021425
APA StyleSambah, F., Malau-Aduli, B. S., Seidu, A.-A., Malau-Aduli, A. E. O., & Emeto, T. I. (2023). Ghana’s Adherence to PASCAR’s 10-Point Action Plan towards Hypertension Control: A Scoping Review. International Journal of Environmental Research and Public Health, 20(2), 1425. https://doi.org/10.3390/ijerph20021425







