Promoting Healthy Behaviors in Older Adults to Optimize Health-Promoting Lifestyle: An Intervention Study
Abstract
:1. Introduction
2. Materials and Methods
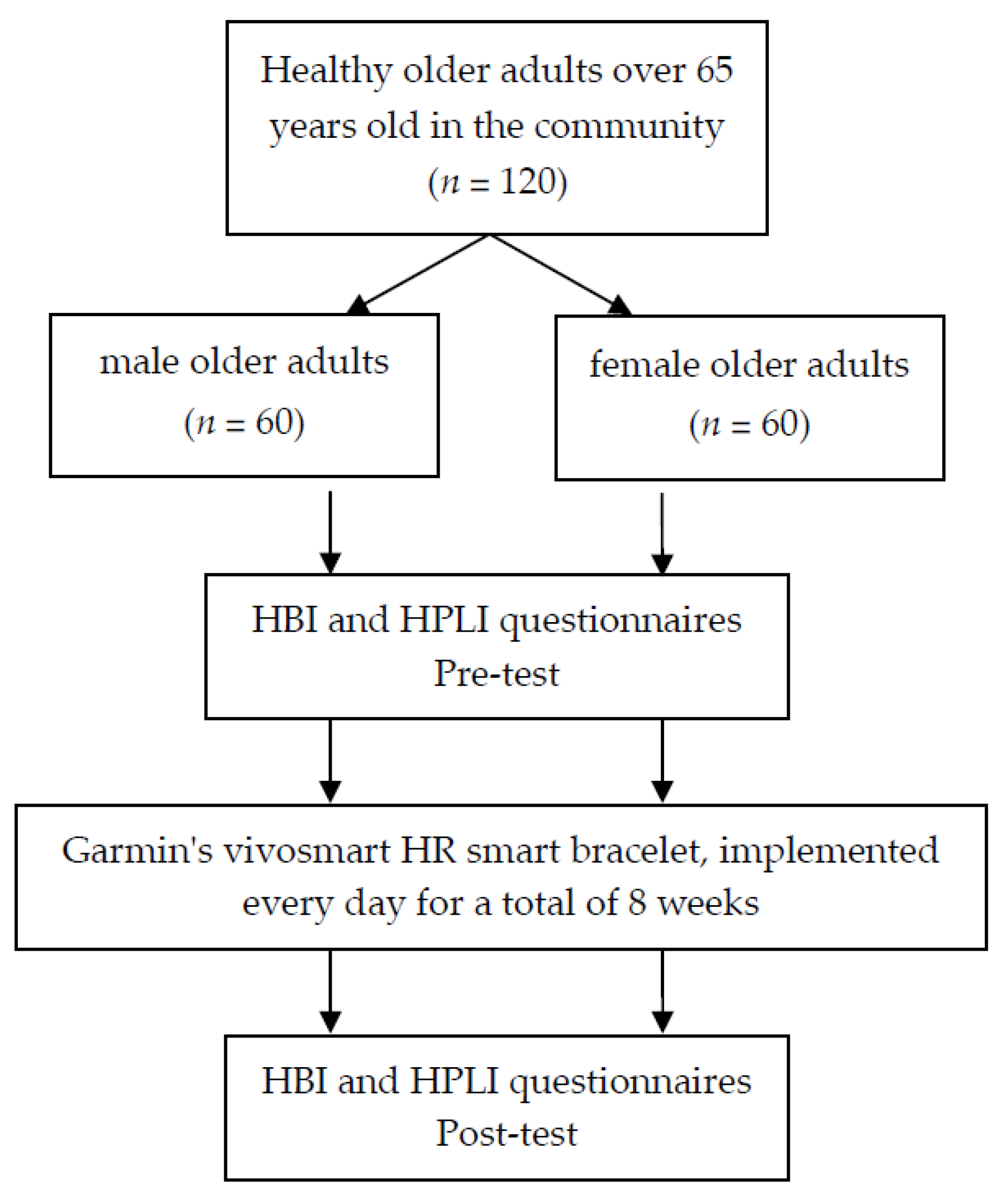
2.1. Research Participants
2.2. Research Materials
2.3. Testing Method
2.3.1. Garmin Built-in Data
2.3.2. Health Behavior Inventory
2.3.3. Health-Promoting Lifestyle Inventory
2.4. Control Variables
2.5. Statistical Analysis
3. Results
3.1. Participant Background Variable Analysis
3.2. Analysis of Daily Walking, Walking Distance, and Calorie Consumption
3.3. Analysis of Participants’ Pre- and Post-Test HBI
3.4. Analysis of Participants’ Pre- and Post-Test HPLI
3.5. Pearson Product-Moment Correlation Analysis of the Post-Test Results of Various Factors between HBI and HPLI
3.6. Explanatory Power of Various Factors of Health Behavior on Health-Promoting Lifestyle
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Typhoid Vaccines: WHO Position Paper, March 2018—Recommendations. Vaccine 2019, 37, 214–216. [Google Scholar] [CrossRef] [PubMed]
- WHO. Health Promoting Schools. 2022. Available online: https://www.who.int/health-topics/health-promoting-schools#tab=tab_1 (accessed on 5 July 2022).
- Amuthavalli Thiyagarajan, J.; Mikton, C.; Harwood, R.H.; Gichu, M.; Gaigbe-Togbe, V.; Jhamba, T.; Pokorna, D.; Stoevska, V.; Hada, R.; Steffan, G.S.; et al. The UN Decade of healthy ageing: Strengthening measurement for monitoring health and wellbeing of older people. Age Ageing 2022, 51, afac147. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Health and Aging. Department of Health and Human Services. National Institute on Aging. National Institutes of Health. 2011. Available online: https://www.nia.nih.gov/sites/default/files/2017-06/global_health_aging.pdf (accessed on 5 July 2022).
- Gretebeck, K.A.; Sabatini, L.M.; Black, D.R.; Gretebeck, R.J. Physical Activity, Functional Ability, and Obesity in Older Adults: A Gender Difference. J. Gerontol. Nurs. 2017, 43, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Ashe, M.C.; Miller, W.C.; Eng, J.J.; Noreau, L. Older adults, chronic disease and leisure-time physical activity. Gerontology 2009, 55, 64–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical activity in older age: Perspectives for healthy ageing and frailty. Biogerontology 2016, 17, 567–580. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cunningham, C.; O’Sullivan, R.; Caserotti, P.; Tully, M.A. Consequences of physical inactivity in older adults: A systematic review of reviews and meta-analyses. Scand. J. Med. Sci. Sports 2020, 30, 816–827. [Google Scholar] [CrossRef]
- Mehri, A.; Solhi, M.; Garmaroudi, G.; Nadrian, H.; Sighaldeh, S.S. Health Promoting Lifestyle and its Determinants Among University Students in Sabzevar, Iran. Int. J. Prev. Med. 2016, 7, 65. [Google Scholar] [CrossRef]
- Hong, K.L.; Glover, B.M. The impact of lifestyle intervention on atrial fibrillation. Curr. Opin. Cardiol. 2018, 33, 14–19. [Google Scholar] [CrossRef]
- Li, Y.; Pan, A.; Wang, D.D.; Liu, X.; Dhana, K.; Franco, O.H.; Kaptoge, S.; Di Angelantonio, E.; Stampfer, M.; Willett, W.C.; et al. Impact of Healthy Lifestyle Factors on Life Expectancies in the US Population. Circulation 2018, 138, 345–355. [Google Scholar] [CrossRef]
- Haugan, G.; Eriksson, M. An Introduction to the Health Promotion Perspective in the Health Care Services. In Health Promotion in Health Care—Vital Theories and Research; Haugan, G., Eriksson, M., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 3–14. [Google Scholar]
- Golinowska, S.; Groot, W.; Baji, P.; Pavlova, M. Health promotion targeting older people. BMC Health Serv. Res. 2016, 16 (Suppl. 5), 345. [Google Scholar] [CrossRef]
- West, R. Tobacco smoking: Health impact, prevalence, correlates and interventions. Psychol. Health 2017, 32, 1018–1036. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, S.C.; Luo, Y.F.; Chiang, C.H. The Associations Among Individual Factors, eHealth Literacy, and Health-Promoting Lifestyles Among College Students. J. Med. Internet Res. 2017, 19, e15. [Google Scholar] [CrossRef] [Green Version]
- Zheng, Z.; Chen, H. Age sequences of the elderly’ social network and its efficacies on well-being: An urban-rural comparison in China. BMC Geriatr. 2020, 20, 372. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, R.; Baixinho, C.L.; Ferreira, Ó.R.; Nunes, A.C.; Mestre, T.; Sousa, L. Health Promotion and Disease Prevention in the Elderly: The Perspective of Nursing Students. J. Pers. Med. 2022, 12, 306. [Google Scholar] [CrossRef] [PubMed]
- Gast, J.; Peak, T.; Hunt, A. Latino Health Behavior: An Exploratory Analysis of Health Risk and Health Protective Factors in a Community Sample. Am. J. Lifestyle Med. 2020, 14, 97–106. [Google Scholar] [CrossRef]
- Tabrizi, J.S.; Behghadami, M.A.; Saadati, M.; Söderhamn, U. Self-care Ability of Older People Living in Urban Areas of Northwestern Iran. Iran J. Public Health 2018, 47, 1899–1905. [Google Scholar]
- Rondón García, L.M.; Ramírez Navarrro, J.M. The Impact of Quality of Life on the Health of Older People from a Multidimensional Perspective. J. Aging Res. 2018, 2018, 4086294. [Google Scholar] [CrossRef] [Green Version]
- Conner, M.; Norman, P. Health behaviour: Current issues and challenges. Psychol. Health 2017, 32, 895–906. [Google Scholar] [CrossRef] [Green Version]
- Harooni, J.; Hassanzadeh, A.; Mostafavi, F. Influencing factors on health promoting behavior among the elderly living in the community. J. Educ. Health Promot. 2014, 3, 40. [Google Scholar] [CrossRef]
- Levant, R.; Wimer, D.; Williams, C. An Evaluation of the Health Behavior Inventory20 (HBI-20) and Its Relationships to Masculinity and Attitudes Towards Seeking Psychological Help Among College Men. Psychol. Men Masc.—Psychol Men Masc. 2011, 12, 26–41. [Google Scholar] [CrossRef]
- Arai, H.; Ouchi, Y.; Yokode, M.; Ito, H.; Uematsu, H.; Eto, F.; Oshima, S.; Ota, K.; Saito, Y.; Sasaki, H.; et al. Toward the realization of a better aged society: Messages from gerontology and geriatrics. Geriatr. Gerontol. Int. 2012, 12, 16–22. [Google Scholar] [CrossRef]
- Rababa, M.; Al Ali, N.; Alshaman, A. Health Promoting Behaviors, Health Needs and Associated Factors among Older Adults in Jordan: A Cross-Sectional Study. Int. J. Community Based Nurs. Midwifery 2021, 9, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Glebova, E.; Desbordes, M. Chapter 5: Technology Innovations in Sports: Typology, Nature, Courses and Impact. In Innovation and Entrepreneurship in Sport Management; Edward Elgar Publishing: Cheltenham, UK, 2021. [Google Scholar]
- Valenti, G.; Bonomi, A.G.; Westerterp, K.R. Walking as a Contributor to Physical Activity in Healthy Older Adults: 2 Week Longitudinal Study Using Accelerometry and the Doubly Labeled Water Method. JMIR Mhealth Uhealth 2016, 4, e56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MacIntosh, B.R.; Murias, J.M.; Keir, D.A.; Weir, J.M. What Is Moderate to Vigorous Exercise Intensity? Front. Physiol. 2021, 12, 682233. [Google Scholar] [CrossRef] [PubMed]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Reeder, B.; David, A. Health at hand: A systematic review of smart watch uses for health and wellness. J. Biomed Inform. 2016, 63, 269–276. [Google Scholar] [CrossRef]
- Lao, C.; Wang, B.; Wang, R.S.; Chang, H. The Combined Effects of Sports Smart Bracelet and Multi-Component Exercise Program on Exercise Motivation among the Elderly in Macau. Medicina 2021, 57, 34. [Google Scholar] [CrossRef]
- Fang, B.; Sun, F.; Quan, Z.; Liu, H.; Shan, J. Smart Bracelet System for Temperature Monitoring and Movement Tracking Analysis. J. Healthc. Eng. 2021, 2021, 8347261. [Google Scholar] [CrossRef]
- Luo, X.; Zhao, H.; Chen, Y. Research on User Experience of Sports Smart Bracelet Based on Fuzzy Comprehensive Appraisal and SSA-BP Neural Network. Comput. Intell. Neurosci. 2022, 2022, 5597662. [Google Scholar] [CrossRef]
- Angelini, L.; Caon, M.; Carrino, S.; Bergeron, L.; Nyffeler, N.; Jean-Mairet, M.; Mugellini, E. Designing a Desirable Smart Bracelet for Older Adults; Association for Computing Machinery: Zurich, Switzerland, 2013; pp. 425–434. [Google Scholar]
- Takahashi, P.Y.; Quigg, S.M.; Croghan, I.T.; Schroeder, D.R.; Ebbert, J.O. Effect of pedometer use and goal setting on walking and functional status in overweight adults with multimorbidity: A crossover clinical trial. Clin. Interv. Aging 2016, 11, 1099–1106. [Google Scholar] [CrossRef] [Green Version]
- Shin, G.; Jarrahi, M.H.; Fei, Y.; Karami, A.; Gafinowitz, N.; Byun, A.; Lu, X. Wearable activity trackers, accuracy, adoption, acceptance and health impact: A systematic literature review. J. Biomed. Inform. 2019, 93, 103153. [Google Scholar] [CrossRef] [PubMed]
- Reichardt, C.S.; Little, T.D. Quasi-Experimentation: A Guide to Design and Analysis; The Guilford Press: New York, NY, USA, 2019. [Google Scholar]
- Rudnicka, E.; Napierała, P.; Podfigurna, A.; Męczekalski, B.; Smolarczyk, R.; Grymowicz, M. The World Health Organization (WHO) approach to healthy ageing. Maturitas 2020, 139, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Gomes, M.; Figueiredo, D.; Teixeira, L.; Poveda, V.; Paúl, C.; Santos-Silva, A.; Costa, E. Physical inactivity among older adults across Europe based on the SHARE database. Age Ageing 2017, 46, 71–77. [Google Scholar] [CrossRef] [Green Version]
- Abt, G.; Boreham, C.; Davison, G.; Jackson, R.; Nevill, A.; Wallace, E.; Williams, M. Power, precision, and sample size estimation in sport and exercise science research. J. Sports Sci. 2020, 38, 1933–1935. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, A.; Haugen Mikalsen, M.; Woldaregay, A.Z.; Muzny, M.; Hartvigsen, G.; Hopstock, L.A.; Grimsgaard, S. Using Fitness Trackers and Smartwatches to Measure Physical Activity in Research: Analysis of Consumer Wrist-Worn Wearables. J. Med. Internet Res. 2018, 20, e110. [Google Scholar] [CrossRef]
- Tedesco, S.; Sica, M.; Ancillao, A.; Timmons, S.; Barton, J.; O’Flynn, B. Validity Evaluation of the Fitbit Charge2 and the Garmin vivosmart HR+ in Free-Living Environments in an Older Adult Cohort. JMIR Mhealth. Uhealth. 2019, 7, e13084. [Google Scholar] [CrossRef] [PubMed]
- Evenson, K.R.; Spade, C.L. Review of Validity and Reliability of Garmin Activity Trackers. J. Meas. Phys. Behav. 2020, 3, 170–185. [Google Scholar] [CrossRef] [PubMed]
- Coswig, V.S.; Barbalho, M.; Raiol, R.; Del Vecchio, F.B.; Ramirez-Campillo, R.; Gentil, P. Effects of high vs moderate-intensity intermittent training on functionality, resting heart rate and blood pressure of elderly women. J. Transl. Med. 2020, 18, 88. [Google Scholar] [CrossRef] [Green Version]
- Suni, E.; Singh, A. How much sleep do we really need? Sleep Foundation. Sleepfoundation.org. 2022. Available online: https://www.sleepfoundation.org/how-sleep-works/how-much-sleep-do-we-really-need (accessed on 5 July 2022).
- Tudor-Locke, C.; Craig, C.L.; Aoyagi, Y.; Bell, R.C.; Croteau, K.A.; De Bourdeaudhuij, I.; Ewald, B.; Gardner, A.W.; Hatano, Y.; Lutes, L.D.; et al. How many steps/day are enough? For older adults and special populations. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 80. [Google Scholar] [CrossRef] [Green Version]
- Joshi, A.; Kale, S.; Chandel, S.; Pal, D. Likert Scale: Explored and Explained. Br. J. Appl. Sci. Technol. 2015, 7, 396–403. [Google Scholar] [CrossRef]
- Chen, M.Y.; Chou, C.C.; Shiau, H.S.; Wang, E.K.; Chiou, H.J.; Liao, J.C. The development of Chinese version health promoting lifestyle profile. Chang. Gung. Nursing. 1997, 8, 14–24. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates, Publishers: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Team, J. Amsterdam, The Netherlands; Version 0.12.2 Computer Software. 2022. Available online: https://jasp-stats.org/previous-versions/ (accessed on 5 July 2022).
- Kelley, K.; Rausch, J.R. Sample size planning for the standardized mean difference: Accuracy in parameter estimation via narrow confidence intervals. Psychol. Methods 2006, 11, 363–385. [Google Scholar] [CrossRef] [PubMed]
- Nuttall, F.Q. Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutr. Today 2015, 50, 117–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laroche, D.P.; Marques, N.R.; Shumila, H.N.; Logan, C.R.; Laurent, R.S.; Gonçalves, M. Excess body weight and gait influence energy cost of walking in older adults. Med. Sci. Sports Exerc. 2015, 47, 1017–1025. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, X.; Wang, L.; Shen, F.; Ma, Y.; Fan, Y.; Niu, H. Dynamic walking stability of elderly people with various BMIs. Gait Posture 2019, 68, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Ðošić, A.; Živković, D.; Milanović, Z.; Živković, M.; Bjelaković, L.; Bratić, M.; Pantelić, S. The Association Between Level of Physical Activity and Body Mass Index, and Quality of Life Among Elderly Women. Front. Psychol. 2021, 12, 804449. [Google Scholar] [CrossRef]
- Bromell, L.; Cagney, K.A. Companionship in the neighborhood context: Older adults’ living arrangements and perceptions of social cohesion. Res. Aging 2014, 36, 228–243. [Google Scholar] [CrossRef] [Green Version]
- Choi, H. Giving or receiving spouse care and marital satisfaction among older Korean individuals. Soc. Sci. Med. 2021, 272, 112071. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, Z.; Zhang, L.; Zhu, P.; Wang, X.; Huang, Y. Association of living arrangements with depressive symptoms among older adults in China: A cross-sectional study. BMC Public Health 2019, 19, 1017. [Google Scholar] [CrossRef] [Green Version]
- Mauldin, R.L.; Fujimoto, K.; Wong, C.; Herrera, S.; Anderson, K.A. Social Networks in an Assisted Living Community: Correlates of Acquaintance and Companionship Ties Among Residents. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021, 76, 1463–1474. [Google Scholar] [CrossRef]
- de Souto Barreto, P. Direct and indirect relationships between physical activity and happiness levels among older adults: A cross-sectional study. Aging Ment. Health 2014, 18, 861–868. [Google Scholar] [CrossRef] [PubMed]
- Harris, T.; Limb, E.S.; Hosking, F.; Carey, I.; DeWilde, S.; Furness, C.; Wahlich, C.; Ahmad, S.; Kerry, S.; Whincup, P.; et al. Effect of pedometer-based walking interventions on long-term health outcomes: Prospective 4-year follow-up of two randomised controlled trials using routine primary care data. PLoS Med. 2019, 16, e1002836. [Google Scholar] [CrossRef]
- Fong, S.S.; Ng, S.S.; Cheng, Y.T.; Zhang, J.; Chung, L.M.; Chow, G.C.; Chak, Y.T.; Chan, I.K.; Macfarlane, D.J. Comparison between smartphone pedometer applications and traditional pedometers for improving physical activity and body mass index in community-dwelling older adults. J. Phys. Ther. Sci. 2016, 28, 1651–1656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sullivan, A.N.; Lachman, M.E. Behavior Change with Fitness Technology in Sedentary Adults: A Review of the Evidence for Increasing Physical Activity. Front. Public Health 2016, 4, 289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strasser, B.; Schobersberger, W. Evidence for resistance training as a treatment therapy in obesity. J. Obes. 2011, 2011, 482564. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Westcott, W.L. Resistance training is medicine: Effects of strength training on health. Curr. Sports Med. Rep. 2012, 11, 209–216. [Google Scholar] [CrossRef]
- Kouvelioti, R.; Vagenas, G.; Langley-Evans, S. Effects of exercise and diet on weight loss maintenance in overweight and obese adults: A systematic review. J. Sports Med. Phys. Fitness 2014, 54, 456–474. [Google Scholar]
- Niemiro, G.M.; Rewane, A.; Algotar, A.M. Exercise and Fitness Effect On Obesity. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Haase, M. Working out only on Weekends is just as Effective as Daily Exercise, Study Finds. 2022. Available online: https://www.prevention.com/fitness/workouts/a40542944/working-out-only-on-weekends-as-effective-as-daily-exercise-study-finds/ (accessed on 5 July 2022).
- Tsirtsakis, A. Regular exercise can improve brain function by up to 15%: Study. 20. 2022. Available online: https://www1.racgp.org.au/newsgp/clinical/regular-exercise-can-improve-brain-function-by-up (accessed on 5 July 2022).
- Notthoff, N.; Carstensen, L.L. Positive messaging promotes walking in older adults. Psychol. Aging 2014, 29, 329–341. [Google Scholar] [CrossRef] [Green Version]
- Del Pozo Cruz, B.; Ahmadi, M.; Naismith, S.L.; Stamatakis, E. Association of Daily Step Count and Intensity With Incident Dementia in 78 430 Adults Living in the UK. JAMA Neurol. 2022, 79, 1059–1063. [Google Scholar] [CrossRef]
- Yuenyongchaiwat, K.; Pipatsitipong, D.; Sangprasert, P. Increasing walking steps daily can reduce blood pressure and diabetes in overweight participants. Diabetol. Int. 2018, 9, 75–79. [Google Scholar] [CrossRef]
- Goh, S.L.; Persson, M.S.M.; Stocks, J.; Hou, Y.; Welton, N.J.; Lin, J.; Hall, M.C.; Doherty, M.; Zhang, W. Relative Efficacy of Different Exercises for Pain, Function, Performance and Quality of Life in Knee and Hip Osteoarthritis: Systematic Review and Network Meta-Analysis. Sports Med. 2019, 49, 743–761. [Google Scholar] [CrossRef] [Green Version]
- Messier, S.P.; Mihalko, S.L.; Beavers, D.P.; Nicklas, B.J.; DeVita, P.; Carr, J.J.; Hunter, D.J.; Lyles, M.; Guermazi, A.; Bennell, K.L.; et al. Effect of High-Intensity Strength Training on Knee Pain and Knee Joint Compressive Forces Among Adults With Knee Osteoarthritis: The START Randomized Clinical Trial. Jama 2021, 325, 646–657. [Google Scholar] [CrossRef] [PubMed]
- Kong, H.; Wang, X.Q.; Zhang, X.A. Exercise for Osteoarthritis: A Literature Review of Pathology and Mechanism. Front. Aging Neurosci. 2022, 14, 854026. [Google Scholar] [CrossRef]
- Lee, I.M.; Shiroma, E.J.; Kamada, M.; Bassett, D.R.; Matthews, C.E.; Buring, J.E. Association of Step Volume and Intensity With All-Cause Mortality in Older Women. JAMA Intern. Med. 2019, 179, 1105–1112. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Action Plan on Physical Activity 2018–2030; World Health Organization: Geneva, Switzerland, 2018; Available online: https://apps.who.int/iris/bitstream/handle/10665/272722/9789241514187-eng.pdf (accessed on 5 July 2022).
- Zaitsu, T.; Kanazawa, T.; Shizuma, Y.; Oshiro, A.; Takehara, S.; Ueno, M.; Kawaguchi, Y. Relationships between occupational and behavioral parameters and oral health status. Ind. Health 2017, 55, 381–390. [Google Scholar] [CrossRef] [Green Version]
- Baylina, P.; Barros, C.; Fonte, C.; Alves, S.; Rocha, Á. Healthcare Workers: Occupational Health Promotion and Patient Safety. J. Med. Syst. 2018, 42, 159. [Google Scholar] [CrossRef] [Green Version]
- Faller, E.M.; Bin Miskam, N.; Pereira, A. Exploratory Study on Occupational Health Hazards among Health Care Workers in the Philippines. Ann. Glob. Health 2018, 84, 338–341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomeer, M.B.; Hernandez, E.; Umberson, D.; Thomas, P.A. Influence of social connections on smoking behavior across the life course. Adv. Life Course Res. 2019, 42, 100294. [Google Scholar] [CrossRef] [Green Version]
- Bobo, J.K.; Husten, C. Sociocultural influences on smoking and drinking. Alcohol. Res. Health 2000, 24, 225–232. [Google Scholar]
- Philip, K.E.; Bu, F.; Polkey, M.I.; Brown, J.; Steptoe, A.; Hopkinson, N.S.; Fancourt, D. Relationship of smoking with current and future social isolation and loneliness: 12-year follow-up of older adults in England. Lancet Reg. Health Eur. 2022, 14, 100302. [Google Scholar] [CrossRef]
- Lim, K.H.; Jasvindar, K.; Cheong, S.M.; Ho, B.K.; Lim, H.L.; Teh, C.H.; Lau, K.J.; Suthahar, A.; Ambigga, D. Prevalence of smoking and its associated factors with smoking among elderly smokers in Malaysia: Findings from a nationwide population-based study. Tob. Induc. Dis. 2016, 14, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Assari, S.; Smith, J.L.; Zimmerman, M.A.; Bazargan, M. Cigarette Smoking among Economically Disadvantaged African-American Older Adults in South Los Angeles: Gender Differences. Int. J. Environ. Res. Public Health 2019, 16, 1208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mihailovic, N.; Szőllősi, G.J.; Rancic, N.; János, S.; Boruzs, K.; Nagy, A.C.; Timofeyev, Y.; Dragojevic-Simic, V.; Antunovic, M.; Reshetnikov, V.; et al. Alcohol Consumption among the Elderly Citizens in Hungary and Serbia-Comparative Assessment. Int. J. Environ. Res. Public Health 2020, 17, 1289. [Google Scholar] [CrossRef] [Green Version]
- Harris, J.C.; Mereish, E.H.; Faulkner, M.L.; Assari, S.; Choi, K.; Leggio, L.; Farokhnia, M. Racial Differences in the Association Between Alcohol Drinking and Cigarette Smoking: Preliminary Findings From an Alcohol Research Program. Alcohol. Alcohol. 2022, 57, 330–339. [Google Scholar] [CrossRef] [PubMed]
- Yannakoulia, M.; Mamalaki, E.; Anastasiou, C.A.; Mourtzi, N.; Lambrinoudaki, I.; Scarmeas, N. Eating habits and behaviors of older people: Where are we now and where should we go? Maturitas 2018, 114, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, M.; Aulisa, G.; Padua, E.; Annino, G.; Iellamo, F.; Pratesi, A.; Caprio, M.; Bellia, A. Gender differences in taste and foods habits. Nutr. Food Sci. 2020, 50, 229–239. [Google Scholar] [CrossRef]
- Ong, R.H.S.; Chow, W.L.; Cheong, M.; Lim, G.H.; Xie, W.; Baggs, G.; Huynh, D.T.T.; Oh, H.C.; How, C.H.; Tan, N.C.; et al. Associations between socio-demographics, nutrition knowledge, nutrition competencies and attitudes in community-dwelling healthy older adults in Singapore: Findings from the SHIELD study. J. Health Popul. Nutr. 2021, 40, 52. [Google Scholar] [CrossRef]
- Raptou, E.; Papastefanou, G. An empirical investigation of the impact of smoking on body weight using an endogenous treatment effects model approach: The role of food consumption patterns. Nutr. J. 2018, 17, 101. [Google Scholar] [CrossRef]
- Aaron, D.J.; Storti, K.L.; Robertson, R.J.; Kriska, A.M.; LaPorte, R.E. Longitudinal study of the number and choice of leisure time physical activities from mid to late adolescence: Implications for school curricula and community recreation programs. Arch. Pediatr. Adolesc. Med. 2002, 156, 1075–1080. [Google Scholar] [CrossRef] [Green Version]
- Sjöberg, A.; Hallberg, L.; Höglund, D.; Hulthén, L. Meal pattern, food choice, nutrient intake and lifestyle factors in The Göteborg Adolescence Study. Eur. J. Clin. Nutr. 2003, 57, 1569–1578. [Google Scholar] [CrossRef] [Green Version]
- Paavola, M.; Vartiainen, E.; Haukkala, A. Smoking, alcohol use, and physical activity: A 13-year longitudinal study ranging from adolescence into adulthood. J. Adolesc. Health 2004, 35, 238–244. [Google Scholar] [CrossRef]
- Larson, N.I.; Story, M.; Perry, C.L.; Neumark-Sztainer, D.; Hannan, P.J. Are diet and physical activity patterns related to cigarette smoking in adolescents? Findings from Project EAT. Prev. Chronic. Dis. 2007, 4, A51. [Google Scholar] [PubMed]
- Rounds, S.; Lu, Q.; Siamwala, J. Cigarette Smoking Increases The Risk of Acute Respiratory Distress Syndrome. Trans. Am. Clin. Climatol. Assoc. 2022, 132, 224–235. [Google Scholar] [PubMed]
- Brooks, R.D.; Grier, T.; Dada, E.O.; Jones, B.H. The Combined Effect of Cigarette Smoking and Fitness on Injury Risk in Men and Women. Nicotine Tob. Res. 2019, 21, 1621–1628. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, B.; Scully, P.; Curtin, R.J.; Plant, B.J. A study to assess smoking habits and smoking exposure in sportspeople. Qjm 2021, 114, 306–310. [Google Scholar] [CrossRef] [PubMed]
- Caetano, S.C.; Silva, C.M.; Vettore, M.V. Gender differences in the association of perceived social support and social network with self-rated health status among older adults: A population-based study in Brazil. BMC Geriatr. 2013, 13, 122. [Google Scholar] [CrossRef]
- Böhm, A.W.; Mielke, G.I.; da Cruz, M.F.; Ramirez, V.V.; Wehrmesister, F.C. Social Support and Leisure-Time Physical Activity Among the Elderly: A Population-Based Study. J. Phys. Act. Health 2016, 13, 599–605. [Google Scholar] [CrossRef]
- Schrempft, S.; Jackowska, M.; Hamer, M.; Steptoe, A. Associations between social isolation, loneliness, and objective physical activity in older men and women. BMC Public Health 2019, 19, 74. [Google Scholar] [CrossRef] [Green Version]
- Stults-Kolehmainen, M.A.; Sinha, R. The effects of stress on physical activity and exercise. Sports Med. 2014, 44, 81–121. [Google Scholar] [CrossRef] [Green Version]
- Childs, E.; de Wit, H. Regular exercise is associated with emotional resilience to acute stress in healthy adults. Front. Physiol. 2014, 5, 161. [Google Scholar] [CrossRef]
- Sharon-David, H.; Tenenbaum, G. The Effectiveness of Exercise Interventions on Coping with Stress: Research Synthesis. Stud. Sport Humanit. 2017, 22, 19–29. [Google Scholar] [CrossRef] [Green Version]
- Churchill, R.; Riadi, I.; Kervin, L.; Teo, K.; Cosco, T. Deciphering the role of physical activity in stress management during a global pandemic in older adult populations: A systematic review protocol. Syst. Rev. 2021, 10, 140. [Google Scholar] [CrossRef] [PubMed]
- Van Hoecke, A.S.; Delecluse, C.; Bogaerts, A.; Boen, F. Effects of need-supportive physical activity counseling on well-being: A 2-year follow-up among sedentary older adults. J. Phys. Act Health 2014, 11, 1492–1502. [Google Scholar] [CrossRef]
- Rovniak, L.S.; Kong, L.; Hovell, M.F.; Ding, D.; Sallis, J.F.; Ray, C.A.; Kraschnewski, J.L.; Matthews, S.A.; Kiser, E.; Chinchilli, V.M.; et al. Engineering Online and In-Person Social Networks for Physical Activity: A Randomized Trial. Ann. Behav. Med. 2016, 50, 885–897. [Google Scholar] [CrossRef] [PubMed]
- Lindsay Smith, G.; Banting, L.; Eime, R.; O’Sullivan, G.; van Uffelen, J.G.Z. The association between social support and physical activity in older adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 56. [Google Scholar] [CrossRef] [Green Version]
- Langhammer, B.; Bergland, A.; Rydwik, E. The Importance of Physical Activity Exercise among Older People. Biomed Res. Int. 2018, 2018, 7856823. [Google Scholar] [CrossRef]
- Dobarrio-Sanz, I.; Ruiz-González, C.; Fernández-Sola, C.; Roman, P.; Granero-Molina, J.; Hernández-Padilla, J.M. Healthcare Professionals’ Perceptions of Loneliness amongst Older Adults: A Qualitative Study. Int. J. Environ. Res. Public Health 2021, 18, 2071. [Google Scholar] [CrossRef]
- Gardiner, C.; Geldenhuys, G.; Gott, M. Interventions to reduce social isolation and loneliness among older people: An integrative review. Health Soc. Care Community 2018, 26, 147–157. [Google Scholar] [CrossRef]
- Turcotte, P.-L.; Carrier, A.; Roy, V.; Levasseur, M. Occupational therapists’ contributions to fostering older adults’ social participation: A scoping review. Br. J. Occup. Ther. 2018, 81, 427–449. [Google Scholar] [CrossRef]
- Han, A.; Kim, J.; Kim, J. A Study of Leisure Walking Intensity Levels on Mental Health and Health Perception of Older Adults. Gerontol. Geriatr. Med. 2021, 7, 2333721421999316. [Google Scholar] [CrossRef]
- Donovan, N.J.; Blazer, D. Social Isolation and Loneliness in Older Adults: Review and Commentary of a National Academies Report. Am. J. Geriatr. Psychiatry 2020, 28, 1233–1244. [Google Scholar] [CrossRef] [PubMed]
- Brawley, L.R.; Rejeski, W.J.; King, A.C. Promoting physical activity for older adults: The challenges for changing behavior. Am. J. Prev. Med. 2003, 25, 172–183. [Google Scholar] [CrossRef] [PubMed]
- Resnick, B.; D’Adamo, C.; Shardell, M.; Orwig, D.; Hawkes, W.; Hebel, J.R.; Golden, J.; Magaziner, J.; Zimmerman, S.; Yu-Yahiro, J. Adherence to an Exercise Intervention Among Older Women Post Hip Fracture. J. Clin. Sport Psychol. 2008, 2, 41–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weber, M.; Belala, N.; Clemson, L.; Boulton, E.; Hawley-Hague, H.; Becker, C.; Schwenk, M. Feasibility and Effectiveness of Intervention Programmes Integrating Functional Exercise into Daily Life of Older Adults: A Systematic Review. Gerontology 2018, 64, 172–187. [Google Scholar] [CrossRef]
- Rivera-Torres, S.; Fahey, T.D.; Rivera, M.A. Adherence to Exercise Programs in Older Adults: Informative Report. Gerontol. Geriatr. Med. 2019, 5, 2333721418823604. [Google Scholar] [CrossRef]
- Izquierdo, M.; Merchant, R.A.; Morley, J.E.; Anker, S.D.; Aprahamian, I.; Arai, H.; Aubertin-Leheudre, M.; Bernabei, R.; Cadore, E.L.; Cesari, M.; et al. International Exercise Recommendations in Older Adults (ICFSR): Expert Consensus Guidelines. J. Nutr. Health Aging 2021, 25, 824–853. [Google Scholar] [CrossRef]
- Sinha, R. Chronic stress, drug use, and vulnerability to addiction. Ann. N. Y. Acad. Sci. 2008, 1141, 105–130. [Google Scholar] [CrossRef] [Green Version]
- Amaro, H.; Reed, E.; Rowe, E.; Picci, J.; Mantella, P.; Prado, G. Brief screening and intervention for alcohol and drug use in a college student health clinic: Feasibility, implementation, and outcomes. J. Am. Coll Health 2010, 58, 357–364. [Google Scholar] [CrossRef]
- Taylor, G.; McNeill, A.; Girling, A.; Farley, A.; Lindson-Hawley, N.; Aveyard, P. Change in mental health after smoking cessation: Systematic review and meta-analysis. Bmj 2014, 348, g1151. [Google Scholar] [CrossRef] [Green Version]
- Quadir, S.G.; Santos, J.R.; Campbell, R.R.; Wroten, M.G.; Singh, N.; Holloway, J.J.; Bal, S.K.; Camarini, R.; Szumlinski, K.K. Homer2 regulates alcohol and stress cross-sensitization. Addict. Biol. 2016, 21, 613–633. [Google Scholar] [CrossRef] [Green Version]
- Torres-Berrio, A.; Cuesta, S.; Lopez-Guzman, S.; Nava-Mesa, M.O. Interaction Between Stress and Addiction: Contributions From Latin-American Neuroscience. Front. Psychol. 2018, 9, 2639. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koehler, K.; Drenowatz, C. Integrated Role of Nutrition and Physical Activity for Lifelong Health. Nutrients 2019, 11, 1437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elliot, C.A.; Hamlin, M.J. Combined diet and physical activity is better than diet or physical activity alone at improving health outcomes for patients in New Zealand’s primary care intervention. BMC Public Health 2018, 18, 230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feng, Z.; Cramm, J.M.; Nieboer, A.P. A healthy diet and physical activity are important to promote healthy ageing among older Chinese people. J. Int. Med. Res. 2019, 47, 6061–6081. [Google Scholar] [CrossRef]
- Vozzi, F.; Palumbo, F.; Ferro, E.; Kreiner, K.; Giugni, F.; Dutton, R.; Hall, S.; Musian, D.; Parolini, M.; Riso, P.; et al. Nutritional and physical improvements in older adults through the DOREMI remote coaching approach: A real-world study. Intell. Med. 2022, 2, 187–192. [Google Scholar] [CrossRef]
| Group | Method | Content |
|---|---|---|
| Male and female | Wristband walker | Dates: 8 weeks in total. Time: Monday to Friday, fixed 3:30–6:00 pm (during this period of time, participants could choose their own exercise time, and there was a roll call and record on site). Location: Walked together in the park from Monday to Friday, interviewer present for monitoring. Self-administered on Saturday and Sunday. Data collection: Participants recorded the total number of steps, time, calorie consumption, sleep time per night (using the built-in device of the smart bracelet) by themselves every day. They gathered in the park from 3:30 to 4:00 pm every other Monday for the test team to collect the data from all participants for the previous week. |
| Variables | Male (n = 60) | Female (n = 60) | t-Value | p-Value |
|---|---|---|---|---|
| M ± SD | M ± SD | |||
| Age (years) | 71.6 ± 1.25 | 72.3 ± 1.28 | 1.281 | 0.09 |
| Weight (kg) | 69.13 ± 4.82 | 62.56 ± 5.17 | 3.675 * | 0.00 |
| Height (cm) | 170.76 ± 7.18 | 159.94 ± 6.34 | 7.856 * | 0.00 |
| BMI (kg/m2) | 23.71 ± 1.65 | 24.46 ± 1.73 | −1.95 | 0.07 |
| Previous occupation (retired) | % | % | t-value | p-value |
| Cultural and educational institutions | 8.5 | 9.5 | −1.15 | 0.14 |
| Public utilities | 8.0 | 9.5 | 1.56 | 0.08 |
| Restaurant or hotel business | 8.0 | 11.0 | −3.42 * | 0.01 |
| Transportation industry | 13.0 | 5.5 | 5.82 * | 0.00 |
| Construction industry | 17.0 | 8.5 | 6.17 * | 0.00 |
| Manufacturing | 7.5 | 5.5 | 2.06 | 0.07 |
| News advertising | 4.5 | 8.0 | −3.54 * | 0.00 |
| Medical and health care industry | 5.5 | 13.5 | −6.58 * | 0.00 |
| Entertainment industry | 8.5 | 8.0 | 1.07 | 0.26 |
| Service industry | 10.5 | 10.5 | 0.84 | 0.54 |
| General business | 9.0 | 10.5 | −1.635 | 0.09 |
| Current residence status | % | % | t-value | p-value |
| Live alone | 14.0 | 3.0 | 10.65 | 0.00 |
| Live with spouse | 44.0 | 49.0 | −3.44 * | 0.01 |
| Living with spouse and children | 39.5 | 47.0 | −9.39 * | 0.00 |
| Live with friends | 2.5 | 1.0 | 1.15 | 0.13 |
| A | B | C | D | E | F | G | H | I | J | K | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Factor 1 | 0.38 */ 0.55 * | 0.44 */ 0.52 * | 0.33 */ 0.38 * | 0.28 */ 0.31 * | 0.28 */ 0.37 * | 0.41 */ 0.52 * | 0.48 */ 0.54 * | 0.47 */ 0.66 * | 0.38 */ 0.43 * | 0.31 */ 0.35 * | 0.33 */ 0.46 * |
| Factor 2 | 0.46 */ 0.59 * | 0.53 */ 0.56 * | 0.47 */ 0.43 * | 0.34 */ 0.35 * | 0.31 */ 0.42 * | 0.56 */ 0.59 * | 0.61 */ 0.67 * | 0.65 */ 0.73 * | 0.45 */ 0.51 * | 0.37 */ 0.43 * | 0.41 */ 0.52 * |
| Factor 3 | 0.45 */ 0.52 * | 0.49 */ 0.51 * | 0.48 */ 0.39 * | 0.38 */ 0.43 * | 0.45 */ 0.41 * | 0.44 */ 0.53 * | 0.47 */ 0.58 * | 0.66 */ 0.69 * | 0.32 */ 0.35 * | 0.48 */ 0.51 * | 0.40 */ 0.47 * |
| Factor 4 | 0.34 */ 0.33 * | 0.41 */ 0.40 * | 0.34 */ 0.31 * | 0.29 */ 0.35 * | 0.27 */ 0.34 * | 0.37 */ 0.35 * | 0.39 */ 0.34 * | 0.41 */ 0.36 * | 0.35 */ 0.32 * | 0.30 */ 0.27 * | 0.34 */ 0.31 * |
| Factor 5 | 0.45 */ 0.66 * | 0.43 */ 0.49 * | 0.37 */ 0.57 * | 0.31 */ 0.45 * | 0.29 */ 0.56 * | 0.24 */ 0.53 * | 0.43 */ 0.59 * | 0.65 */ 0.78 * | 0.31 */ 0.52 * | 0.33 */ 0.47 * | 0.27 */ 0.33 * |
| Day | Males (n = 60) | Females (n = 60) | t-Value | p-Value |
|---|---|---|---|---|
| M ± SD | M ± SD | |||
| Stride, cm | 64.16 ± 4.25 | 60.38 ± 4.41 | 3.62 * | 0.01 |
| Monday, steps | 7951.71 ± 153,42 | 7218.49 ± 114.73 | 4.76 * | 0.00 |
| Distance, km | 5.10 ± 0.27 | 4.36 ± 0.31 | 3.62 * | 0.01 |
| Calories, kcal | 467.56 ± 17.32 | 422.73 ± 13.64 | 4.76 * | 0.00 |
| Walking intensity—HR, beats/min | 104.45 ± 2.84 | 103.92 ± 2.57 | 1.35 | 0.09 |
| Sleep, hours | 7.23 ± 0.51 | 7.18 ± 0.46 | 1.24 | 0.11 |
| Tuesday, steps | 8613.55 ± 142.81 | 7261.58± 146.25 | 10.48 * | 0.00 |
| Distance, km | 5.53 ± 0.37 | 4.38 ± 0.29 | 5.13 * | 0.00 |
| Calories, kcal | 485.49 ± 17.62 | 431.44 ± 15,77 | 5.16 * | 0.00 |
| Walking intensity—HR, beats/min | 105.17 ± 2.56 | 104.63 ± 2.24 | 1.48 | 0.09 |
| Sleep, hours | 7.57 ± 0.46 | 7.46 ± 0.31 | 1.17 | 0.23 |
| Wednesday, steps | 8535.15 ± 166.25 | 7434.82 ± 136.41 | 11.46 * | 0.00 |
| Distance, km | 5.48 ± 0.37 | 4.49 ± 0.25 | 4.95 * | 0.00 |
| Calories, kcal | 502.16 ± 22.72 | 443.85 ± 17.33 | 6.76 * | 0.00 |
| Walking intensity—HR, beats/min | 107.61 ± 2.38 | 105.59 ± 2.44 | 1.43 | 0.09 |
| Sleep, hours | 7.81 ± 0.47 | 7.67 ± 0.39 | 1.39 | 0.10 |
| Thursday, steps | 8342.21 ± 119.15 | 7436.42 ± 121.28 | 9.17 * | 0.00 |
| Distance, km | 5.35 ± 0.27 | 4.49 ± 0.31 | 4.02 * | 0.00 |
| Calories, kcal | 492.36 ± 16.83 | 447.62 ± 15.53 | 4.73 * | 0.00 |
| Walking intensity—HR, beats/min | 103.93 ± 2.85 | 102.61 ± 2.63 | 1.41 | 0.09 |
| Sleep, hours | 7.55 ± 0.41 | 7.51 ± 0.39 | 1.06 | 0.23 |
| Friday, steps | 7812.52 ± 96.44 | 7347.75 ± 101.17 | 5.33* | 0.00 |
| Distance, km | 5.01 ± 0.18 | 4.44 ± 0.23 | 3.45 * | 0.01 |
| Calories, kcal | 471.85 ± 11.24 | 442.59 ± 11.08 | 4.64 * | 0.00 |
| Walking intensity- HR, beats/min | 104.92 ± 2.59 | 104.11 ± 2.33 | 1.15 | 0.21 |
| Sleep, hours | 7.86 ± 0.42 | 7.29 ± 0.38 | 1.76 | 0.08 |
| Saturday, steps | 5574.26 ± 185.29 | 5158.92 ± 172.31 | 3.25 * | 0.02 |
| Distance, km | 3.58 ± 0.27 | 3.12 ± 0.19 | 3.21 * | 0.04 |
| Calories, kcal | 332.93 ± 10.25 | 309.17 ± 9.43 | 3.23 * | 0.03 |
| Walking intensity—HR, beats/min | 68.71 ± 5.91 | 67.37 ± 4.76 | 1.15 | 0.17 |
| Sleep, hours | 8.17 ± 0.76 | 7.85 ± 0.64 | 2.23 | 0.06 |
| Sunday, steps | 4652.22 ± 174.53 | 4583.65 ± 125.34 | 1.83 | 0.08 |
| Distance, km | 2.98 ± 0.19 | 2.77 ± 0.23 | 1.16 | 0.12 |
| Calories, kcal | 271.45 ± 12.78 | 255.37 ± 10.49 | 1.54 | 0.09 |
| Walking intensity—HR, beats/min | 67.14 ± 4.85 | 66.25 ± 4.51 | 1.13 | 0.18 |
| Sleep, hours | 7.94 ± 0.67 | 7.75 ± 0.59 | 1.86 | 0.08 |
| Factors and Items | Males (n = 60) | Females (n = 60) | ||||
|---|---|---|---|---|---|---|
| Pre-Test M ± SD | Post-Test M ± SD | t-Value (p-Value) | Pre-Test M ± SD | Post-Test M ± SD | t-Value (p-Value) | |
| Factor 1: Healthy diet habit | 3.09 ± 0.28 | 4.02 ± 0.19 | −8.01 * (0.001) | 3.86 ± 0.21 | 4.16 ± 0.13 | −3.69 * (0.013) |
| 1. I control the amount of fat I eat. | 3.28 ± 0.26 | 4.16 ± 0.18 | −7.69 * (0.002) | 3.79 ± 0.26 | 4.14 ± 0.16 | −3.75 * (0.011) |
| 2. I control the amount of salt I eat. | 3.13 ± 0.29 | 4.01 ± 0.21 | −7.73 * (0.002) | 3.71 ± 0.28 | 4.13 ± 0.17 | −4.13 * (0.008) |
| 3. I avoid eating large amounts of sugar. | 3.15 ± 0.27 | 4.07 ± 0.16 | −8.87 * (0.001) | 3.85 ± 0.22 | 4.23 ± 0.11 | −4.22 * (0.007) |
| 4. I avoid chips and fried foods. | 2.81 ± 0.33 | 3.76 ± 0.25 | −8.95 * (0.001) | 3.96 ± 0.20 | 4.16 ± 0.15 | −3.18 * (0.015) |
| 5. I control the amount of red meat I eat. | 3.08 ± 0.34 | 4.09 ± 0.17 | −9.09 * (0.001) | 3.98 ± 0.19 | 4.12 ± 0.18 | −1.12 (0.102) |
| Factor 2: Proper use of health care resources | 3.11 ± 0.30 | 4.03 ± 0.19 | −8.65 * (0.001) | 3.11 ± 0.26 | 4.10 ± 0.16 | −9.68 * (0.001) |
| 6. I take the medicine according to the prescription. | 3.31 ± 0.27 | 4.09 ± 0.17 | −6.64 * (0.004) | 3.34 ± 0.22 | 4.11 ± 0.17 | −7.36 * (0.0011) |
| 7. I go to all my scheduled health care appointments. | 2.94 ± 0.31 | 3.87 ± 0.24 | −8.97 * (0.001) | 2.98 ± 0.31 | 3.98 ± 0.21 | −9.61 * (0.0003) |
| 8. I have dental exams every year. | 2.93 ± 0.33 | 3.91 ± 0.24 | −9.01 * (0.001) | 2.95 ± 0.34 | 3.95 ± 0.22 | −9.53 * (0.0003) |
| 9. I take prescription medication only as directed by a health care provider. | 3.19 ± 0.30 | 4.08 ± 0.19 | −8.14 * (0.001) | 3.18 ± 0.24 | 4.21 ± 0.12 | −10.12 * (0.0002) |
| 10. I take my blood pressure anytime. | 3.13 ± 0.32 | 4.09 ± 0.18 | −9.23 * (0.0005) | 3.08 ± 0.29 | 4.13 ± 0.16 | −10.24 * (0.0001) |
| 11. I ask a healthcare provider when I have unfamiliar physical symptoms. | 3.17 ± 0.31 | 4.15 ± 0.14 | −9.31 * (0.0004) | 3.15 ± 0.26 | 4.19 ± 0.14 | −10.16 * (0.0002) |
| Factor 3: Avoid strong emotions, tension and stress | 3.35 ± 0.22 | 3.87 ± 0.25 | −4.34 * (0.005) | 3.79 ± 0.25 | 4.00 ± 0.19 | −3.15 * (0.037) |
| 12. I get irritated and mad when waiting in lines. | 3.31 ± 0.25 | 3.87 ± 0.21 | −6.23 * (0.0017) | 3.74 ± 0.27 | 3.98 ± 0.21 | −3.19 * (0.018) |
| 13. I get angry and annoyed when I am caught in traffic. | 3.34 ± 0.23 | 3.85 ± 0.22 | −5.24 * (0.004) | 3.65 ± 0.29 | 3.92 ± 0.23 | −3.21 * (0.012) |
| 14. Things build up inside until I lose my temper. | 3.39 ± 0.22 | 3.89 ± 0.20 | −5.13 * (0.004) | 3.97 ± 0.24 | 4.11 ± 0.15 | −1.16 (0.17) |
| Factor 4: Regular physical activity | 2.95 ± 0.26 | 4.12 ± 0.16 | −11.41 * (0.0001) | 2.75 ± 0.28 | 4.05 ± 0.18 | −14.36 * (0.0001) |
| 15. I exercise at least three days a week for more than 30 min each time. | 2.56 ± 0.34 | 4.05 ± 0.23 | −18.42 * (0.0001) | 2.34 ± 0.37 | 4.01 ± 0.17 | −19.26 * (0.0001) |
| 16. I often have partner who exercises with me. | 3.11 ± 0.25 | 4.12 ± 0.18 | −10.17 * (0.0001) | 2.89 ± 0.26 | 4.08 ± 0.15 | −14.08 * (0.0001) |
| 17. When I am free, I think about being outdoors or exercise. | 3.17 ± 0.21 | 4.18 ± 0.17 | −10.23 * (0.0001) | 3.02 ± 0.24 | 4.05 ± 0.16 | −10.17 * (0.0001) |
| Factor 5: Avoid tobacco, alcohol and drug use | 3.14 ± 0.24 | 3.95 ± 0.17 | −7.81 * (0.0009) | 4.12 ± 0.13 | 4.22 ± 0.11 | −0.85 (0.34) |
| 18. I don’t smoke. | 3.01 ± 0.27 | 3.89 ± 0.19 | −8.58 * (0.0005) | 4.31 ± 0.11 | 4.44 ± 0.09 | −0.96 (0.21) |
| 19. I do not use recreational drugs. | 3.54 ± 0.21 | 4.11 ± 0.15 | 4.92 * (0.007) | 4.03 ± 0.17 | 4.12 ± 0.16 | −0.82 (0.33) |
| 20. I don’t use alcoholic beverages. | 2.87 ± 0.25 | 3.84 ± 0.20 | −9.81 * (0.0001) | 4.01 ± 0.19 | 4.09 ± 0.18 | −0.77 (0.39) |
| Factors and Items | Males (n = 60) | Females (n = 60) | |||||
|---|---|---|---|---|---|---|---|
| Pre-Test M ± SD | Post-Test M ± SD | t-Value (p-Value) | Post-Test M ± SD | Pre-Test M ± SD | t-Value (p-Value) | ||
| Factor 1: Health responsibility | 3.87 ± 0.27 | 4.09 ± 0.15 | −3.76 * (0.015) | 3.92 ± 0.25 | 4.16 ± 0.11 | −3.31 * (0.037) | |
| 1 | Watch TV programs about improving health. | 3.99 ± 0.21 | 4.19 ± 0.10 | −3.84 * (0.013) | 3.98 ± 0.21 | 4.28 ± 0.08 | −3.97 * (0.007) |
| 2 | Discuss my health concerns with a health professional. | 4.00 ± 0.19 | 4.11 ± 0.12 | −1.07 (0.124) | 4.06 ± 0.16 | 4.17 ± 0.11 | −1.22 (0.094) |
| 3 | Get a second opinion when I suspect advice given by my healthcare professional. | 3.97 ± 0.22 | 4.08 ± 0.16 | −1.18 (0.116) | 4.01 ± 0.18 | 4.15 ± 0.13 | −1.43 (0.075) |
| 4 | Examine my body at least once a year to detect any physical changes. | 3.91 ± 0.25 | 4.05 ± 0.17 | −1.55 (0.085) | 3.97 ± 0.23 | 4.08 ± 0.17 | −1.31 (0.087) |
| 5 | Attend educational programs on health care. | 3.47 ± 0.35 | 4.02 ± 0.19 | −7.16 * (0.0003) | 3.59 ± 0.32 | 4.11 ± 0.15 | −6.54 * (0.0005) |
| Factor 2: Physical activity | 3.23 ± 0.27 | 4.24 ± 0.10 | −11.15 * (0.0001) | 3.19 ± 0.22 | 4.09 ± 0.12 | −9.82 * (0.0002) | |
| 6 | Exercise vigorously for 30 min or more at least three times a week. | 3.24 ± 0.27 | 4.21 ± 0.13 | −9.68 * (0.0002) | 3.19 ± 0.24 | 4.18 ± 0.08 | −9.25 * (0.0003) |
| 7 | Participate in physical activity at a mild to moderate level. | 3.20 ± 0.28 | 4.24 ± 0.11 | −11.71 * (0.0001) | 3.15 ± 0.26 | 4.07 ± 0.13 | −8.41 * (0.0007) |
| 8 | Do stretching exercises at least 3 times a week. | 3.19 ± 0.29 | 4.25 ± 0.16 | −11.58 * (0.0001) | 3.21 ± 0.23 | 4.05 ± 0.15 | −8.23 * (0.0009) |
| 9 | Participate in leisure physical activities. | 3.24 ± 0.27 | 4.19 ± 0.14 | −10.26 * (0.0001) | 3.15 ± 0.26 | 4.04 ± 0.17 | −8.04 * (0.0012) |
| 10 | Exercise while doing daily activities. | 3.18 ± 0.29 | 4.25 ± 0.10 | −11.79 * (0.0001) | 3.17 ± 0.25 | 4.13 ± 0.11 | −9.61 * (0.0002) |
| 11 | Checking my pulse rate while exercising. | 3.30 ± 0.23 | 4.31 ± 0.07 | −10.23 * (0.0001) | 3.25 ± 0.22 | 4.06 ± 0.13 | −7.57 * (0.0016) |
| Factor 3: Nutrition | 3.65 ± 0.23 | 4.08 ± 0.12 | −4.77 * (0.0046) | 3.81 ± 0.21 | 4.21 ± 0.09 | −4.30 * (0.0081) | |
| 12 | Choose a diet low in fat, saturated fat and cholesterol. | 3.59 ± 0.29 | 4.13 ± 0.11 | −5.66 * (0.0011) | 3.79 ± 0.25 | 4.25 ± 0.08 | −4.61 * (0.0062) |
| 13 | Limit sugar intake and foods that contain sugar (sweet). | 3.81 ± 0.21 | 4.11 ± 0.11 | −4.23 * (0.0093) | 3.85 ± 0.21 | 4.27 ± 0.07 | −4.35 * (0.0075) |
| 14 | Eat 1.5 to 4 bowls of staple food, including cereals, rice and noodles daily. | 3.66 ± 0.23 | 4.08 ± 0.13 | −4.41 * (0.0065) | 3.78 ± 0.27 | 4.19 ± 0.13 | −3.73 * (0.028) |
| 15 | Eat 2 to 4 fist-sized pieces of fruit daily. | 3.61 ± 0.20 | 3.95 ± 0.18 | −3.54 * (0.032) | 3.81 ± 0.23 | 4.11 ± 0.17 | −3.45 * (0.037) |
| 16 | Eat 3 to 5 plates of vegetables daily. | 3.69 ± 0.23 | 4.05 ± 0.14 | −4.16 * (0.011) | 3.82 ± 0.22 | 4.15 ± 0.15 | −3.92 * (0.022) |
| 17 | Drink 350 to 500 mL of dairy daily. | 3.53 ± 0.31 | 4.14 ± 0.10 | −5.33 * (0.0028) | 3.79 ± 0.26 | 4.20 ± 0.10 | −4.12 * (0.015) |
| 18 | Eat 115–300 g based on meat, chicken, fish, dried beans, eggs and bean groups daily. | 3.68 ± 0.22 | 4.09 ± 0.12 | −4.37 * (0.0074) | 3.86 ± 0.19 | 4.26 ± 0.07 | −4.42 * (0.0063) |
| Factor 4: Spiritual growth | 3.58 ± 0.21 | 4.18 ± 0.10 | −5.45 * (0.0026) | 3.63 ± 0.23 | 4.19 ± 0.11 | −5.25 * (0.0054) | |
| 19 | Get enough sleep. | 3.63 ± 0.19 | 4.16 ± 0.12 | −4.87 * (0.0062) | 3.66 ± 0.22 | 4.14 ± 0.13 | −4.54 * (0.0076) |
| 20 | Feeling I am growing and changing in a positive way. | 3.57 ± 0.21 | 4.11 ± 0.16 | −4.65 * (0.0074) | 3.60 ± 0.25 | 4.15 ± 0.12 | −5.33 * (0.0047) |
| 21 | Believe that my life has a purpose. | 3.61 ± 0.20 | 4.18 ± 0.12 | −5.39 * (0.0031) | 3.78 ± 0.18 | 4.26 ± 0.06 | −4.81 * (0.0064) |
| 22 | Looking to the future. | 3.64 ± 0.19 | 4.29 ± 0.09 | −9.42 * (0.0004) | 3.69 ± 0.21 | 4.23 ± 0.07 | −5.26 * (0.0053) |
| 23 | Concentrate on pleasant thoughts before bed. | 3.41 ± 0.25 | 4.15 ± 0.13 | −8.38 * (0.0006) | 3.42 ± 0.28 | 4.16 ± 0.12 | −7.49 * (0.0012) |
| Factor 5: Social support | 3.45 ± 0.22 | 4.26 ± 0.09 | −8.75 * (0.0005) | 3.32 ± 0.22 | 4.21 ± 0.13 | −9.28 * (0.00034) | |
| 24 | Discuss exercise patterns with friends. | 3.31 ± 0.26 | 4.17 ± 0.12 | −9.47 * (0.0004) | 3.26 ± 0.26 | 4.12 ± 0.16 | −8.51 * (0.00057) |
| 25 | I would compliment a friend’s athleticism. | 3.33 ± 0.25 | 4.16 ± 0.14 | −9.59 * (0.0003) | 3.21 ± 0.28 | 4.15 ± 0.14 | −10.97 * (0.0001) |
| 26 | Exercise with friends. | 3.35 ± 0.25 | 4.27 ± 0.09 | −10.96 * (0.0001) | 3.23 ± 0.27 | 4.17 ± 0.13 | −11.09 * (0.0001) |
| 27 | I will show concern to my friends. | 3.62 ± 0.18 | 4.24 ± 0.10 | −7.34 * (0.0009) | 3.54 ± 0.19 | 4.25 ± 0.11 | −7.86 * (0.0008) |
| 28 | Playing sports with friends makes me happy. | 3.49 ± 0.22 | 4.36 ± 0.07 | −9.81 * (0.0002) | 3.37 ± 0.23 | 4.32 ± 0.07 | −11.53 * (0.0001) |
| 29 | Get support from friends while exercising. | 3.58 ± 0.19 | 4.37 ± 0.06 | −7.12 * (0.0011) | 3.33 ± 0.24 | 4.24 ± 0.11 | −11.67 * (0.0001) |
| Factor 6: Stress management | 3.45 ± 0.23 | 4.28 ± 0.10 | −8.46 * (0.0005) | 3.47 ± 0.25 | 4.21 ± 0.11 | −7.16 * (0.0018) | |
| 30 | Accepting things I can’t change in my life. | 3.39 ± 0.26 | 4.19 ± 0.13 | −8.38 * (0.0007) | 3.35 ± 0.30 | 4.11 ± 0.15 | −7.22 * (0.0014) |
| 31 | Feel satisfied and calm with yourself. | 3.62 ± 0.21 | 4.24 ± 0.11 | −7.59 * (0.0011) | 3.59 ± 0.23 | 4.14 ± 0.14 | −4.79 * (0.0093) |
| 32 | Exercise makes me less stressed. | 3.34 ± 0.28 | 4.53 ± 0.07 | −14.53 * (0.0001) | 3.44 ± 0.26 | 4.32 ± 0.07 | −9.94 * (0.0003) |
| 33 | Finding that every day is exciting and challenging. | 3.43 ± 0.25 | 4.33 ± 0.09 | −10.26 * (0.0003) | 3.41 ± 0.27 | 4.19 ± 0.12 | −7.85 * (0.0008) |
| 34 | Calm myself to avoid fatigue. | 3.49 ± 0.24 | 4.12 ± 0.15 | −6.77 * (0.0015) | 3.54 ± 0.24 | 4.31 ± 0.08 | −7.39 * (0.0011) |
| HBI | ||||||
|---|---|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | ||
| Healthy Diet Habit | Proper Use of Health Care Resources | Avoid Strong Emotions, Tension, Stress | Regular Physical Activity | Avoid Tobacco, Alcohol, and Drug Use | ||
| HPLI | Factor 1: Health responsibility | 0.74 * | 0.78 * | 0.73 * | 0.81 * | 0.78 * |
| Factor 2: Physical activity | 0.80 * | 0.83 * | 0.85 * | 0.92 * | 0.75 * | |
| Factor 3: Nutrition | 0.79 * | 0.77 * | 0.68 * | 0.83 * | 0.74 * | |
| Factor 4: Spiritual growth | 0.68 * | 0.73 * | 0.81 * | 0.84 * | 0.66 * | |
| Factor 5: Social support | 0.60 * | 0.75 * | 0.76 * | 0.81 * | 0.63 * | |
| Factor 6: Stress management | 0.67 * | 0.65 * | 0.84 * | 0.89 * | 0.79 * | |
| HBI | ||||||
|---|---|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | ||
| Healthy Diet Habit | Proper Use of Health Care Resources | Avoid Strong Emotions, Tension, Stress | Regular Physical Activity | Avoid Tobacco, Alcohol, and Drug Use | ||
| HPLI | Factor 1: Health responsibility | 0.86 * | 0.87 * | 0.84 * | 0.86 * | 0.87 * |
| Factor 2: Physical activity | 0.84 * | 0.78 * | 0.84 * | 0.91 * | 0.88 * | |
| Factor 3: Nutrition | 0.87 * | 0.81 * | 0.75 * | 0.84 * | 0.78 * | |
| Factor 4: Spiritual growth | 0.78 * | 0.79 * | 0.83 * | 0.80 * | 0.78 * | |
| Factor 5: Social support | 0.83 * | 0.83 * | 0.86 * | 0.94 * | 0.62 * | |
| Factor 6: Stress management | 0.79 * | 0.84 * | 0.84 * | 0.87 * | 0.74 * | |
| Variables | β | R | R2 | Adjusted R2 | p |
|---|---|---|---|---|---|
| Healthy diet habits | 0.531 * | 0.842 | 0.709 | 0.707 | <0.001 |
| Proper use of health care resources | 0.517 * | <0.002 | |||
| Avoid strong emotions, tension, and stress | 0.439 * | <0.006 | |||
| Regular physical activity | 0.624 * | <0.001 | |||
| Avoid tobacco, alcohol, and drug use | 0.481 * | <0.004 |
| Variables | β | R | R2 | Adjusted R2 | p |
|---|---|---|---|---|---|
| Healthy diet habits | 0.578 * | 0.861 | 0.741 | 0.739 | <0.001 |
| Proper use of health care resources | 0.494 * | <0.003 | |||
| Avoid strong emotions, tension, and stress | 0.473 * | <0.004 | |||
| Regular physical activity | 0.606 * | <0.001 | |||
| Avoid tobacco, alcohol, and drug use | 0.455 * | <0.006 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chia, F.; Huang, W.-Y.; Huang, H.; Wu, C.-E. Promoting Healthy Behaviors in Older Adults to Optimize Health-Promoting Lifestyle: An Intervention Study. Int. J. Environ. Res. Public Health 2023, 20, 1628. https://doi.org/10.3390/ijerph20021628
Chia F, Huang W-Y, Huang H, Wu C-E. Promoting Healthy Behaviors in Older Adults to Optimize Health-Promoting Lifestyle: An Intervention Study. International Journal of Environmental Research and Public Health. 2023; 20(2):1628. https://doi.org/10.3390/ijerph20021628
Chicago/Turabian StyleChia, Fan, Wei-Yang Huang, Hsuan Huang, and Cheng-En Wu. 2023. "Promoting Healthy Behaviors in Older Adults to Optimize Health-Promoting Lifestyle: An Intervention Study" International Journal of Environmental Research and Public Health 20, no. 2: 1628. https://doi.org/10.3390/ijerph20021628





