Eating Behaviors, Lifestyle, and Ischemic Stroke: A Lebanese Case-Control Study
Abstract
1. Background
2. Materials and Methods
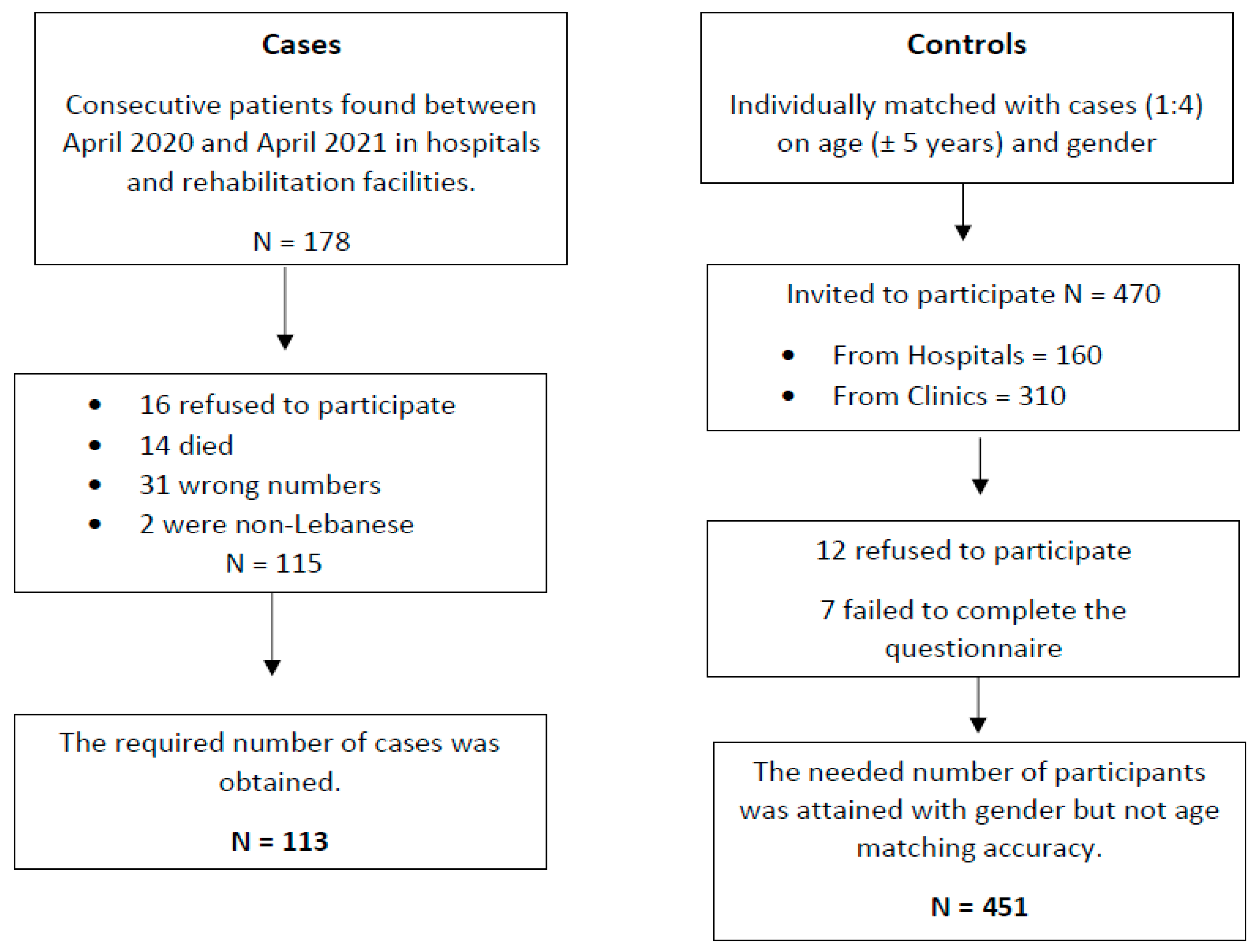
2.1. Participants
2.2. Minimal Sample Size Calculation
2.3. Procedure
2.4. Measures/Instruments
- ▪
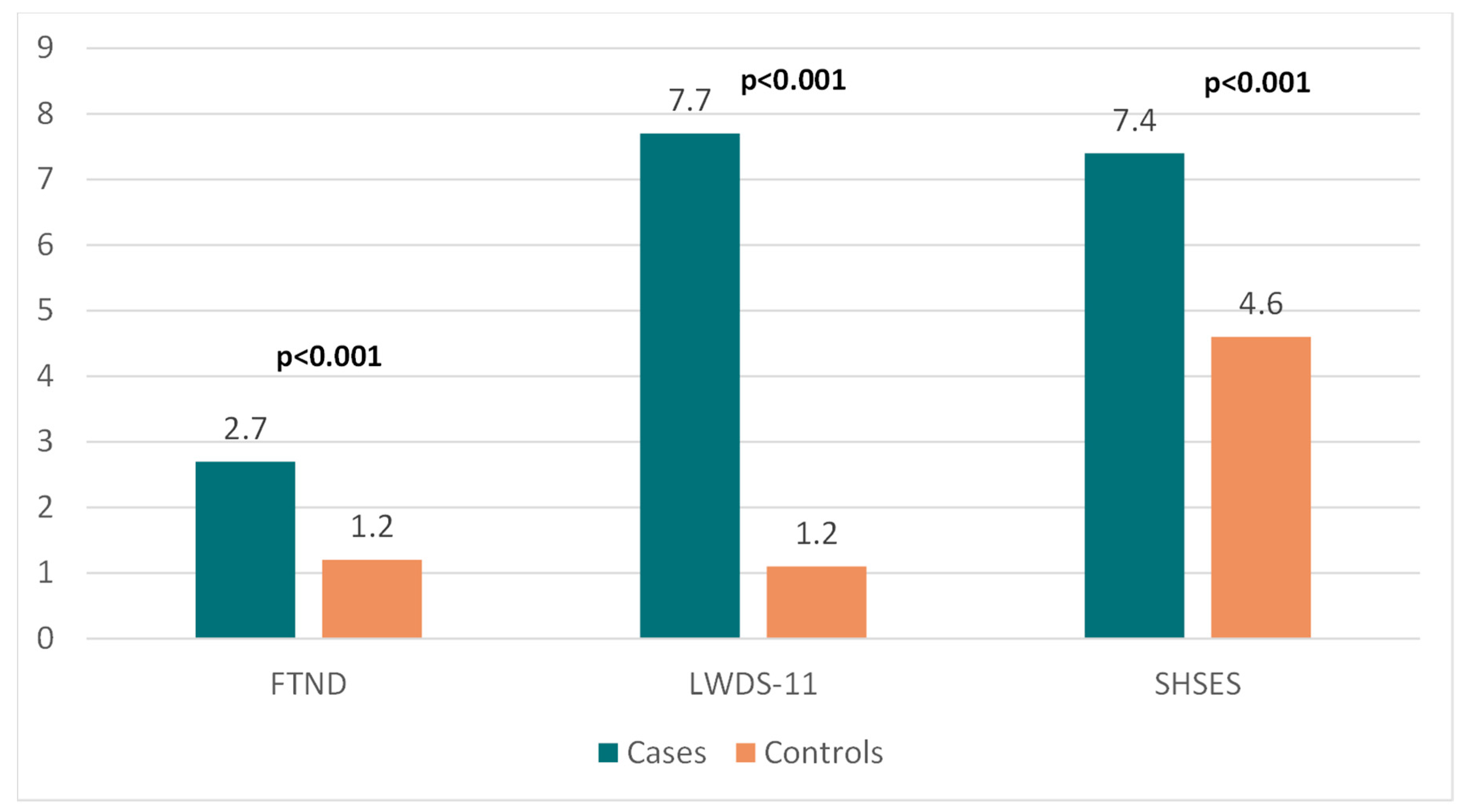
- Fagerström Test for Nicotine Dependence (FTND)
- ▪
- Lebanon Waterpipe Dependence Scale-11 (LWDS-11)
- ▪
- Secondhand Smoking Exposure Score (SHSES)
- ▪
- Mediterranean Diet Adherence
- ▪
- International Physical Activity Questionnaire (IPAQ)—short version
- ▪
- Diet and Body Image
- ▪
- Eating Attitudes Test (EAT)
- ▪
- Disordered Eating Attitude Scale (DEAS)
- ▪
- Düsseldorf Orthorexia Scale (DOS)
2.5. Translation Procedure
2.6. Statistical Analysis
3. Results
3.1. Demographic Characteristics and Socioeconomic Factors of the Participants (N = 564)
3.2. Bivariate Analysis of Other Factors Associated with Ischemic Stroke
3.3. Multivariable Analysis
4. Discussion
4.1. Limitations and Strengths
4.2. Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MeD | Mediterranean Diet |
| ON | Orthorexia Nervosa |
| CDC | Centers for Disease Control and Prevention |
| SPSS | Statistical Package for Social Science |
References
- Katan, M.; Luft, A. Global burden of stroke. Semin. Neurol. 2018, 38, 208–211. [Google Scholar] [CrossRef] [PubMed]
- Benamer, H.; Grosset, D. Stroke in Arab countries: A systematic literature review. J. Neurol. Sci. 2009, 284, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Saver, J.L. Time is brain–quantified. Stroke 2006, 37, 263–266. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M.J.; Xavier, D.; Liu, L.; Zhang, H.; Chin, S.L.; Rao-Melacini, P.; Rangarajan, S.; Islam, S.; Pais, P.; McQueen, M.J.; et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): A case-control study. Lancet 2010, 376, 112–123. [Google Scholar] [CrossRef] [PubMed]
- Markidan, J.; Cole, J.W.; Cronin, C.A.; Merino, J.G.; Phipps, M.S.; Wozniak, M.A.; Kittner, S.J. Smoking and risk of ischemic stroke in young men. Stroke 2018, 49, 1276–1278. [Google Scholar] [CrossRef]
- Pan, B.; Jin, X.; Jun, L.; Qiu, S.; Zheng, Q.; Pan, M. The relationship between smoking and stroke. Medicine 2019, 98, e14872. [Google Scholar] [CrossRef]
- Gallanagh, S.; Quinn, T.J.; Alexander, J.; Walters, M.R. Physical activity in the prevention and treatment of stroke. ISRN Neurol. 2011, 2011, 953818. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.N.; Forey, B.A. Environmental tobacco smoke exposure and risk of stroke in nonsmokers: A review with meta-analysis. J. Stroke Cerebrovasc. Dis. 2006, 15, 190–201. [Google Scholar] [CrossRef]
- Heuschmann, P.U.; Heidrich, J.; Wellmann, J.; Kraywinkel, K.; Keil, U. Stroke mortality and morbidity attributable to passive smoking in Germany. Eur. J. Cardiovasc. Prev. Rehabil. 2007, 14, 793–795. [Google Scholar] [CrossRef]
- Boden-Albala, B.; Sacco, R.L. Lifestyle factors and stroke risk: Exercise, alcohol, diet, obesity, smoking, drug use, and stress. Curr. Atheroscler. Rep. 2000, 2, 160–166. [Google Scholar] [CrossRef]
- CDC, National Center for Chronic Disease Prevention and Health Promotion, Division for Heart Disease and Stroke. Available online: https://www.cdc.gov/chronicdisease/resources/publications/factsheets/heart-disease-stroke.htm (accessed on 1 January 2022).
- Psaltopoulou, T.; Sergentanis, T.N.; Panagiotakos, D.B.; Sergentanis, I.N.; Kosti, R.; Scarmeas, N. Mediterranean diet, stroke, cognitive impairment, and depression: A meta-analysis. Ann. Neurol. 2013, 74, 580–591. [Google Scholar] [CrossRef]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediterranean diet pyramid: A cultural model for healthy eating. Am. J. Clin. Nutr. 1995, 61, 1402S–1406S. [Google Scholar] [CrossRef] [PubMed]
- Nestle, M. Mediterranean diets: Historical and research overview. Am. J. Clin. Nutr. 1995, 61, 1313S–1320S. [Google Scholar] [CrossRef] [PubMed]
- Tsivgoulis, G.; Psaltopoulou, T.; Wadley, V.G.; Alexandrov, A.V.; Howard, G.; Unverzagt, F.W.; Moy, C.; Howard, V.J.; Kissela, B.; Judd, S.E. Adherence to a Mediterranean diet and prediction of incident stroke. Stroke 2015, 46, 780. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Tuttolomondo, A.; Casuccio, A.; Buttà, C.; Pecoraro, R.; Di Raimondo, D.; Della Corte, V.; Arnao, V.; Clemente, G.; Maida, C.; Simonetta, I.; et al. Mediterranean diet in patients with acute ischemic stroke: Relationships between Mediterranean diet score, diagnostic subtype, and stroke severity index. Atherosclerosis 2015, 243, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Bratman, S. Health food junkie. Yoga J. 1997, 136, 42–50. [Google Scholar]
- Moroze, R.M.; Dunn, T.M.; Holland, J.C.; Yager, J.; Weintraub, P. Microthinking about micronutrients: A case of transition from obsessions about healthy eating to near-fatal “orthorexia nervosa” and proposed diagnostic criteria. Psychosomatics 2015, 56, 397–403. [Google Scholar] [CrossRef]
- Nevin, S.M.; Vartanian, L.R. The stigma of clean dieting and orthorexia nervosa. J. Eat. Disord. 2017, 5, 37. [Google Scholar] [CrossRef]
- Hankey, G.J. Nutrition and the risk of stroke. Lancet Neurol. 2012, 11, 66–81. [Google Scholar] [CrossRef]
- Hong, Y.C.; Lee, J.T.; Kim, H.; Kwon, H.J. Air pollution: A new risk factor in ischemic stroke mortality. Stroke 2002, 33, 2165–2169. [Google Scholar] [CrossRef] [PubMed]
- Lisabeth, L.D.; Escobar, J.D.; Dvonch, J.T.; Sánchez, B.N.; Majersik, J.J.; Brown, D.; Smith, M.A.; Morgenstern, L.B. Ambient air pollution and risk for ischemic stroke and transient ischemic attack. Ann. Neurol. 2008, 64, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Villeneuve, P.J.; Chen, L.; Stieb, D.; Rowe, B.H. Associations between outdoor air pollution and emergency department visits for stroke in Edmonton, Canada. Eur. J. Epidemiol. 2006, 21, 689–700. [Google Scholar] [CrossRef] [PubMed]
- Gillum, R.F.; Mussolino, M.E. Education, poverty, and stroke incidence in whites and blacks: The NHANES I Epidemiologic Follow-up Study. J. Clin. Epidemiol. 2003, 56, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Bernal-Pacheco, O.; Roman, G.C. Environmental vascular risk factors: New perspectives for stroke prevention. J. Neurol. Sci. 2007, 262, 60–70. [Google Scholar] [CrossRef]
- Kumar, A.; Prasad, M.; Kathuria, P.; Nair, P.; Pandit, A.K.; Sahu, J.K.; Prasad, K. Low Socioeconomic Status is an independent risk factor for ischemic stroke: A case-control study in north Indian population. Neuroepidemiology 2015, 44, 138–143. [Google Scholar] [CrossRef]
- Agyemang, C.; van Oeffelen, A.A.; Norredam, M.; Kappelle, L.J.; Klijn, C.J.; Bots, M.L.; Stronks, K.; Vaartjes, I. Socioeconomic inequalities in stroke incidence among migrant groups. Stroke 2014, 45, 2397–2403. [Google Scholar] [CrossRef]
- Honjo, K.; Iso, H.; Nakaya, T.; Hanibuchi, T.; Ikeda, A.; Inoue, M.; Sawada, N.; Tsugane, S.; the Japan Public Health Center-based Prospective Study Group. Impact of neighborhood Socioeconomic conditions on the risk of stroke in Japan. J. Epidemiol. 2015, 25, 254–260. [Google Scholar] [CrossRef]
- Simons, L.A.; McCallum, J.; Friedlander, Y.; Simons, J. Risk factors for ischemic stroke: Dubbo Study of the elderly. Stroke 1998, 29, 1341–1346. [Google Scholar] [CrossRef] [PubMed]
- Öhgren, B.; Weinehall, L.; Stegmayr, B.; Boman, K.; Hallmans, G.; Wall, S. What else adds to hypertension in predicting stroke? An incident case-referent study. J. Intern. Med. 2000, 248, 475–482. [Google Scholar] [CrossRef]
- Boysen, G.; Nyboe, J.; Appleyard, M.; Sorensen, P.S.; Boas, J.; Somnier, F.; Jensen, G.; Schnohr, P. Stroke incidence and risk factors for stroke in Copenhagen, Denmark. Stroke 1988, 19, 1345–1353. [Google Scholar] [CrossRef] [PubMed]
- Thompson, S.G.; Greenberg, G.; Meade, T.W. Risk factors for stroke and myocardial infarction in women in the United States as assessed in general practice: A case-control study. Br. Heart J. 1989, 61, 403–409. [Google Scholar] [CrossRef]
- Honjo, K.; Iso, H.; Ikeda, A.; Inoue, M.; Sawada, N.; Tsugane, S.; JPHC Study Group. Marital Transition and Risk of Stroke: How Living Arrangement and Employment Status Modify Associations. Stroke 2016, 47, 991–998. [Google Scholar] [CrossRef]
- Sibai, A.; Hwalla, N. WHO STEPS-Chronic Disease Risk Factor Surveillance: Data Book for Lebanon. Available online: http://www.who.int/chp/steps/2008_STEPS_Lebanon.pdf (accessed on 22 May 2015).
- Nasreddine, L.; Naja, F.; Chamieh, M.C.; Adra, N.; Sibai, A.-M.; Hwalla, N. Trends in overweight and obesity in Lebanon: Evidence from two national cross-sectional surveys (1997 and 2009). BMC Public Health 2012, 12, 798. [Google Scholar] [CrossRef]
- El-Roueiheb, Z.; Tamim, H.; Kanj, M.; Jabbour, S.; Alayan, I.; Musharrafieh, U. Cigarette and waterpipe smoking among Lebanese adolescents, a cross-sectional study, 2003–2004. Nicotine Tob. Res. Off. J. Soc. Res. Nicotine Tob. 2008, 10, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Chacar, H.R.; Salameh, P. Public schools adolescents’ obesity and growth curves in Lebanon. Leban. Med. J. 2011, 59, 81. [Google Scholar]
- El-Hajj, M.; Salameh, P.; Rachidi, S.; Al-Hajje, A.; Lahoud, N.; Hosseini, H. Stroke risk factors: A hospital-based case–control study in Lebanon. J. R. Soc. Med. Open 2017, 8, 1–10. [Google Scholar]
- El-Hajj, M.; Salameh, P.; Rachidi, S.; Al-Hajje, A.; Hosseini, H. Adherence to the Mediterranean diet decreases the risk of stroke in the Lebanese population: A case-control study. Pharm. Pract. 2021, 19, 2157. [Google Scholar] [CrossRef]
- Lakkur, S.; Judd, S.E. Diet and Stroke: Recent Evidence Supporting a Mediterranean-Style Diet and Food in the Primary Prevention of Stroke. Stroke 2015, 46, 2007–2011. [Google Scholar] [CrossRef]
- American Stroke Association. Together to End Stroke [Internet] American Stroke Association. 2013. Available online: http://www.strokeassociation.org/STROKEORG/AboutStroke/TypesofStroke/Types-of-Stroke_UCM_308531_SubHomePage.jsp (accessed on 29 May 2016).
- Karam, E.G.; Mneimneh, Z.N.; Karam, A.N.; Fayyad, J.A.; Nasser, S.C.; Chatterji, S.; Kessler, R.C. Prevalence and treatment of mental disorders in Lebanon: A national epidemiological survey. Lancet 2006, 367, 1000–1006. [Google Scholar] [CrossRef]
- Zuflacht, J.P.; Shao, Y.; Kronish, I.M.; Edmondson, D.; Elkind, M.S.V.; Kamel, H.; Boehme, A.K.; Willey, J.Z. Psychiatric Hospitalization Increases Short-Term Risk of Stroke. Stroke 2017, 48, 1795–1801. [Google Scholar] [CrossRef] [PubMed]
- Heatherton, T.F.; Kozlowski, L.T.; Frecker, R.C.; Fagerstrom, K.O. The Fagerström test for nicotine dependence: A revision of the Fagerstrom tolerance questionnaire. Br. J. Addict. 1991, 86, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Salameh, P.; Waked, M.; Aoun, Z. Waterpipe smoking: Construction and validation of the Lebanon Waterpipe dependence scale (LWDS-11). Nicotine Tob. Res. 2008, 10, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Hallit, S.; Obeid, S.; Sacre, H.; Salameh, P. Lebanese Waterpipe Dependence Scale (LWDS-11) validation in a sample of Lebanese adolescents. BMC Public Health 2021, 21, 1627. [Google Scholar] [CrossRef]
- Vardavas, C.; Agaku, I.; Filippidis, F.; Kousoulis, A.A.; Girvalaki, C.; Symvoulakis, E.; Tzatzarakis, M.; Tsatsakis, A.M.; Behrakis, P.; Lionis, C. The Secondhand Smoke Exposure Scale (SHSES): A hair nicotine validated tool for assessing exposure to secondhand smoke among elderly adults in primary care. Tob. Prev. Cessat. 2017, 3, 9. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; García-Arellano, A.; Toledo, E.; Salas-Salvadó, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schröder, H.; Arós, F.; Gómez-Gracia, E.; et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: The PREDIMED trial. PLoS One 2012, 7, e43134. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the international physical activity questionnaire short form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef]
- IPAQ. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ). The International Physical Activity Questionnaire. 2005. Available online: https://cir.nii.ac.jp/crid/1573950400545533440?lang=en#citations_container (accessed on 2 February 2022).
- Haddad, C.; Khoury, C.; Salameh, P.; Sacre, H.; Hallit, R.; Kheir, N.; Obeid, S.; Hallit, S. Validation of the Arabic version of the eating attitude test in Lebanon: A population study. Public Health Nutr. 2020, 24, 1–12. [Google Scholar] [CrossRef]
- Garner, D.M.; Olmsted, M.P.; Bohr, Y.; Garfinkel, P.E. The eating attitudes test: Psychometric features and clinical correlates. Psychol. Med. 1982, 12, 871–878. [Google Scholar] [CrossRef]
- Alvarenga Mdos, S.; Scagliusi, F.B.; Philippi, S.T. Development and validity of the Disordered Eating Attitude Scale (DEAS). Percept. Mot. Ski. 2010, 110, 379–395. [Google Scholar] [CrossRef]
- Rogoza, R.; Hallit, S.; Soufia, M.; Barthels, F.; Obeid, S. Validation of the Arabic version of the Dusseldorf Orthorexia Scale (DOS) among Lebanese adolescents. J. Eat. Disord. 2021, 9, 130. [Google Scholar] [CrossRef] [PubMed]
- Hair, J.F., Jr.; Hult, G.T.M.; Ringle, C.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM); Sage publications: New York, NY, USA, 2017. [Google Scholar]
- Keane, A.; Willetts, A. Factors that affect food choice. Nutr. Food Sci. 1994, 4, 15–17. [Google Scholar] [CrossRef]
- Kearney, J.M.; Gibney, M.J.; Livingstone, M.B.; Robson, P.J.; Kiely, M.; Harrington, K.E. Attitudes towards and beliefs about nutrition and health among a random sample of adults in the Republic of Ireland and Northern Ireland. Public Health Nutr. 2001, 4, 1117–1126. [Google Scholar] [CrossRef] [PubMed]
- Reime, B.; Novak, P.; Born, J.; Hagel, E.; Wanek, V. Eating habits, health status, and concern about health: A study among 1641 employees in the German metal industry. Prev. Med. 2000, 30, 295–300. [Google Scholar] [CrossRef]
- Davis, C. From passive overeating to “food addiction”: A spectrum of compulsion and severity. ISRN Obes. 2013, 2013, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Brytek-Matera, A.; Onieva-Zafra, M.D.; Parra-Fernández, M.L.; Staniszewska, A.; Modrzejewska, J.; Fernández-Martínez, E. Evaluation of Orthorexia Nervosa and Symptomatology Associated with Eating Disorders among European University Students: A Multicentre Cross-Sectional Study. Nutrients 2020, 12, 3716. [Google Scholar] [CrossRef]
- Mitrofanova, E. From a Healthy Diet to Pathology: Exploring the Complexity of Orthorexia Nervosa. Ph.D. Thesis, Kingston University, London, UK, 2020. [Google Scholar]
- Health Consequences. National Eating Disorders Association. 2022. Available online: https://www.nationaleatingdisorders.org/health-consequences (accessed on 2 March 2022).
- Scarff, J.R. Orthorexia Nervosa: An Obsession With Healthy Eating. Fed. Pract. Health Care Prof. VA DoD PHS 2017, 34, 36–39. [Google Scholar]
- Koven, N.S.; Abry, A.W. The clinical basis of orthorexia nervosa: Emerging perspectives. Neuropsychiatr. Dis. Treat. 2015, 11, 385–394. [Google Scholar] [CrossRef]
- Academy for Eating Disorders. Eating Disorders: A Guide to Medical Care, 3rd ed.; Academy for Eating Disorders: Hong Kong, China, 2016. [Google Scholar]
- Hankey, G.J. The Role of Nutrition in the Risk and Burden of Stroke: An Update of the Evidence. Stroke 2017, 48, 3168–3174. [Google Scholar] [CrossRef]
- Spence, J. Nutrition and risk of stroke. Nutrients 2019, 11, 647. [Google Scholar] [CrossRef]
- Casas, R.; Sacanella, E.; Estruch, R. The immune protective effect of the Mediterranean diet against chronic low-grade inflammatory diseases. Endocr. Metab. Immune Disord. Drug Targets 2014, 14, 245–254. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013, 368, 1279–1290. [Google Scholar] [CrossRef] [PubMed]
- Samieri, C.; Sun, Q.; Townsend, M.K.; Chiuve, S.E.; Okereke, O.I.; Willett, W.C.; Stampfer, M.; Grodstein, F. The association between dietary patterns at midlife and health in aging: An observational study. Ann. Intern. Med. 2013, 159, 584–591. [Google Scholar] [CrossRef] [PubMed]
- Lourida, I.; Soni, M.; Thompson-Coon, J.; Purandare, N.; Lang, I.A.; Ukoumunne, O.C.; Llewellyn, D.J. Mediterranean diet, cognitive function, and dementia: A systematic review. Epidemiology 2013, 24, 479–489. [Google Scholar] [CrossRef]
- van de Rest, O.; Berendsen, A.A.; Haveman-Nies, A.; de Groot, L.C. Dietary patterns, cognitive decline, and dementia: A systematic review. Adv. Nutr. 2015, 6, 154–168. [Google Scholar] [CrossRef] [PubMed]
- Feart, C.; Samieri, C.; Barberger-Gateau, P. Mediterranean diet and cognitive health: An update of available knowledge. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 51–62. [Google Scholar] [CrossRef]
- Singh, B.; Parsaik, A.K.; Mielke, M.M.; Erwin, P.J.; Knopman, D.S.; Petersen, R.C.; Roberts, R.O. Association of Mediterranean diet with mild cognitive impairment and Alzheimer’s disease: A systematic review and meta-analysis. J. Alzheimers Dis. 2014, 39, 271–282. [Google Scholar] [CrossRef] [PubMed]
- Kontogianni, M.D.; Panagiotakos, D.B. Dietary patterns and stroke: A systematic review and re-meta-analysis. Maturitas 2014, 79, 41–47. [Google Scholar] [CrossRef]
- Demarin, V.; Lisak, M.; Morović, S. Mediterranean diet in healthy lifestyle and prevention of stroke. Acta Clin. Croat. 2011, 50, 67–77. [Google Scholar]
- Gardener, H.; Wright, C.B.; Gu, Y.; Demmer, R.; Boden-Albala, B.; Elkind, M.S.V.; Sacco, R.L.; Scarmeas, N. Mediterranean-style diet and risk of ischemic stroke, myocardial infarction, and vascular death: The Northern Manhattan Study. Am. J. Clin. Nutr. 2011, 94, 1458–1464. [Google Scholar] [CrossRef]
- Willett, W.C. The Mediterranean diet: Science and practice. Public Health Nutr. 2006, 9, 105–110. [Google Scholar] [CrossRef]
- Tuttolomondo, A.; Di Raimondo, D.; Pecoraro, R.; Casuccio, A.; Di Bona, D.; Aiello, A.; Accardi, G.; Arnao, V.; Clemente, G.; Corte, V.D.; et al. HLA and killer cell immunoglobulin-like receptor (KIRs) genotyping in patients with acute ischemic stroke. J. Neuroinflammation 2019, 16, 88. [Google Scholar] [CrossRef]
- Stromsnes, K.; Correas, A.G.; Lehmann, J.; Gambini, J.; Olaso-Gonzalez, G. Anti-Inflammatory Properties of Diet: Role in Healthy Aging. Biomedicines 2021, 9, 922. [Google Scholar] [CrossRef] [PubMed]
- Calle, M.C.; Andersen, C.J. Assessment of Dietary Patterns Represents a Potential, Yet Variable, Measure of Inflammatory Status: A Review and Update. Dis. Markers 2019, 2019, 3102870, Erratum in Dis. Markers 2019, 2019, 5454602. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, M.; Sánchez-Villegas, A.; De Irala, J.; Marti, A. Mediterranean Diet and Stroke: Objectives and Design of the SUN Project. Nutr. Neurosci. 2002, 5, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Salameh, P.; Farah, R.; Hallit, S.; Zeidan, R.K.; Chahine, M.N.; Asmar, R.; Hosseini, H. Self-reported history of stroke and long-term living conditions near air pollution sources: Results of a national epidemiological study in Lebanon. Environ. Monit. Assess. 2018, 190, 153. [Google Scholar] [CrossRef] [PubMed]
- Salameh, P.; Chahine, M.; Hallit, S.; Farah, R.; Zeidan, R.K.; Asmar, R.; Hosseiny, H. Hypertension prevalence and living conditions related to air pollution: Results of a national epidemiological study in Lebanon. Environ. Sci. Pollut. Res. Int. 2018, 25, 11716–11728. [Google Scholar] [CrossRef] [PubMed]
- Salameh, P.; Zeidan, R.K.; Hallit, S.; Farah, R.; Chahine, M.; Asmar, R.; Hosseini, H. Cardiovascular Diseases and Long-term Self-reported Exposure to Pollution: RESULTS OF A NATIONAL EPIDEMIOLOGICAL STUDY IN LEBANON. J. Cardiopulm. Rehabil. Prev. 2019, 39, 43–49. [Google Scholar] [CrossRef]
- Hu, Z.; Liebens, J.; Rao, K.R. Linking stroke mortality with air pollution, income, and greenness in northwest Florida: An ecological geographical study. Int. J. Health Geogr. 2008, 7, 20. [Google Scholar] [CrossRef]
- El-Hajj, M.; Salameh, P.; Rachidi, S.; Al-Hajje, A.; Hosseini, H. Cigarette and Waterpipe Smoking are Associated with the Risk of Stroke in Lebanon. J. Epidemiol. Glob. Health 2019, 9, 62–70. [Google Scholar] [CrossRef]
- Akl, E.A.; Gunukula, S.K.; Aleem, S.; Obeid, R.; Jaoude, P.A.; Honeine, R.; Irani, J. The prevalence of waterpipe tobacco smoking among the general and specific populations: A systematic review. BMC Public Health 2011, 11, 244. [Google Scholar] [CrossRef]
- Hou, L.; Han, W.; Jiang, J.; Liu, B.; Wu, Y.; Zou, X.; Xue, F.; Chen, Y.; Zhang, B.; Pang, H.; et al. Passive smoking and stroke in men and women: A national population-based case-control study in China. Sci. Rep. 2017, 7, 45542. [Google Scholar] [CrossRef] [PubMed]
- Jackson, C.A.; Sudlow, C.; Mishra, G.D. Education, sex and risk of stroke: A prospective cohort study in New South Wales, Australia. BMJ Open 2018, 8, e024070. [Google Scholar] [CrossRef] [PubMed]
- Wen, X.; Wu, Q.; Xie, M.; Li, W.; Liao, L. Education and stroke: Evidence from epidemiology and Mendelian randomization study. Sci. Rep. 2020, 10, 21208. [Google Scholar]
- Chen, R.; Ovbiagele, B.; Feng, W. Diabetes and Stroke: Epidemiology, Pathophysiology, Pharmaceuticals and Outcomes. Am. J. Med. Sci. 2016, 351, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Arboix, A. Cardiovascular risk factors for acute stroke: Risk profiles in the different subtypes of ischemic stroke. World J. Clin. Cases 2015, 3, 418–429. [Google Scholar] [CrossRef] [PubMed]
- Corlateanu, A.; Stratan, I.; Covantev, S.; Botnaru, V.; Siafakas, N. Asthma and stroke: A narrative review. Asthma Res. Pract. 2021, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.R.; Hwang, I.C.; Lee, Y.J.; Ham, E.B.; Park, D.K.; Kim, S. Stroke risk among patients with chronic obstructive pulmonary disease: A systematic review and meta-analysis. Clinics (Sao Paulo) 2018, 73, e177. [Google Scholar] [CrossRef] [PubMed]
- Guasch, E.; Mont, L. Exercise and the heart: Unmasking Mr Hyde. Heart 2014, 100, 999–1000. [Google Scholar] [CrossRef] [PubMed]
- Mostofsky, E.; Laier, E.; Levitan, E.B.; Rosamond, W.D.; Schlaug, G.; Mittleman, M.A. Physical Activity and Onset of Acute Ischemic Stroke: The Stroke Onset Study. Am. J. Epidemiol. 2011, 173, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Zakhour, M.; Haddad, C.; Sacre, H.; Tarabay, C.; Zeidan, R.K.; Akel, M.; Hallit, R.; Kheir, N.; Obeid, S.; Salameh, P.; et al. Differences in the Associations between Body Dissatisfaction and Eating Outcomes by Gender? A Lebanese Population Study. Rev. Epidemiol. Sante Publique 2021, 69, 134–144. [Google Scholar] [CrossRef] [PubMed]

| Variable | Ischemic Stroke Patients (N = 113) | Ischemic Stroke-Free Patients (N = 451) | p-Value |
|---|---|---|---|
| Mean ± SD | 0.035 | ||
| Age | 65.5 ± 11.9 | 62.9 ± 11.6 | |
| Gender | N (%) | 1 | |
| Male | 51 (45.1%) | 203 (45.0%) | |
| Female | 62 (54.9%) | 248 (55.0%) | |
| Marital Status | 0.020 | ||
| Single | 13 (11.5%) | 135 (29.9%) | |
| Married | 85 (75.2%) | 286 (63.4%) | |
| Divorced | 3 (2.7%) | 20 (4.4%) | |
| Widowed | 12 (10.6%) | 10 (2.2%) | |
| Educational Level | <0.001 | ||
| Primary-Complementary | 61 (54.0%) | 141 (31.3%) | |
| Secondary | 20 (17.7%) | 164 (36.4%) | |
| University | 32 (28.3%) | 146 (32.4%) | |
| MonthlyIncome | <0.001 | ||
| Low (<1000 USD) | 66 (58.4%) | 290 (64.3%) | |
| Intermediate (1000–2000 USD) | 25 (22.1%) | 147 (32.6%) | |
| High (>2000 USD) | 22 (19.5%) | 14 (3.1%) | |
| Pre-existing Physical Disorders | |||
| Hypertension | 82 (72.6%) | 254 (56.3%) | 0.002 |
| Dyslipidemia | 65 (57.5%) | 205 (45.5%) | 0.027 |
| Diabetes | 41 (36.3%) | 120 (26.6%) | 0.048 |
| Heart Diseases | 48 (42.5%) | 53 (11.8%) | <0.001 |
| Atrial Fibrillation | 34 (30.1%) | 36 (8.0%) | <0.001 |
| Asthma-COPD | 44 (38.9%) | 118 (26.2%) | 0.008 |
| Cancer | 2 (1.8%) | 15 (3.3%) | 0.545 |
| Obesity | 70 (61.9%) | 229 (50.8%) | 0.035 |
| Variable | Cases (N = 113) | Matched Controls (N = 451) | p-Value |
|---|---|---|---|
| Mean ± SD | |||
| MeD | 5.4 ± 3.1 | 7.6 ± 1.9 | <0.001 |
| Physical Activity (IPAQ) | 163.8 ± 232.7 | 79.3 ± 139.3 | <0.001 |
| Pollution Exposure | N (%) | ||
| Living 100 m from a crowded road | 0.002 | ||
| No | 47 (41.6%) | 261 (57.9%) | |
| Yes | 66 (58.4%) | 190 (42.1%) | |
| Living 100 m from an electricity generator | <0.001 | ||
| No | 55 (48.7%) | 332 (73.6%) | |
| Yes | 58 (51.3%) | 119 (26.4%) | |
| Model 1: Logistic regression taking the presence vs. absence of ischemic stroke as the dependent variable and taking eating attitudes as the independent variable. | |||
| Variables | p | aOR | 95% CI |
| Eating attitudes (EAT) | 0.020 | 1.040 | 1.006–1.074 |
| Living 100 m from a crowded road | 0.002 | 3.421 | 1.585–7.387 |
| Living 100 m from an electricity generator | 0.001 | 3.686 | 1.681–8.085 |
| Waterpipe (LWDS-11) | <0.001 | 1.204 | 1.117–1.297 |
| Exposure to passive smoking (SHSES) | <0.001 | 2.651 | 2.051–3.426 |
| Marital status (Yes vs. no) | 0.014 | 3.545 | 1.297–9.689 |
| Educational level (High vs. low) | 0.007 | 0.239 | 0.084–0.679 |
| Physical activity (IPAQ) | 0.007 | 1.003 | 1.001–1.006 |
| Diabetes | 0.019 | 2.550 | 1.169–5.561 |
| Heart diseases | 0.001 | 6.193 | 2.196–17.463 |
| Atrial fibrillation | 0.048 | 2.945 | 1.010–8.585 |
| Model 2: Logistic regression taking the presence vs. absence of ischemic stroke as the dependent variable and taking orthorexia nervosa and the Mediterranean diet (MD) as the independent variables. | |||
| Variables | p | aOR | 95% CI |
| Orthorexia nervosa (DOS) | 0.017 | 1.123 | 1.021–1.235 |
| Mediterranean diet (MeD) | <0.001 | 0.691 | 0.583–0.819 |
| Living 100 m from a crowded road | 0.015 | 2.731 | 1.212–6.151 |
| Living 100 m from an electricity generator | 0.002 | 3.842 | 1.659–8.902 |
| Waterpipe (LWDS-11) | <0.001 | 1.204 | 1.115–1.300 |
| Exposure to passive smoking (SHSES) | <0.001 | 2.641 | 1.998–3.491 |
| Marital status (Yes vs. no) | 0.010 | 4.457 | 1.419–14.002 |
| Educational level (High vs. low) | 0.006 | 0.195 | 0.061–0.623 |
| Heart diseases | 0.020 | 3.727 | 1.234–11.254 |
| Atrial fibrillation | 0.006 | 5.357 | 1.615–17.773 |
| Hypertension | 0.040 | 2.744 | 1.049–7.180 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maalouf, E.; Hallit, S.; Salameh, P.; Hosseini, H. Eating Behaviors, Lifestyle, and Ischemic Stroke: A Lebanese Case-Control Study. Int. J. Environ. Res. Public Health 2023, 20, 1487. https://doi.org/10.3390/ijerph20021487
Maalouf E, Hallit S, Salameh P, Hosseini H. Eating Behaviors, Lifestyle, and Ischemic Stroke: A Lebanese Case-Control Study. International Journal of Environmental Research and Public Health. 2023; 20(2):1487. https://doi.org/10.3390/ijerph20021487
Chicago/Turabian StyleMaalouf, Elise, Souheil Hallit, Pascale Salameh, and Hassan Hosseini. 2023. "Eating Behaviors, Lifestyle, and Ischemic Stroke: A Lebanese Case-Control Study" International Journal of Environmental Research and Public Health 20, no. 2: 1487. https://doi.org/10.3390/ijerph20021487
APA StyleMaalouf, E., Hallit, S., Salameh, P., & Hosseini, H. (2023). Eating Behaviors, Lifestyle, and Ischemic Stroke: A Lebanese Case-Control Study. International Journal of Environmental Research and Public Health, 20(2), 1487. https://doi.org/10.3390/ijerph20021487







