Evaluating Therapeutic Healthcare Environmental Criteria: Architectural Designers’ Perspectives
Abstract
:1. Introduction
1.1. Background
1.2. Healthcare Environmental Attributes and Their Impacts on Hospital Users Healing Experiences
1.2.1. Physical Space
1.2.2. Ambient Indoor Comfort
1.2.3. Interior Design
1.2.4. Nature and View
1.2.5. Safety
1.2.6. Management and Maintenance
1.2.7. Service and Social Support
1.3. Research Aim
- What are the essential therapeutic environmental factors perceived by architectural designers for the successful delivery of patient-centered, therapeutic, healthcare design?
- What healthcare environmental factors are perceived most importantly by architectural designers? How do such factors relate to architects’ personal and professional characteristics?
- Why are certain factors considered more important by architectural designers? Does the priority differ between their personal and firms perspectives?
- What are the hurdles in the implementation of such therapeutic healthcare environmental factors in hospital design practice? What can be suggested to improve the quality of therapeutic healthcare environments in the hospital design process?
2. Materials and Methods
2.1. Instrument and Variables
2.1.1. Survey
- Respondents’ personal and professional characteristics: sex, age, education, hospital design experiences (years), architect licensure, and field of design specialty.
- Importance of therapeutic healthcare environmental attributes: 27 variables from the relevant literature sources (Table 1). Respondents were asked to evaluate the importance of the 27 variables, considering a user-centric hospital design task. Respondents indicated the degree that they considered it important. A five-point Likert scale (1 = least important, 2 = not so important, 3 = neutral, 4 = important, and 5 = very important) was used to assess the level of importance of the 27 variables in the delivery of therapeutic healthcare facility design.
- Utilizing the two sections, the relationship between respondents’ personal and professional profiles and the assessment of the importance of the variables was examined. Respondents’ personal and practice profiles may impact architects’ response patterns on the level of importance of the 27 variables. All 27 variables in the survey were described in both Korean and English texts to ensure the meanings were clear. Additional visual aids (e.g., hospital photos, images, or virtual reality) were not combined because the visual representation may alter the way in which survey respondents judge the meaning of the text description [127,128]. As such, respondents’ evaluations relied on their tacit and explicit architectural knowledge developed through their professional practice experiences [129].
2.1.2. Interview
- Respondents’ personal and professional characteristics: sex, age, education, hospital design experiences (years), architect licensure, and the size of the firm (number of employees).
- The most important therapeutic environmental attributes among the 27 variables for the successful project delivery and the explanation of their importance from the personal point of view as well as from firms’ perspectives: a multiple selection of the variables is permitted and the reasons for the importance of each selected variable needs to be described.
- The selection of the therapeutic environmental attributes from the 27 variables that are more or less frequently implemented in the hospital design projects and the explanation of the reasons.
- Suggesting the ways to implement the therapeutic environmental attributes holistically in the healthcare facility design for the success of healing hospital design delivery.
2.2. Participants
2.2.1. Survey
2.2.2. Interview
2.2.3. Ethical Considerations
2.3. Analysis
2.3.1. Survey
2.3.2. Interview
3. Results
3.1. Survey
3.1.1. Respondents’ Personal and Professional Characteristics
3.1.2. Important Therapeutic Environmental Criteria (Factors and Items)
3.1.3. Priority among the Therapeutic Environmental Criteria (Factors and Items)
3.1.4. Relationship between Important Therapeutic Environmental Criteria and Respondents’ Personal and Professional Characteristics
3.2. Interview
3.2.1. Participants’ Personal and Professional Characteristics
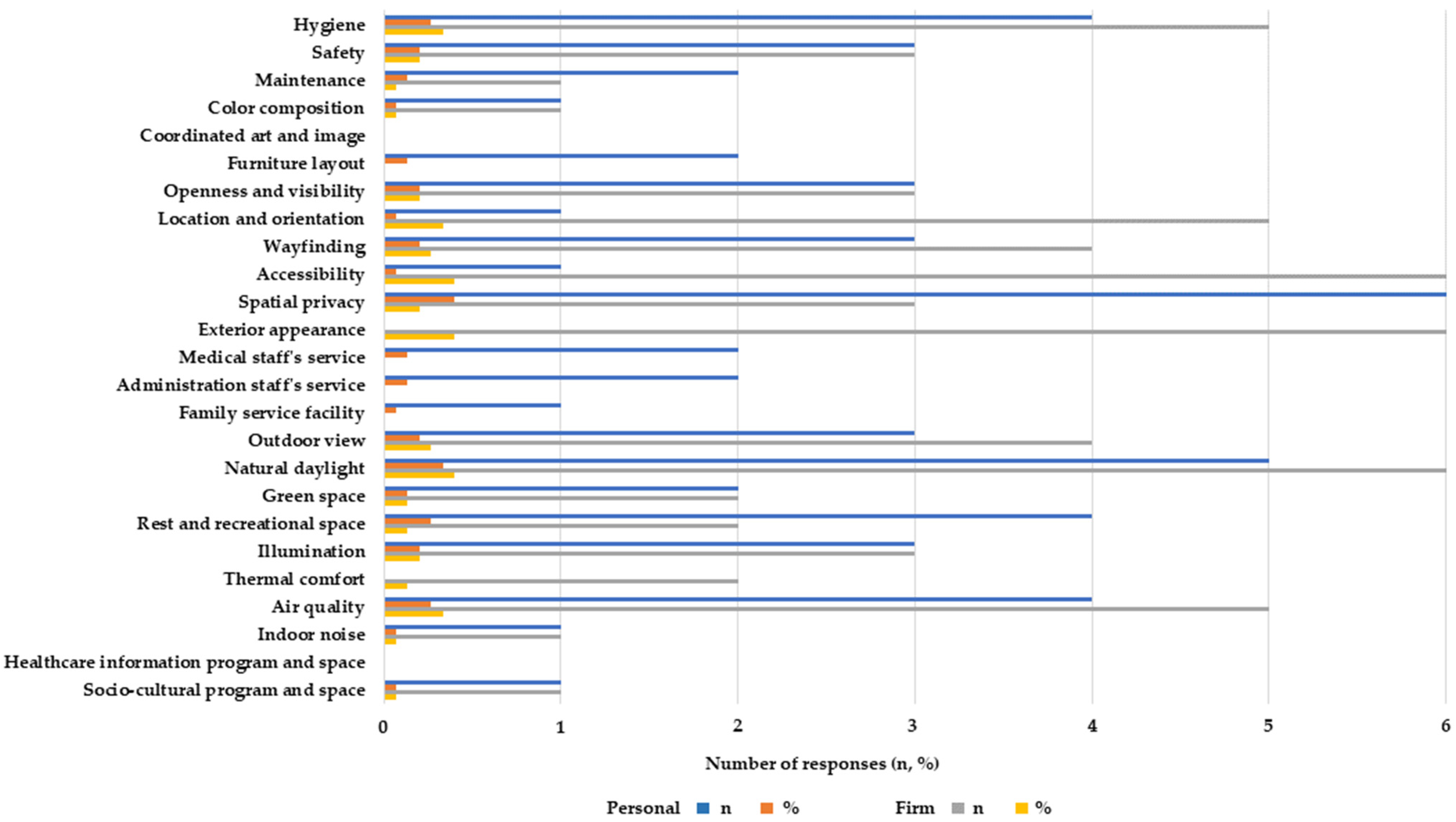
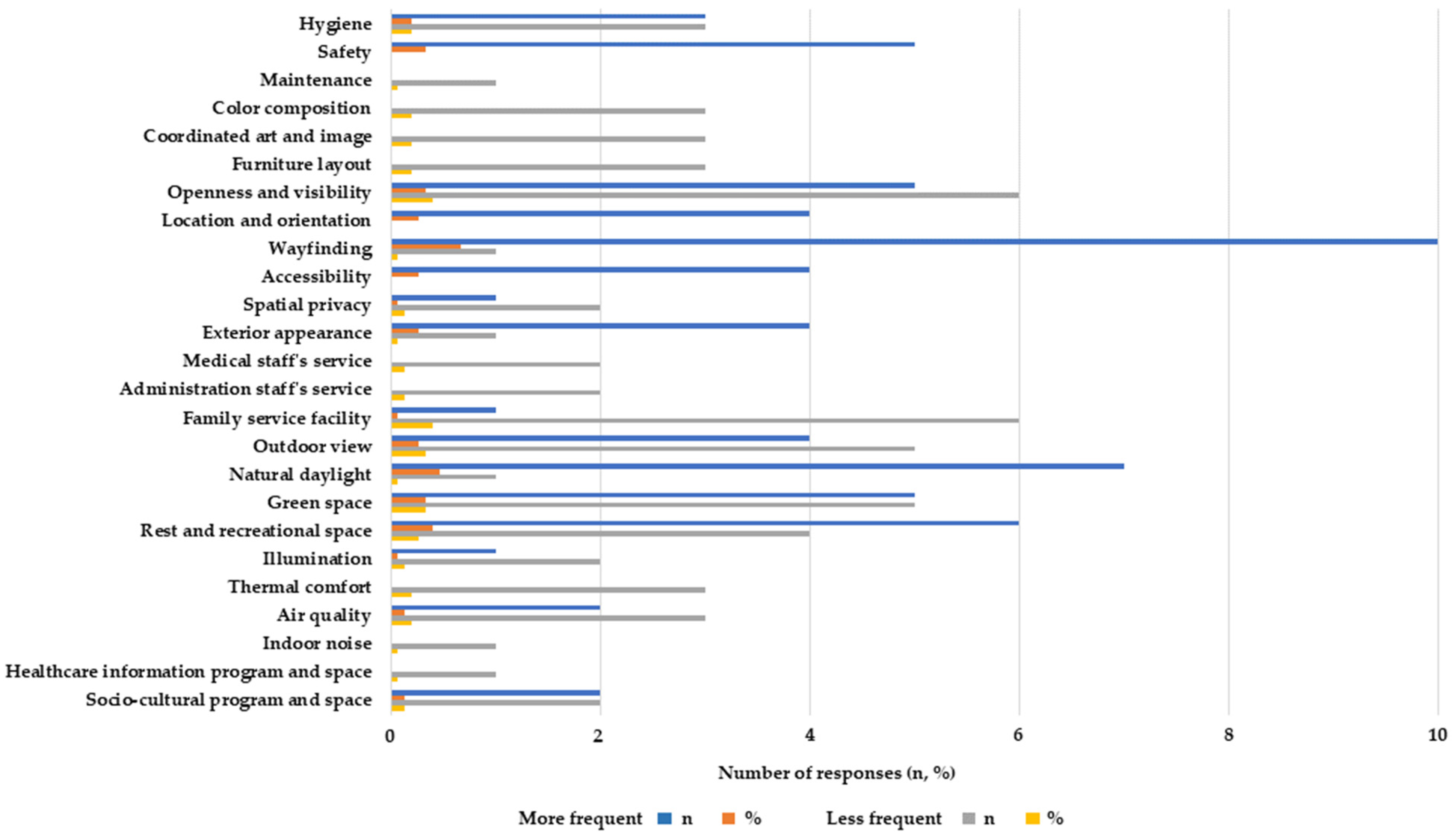
3.2.2. Priority in Design Implementation
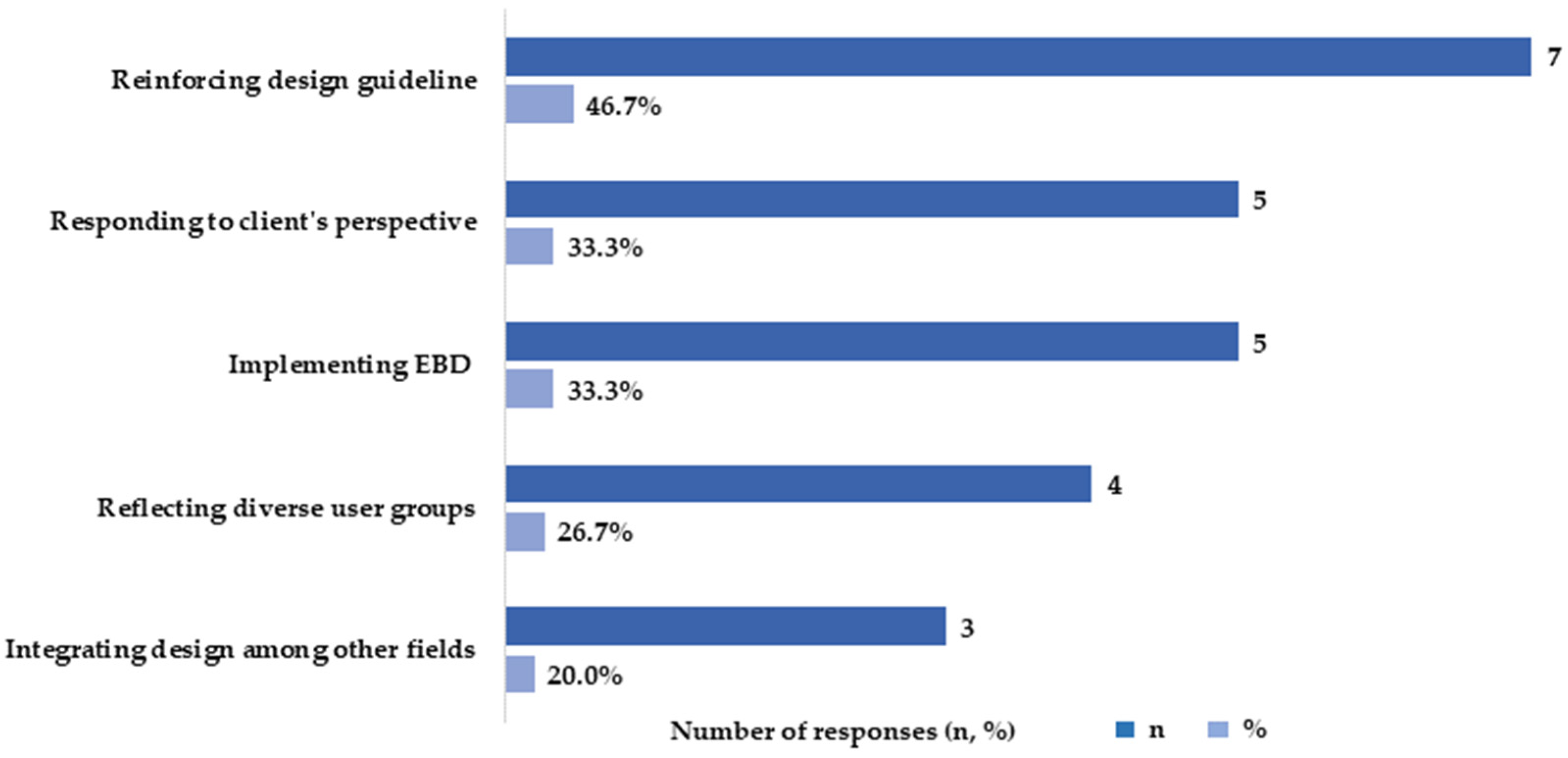
3.2.3. Hurdles and Suggestions in Design Practice
4. Discussion
4.1. Important Therapeutic Environmental Criteria
4.2. Relationship between the Important Environmental Criteria and the Respondents’ Characteristics
4.3. Implementation in Healthcare Design Practice
4.3.1. Personal vs. Firms’ Professional Dimension
“Facilitating the good quality daylight and air flow are perhaps, the most fundamental norms in the design of healthy hospital environment. Introducing natural daylight and allowing natural ventilation as well as maintaining good indoor air quality, are essential in the design of inpatient rooms and corridors. Such design principles are also significant in outpatient areas (i.e., lobby, hall, lounge, cafeteria, etc.). Hospital facilities with good quality natural daylight and air movement affect not only building occupants’ physiological health but also their psycho-emotional wellness.”
“In my personal view, natural elements and ambient atmosphere are primary for healing environments. However, in my firm’s sphere, physical and spatial properties become priority because spatial organization of rooms and equipment affects the overall design configuration as well as management performance and cost.”
“Functional layout of rooms and equipment is primal in my firms’ design approach, for the physical built environment impact on the long-term efficiency in usage, operation, and maintenance of buildings. Moreover, the physical design attributes affect the overall building aesthetics and for the most, impact on the sustainability of the hospital building.”
“As healthcare service becomes a more competitive industry, good quality physical design is emphasized more importantly as means to establish trustful and reputable image of hospitals.”
4.3.2. More vs. Less Frequent Implementation
“In the past, the motto of family-oriented healthcare service led to facilitation of family service spaces such as a family lounge, caretaker’s bed, rest area for families and visitors, etc. Since the spread of severe acute respiratory syndrome and COVID-19, family spaces received lesser attention, but instead moved toward non-caretaker healthcare service approach. Especially since the COVID-19 pandemic, families and visitors’ access is restricted and service spaces for family and visitors are getting eliminated in the hospital.”
“In many urban hospital projects, creating a sense of openness and providing sufficient green space are restricted. The complex list of a space program often requires more rooms for patients and medical services, compared to the available plot area of the project site. To offer green space, my project team used a roof-top garden. We throve to provide a separate green zone for inpatients from outpatients and visitors because of COVID-19. However, in many cases, a roof-top garden or an available lot for garden is not available owing to the complex requirement of rooms and equipment.”
4.4. Barriers and Suggestions in Design Practice
4.4.1. Reinforcing Design Guideline
“For instance, provision of a mandatory rest area per a hospital’s square area, or per the number of bed sits can be one of the design rules to improve implementation of the healing environment in hospitals.”
“For an effective design input, I recommend to revise the present healthcare service accreditation system to assess the quality of healing environmental design in hospital. In most cases, for the user-oriented operation and management of the hospital’s healthcare service, the South Korean Ministry of Health and Welfare runs healthcare accreditation system to monitor patient safety and hospital’s service quality. In most cases, larger hospitals or specialized hospital programs participate in the accreditation, whereas smaller or rural healthcare facilities do not. Under the current healthcare accreditation system, the facility’s spatial and physical environmental quality is a less concerned criteria.”
4.4.2. Clients’ Perspective
“Due to the changes in healthcare service policies and regulatory issues, the design construction budget and time are often fluctuating to reflect such changes in the design process. In many cases, clients concern more on the issues of functional requirement in facility programming and building operation but are less considerate on the aspects of the healing effects that can be achieved through the careful orchestration of the physical and socio-emotional design criteria for building users.”
4.4.3. EBD Practice
“In many cases, clients and users are healthcare professionals. They are very specific about their needs and think they know a lot more than architects in hospital design. Because of this low credibility on architects, we are often struggled to persuade clients to draw a better design solution.”
4.4.4. Consideration of Diverse User Groups
“Users are knowledgeable of their needs. Particularly, the clients, mostly, healthcare professionals have very specific desires. However, the access to information on other facets of healthcare users are extremely limited.”
4.4.5. Design Integration
“In the project design team, architects are responsible and in charge of almost everything from the exterior building design to medical space arrangement, mechanical electrical and plumbing technical solutions, document permitting, design supervision during construction, etc.”
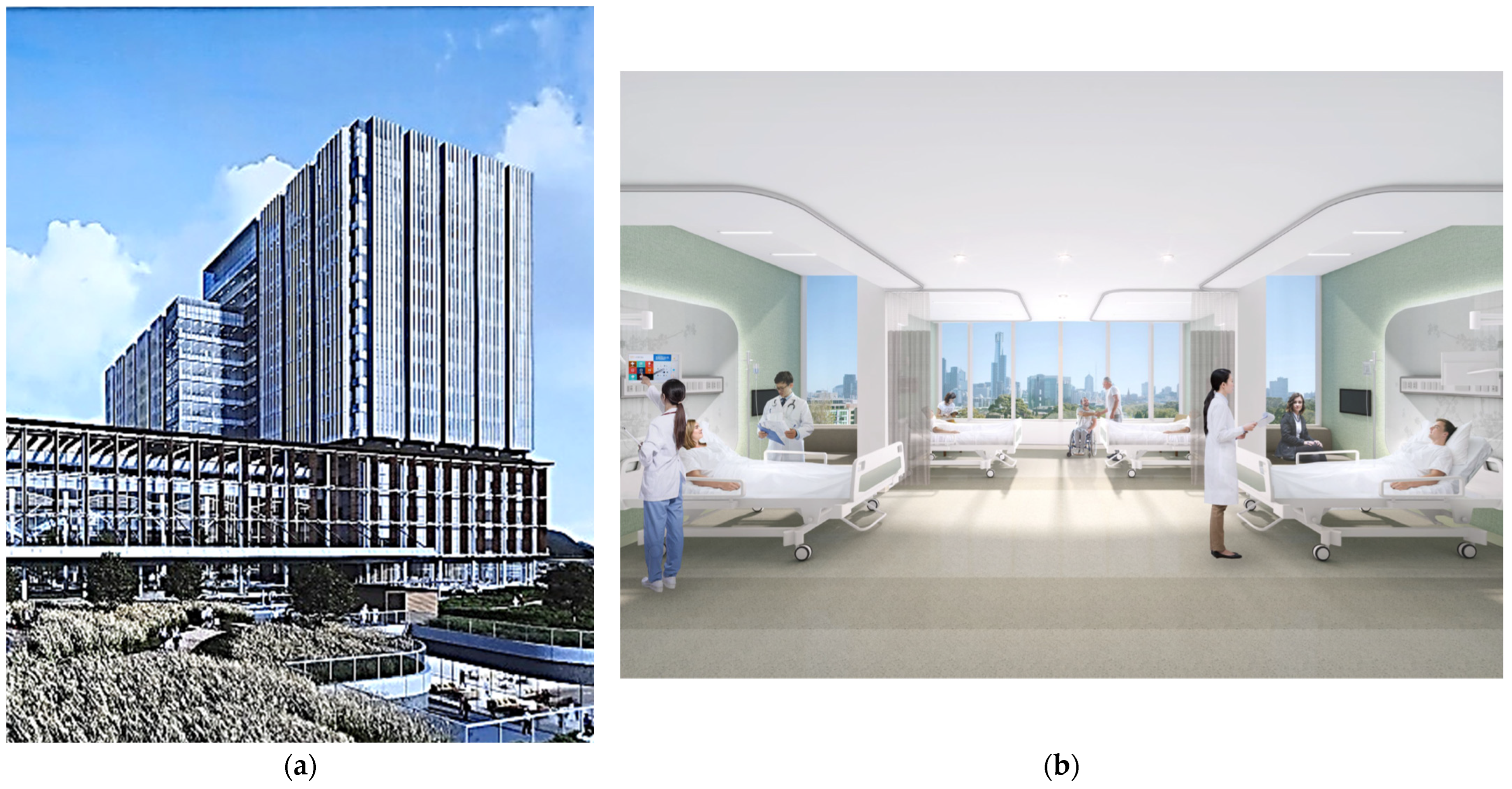
4.5. Design Examples
“It could have been an abandoned exterior space between the buildings, but I think this lounge design is a pinpoint at which the client’s consumer-oriented value and the architect’s design orientation are aligned. Usually, persuasion of medical clients is not an easy process because functionality, efficiency, and saving construction costs are the clients’ primary interests. But, in this case, a consensus was found between the client and the design team. The clients’ understanding of the healing space was very sophisticated. I think the most fundamental part in creating a healing environment comes through the process of finding a common point between the client’s and designer’s values.”
“We have not found any research information from the hospital’s own investigation or from any academic research institute on this lounge design. Either such data does not exist, or even if it does, access to the data, especially if done from the hospital, would be difficult to obtain. Typically, hospitals restrict disclosure of any kind of user related data, even when such information is not relevant to their medical record.”
“Since most hospitals do not have their own facility design guidelines concerning healing environments, design guidelines are mostly tailored to the specific hospital, which are suggested by the project architects via consultation with healthcare staff during the hospital design process. This was an exemplary case in which the clients’ advocation and hospital users’ satisfaction (although not systematically researched) for the indoor healing garden were high, and the lesson from this example will allow us to pursue a similar or an upgraded indoor atrium space in other hospitals.”
“As a trade-off for the wider and expanded unit area, we proposed a more efficient parking layout module which can reduce dead space in the basement parking floors. This idea convinced the client because the improved inpatient ward design could improve competitiveness with similar hospitals.”
“We collaborated with an overseas design firm that conducts behavior simulation design through data algorithms. During the design process, our teams were able to create a scenario based on nurses’ daily routines from the design team’s observational studies and direct interviews with nurses because such data were not available from the hospital. By comparing the experimental results of the nurses’ simulated movement distance according to the daily routine scenario in the square vs. linear floorplan, we confirmed that the square floorplan shape reduced the nurse’s movement distance by approximately 38%. With the help of this simulation, we refined the floorplan and adjusted orientation of the overall building so that there are no wards facing due direct north. Furthermore, this data-based design collaboration resulted in higher praise from the medical clients and eventually won the competition via our unique design challenge.”
5. Conclusions
- Avoiding obsolescence and rigidity to allow for flexible spatial reconfiguration for future expansion and particularly for effective infection control and management.
- Fostering socio-cultural service functions in healthcare facility design by integrating art, new technology, and the organization’s healthcare design and service philosophy.
- Suggesting a new design guidance or accreditation system that promotes the implementation of therapeutic healthcare design; for example, regulating a minimum rest space area per bedsit, or by a certain percentage of patient and staff areas.
- Promoting a multi-disciplinary and integrated healthcare design practice, based on scientific research data. Validated design strategies through case studies and evidence-based evaluation in domestic empirical hospital settings have not been sufficiently linked to healthcare design practices. Through integrated research and design practice, decision-making in the design and management phases can be more fluent, leading to successful healthcare design delivery.
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Factors and Items | Personal | Firm | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Factor 1: Management | Hygiene | 4 | 26.7 | 5 | 33.3 |
| Safety | 3 | 20.0 | 3 | 20.0 | |
| Maintenance | 2 | 13.3 | 1 | 6.7 | |
| Factor 2: Interior design | Color composition | 1 | 6.7 | 1 | 6.7 |
| Coordinated art and image | 0 | 0.0 | 0 | 0.0 | |
| Furniture layout | 2 | 13.3 | 0 | 0.0 | |
| Factor 3: Spatial quality | Openness and visibility | 3 | 20.0 | 3 | 20.0 |
| Location and orientation | 1 | 6.7 | 5 | 33.3 | |
| Wayfinding | 3 | 20.0 | 4 | 26.7 | |
| Accessibility | 1 | 6.7 | 6 | 40.0 | |
| Spatial privacy | 6 | 40.0 | 3 | 20.0 | |
| Exterior appearance | 0 | 0.0 | 6 | 40.0 | |
| Factor 4: Service | Medical staff’s service | 2 | 13.3 | 0 | 0.0 |
| Administration staff’s service | 2 | 13.3 | 0 | 0.0 | |
| Family service facility | 1 | 6.7 | 0 | 0.0 | |
| Factor 5: Nature and rest | Outdoor view | 3 | 20.0 | 4 | 26.7 |
| Natural daylight | 5 | 33.3 | 6 | 40.0 | |
| Green space | 2 | 13.3 | 2 | 13.3 | |
| Rest and recreational space | 4 | 26.7 | 2 | 13.3 | |
| Factor 6: Ambient indoor comfort | Illumination | 3 | 20.0 | 3 | 20.0 |
| Thermal comfort | 0 | 0.0 | 2 | 13.3 | |
| Air quality | 4 | 26.7 | 5 | 33.3 | |
| Indoor noise | 1 | 6.7 | 1 | 6.7 | |
| Factor 7: Social program and space | Health information program and space | 0 | 0.0 | 0 | 0.0 |
| Socio-cultural program and space | 1 | 6.7 | 1 | 6.7 | |
| Factors and Items | More Frequent | Less Frequent | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Factor 1: Management | Hygiene | 3 | 20.0 | 3 | 20.0 |
| Safety | 5 | 33.3 | 0 | 0.0 | |
| Maintenance | 0 | 0.0 | 1 | 6.7 | |
| Factor 2: Interior design | Color composition | 0 | 0.0 | 3 | 20.0 |
| Coordinated art and image | 0 | 0.0 | 3 | 20.0 | |
| Furniture layout | 0 | 0.0 | 3 | 20.0 | |
| Factor 3: Spatial quality | Openness and visibility | 5 | 33.3 | 6 | 40.0 |
| Location and orientation | 4 | 26.7 | 0 | 0.0 | |
| Wayfinding | 10 | 66.7 | 1 | 6.7 | |
| Accessibility | 4 | 26.7 | 0 | 0.0 | |
| Spatial privacy | 1 | 6.7 | 2 | 13.3 | |
| Exterior appearance | 4 | 26.7 | 1 | 6.7 | |
| Factor 4: Service | Medical staff’s service | 0 | 0.0 | 2 | 13.3 |
| Administration staff’s service | 0 | 0.0 | 2 | 13.3 | |
| Family service facility | 1 | 6.7 | 6 | 40.0 | |
| Factor 5: Nature and rest | Outdoor view | 4 | 26.7 | 5 | 33.3 |
| Natural daylight | 7 | 46.7 | 1 | 6.7 | |
| Green space | 5 | 33.3 | 5 | 33.3 | |
| Rest and recreational space | 6 | 40.0 | 4 | 26.7 | |
| Factor 6: Ambient indoor comfort | Illumination | 1 | 6.7 | 2 | 13.3 |
| Thermal comfort | 0 | 0.0 | 3 | 20.0 | |
| Air quality | 2 | 13.3 | 3 | 20.0 | |
| Indoor noise | 0 | 0.0 | 1 | 6.7 | |
| Factor 7: Social program and space | Health information program and space | 0 | 0.0 | 1 | 6.7 |
| Socio-cultural program and space | 2 | 13.3 | 2 | 13.3 | |
References
- Curtis, S.; Gesler, W.; Fabian, K.; Francis, S.; Priebe, S. Therapeutic landscapes in hospital design: A qualitative assessment by staff and service users of the design of a new mental health inpatient unit. Environ. Plan. C Gov. Policy 2007, 25, 591–610. [Google Scholar] [CrossRef] [Green Version]
- Gaminiesfahani, H.; Lozanovska, M.; Tucker, R.A. Scoping review of the impact on children of the built environment design characteristics of healing spaces. Health Environ. Res. Des. J. 2020, 13, 98–114. [Google Scholar] [CrossRef] [PubMed]
- Gesler, W.; Bell, M.; Curtis, S.; Hubbard, P.; Francis, S. Therapy by design: Evaluating the UK hospital building program. Health Place 2004, 10, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Huisman, E.R.; Morales, E.; van Hoof, J.; Kort, H.S. Healing environment: A review of the impact of physical environmental factors on users. Build. Environ. 2012, 58, 70–80. [Google Scholar] [CrossRef] [Green Version]
- Iyendo, T.O.; Uwajeh, P.C.; Ikenna, E.S. The therapeutic impacts of environmental design interventions on wellness in clinical settings: A narrative review. Complement. Ther. Clin. Pract. 2016, 24, 174–188. [Google Scholar] [CrossRef] [PubMed]
- Schweitzer, M.; Gilpin, L.; Frampton, S. Healing spaces: Elements of environmental design that make an impact on health. J. Altern. Complement. Med. 2004, 10 (Suppl. 1), S71–S83. [Google Scholar] [CrossRef] [Green Version]
- Stichler, J.F. Creating healing environments in critical care units. Crit. Care Nurs. Q. 2004, 24, 1–20. [Google Scholar] [CrossRef]
- Andrade, C.C.; Lima, M.L.; Pereira, C.R.; Fornara, F.; Bonaiuto, M. Inpatients’ and outpatients’ satisfaction: The mediating role of perceived quality of physical and social environment. Health Place 2013, 21, 122–132. [Google Scholar] [CrossRef] [Green Version]
- Dijkstra, K.; Pieterse, M.; Pruyn, A. Physical environmental stimuli that turn healthcare facilities into healing environments through psychologically mediated effects: Systematic review. J. Adv. Nurs. 2006, 56, 166–181. [Google Scholar] [CrossRef]
- Rashid, M.; Zimring, C. A review of the empirical literature on the relationships between indoor environment and stress in health care and office settings: Problems and prospects of sharing evidence. Environ. Behav. 2008, 40, 151–190. [Google Scholar] [CrossRef]
- Salonen, H.; Lahtinen, M.; Lappalainen, S.; Nevala, N.; Knibbs, L.D.; Morawska, L.; Reijula, K. Physical characteristics of the indoor environment that affect health and wellbeing in healthcare facilities: A review. Intell. Build. Int. 2013, 5, 3–25. [Google Scholar] [CrossRef] [Green Version]
- Simonsen, T.; Sturge, J.; Duff, C. Healing architecture in healthcare: A scoping review. Health Environ. Res. Des. J. 2022, 15, 315–328. [Google Scholar] [CrossRef] [PubMed]
- Codinhoto, R.; Tzortzopoulos, P.; Kagioglou, M.; Aouad, G.; Cooper, R. The impacts of the built environment on health outcomes. Facilities 2009, 27, 138–151. [Google Scholar] [CrossRef]
- Devlin, A.S.; Arneill, A.B. Health care environments and patient outcomes: A review of the literature. Environ. Behav. 2003, 35, 665–694. [Google Scholar] [CrossRef]
- Zhang, Y.; Tzortzopoulos, P.; Kagioglou, M. Healing built-environment effects on health outcomes: Environment-occupant-health framework. Build. Res. Inf. 2019, 47, 747–766. [Google Scholar] [CrossRef] [Green Version]
- Joseph, A.; Quan, X.; Keller, A.B.; Taylor, E.; Nanda, U.; Hua, Y. Building a knowledge base for evidence-based healthcare facility design through a post-occupancy evaluation toolkit. Intell. Build. Int. 2014, 6, 155–169. [Google Scholar] [CrossRef]
- Peters, T.; Verderber, S. Territories of engagement in the design of ecohumanist healthcare environments. Health Environ. Res. Des. J. 2017, 10, 104–123. [Google Scholar] [CrossRef]
- Becker, F.; Parsons, K.S. Hospital facilities and the role of evidence-based design. J. Facil. Manag. 2007, 5, 263–274. [Google Scholar] [CrossRef] [Green Version]
- Brown, C.E.; Ecoff, L.A. Systematic approach to the inclusion of evidence in healthcare design. Health Environ. Res. Des. J. 2011, 4, 7–16. [Google Scholar] [CrossRef]
- Ulrich, R.S.; Zimring, C.; Zhu, X.; Dubose, J.; Seo, H.B.; Choi, Y.S.; Quan, X.; Joseph, A. A review of the research literature on evidence-based healthcare design. Health Environ. Res. Des. J. 2008, 1, 61–125. [Google Scholar] [CrossRef]
- Verderber, S.; Jiang, S.; Hughes, G.; Xiao, Y. The evolving role of evidence-based research in healthcare facility design competitions. Front. Archit. Res. 2014, 3, 238–249. [Google Scholar] [CrossRef] [Green Version]
- Jiang, S.; Verderber, S. On the planning and design of hospital circulation zones: A review of the evidence-based literature. Health Environ. Res. Des. J. 2017, 10, 124–146. [Google Scholar] [CrossRef] [PubMed]
- Pati, D.; Harvey, T.E., Jr.; Willis, D.A.; Pati, S. Identifying elements of the health care environment that contribute to wayfinding. Health Environ. Res. Des. J. 2015, 8, 44–67. [Google Scholar] [CrossRef] [PubMed]
- Hua, Y.; Becker, F.; Wurmser, T.; Bliss-Holtz, J.; Hedges, C. Effects of nursing unit spatial layout on nursing team communication patterns, quality of care, and patient safety. Health Environ. Res. Des. J. 2012, 6, 8–38. [Google Scholar] [CrossRef] [PubMed]
- Seo, H.B.; Choi, Y.S.; Zimring, C. Impact of hospital unit design for patient-centered care on nurses’ behavior. Environ. Behav. 2011, 43, 443–468. [Google Scholar] [CrossRef]
- Zamani, Z. Effects of emergency department physical design elements on security, wayfinding, visibility, privacy, and efficiency and its implications on staff satisfaction and performance. Health Environ. Res. Des. J. 2019, 12, 72–88. [Google Scholar] [CrossRef]
- Chaudhury, H.; Mahmood, A.; Valente, M. Advantages and disadvantages of single-versus multiple-occupancy rooms in acute care environments: A review and analysis of the literature. Environ. Behav. 2005, 37, 760–786. [Google Scholar] [CrossRef]
- Shepley, M.M.; Harris, D.D.; White, R. Open-bay and single-family room neonatal intensive care units: Caregiver satisfaction and stress. Environ. Behav. 2008, 40, 249–268. [Google Scholar] [CrossRef]
- Barlas, D.; Sama, A.E.; Ward, M.F.; Lesser, M.L. Comparison of the auditory and visual privacy of emergency department treatment areas with curtains versus those with solid walls. Ann. Emerg. Med. 2001, 38, 135–139. [Google Scholar] [CrossRef]
- Devlin, A.S. Judging a book by its cover: Medical building facades and judgments of care. Environ. Behav. 2008, 40, 307–329. [Google Scholar] [CrossRef]
- Gola, M.; Caggiano, G.; De Giglio, O.; Napoli, C.; Diella, G.; Carlucci, M.; Carpagnano, L.F.; D’Alessandro, D.; Joppolo, C.M.; Capolongo, S.; et al. SARS-CoV-2 indoor contamination: Considerations on anti-COVID-19 management of ventilation systems, and finishing materials in healthcare facilities. Ann. Ig. 2021, 33, 381–392. [Google Scholar] [PubMed]
- Capolongo, S.; Gola, M.; Brambilla, A.; Morganti, A.; Mosca, E.I.; Barach, P. COVID-19 and Healthcare facilities: A decalogue of design strategies for resilient hospitals. Acta Biomed. 2020, 91, 50–60. [Google Scholar] [PubMed]
- Van den Berg, A.E. Health benefits of natural elements. In Health Impacts of Healing Environments: A Review of Evidence for Benefits of Nature, Daylight, Fresh Air, and Quiet in Healthcare Settings; UMCG: Groningen, The Netherlands, 2005; pp. 37–41. [Google Scholar]
- Choi, J.H.; Beltran, L.O.; Kim, H.S. Impacts of indoor daylight environments on patient average length of stay (ALOS) in a healthcare facility. Build. Environ. 2012, 50, 65–75. [Google Scholar] [CrossRef]
- Lieverse, R.; Van Someren, E.J.; Nielen, M.M.; Uitdehaag, B.M.; Smit, J.H.; Hoogendijk, W.J. Bright light treatment in elderly patients with nonseasonal major depressive disorder: A randomized placebo-controlled trial. Arch. Gen. Psychiatry 2011, 68, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Shepley, M.M.; Gerbi, R.P.; Watson, A.E.; Imgrund, S.; Sagha-Zadeh, R. The impact of daylight and views on ICU patients and staff. Health Environ. Res. Des. J. 2012, 5, 46–60. [Google Scholar] [CrossRef] [PubMed]
- Zadeh, R.S.; Shepley, M.M.; Williams, G.; Chung, S.S.E. The impact of windows and daylight on acute-care nurses’ physiological, psychological, and behavioral health. Health Environ. Res. Des. J. 2014, 7, 35–61. [Google Scholar] [CrossRef] [PubMed]
- Hsu, T.; Ryherd, E.; Waye, K.P.; Ackerman, J. Noise pollution in hospitals: Impact on patients. JCOM 2012, 19, 301–309. [Google Scholar]
- Choiniere, D.B. The effects of hospital noise. Nurs. Adm. Q. 2010, 34, 327–333. [Google Scholar] [CrossRef]
- Balaras, C.A.; Dascalaki, E.; Gaglia, A. HVAC and indoor thermal conditions in hospital operating rooms. Energy Build. 2007, 39, 454–470. [Google Scholar] [CrossRef]
- Hwang, R.L.; Lin, T.P.; Cheng, M.J.; Chien, J.H. Patient thermal comfort requirement for hospital environments in Taiwan. Build. Environ. 2007, 42, 2980–2987. [Google Scholar] [CrossRef]
- Gola, M.; Settimo, G.; Capolongo, S. Indoor air quality in inpatient environments: A systematic review on factors that influence chemical pollution in inpatient wards. J. Healthc. Eng. 2019, 2019, 8358306. [Google Scholar] [CrossRef] [PubMed]
- Gola, M.; Settimo, G.; Capolongo, S. How can design features and other factors affect the indoor air quality in inpatient rooms? Check-lists for the design phase, daily procedures and maintenance activities for reducing the air concentrations of chemical pollution. Int. J. Environ. Res. Public Health 2020, 17, 4280. [Google Scholar] [CrossRef] [PubMed]
- Aghalari, Z.; Dahms, H.U.; Sosa-Hernandez, J.E.; Oyervides-Munoz, M.A.; Parra-Saldívar, R. Evaluation of SARS-COV-2 transmission through indoor air in hospitals and prevention methods: A systematic review. Environ. Res. 2021, 195, 110841. [Google Scholar] [CrossRef] [PubMed]
- Karlin, B.E.; Zeiss, R.A. Best practices: Environmental and therapeutic issues in psychiatric hospital design: Toward best practices. Psychiatr. Serv. 2006, 57, 1376–1378. [Google Scholar] [CrossRef]
- Leather, P.; Beale, D.; Santos, A.; Watts, J.; Lee, L. Outcomes of environmental appraisal of different hospital waiting areas. Environ. Behav. 2003, 35, 842–869. [Google Scholar] [CrossRef] [Green Version]
- Mroczek, J.; Mikitarian, G.; Vieira, E.K.; Rotarius, T. Hospital design and staff perceptions: An exploratory analysis. Health Care Manag. 2005, 24, 233–244. [Google Scholar] [CrossRef]
- Chaudhury, H.; Mahmood, A.; Valente, M. The effect of environmental design on reducing nursing errors and increasing efficiency in acute care settings: A review and analysis of the literature. Environ. Behav. 2009, 41, 755–786. [Google Scholar] [CrossRef]
- Tzeng, H.M.; Yin, C.Y. Perspectives of recently discharged patients on hospital fall-prevention programs. J. Nurs. Care Qual. 2009, 24, 42–49. [Google Scholar] [CrossRef]
- Alzoubi, H.; Bataineh, R.F. Pre-versus post-occupancy evaluation of daylight quality in hospitals. Build. Environ. 2010, 45, 2652–2665. [Google Scholar] [CrossRef]
- Devlin, A.S.; Donovan, S.; Nicolov, A.; Nold, O.; Packard, A.; Zandan, G. “Impressive?” Credentials, family photographs, and the perception of therapist qualities. J. Environ. Psychol. 2009, 29, 503–512. [Google Scholar] [CrossRef]
- Nanda, U.; Chanaud, C.; Nelson, M.; Zhu, X.; Bajema, R.; Jansen, B.H. Impact of visual art on patient behavior in the emergency department waiting room. J. Emerg. Med. 2012, 43, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Coad, J.; Coad, N. Children and young people’s preference of thematic design and colour for their hospital environment. J. Child Health Care 2008, 12, 33–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalantari, S.; Snell, R. Post-occupancy evaluation of a mental healthcare facility based on staff perceptions of design innovations. Health Environ. Res. Des. J. 2017, 10, 121–135. [Google Scholar] [CrossRef] [PubMed]
- Dianat, I.; Sedghi, A.; Bagherzade, J.; Jafarabadi, M.A.; Stedmon, A.W. Objective and subjective assessments of lighting in a hospital setting: Implications for health, safety and performance. Ergonomics 2013, 56, 1535–1545. [Google Scholar] [CrossRef]
- Kamali, N.J.; Abbas, M.Y. Healing environment: Enhancing nurses’ performance through proper lighting design. Procedia Soc. Behav. Sci. 2012, 35, 205–212. [Google Scholar] [CrossRef] [Green Version]
- Joseph, A.; Rashid, M. The architecture of safety: Hospital design. Curr. Opin. Crit. Care 2007, 13, 714–719. [Google Scholar] [CrossRef]
- Abdelaal, M.S.; Soebarto, V. Biophilia and salutogenesis as restorative design approaches in healthcare architecture. Archit. Sci. Rev. 2019, 62, 195–205. [Google Scholar] [CrossRef]
- Ulrich, R.S. Health benefits of gardens in hospitals. In Proceedings of the Plants for People International Exhibition, Floriade, The Netherlands, 22 April 2002. [Google Scholar]
- Whitehouse, S.; Varni, J.W.; Seid, M.; Cooper-Marcus, C.; Ensberg, M.J.; Jacobs, J.R.; Mehlenbeck, R.S. Evaluating a children’s hospital garden environment: Utilization and consumer satisfaction. J. Environ. Psychol. 2001, 21, 301–314. [Google Scholar] [CrossRef] [Green Version]
- Beukeboom, C.J.; Langeveld, D.; Tanja-Dijkstra, K. Stress-reducing effects of real and artificial nature in a hospital waiting room. J. Altern. Complement. Med. 2012, 18, 329–333. [Google Scholar] [CrossRef]
- Dijkstra, K.; Pieterse, M.E.; Pruyn, A. Stress-reducing effects of indoor plants in the built healthcare environment: The mediating role of perceived attractiveness. Prev. Med. 2008, 47, 279–283. [Google Scholar] [CrossRef]
- Marcus, C.C. Healing gardens in hospitals. Interdiscip. Des. Res. e-J. 2007, 1, 1–27. [Google Scholar]
- Park, S.H.; Mattson, R.H. Ornamental indoor plants in hospital rooms enhanced health outcomes of patients recovering from surgery. J. Altern. Complement. Med. 2009, 15, 975–980. [Google Scholar] [CrossRef] [PubMed]
- Grinde, B.; Patil, G.G. Biophilia: Does visual contact with nature impact on health and well-being? Int. J. Environ. Res. Public Health 2009, 6, 2332–2343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raanaas, R.K.; Patil, G.G.; Hartig, T. Health benefits of a view of nature through the window: A quasi-experimental study of patients in a residential rehabilitation center. Clin. Rehabil. 2012, 26, 21–32. [Google Scholar] [CrossRef]
- Cordoza, M.; Ulrich, R.S.; Manulik, B.J.; Gardiner, S.K.; Fitzpatrick, P.S.; Hazen, T.M.; Mirka, A.; Perkins, R.S. Impact of nurses taking daily work breaks in a hospital garden on burnout. Am. J. Crit. Care 2018, 27, 508–512. [Google Scholar] [CrossRef]
- Naderi, J.R.; Shin, W.H. Humane design for hospital landscapes: A case study in landscape architecture of a healing garden for nurses. Health Environ. Res. Des. J. 2008, 2, 82–119. [Google Scholar] [CrossRef]
- Ulrich, R.S.; Cordoza, M.; Gardiner, S.K.; Manulik, B.J.; Fitzpatrick, P.S.; Hazen, T.M.; Perkins, R.S. ICU patient family stress recovery during breaks in a hospital garden and indoor environments. Health Environ. Res. Des. J. 2020, 13, 83–102. [Google Scholar] [CrossRef]
- Pasha, S. Barriers to garden visitation in children’s hospitals. Health Environ. Res. Des. J. 2013, 6, 76–96. [Google Scholar] [CrossRef]
- Pasha, S.; Shepley, M.M. Research note: Physical activity in pediatric healing gardens. Landsc. Urban Plan. 2013, 118, 53–58. [Google Scholar] [CrossRef]
- Lakhani, A.; Martin, K.; Gray, L.; Mallison, J.; Grimbeek, P.; Hollins, I.; Mackareth, C. What is the impact of engaging with natural environments delivered via virtual reality on the psycho-emotional health of people with spinal cord injury receiving rehabilitation in hospital? Findings from a pilot randomized controlled trial. Arch. Phys. Med. Rehabil. 2020, 101, 1532–1540. [Google Scholar] [CrossRef]
- Ehrlich, H.; McKenney, M.; Elkbuli, A. Protecting our healthcare workers during the COVID-19 pandemic. Am. J. Emerg. Med. 2020, 38, 1527. [Google Scholar] [CrossRef] [PubMed]
- Shreffler, J.; Petrey, J.; Huecker, M. The impact of COVID-19 on healthcare worker wellness: A scoping review. West. J. Emerg. Med. 2020, 21, 1059. [Google Scholar] [CrossRef] [PubMed]
- Putrino, D.; Ripp, J.; Herrera, J.E.; Cortes, M.; Kellner, C.; Rizk, D.; Dams-O’Connor, K. Multisensory, nature-inspired recharge rooms yield short-term reductions in perceived stress among frontline healthcare workers. Front. Psychol. 2020, 11, 560833. [Google Scholar] [CrossRef] [PubMed]
- Stichler, J.F. Patient safety: A priority for healthcare and for healthcare design. Health Environ. Res. Des. J. 2016, 9, 10–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zadeh, R.; Sadatsafavi, H.; Xue, R. Evidence-based and value-based decision making about healthcare design: An economic evaluation of the safety and quality outcomes. Health Environ. Res. Des. J. 2015, 8, 58–76. [Google Scholar] [CrossRef] [PubMed]
- Reiling, J.; Hughes, R.G.; Murphy, M.R. The Impact of Facility Design on Patient Safety. Patient Safety and Quality: An Evidence-Based Handbook for Nurses; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2008. [Google Scholar]
- Oeljeklaus, L.; Schmid, H.L.; Kornfeld, Z.; Hornberg, C.; Norra, C.; Zerbe, S.; McCall, T. Therapeutic landscapes and psychiatric care facilities: A qualitative meta-analysis. Int. J. Environ. Res. Public Health 2022, 19, 1490. [Google Scholar] [CrossRef]
- Keys, Y.; Stichler, J.F. Safety and security concerns of nurses working in the intensive care unit. Crit. Care Nurs. Q. 2018, 41, 68–75. [Google Scholar] [CrossRef]
- Oliver, D.; Healey, F.; Haines, T.P. Preventing falls and fall-related injuries in hospitals. Clin. Geriatr. Med. 2010, 26, 645–692. [Google Scholar] [CrossRef]
- Stichler, J.F. Facility design and healthcare-acquired infections: State of the science. J. Nurs. Admin. 2014, 44, 129–132. [Google Scholar] [CrossRef]
- Yousefli, Z.; Nasiri, F.; Moselhi, O. Healthcare facilities maintenance management: A literature review. J. Facil. Manag. 2017, 15, 352–375. [Google Scholar] [CrossRef]
- Mourshed, M.; Zhao, Y. Healthcare providers’ perception of design factors related to physical environments in hospitals. J. Environ. Psychol. 2010, 32, 362–370. [Google Scholar] [CrossRef] [Green Version]
- Choi, K.S.; Cho, W.H.; Lee, S.; Lee, H.; Kim, C. The relationships among quality, value, satisfaction and behavioral intention in health care provider choice: A South Korean study. J. Bus. Res. 2004, 57, 913–921. [Google Scholar] [CrossRef]
- Meesala, A.; Paul, J. Service quality, consumer satisfaction and loyalty in hospitals: Thinking for the future. J. Retail. Consum. Serv. 2018, 40, 261–269. [Google Scholar] [CrossRef]
- Rashid, W.E.W.; Jusoff, K. Service quality in health care setting. Int. J. Health Care Qual. Assur. 2009, 22, 471–482. [Google Scholar] [CrossRef]
- Jabnoun, N.; Chaker, M. Comparing the quality of private and public hospitals. Manag. Serv. Qual. Int. J. 2003, 13, 290–299. [Google Scholar] [CrossRef]
- Pitt, M.; Chotipanich, S.; Issarasak, S.; Mulholland, K.; Panupattanapong, P. An examination of facility management, customer satisfaction and service relationship in the Bangkok healthcare system. Indoor Built. Environ. 2016, 25, 442–458. [Google Scholar] [CrossRef]
- Arneill, A.B.; Devlin, A.S. Perceived quality of care: The influence of the waiting room environment. J. Environ. Psychol. 2002, 22, 345–360. [Google Scholar] [CrossRef]
- Cohen, S. Social relationships and health. Am. Psychol. 2004, 59, 676–684. [Google Scholar] [CrossRef]
- Halding, A.G.; Wahl, A.; Heggdal, K. ‘Belonging’. Patients’ experiences of social relationships during pulmonary rehabilitation. Disabil. Rehabil. 2010, 32, 1272–1280. [Google Scholar] [CrossRef] [Green Version]
- Koivula, M.; Tarkka, M.T.; Tarkka, M.; Laippala, P.; Paunonen-Ilmonen, M. Fear and in-hospital social support for coronary artery bypass grafting patients on the day before surgery. Int. J. Nur. Stud. 2002, 39, 415–427. [Google Scholar] [CrossRef]
- Medland, J.; Howard-Ruben, J.; Whitaker, E. Fostering psychosocial wellness in oncology nurses: Addressing burnout and social support in the workplace. Oncol. Nurs. Forum 2004, 31, 47–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ulrich, R.S. Effects of healthcare environmental design on medical outcomes. In Design and Health: Proceedings of the Second International Conference on Health and Design; Svensk Byggtjanst: Stockholm, Sweden, 2001; pp. 49–59. [Google Scholar]
- Pelletier, D.; Green-Demers, I.; Collerette, P.; Heberer, M. Modeling the communication-satisfaction relationship in hospital patients. SAGE Open Med. 2019, 7, 2050312119847924. [Google Scholar] [CrossRef] [PubMed]
- Browall, M.; Koinberg, I.; Falk, H.; Wijk, H. Patients’ experience of important factors in the healthcare environment in oncology care. Int. J. Qual. Stud. Health Well-Being 2013, 8, 20870. [Google Scholar] [CrossRef]
- Douglas, C.H.; Douglas, M.R. Patient-centered improvements in health-care built environments: Perspectives and design indicators. Health Expect. 2005, 8, 264–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bokolo, A.J. Application of telemedicine and eHealth technology for clinical services in response to COVID-19 pandemic. Health Technol. 2021, 11, 359–366. [Google Scholar] [CrossRef]
- Dalke, H.; Little, J.; Niemann, E.; Camgoz, N.; Steadman, G.; Hill, S.; Stott, L. Colour and lighting in hospital design. Opt. Laser Technol. 2006, 38, 343–365. [Google Scholar] [CrossRef]
- McCunn, L.J.; Safranek, S.; Wilkerson, A.; Davis, R.G. Lighting control in patient rooms: Understanding nurses’ perceptions of hospital lighting using qualitative methods. Health Environ. Res. Des. J. 2021, 14, 204–218. [Google Scholar] [CrossRef]
- Leung, M.; Chan, A.H.S. Control and management of hospital indoor air quality. Med. Sci. Monit. 2006, 12, 23. [Google Scholar]
- Mousavi, E.S.; Kananizadeh, N.; Martinello, R.A.; Sherman, J.D. COVID-19 outbreak and hospital air quality: A systematic review of evidence on air filtration and recirculation. Environ. Sci. Technol. 2020, 55, 4134–4147. [Google Scholar] [CrossRef]
- Lindahl, J.; Thulesius, H.; Rask, M.; Wijk, H.; Edvardsson, D.; Elmqvist, C. Assessing the supportiveness of healthcare environments’ light and color: Development and validation of the light and color questionnaire (LCQ). Health Environ. Res. Des. J. 2021, 14, 130–144. [Google Scholar] [CrossRef]
- Khodakarami, J.; Nasrollahi, N. Thermal comfort in hospitals—A literature review. Renew. Sustain. Energy Rev. 2012, 16, 4071–4077. [Google Scholar] [CrossRef]
- Verheyen, J.; Theys, N.; Allonsius, L.; Descamps, F. Thermal comfort of patients: Objective and subjective measurements in patient rooms of a Belgian healthcare facility. Build. Environ. 2011, 46, 1195–1204. [Google Scholar] [CrossRef]
- Yuan, F.; Yao, R.; Sadrizadeh, S.; Li, B.; Cao, G.; Zhang, S.; Zhou, S.; Liu, H.; Bogdan, A.; Croitoru, C.; et al. Thermal comfort in hospital buildings—A literature review. J. Build. Eng. 2022, 45, 103463. [Google Scholar] [CrossRef]
- de Lima Andrade, E.; da Cunha e Silva, D.C.; de Lima, E.A.; de Oliveira, R.A.; Zannin, P.H.T.; Martins, A.C.G. Environmental noise in hospitals: A systematic review. Environ. Sci. Pollut. Res. 2021, 28, 19629–19642. [Google Scholar] [CrossRef]
- Short, C.A.; Al-Maiyah, S. Design strategy for low-energy ventilation and cooling of hospitals. Build. Res. Inf. 2009, 37, 264–292. [Google Scholar] [CrossRef]
- Yau, Y.H.; Chandrasegaran, D.; Badarudin, A. The ventilation of multiple-bed hospital wards in the tropics: A review. Build. Environ. 2011, 46, 1125–1132. [Google Scholar] [CrossRef] [PubMed]
- Kohn, R.; Harhay, M.O.; Cooney, E.; Small, D.S.; Halpern, S.D. Do windows or natural views affect outcomes or costs among patients in ICUs? Crit. Care Med. 2013, 41, 1645–1655. [Google Scholar] [CrossRef] [Green Version]
- Karanikola, P.; Andrea, V.; Tampakis, S.; Tsolakidou, A. Indoor and outdoor design in healthcare environments: The employees’ views in the general university hospital of Alexandroupolis, Greece. Environments 2020, 7, 61. [Google Scholar] [CrossRef]
- Nanda, U.; Eisen, S.; Zadeh, R.S.; Owen, D. Effect of visual art on patient anxiety and agitation in a mental health facility and implications for the business case. J. Psychiatr. Ment. Health Nurs. 2011, 18, 386–393. [Google Scholar] [CrossRef]
- Ulrich, R.S.; Gilpin, L. Healing arts: Nutrition for the soul. In Putting Patients First: Designing and Practicing Patient-Centered Care; Frampton, S.B., Gilpin, L., Charmel, P.A., Eds.; John Wiley & Sons: San Francisco, CA, USA, 2003; pp. 117–146. [Google Scholar]
- Malone, E.B.; Dellinger, B.A. Furniture Design Features and Healthcare Outcomes; The Center for Health Design: Concord, CA, USA, 2011. [Google Scholar]
- Emmanuel, U.; Osondu, E.D.; Kalu, K.C. Architectural design strategies for infection prevention and control (IPC) in health-care facilities: Towards curbing the spread of Covid-19. J. Environ. Health Sci. Eng. 2020, 18, 1699–1707. [Google Scholar] [CrossRef]
- Lateef, F. Hospital design for better infection control. J. Emerg. Trauma Shock 2009, 2, 175. [Google Scholar] [CrossRef] [PubMed]
- Zimring, C.; Denham, M.E.; Jacob, J.T.; Cowan, D.Z.; Do, E.; Hall, K.; Kamerow, D.; Kasali, A.; Steinberg, J.P. Evidence-based design of healthcare facilities: Opportunities for research and practice in infection prevention. Infect. Control Hosp. Epidemiol. 2013, 34, 514–516. [Google Scholar] [CrossRef] [PubMed]
- Capolongo, S.; Gola, M.; Di Noia, M.; Nickolova, M.; Nachiero, D.; Rebecchi, A.; Settimo, G.; Vittori, G.; Buffoli, M. Social sustainability in healthcare facilities: A rating tool for analysing and improving social aspects in environments of care. Ann. Ist. Super. Sanita 2016, 52, 15–23. [Google Scholar] [PubMed]
- Carthey, J. Reinterpreting the hospital corridor: “Wasted space” or essential for quality multidisciplinary clinical care? Health Environ. Res. Des. J. 2008, 2, 17–29. [Google Scholar] [CrossRef] [PubMed]
- Devlin, A.S. Wayfinding in healthcare facilities: Contributions from environmental psychology. Behav. Sci. 2014, 4, 423–436. [Google Scholar] [CrossRef] [Green Version]
- Pachilova, R.; Sailer, K. Providing care quality by design: A new measure to assess hospital ward layouts. J. Archit. 2020, 25, 186–202. [Google Scholar] [CrossRef]
- Seo, J.Y.; Cho, M.J. Analyzing therapeutic design characteristics in the indoor atrium of the outpatient areas in children’s hospitals overseas. J. Archit. Inst. Korea Plan. Des. 2019, 35, 65–75. [Google Scholar]
- Fornara, F.; Bonaiuto, M.; Bonnes, M. Perceived hospital environment quality indicators: A study of orthopaedic units. J. Environ. Psychol. 2006, 26, 321–334. [Google Scholar] [CrossRef]
- Alalouch, C.; Aspinall, P.; Smith, H. On locational preferences for privacy in hospital wards. Facilities 2009, 27, 88–106. [Google Scholar] [CrossRef]
- Meng, R.; Li, J.; Zhang, Y.; Yu, Y.; Luo, Y.; Liu, X.; Zhao, Y.; Hao, Y.; Hu, Y.; Yu, C. Evaluation of patient and medical staff satisfaction regarding healthcare services in Wuhan Public Hospitals. Int. J. Environ. Res. Public Health 2018, 15, 769. [Google Scholar] [CrossRef] [Green Version]
- Couper, M.P.; Conrad, F.G.; Tourangeau, R. Visual context effects in web surveys. Public Opin. Q. 2007, 71, 623–634. [Google Scholar] [CrossRef] [Green Version]
- Shr, Y.H.J.; Ready, R.; Orland, B.; Echols, S. How do visual representations influence survey responses? Evidence from a choice experiment on landscape attributes of green infrastructure. Ecol. Econ. 2019, 156, 375–386. [Google Scholar] [CrossRef]
- Kim, D.S.; Shepley, M.M. Healthcare architects’ professional autonomy: Interview case studies. Health Environ. Res. Des. J. 2008, 1, 14–26. [Google Scholar] [CrossRef]
- Jeong, S.H.; Lee, B.S.; Choi, Y.G. A study on the construction of cloud BIM-based medical facility design support system. J. Archi. Inst. Korea 2019, 35, 39–46. [Google Scholar]
- Choi, G.S. A study on the characteristics of design process for healthcare architecture. Korea Inst. Healthc. Archit. 2009, 15, 13–22. [Google Scholar]
- Stevens, J.P. Applied Multivariate Statistics for the Social Sciences, 5th ed.; Routledge: New York, NY, USA, 2012; pp. 271–285. [Google Scholar]
- Cerny, B.A.; Kaiser, H.F. A study of a measure of sampling adequacy for factor-analytic correlation matrices. Multivar. Behav. Res. 1977, 12, 43–47. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S.; Ullman, J.B. Using Multivariate Statistics; Pearson: Boston, MA, USA, 2007; pp. 476–527. [Google Scholar]
- Kaiser, H.F. An index of factorial simplicity. Psychometrika 1974, 39, 31–36. [Google Scholar] [CrossRef]
- Reijula, J.; Kouri, J.; Aalto, L.; Miettunen, R.; Reijula, K. Healthcare facility design development in Kuopio University Hospital. Intell. Build. Int. 2017, 9, 137–147. [Google Scholar] [CrossRef]
- Haddad, T.H.; Jaaron, A.A. The applicability of total productive maintenance for healthcare facilities: An implementation methodology. Int. J. Bus. Humanit. Technol. 2012, 2, 148–155. [Google Scholar]
- Gharaveis, A.; Hamilton, D.K.; Pati, D. The impact of environmental design on teamwork and communication in healthcare facilities: A systematic literature review. Health Environ. Res. Des. J. 2018, 11, 119–137. [Google Scholar] [CrossRef] [Green Version]
- Ferri, P.; Muzzalupo, J.; Di Lorenzo, R. Patients’ perception of dignity in an Italian general hospital: A cross-sectional analysis. BMC Health Serv. Res. 2015, 15, 41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hartig, T.; Marcus, C.C. Essay: Healing gardens—Places for nature in health care. Lancet 2006, 368, S36–S37. [Google Scholar] [CrossRef]
- Paraskevopoulou, A.T.; Kamperi, E. Design of hospital healing gardens linked to pre-or post-occupancy research findings. Front. Archit. Res. 2018, 7, 395–414. [Google Scholar] [CrossRef]
- Pruyn, A.; Smidts, A. Effects of waiting on the satisfaction with the service: Beyond objective time measures. Int. J. Res. Mark. 1998, 15, 321–334. [Google Scholar] [CrossRef]
- Sasanfar, S.; Bagherpour, M.; Moatari-Kazerouni, A. Improving emergency departments: Simulation-based optimization of patients waiting time and staff allocation in an Iranian hospital. Int. J. Healthc. Manag. 2021, 14, 1449–1456. [Google Scholar] [CrossRef]
- Iedema, R.; Long, D.; Carroll, K.; Stenglin, M.; Braithwaite, J. Corridor Work: How Liminal Space Becomes a Resource for Handling Complexities of Multidisciplinary Healthcare. In Proceedings of the Apros 11: Asia Pacific Researchers in Organization Studies, Melbourne, Australia, 4–7 December 2005. [Google Scholar]
- Ahmed, J.; Malik, F.; Memon, Z.A.; Arif, T.B.; Ali, A.; Nasim, S.; Ahmad, J.; Khan, M.A. Compliance and knowledge of healthcare workers regarding hand hygiene and use of disinfectants: A study based in Karachi. Cureus 2020, 12, e7036. [Google Scholar] [CrossRef] [Green Version]
- Sax, H.; Uçkay, I.; Richet, H.; Allegranzi, B.; Pittet, D. Determinants of good adherence to hand hygiene among healthcare workers who have extensive exposure to hand hygiene campaigns. Infect. Control Hosp. Epidemiol. 2007, 28, 1267–1274. [Google Scholar] [CrossRef]
- Velle, W. Sex differences in sensory functions. Perspect. Biol. Med. 1987, 30, 490–522. [Google Scholar] [CrossRef]
- Ahrentzen, S.; Anthony, K.H. Sex, stars, and studios: A look at gendered educational practices in architecture. J. Archit. Educ. 1993, 47, 11–29. [Google Scholar]
- Franck, K.A. A feminist approach to architecture: Acknowledging women’s ways of knowing. In Architecture: A Place for Women; Berkeley, E.P., McQuaid, M., Eds.; Smithsonian Institution Press: Washington, DC, USA, 1989; pp. 201–218. [Google Scholar]
- Fottler, M.D.; Ford, R.C.; Roberts, V.; Ford, E.W. Creating a healing environment: The importance of the service setting in the new consumer-oriented healthcare system. J. Healthc. Manag. 2000, 45, 91–106. [Google Scholar]
- Lee, K.S.; Shin, M.G. Goals and assignments of healthcare accreditation program in Korea. J. Korean Med. Assoc. 2012, 55, 7–16. [Google Scholar] [CrossRef] [Green Version]
- McCormick, M.; Shepley, M.M. How can consumers benefit from therapeutic environments? J. Archit. Plann. Res. 2003, 20, 4–15. [Google Scholar]
- Kim, J.A. A study on natural element application method for creating healing environment in hospital’s interior space. Korean Inst. Int. Des. J. 2011, 20, 245–253. [Google Scholar]
- Son, J.H.; Yang, N.W. A study on characteristics of considering healing environmental concept in domestic healthcare architectures schematic design: Focusing on the prizewinner of healthcare architecture design competition since 2000. J. Archi. Inst. Korea 2012, 28, 125–132. [Google Scholar]
- Korea Institute for Healthcare Accreditation: Accreditation Standard. Available online: https://www.koiha.or.kr/web/en/assessment/accStandard.do (accessed on 30 December 2022).
- Architectural Guidelines for the Design of Healthcare Facilities: Focused on General Ward, Isolation Ward, ICU, Newborn Unit, NICU, Dialysis Unit, Surgical Unit, HVAC. Available online: http://www.mohw.go.kr/react/jb/sjb030301vw.jsp?PAR_MENU_ID=03&MENU_ID=032901&CONT_SEQ=349025/ (accessed on 30 December 2022).
- Kim, Y.; Lee, H.; Song, S. Comparative study of hospital architecture design guidelines and frameworks for the patient safety: Focused on the US and UK. Korea Inst. Healthc. Archit. 2021, 27, 27–37. [Google Scholar]
- Lee, H.J.; Ju, Y.O. Changes of ward modules according to the 2017 revision of medical law. J. Korea Inst. Ecol. Archit. Environ. 2017, 17, 55–61. [Google Scholar]
- Kim, Y.W.; Yang, N.W. A study on the architectural planning for improvement of the healing environment in multi-bed room of general hospitals. Korean Inst. Int. Des. J. 2003, 36, 76–83. [Google Scholar]
- Oh, C.O.; Paik, J.K. A case study on user evaluation of patients’ room for user-oriented design-focused on H general hospital in Busan. Korean Inst. Int. Des. J. 2012, 21, 12–22. [Google Scholar]
- Mallak, L.A.; Lyth, D.M.; Olson, S.D.; Ulshafer, S.M.; Sardone, F.J. Culture, the built environment and healthcare organizational performance. Manag. Serv. Qual. 2003, 13, 27–38. [Google Scholar] [CrossRef] [Green Version]
- Chan, A.P.; Chan, E.H.; Chan, A.P. Managing health care projects in Hong Kong: A case study of the North District hospital. Int. J. Const. Manag. 2003, 3, 1–13. [Google Scholar] [CrossRef]
- Chan, A.P.; Chan, A.P.; Chan, D.W. An empirical survey of the success criteria for running healthcare projects. Archit. Sci. Rev. 2005, 48, 61–68. [Google Scholar] [CrossRef]
- Ha, J.Y.; Choi, E.Y. Health perception, health concern, and health promotion behavior of the elders. J. Korean Gerontol. Nurs. 2013, 15, 277–285. [Google Scholar]
- Park, S.; Lee, Y.H. Effects of perceived health status, health attitude, and health concern on health promoting behavior in adults. J. Korea Content Assoc. 2016, 16, 192–202. [Google Scholar] [CrossRef]

| Variables | Citation(s) |
|---|---|
| Illumination | [55,100,101] |
| Air quality | [42,102,103] |
| Natural daylight | [34,100,101,104] |
| Thermal comfort | [105,106,107] |
| Noise | [38,39,108] |
| Ventilation | [107,109,110] |
| View | [65,66,111] |
| Plants and gardens | [9,58,62,63,64] |
| Rest and recreational space | [98,112] |
| Color | [62,100,104] |
| Art image | [113,114] |
| Furniture | [115] |
| Maintenance | [83,84] |
| Safety | [57,76] |
| Hygiene | [82,116,117,118] |
| Spatial access | [22,119,120] |
| Wayfinding | [23,121] |
| Openness and visibility | [25,122,123] |
| Location and orientation | [8,124] |
| Exterior appearance | [8,124] |
| Privacy | [28,29,125] |
| Family service and convenience space | [21,98] |
| Communication and information | [96,97,126] |
| Socio-cultural support | [93,95,98] |
| Medical and administrative staff relationship | [8,124,126] |
| Variable | n | % | |
|---|---|---|---|
| Sex | Male | 131 | 72.0 |
| Female | 51 | 28.0 | |
| Age (years) | 20s | 35 | 19.2 |
| 30s | 44 | 24.2 | |
| 40s | 74 | 40.7 | |
| 50s or older | 29 | 15.9 | |
| Education | Bachelor | 87 | 47.8 |
| Graduate | 79 | 43.4 | |
| Doctorial | 16 | 8.8 | |
| Experience with hospital design (years) | <1 | 95 | 52.2 |
| 1–5 | 34 | 18.7 | |
| 6–10 | 25 | 13.7 | |
| >10 | 28 | 15.4 | |
| Architect licensure ship | Yes | 62 | 34.1 |
| No | 120 | 65.9 | |
| Field of specialty | Healthcare and welfare | 69 | 37.9 |
| Commercial and cultural | 41 | 22.5 | |
| Office/workspace | 13 | 7.1 | |
| Housing and urban planning | 39 | 21.4 | |
| Educational, etc. | 20 | 11.0 | |
| Total | 182 | 100.0 | |
| Factor and Items | Factor Loading | Eigenvalue | % Variance | Cronbach’s α |
|---|---|---|---|---|
| Factor 1: Management | 2.700 | 10.801 | 0.761 | |
| Hygiene | 0.732 | |||
| Safety | 0.708 | |||
| Maintenance | 0.704 | |||
| Factor 2: Interior design | 2.628 | 10.513 | 0.776 | |
| Color composition | 0.814 | |||
| Coordinated art and image | 0.765 | |||
| Furniture layout | 0.641 | |||
| Factor 3: Spatial quality | 2.571 | 10.285 | 0.765 | |
| Openness and visibility | 0.745 | |||
| Location and orientation | 0.657 | |||
| Wayfinding | 0.653 | |||
| Accessibility | 0.587 | |||
| Spatial privacy | 0.476 | |||
| Exterior appearance | 0.465 | |||
| Factor 4: Service | 2.285 | 9.141 | 0.754 | |
| Medical staff’s service | 0.832 | |||
| Administration staff’s service | 0.825 | |||
| Family service facility | 0.508 | |||
| Factor 5: Nature and rest | 2.085 | 8.339 | 0.712 | |
| Outdoor view | 0.767 | |||
| Natural daylight | 0.674 | |||
| Green space | 0.609 | |||
| Rest and recreational space | 0.572 | |||
| Factor 6: Ambient indoor comfort | 2.046 | 8.183 | 0.679 | |
| Illumination | 0.627 | |||
| Thermal comfort | 0.612 | |||
| Air quality | 0.588 | |||
| Indoor noise | 0.508 | |||
| Factor 7: Social program and space | 1.914 | 7.655 | 0.663 | |
| Health information program and space | 0.789 | |||
| Socio-cultural program and space | 0.693 | |||
| Total variance explained: 64.917% | ||||
| Bartlett’s test: chi square = 1783.088, df = 300 (p < 0.001), Kaiser–Meyer–Olkin = 0.835 | ||||
| Factors and Items | Mean | Standard Deviation |
|---|---|---|
| Factor 1: Management | 4.52 | 0.573 |
| Hygiene | 4.65 | 0.620 |
| Safety | 4.51 | 0.763 |
| Maintenance | 4.42 | 0.698 |
| Factor 2: Interior design | 3.59 | 0.699 |
| Color composition | 3.72 | 0.850 |
| Coordinated art and image | 3.43 | 0.900 |
| Furniture layout | 3.63 | 0.767 |
| Factor 3: Spatial quality | 3.77 | 0.548 |
| Openness and visibility | 3.87 | 0.746 |
| Location and orientation | 3.82 | 0.829 |
| Wayfinding | 3.79 | 0.782 |
| Accessibility | 3.80 | 0.852 |
| Spatial privacy | 3.96 | 0.761 |
| Exterior appearance | 3.37 | 0.868 |
| Factor 4: Service | 4.15 | 0.606 |
| Medical staff’s service | 4.42 | 0.691 |
| Administration staff’s service | 4.18 | 0.762 |
| Family service facility | 3.84 | 0.767 |
| Factor 5: Nature and rest | 4.04 | 0.556 |
| Outdoor view | 3.82 | 0.797 |
| Natural daylight | 4.54 | 0.618 |
| Green space | 3.58 | 0.855 |
| Rest and recreational space | 4.21 | 0.746 |
| Factor 6: Ambient indoor comfort | 4.26 | 0.501 |
| Illumination | 4.18 | 0.677 |
| Thermal comfort | 4.37 | 0.667 |
| Air quality | 4.66 | 0.597 |
| Indoor noise | 3.84 | 0.844 |
| Factor 7: Social program and space | 3.39 | 0.738 |
| Health information program and space | 3.23 | 0.855 |
| Socio-cultural program and space | 3.54 | 0.851 |
| Variable | f(n) | Mean | Standard Deviation | t/F | p | |
|---|---|---|---|---|---|---|
| Sex | Male | 131 | 4.45 | 0.612 | 3.228 | 0.002 |
| Female | 51 | 4.71 | 0.409 | |||
| Variable | f(n) | Mean | Standard Deviation | t/F | p | |
|---|---|---|---|---|---|---|
| Age (years) | 20s | 35 | 3.37 a | 0.753 | 2.683 | 0.048 |
| 30s | 44 | 3.55 ab | 0.705 | |||
| 40s | 74 | 3.63 ab | 0.648 | |||
| 50s or older | 29 | 3.85 b | 0.688 | |||
| Variable | f(n) | Mean | Standard Deviation | t/F | p | |
|---|---|---|---|---|---|---|
| Sex | Male | 131 | 3.71 | 0.590 | 2.608 | 0.010 |
| Female | 51 | 3.91 | 0.391 | |||
| Variables | n | % | |
|---|---|---|---|
| Sex | Female | 8 | 53.3 |
| Male | 7 | 46.7 | |
| Age (years) | 30s | 10 | 66.7 |
| 40s | 3 | 20.0 | |
| 50s or older | 2 | 13.3 | |
| Education | Bachelor | 7 | 46.7 |
| Graduate | 8 | 53.3 | |
| Doctorial | 0 | 0.0 | |
| Experience in hospital design project management (years) | ≤5 | 2 | 13.3 |
| 6–10 | 4 | 26.7 | |
| 11–15 | 4 | 26.7 | |
| >15 | 5 | 33.3 | |
| Architectural licensure ship | Yes | 8 | 53.3 |
| No | 7 | 46.7 | |
| Size of firm (persons) | ≤100 | 4 | 26.7 |
| 101–300 | 1 | 6.7 | |
| 301–600 | 3 | 20.0 | |
| >600 | 7 | 46.7 | |
| Total | 15 | 100.0 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, M. Evaluating Therapeutic Healthcare Environmental Criteria: Architectural Designers’ Perspectives. Int. J. Environ. Res. Public Health 2023, 20, 1540. https://doi.org/10.3390/ijerph20021540
Cho M. Evaluating Therapeutic Healthcare Environmental Criteria: Architectural Designers’ Perspectives. International Journal of Environmental Research and Public Health. 2023; 20(2):1540. https://doi.org/10.3390/ijerph20021540
Chicago/Turabian StyleCho, Minjung. 2023. "Evaluating Therapeutic Healthcare Environmental Criteria: Architectural Designers’ Perspectives" International Journal of Environmental Research and Public Health 20, no. 2: 1540. https://doi.org/10.3390/ijerph20021540
APA StyleCho, M. (2023). Evaluating Therapeutic Healthcare Environmental Criteria: Architectural Designers’ Perspectives. International Journal of Environmental Research and Public Health, 20(2), 1540. https://doi.org/10.3390/ijerph20021540






