Protocols and Features of Goal-Setting-Based Intervention for Frail Older Adults in Community Exercise Facilities
Abstract
:1. Introduction
2. Materials and Methods
2.1. Overall Study Project
2.2. Study Population
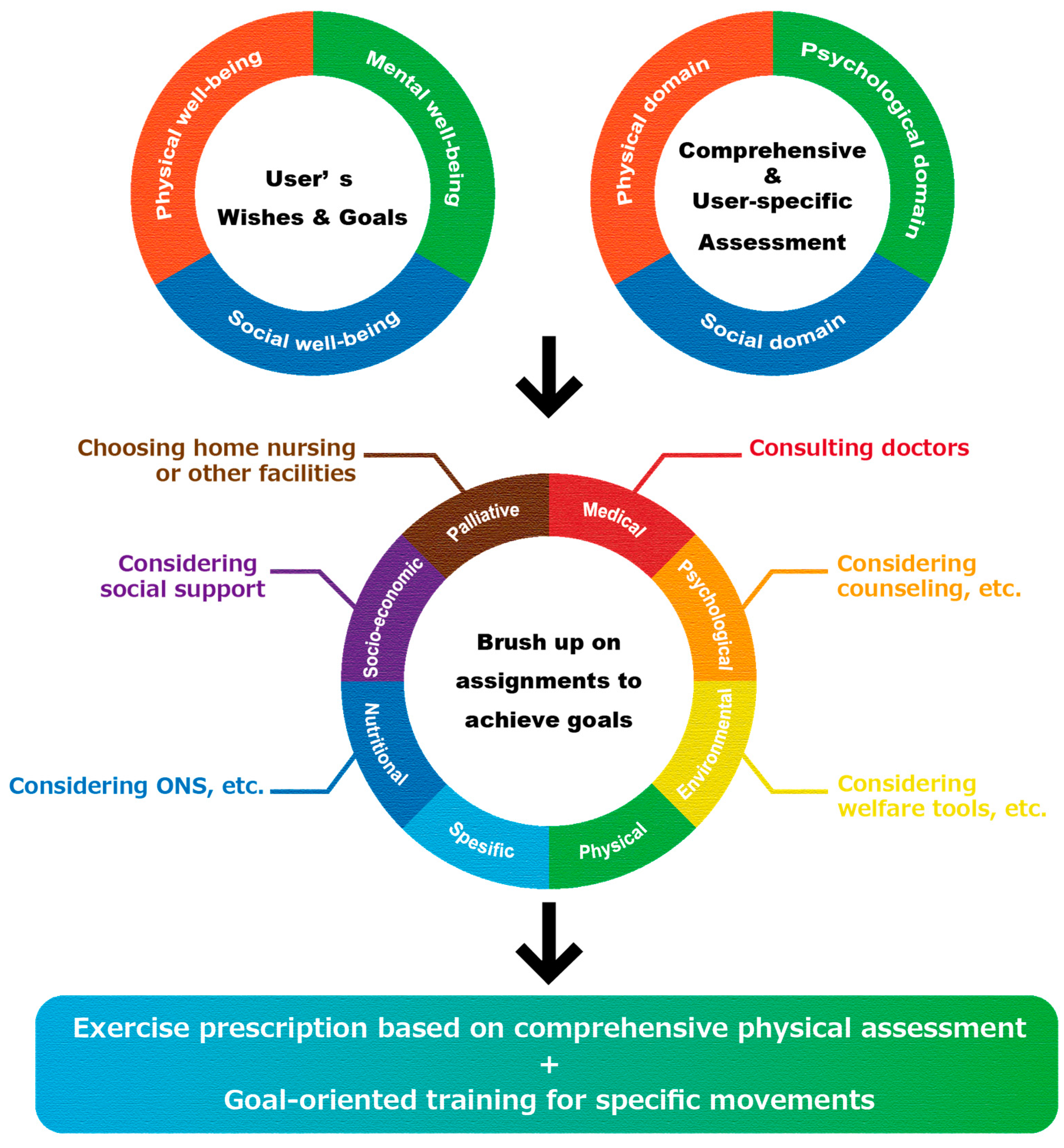
2.3. Rehabilitation Protocol and Setting Goals for Rehabilitation
2.4. Assessment of Each Frailty Domain and International Classification of Functioning, Disability and Health (ICF) Classification
2.5. Statistical Analysis
3. Results
3.1. Subjects’ Characteristics
3.2. Prevalence of Each Frailty Domain and Overlapping Frailties
3.3. Setting Goals According to the Subjects’ Wishes
3.4. Relation between Goal Setting and Frailty Domain
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ikegami, N. Public long-term care insurance in Japan. JAMA 1997, 278, 1310–1314. [Google Scholar] [CrossRef]
- Yamada, M.; Arai, H. Long-Term Care System in Japan. Ann. Geriatr. Med. Res. 2020, 24, 174–180. [Google Scholar] [CrossRef]
- Yamada, M.; Arai, H. Predictive Value of Frailty Scores for Healthy Life Expectancy in Community-Dwelling Older Japanese Adults. J. Am. Med. Dir. Assoc. 2015, 16, 1002.e7–1002.e11. [Google Scholar] [CrossRef]
- Lee, Y.; Kim, E.; Yun, J.; Chuck, K.W. The influence of multiple frailty profiles on institutionalization and all-cause mortality in community-living older adults. J. Cachexia Sarcopenia Muscle 2022, 13, 2322–2330. [Google Scholar] [CrossRef] [PubMed]
- Arias-Casais, N.; Amuthavalli Thiyagarajan, J.; Rodrigues Perracini, M.; Park, E.; Van den Block, L.; Sumi, Y.; Sadana, R.; Banerjee, A.; Han, Z.A. What long-term care interventions have been published between 2010 and 2020? Results of a WHO scoping review identifying long-term care interventions for older people around the world. BMJ Open 2022, 12, e054492. [Google Scholar] [CrossRef]
- Bernabei, R.; Landi, F.; Calvani, R.; Cesari, M.; Del Signore, S.; Anker, S.D.; Bejuit, R.; Bordes, P.; Cherubini, A.; Cruz-Jentoft, A.J.; et al. Multicomponent intervention to prevent mobility disability in frail older adults: Randomised controlled trial (SPRINTT project). BMJ 2022, 377, e068788. [Google Scholar] [CrossRef] [PubMed]
- Levack, W.M.; Weatherall, M.; Hay-Smith, J.C.; Dean, S.G.; McPherson, K.; Siegert, R.J. Goal setting and strategies to en-hance goal pursuit in adult rehabilitation: Summary of a Cochrane systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 2016, 52, 400–416. [Google Scholar]
- Boeykens, D.; Boeckxstaens, P.; De Sutter, A.; Lahousse, L.; Pype, P.; De Vriendt, P.; Van de Velde, D. Goal-oriented care for patients with chronic conditions or multimorbidity in primary care: A scoping review and concept analysis. PLoS ONE 2022, 17, e0262843. [Google Scholar] [CrossRef]
- Yamashita, M.; Obata, H.; Kamiya, K.; Matsunaga, A.; Hotta, K.; Izumi, T. Overlapping states of AWGS muscle dysfunc-tion and inverse feasibility of ADL recovery by rehabilitation in older inpatients. Sci. Rep. 2022, 12, 22283. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Stubbs, B.; Volpato, S.; Zuliani, G.; Maggi, S.; Cesari, M.; Lipnicki, D.M.; Smith, L.; Schofield, P.; Firth, J.; et al. Association Between Gait Speed With Mortality, Cardiovascular Disease and Cancer: A Systematic Review and Me-ta-analysis of Prospective Cohort Studies. J. Am. Med. Dir. Assoc. 2018, 19, 981–988.e987. [Google Scholar] [CrossRef]
- Rijk, J.M.; Roos, P.R.; Deckx, L.; van den Akker, M.; Buntinx, F. Prognostic value of handgrip strength in people aged 60 years and older: A systematic review and meta-analysis. Geriatr. Gerontol. Int. 2016, 16, 5–20. [Google Scholar] [CrossRef] [PubMed]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A short physical performance battery assessing lower extremity function: Association with self-reported disability and predic-tion of mortality and nursing home admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef] [PubMed]
- Kamiya, K.; Masuda, T.; Tanaka, S.; Hamazaki, N.; Matsue, Y.; Mezzani, A.; Matsuzawa, R.; Nozaki, K.; Maekawa, E.; Noda, C.; et al. Quadriceps Strength as a Predictor of Mortality in Coronary Artery Disease. Am. J. Med. 2015, 128, 1212–1219. [Google Scholar] [CrossRef] [Green Version]
- Kamiya, K.; Masuda, T.; Matsue, Y.; Hamazaki, N.; Matsuzawa, R.; Tanaka, S.; Nozaki, K.; Maekawa, E.; Noda, C.; Yamaoka-Tojo, M.; et al. Prognostic Usefulness of Arm and Calf Circumference in Patients ≥65 Years of Age With Car-diovascular Disease. Am. J. Cardiol. 2017, 119, 186–191. [Google Scholar] [CrossRef]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e302. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, S.; Shiroiwa, T.; Igarashi, A.; Noto, S.; Fukuda, T.; Saito, S.; Shimozuma, K. Developing a Japanese version of the EQ-5D-5L value set. J. Natl. Inst. Public Health 2015, 64, 47–55. [Google Scholar]
- Law, M.; Baptiste, S.; McColl, M.; Opzoomer, A.; Polatajko, H.; Pollock, N. The Canadian occupational performance measure: An outcome measure for occupational therapy. Can. J. Occup. Ther. 1990, 57, 82–87. [Google Scholar] [CrossRef]
- Komatsu, H.; Yagasaki, K.; Saito, Y.; Oguma, Y. Regular group exercise contributes to balanced health in older adults in Japan: A qualitative study. BMC Geriatr. 2017, 17, 190. [Google Scholar] [CrossRef] [Green Version]
- Bovend’Eerdt, T.J.; Botell, R.E.; Wade, D.T. Writing SMART rehabilitation goals and achieving goal attainment scaling: A practical guide. Clin. Rehabil. 2009, 23, 352–361. [Google Scholar] [CrossRef]
- Tomori, K.; Uezu, S.; Kinjo, S.; Ogahara, K.; Nagatani, R.; Higashi, T. Utilization of the iPad application: Aid for Deci-sion-making in Occupation Choice. Occup. Ther. Int. 2012, 19, 88–97. [Google Scholar] [CrossRef]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef] [PubMed]
- Izquierdo, M.; Merchant, R.A.; Morley, J.E.; Anker, S.D.; Aprahamian, I.; Arai, H.; Aubertin-Leheudre, M.; Bernabei, R.; Cadore, E.L.; Cesari, M.; et al. International Exercise Recommendations in Older Adults (ICFSR): Expert Consensus Guidelines. J. Nutr. Health Aging 2021, 25, 824–853. [Google Scholar] [CrossRef]
- Makita, S.; Yasu, T.; Akashi, Y.J.; Adachi, H.; Izawa, H.; Ishihara, S.; Iso, Y.; Ohuchi, H.; Omiya, K.; Ohya, Y.; et al. JCS/JACR 2021 Guideline on Rehabilitation in Patients With Cardiovascular Disease. Circ. J. 2022, 87, 155–235. [Google Scholar] [CrossRef]
- Miyakoshi, K. Patient Safety in Rehabilitation Medicine. J. Rehabil. Med. 2021, 58, 242–246. [Google Scholar] [CrossRef]
- Violan, C.; Foguet-Boreu, Q.; Flores-Mateo, G.; Salisbury, C.; Blom, J.; Freitag, M.; Glynn, L.; Muth, C.; Valderas, J.M. Prevalence, determinants and patterns of multimorbidity in primary care: A systematic review of observational studies. PLoS ONE 2014, 9, e102149. [Google Scholar] [CrossRef]
- Winstein, C.J.; Stein, J.; Arena, R.; Bates, B.; Cherney, L.R.; Cramer, S.C.; Deruyter, F.; Eng, J.J.; Fisher, B.; Harvey, R.L.; et al. Guidelines for Adult Stroke Rehabilitation and Recovery: A Guideline for Healthcare Professionals From the Amer-ican Heart Association/American Stroke Association. Stroke 2016, 47, e98–e169. [Google Scholar] [CrossRef]
- Timmermans, A.A.; Spooren, A.I.; Kingma, H.; Seelen, H.A. Influence of task-oriented training content on skilled arm-hand performance in stroke: A systematic review. Neurorehabil. Neural Repair 2010, 24, 858–870. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charles, C.; Gafni, A.; Whelan, T. Shared decision-making in the medical encounter: What does it mean? (or it takes at least two to tango). Soc. Sci. Med. 1997, 44, 681–692. [Google Scholar] [CrossRef] [PubMed]
- Rose, A.; Rosewilliam, S.; Soundy, A. Shared decision making within goal setting in rehabilitation settings: A systematic review. Patient Educ. Couns. 2017, 100, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Matsue, Y.; Kamiya, K.; Saito, H.; Saito, K.; Ogasahara, Y.; Maekawa, E.; Konishi, M.; Kitai, T.; Iwata, K.; Jujo, K.; et al. Prevalence and prognostic impact of the coexistence of multiple frailty domains in elderly patients with heart failure: The FRAGILE-HF cohort study. Eur. J. Heart Fail. 2020, 22, 2112–2119. [Google Scholar] [CrossRef]
- Satake, S.; Arai, H. The revised Japanese version of the Cardiovascular Health Study criteria (revised J-CHS criteria). Geriatr. Gerontol. Int. 2020, 20, 992–993. [Google Scholar] [CrossRef] [PubMed]
- Makizako, H.; Shimada, H.; Tsutsumimoto, K.; Lee, S.; Doi, T.; Nakakubo, S.; Hotta, R.; Suzuki, T. Social Frailty in Community-Dwelling Older Adults as a Risk Factor for Disability. J. Am. Med. Dir. Assoc. 2015, 16, 1003.e7–1003.e11. [Google Scholar] [CrossRef] [PubMed]
- Borson, S.; Scanlan, J.; Brush, M.; Vitaliano, P.; Dokmak, A. The mini-cog: A cognitive ’vital signs’ measure for dementia screening in multi-lingual elderly. Int. J. Geriatr. Psychiatry 2000, 15, 1021–1027. [Google Scholar] [CrossRef] [PubMed]
- Bagraith, K.S.; Hayes, J.; Strong, J. Mapping patient goals to the International Classification of Functioning, Disability and Health (ICF): Examining the content validity of the low back pain core sets. J. Rehabil. Med. 2013, 45, 481–487. [Google Scholar] [CrossRef] [Green Version]
- Matérne, M.; Frank, A.; Arvidsson, P. The utility of goal attainment scaling in evaluating a structured water dance in-tervention for adults with profound intellectual and multiple disabilities. Heliyon 2021, 7, e07902. [Google Scholar] [CrossRef]
- Cieza, A.; Geyh, S.; Chatterji, S.; Kostanjsek, N.; Ustün, B.; Stucki, G. ICF linking rules: An update based on lessons learned. J. Rehabil. Med 2005, 37, 212–218. [Google Scholar] [CrossRef] [Green Version]
- Maruta, M.; Makizako, H.; Ikeda, Y.; Han, G.; Shimokihara, S.; Miyata, H.; Nakamura, A.; Tokuda, K.; Kubozono, T.; Ohishi, M.; et al. Characteristics of meaningful activities in community-dwelling Japanese older adults with pre-frailty and frailty. Arch. Gerontol. Geriatr. 2022, 99, 104616. [Google Scholar] [CrossRef]
- Kojima, G.; Iliffe, S.; Taniguchi, Y.; Shimada, H.; Rakugi, H.; Walters, K. Prevalence of frailty in Japan: A systematic re-view and meta-analysis. J. Epidemiol. 2017, 27, 347–353. [Google Scholar] [CrossRef] [Green Version]
- Murayama, H.; Kobayashi, E.; Okamoto, S.; Fukaya, T.; Ishizaki, T.; Liang, J.; Shinkai, S. National prevalence of frailty in the older Japanese population: Findings from a nationally representative survey. Arch. Gerontol. Geriatr. 2020, 91, 104220. [Google Scholar] [CrossRef]
- Yuri, Y.; Takabatake, S.; Nishikawa, T.; Oka, M.; Fujiwara, T. The effects of a life goal-setting technique in a preventive care program for frail community-dwelling older people: A cluster nonrandomized controlled trial. BMC Geriatr. 2016, 16, 101. [Google Scholar] [CrossRef] [Green Version]
- Wong, M.Y.C.; Ou, K.L.; Chung, P.K. Healthy Lifestyle Behavior, Goal Setting, and Personality among Older Adults: A Synthesis of Literature Reviews and Interviews. Geriatrics 2022, 7, 131. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.H.; Chang, W.P.; Chen, S.R.; Cheng, W.J.; Chou, K.R.; Pien, L.C. Health Literacy and Exercise to Treat Frailty in Community-Dwelling Older Adults: A National Survey Study. Int. J. Environ. Res. Public Health 2022, 19, 8711. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.Y.; Shin, H.; Kim, S.; Lee, H.Y.; Kim, Y.S. Limited health literacy increases the risk of frailty among communi-ty-dwelling older adults: Longitudinal findings from the Korean Frailty and Aging Cohort Study. Geriatr. Gerontol. Int. 2022, 22, 325–331. [Google Scholar] [CrossRef] [PubMed]
- de Waal, M.W.M.; Haaksma, M.L.; Doornebosch, A.J.; Meijs, R.; Achterberg, W.P. Systematic review of measurement properties of the Canadian Occupational Performance Measure in geriatric rehabilitation. Eur. Geriatr. Med. 2022, 13, 1281–1298. [Google Scholar] [CrossRef] [PubMed]


| (n = 201) | All Subjects | Missing Data |
|---|---|---|
| Age, year | 79 (74–82) | - |
| Male, n (%) | 88 (43.8) | - |
| BMI, kg/m2 | 22.6 (22.1–24.6) | 5 (2.5) |
| Frequency of use, n (%) | - | |
| - 1/week | 155 (77.1) | |
| - 2/week | 43 (21.4) | |
| - 3 or more/week | 3 (1.5) | |
| Disease, n (%) | - | |
| - Orthopedic disease | 124 (61.7) | |
| - Cerebrovascular disease | 54 (26.9) | |
| - Cardiovascular disease | 37 (18.4) | |
| - Cancer | 28 (13.9) | |
| - Intractable disease 1 | 12 (6.0) | |
| Frailty domain, n (%) | ||
| - Physical frailty | 71 (40.6) | 26 (12.9) |
| - Cognitive dysfunction | 41 (24.7) | 35 (17.4) |
| - Social frailty | 122 (75.8) | 40 (19.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamashita, M.; Mashizume, Y.; Yama, K.; Sasaki, S.; Uehara, D.; Kamiya, K. Protocols and Features of Goal-Setting-Based Intervention for Frail Older Adults in Community Exercise Facilities. Int. J. Environ. Res. Public Health 2023, 20, 1615. https://doi.org/10.3390/ijerph20021615
Yamashita M, Mashizume Y, Yama K, Sasaki S, Uehara D, Kamiya K. Protocols and Features of Goal-Setting-Based Intervention for Frail Older Adults in Community Exercise Facilities. International Journal of Environmental Research and Public Health. 2023; 20(2):1615. https://doi.org/10.3390/ijerph20021615
Chicago/Turabian StyleYamashita, Masashi, Yuki Mashizume, Kento Yama, Shun Sasaki, Daiki Uehara, and Kentaro Kamiya. 2023. "Protocols and Features of Goal-Setting-Based Intervention for Frail Older Adults in Community Exercise Facilities" International Journal of Environmental Research and Public Health 20, no. 2: 1615. https://doi.org/10.3390/ijerph20021615






