Physiotherapists Using the Biopsychosocial Model for Chronic Pain: Barriers and Facilitators—A Scoping Review
Abstract
:1. Introduction
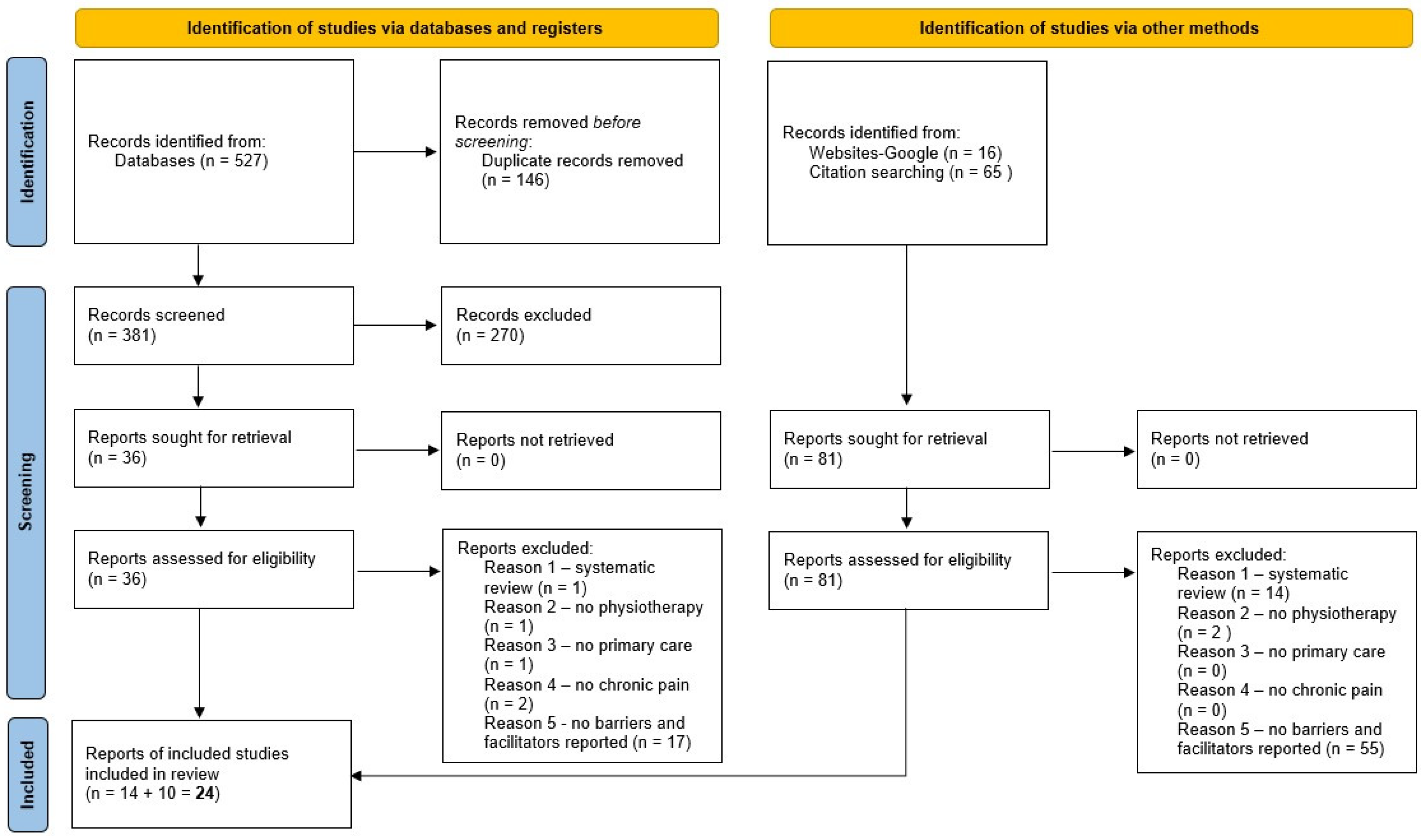
2. Materials and Methods
2.1. Framework, Protocol, and Registration
2.2. Search
2.3. Study Selection
2.4. Data Charting (Incl. Data Items and Critical Appraisal)
- study article: authors, publication data, country
- study design and statistical methods
- whether the study is part of a larger trial; the underlying perspective, intervention or method
- characteristics of the study population (patients and therapists)
- primary outcomes (challenges, barriers and facilitators)
2.5. Data Synthesis
3. Results
3.1. Knowledge, Skills, and Attitudes/TDF(v2) Knowledge, Skills, and Intentions [20]
3.2. Confidence/(TDF(v2) Beliefs about Capabilities [20]
3.3. Role Clarity/TDF(v2) Social/Professional Role and Identity [20]
3.4. Environmental Context and Resources/TDF(v2) Environmental Context and Resources [20]
3.5. Patient Expectations, Beliefs and Attitudes/TDF(v2) -
3.6. Therapeutic Alliance/TDF(v2) Beliefs about Consequences [20]
3.7. Themes Relating to the Theoretical Domains Framework (TDFv2)
4. Discussion
4.1. Strengths and Limitations
4.2. Implications for Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| APTA | American Physical Therapy Association |
| BCT | Behavioral Change Technique |
| BM | biomedical |
| BPS | biopsychosocial |
| CBA | Cognitive Behavioral Approach |
| CBT | Cognitive Behavioral Therapy |
| CFT | Cognitive Functional Therapy |
| HCP | health care providers |
| LBP | low back pain |
| MTP | Manual Therapist |
| NP | neck pain |
| NSCLBP | Non-specific Chronic Low Back Pain |
| NSLBP | Nonspecific Low Back Pain |
| OA | osteoarthritis |
| PCST | Pain Coping Skills Training |
| PRISMA-ScR | Preferred Reporting Items for Systematic reviews and Meta-analyses extension for Scoping Reviews |
| PS | psychosocial |
| PT | physiotherapist |
| RAAK-publiek | Regionale actie en aandacht voor kenniscirculatie (Regional action and attention for knowledge-circulation) |
| SCA | Stratified Care Approach |
| TDF | Theoretical Domains Framework |
| TDF(v2) | Theoretical Domains Framework–version 2 |
Appendix A. Search PubMed, Embase, CINAHL and ERIC
Appendix B. Searched Grey Literature Sources
- Dissertations:
- DART Europe: https://www.dart-europe.org/basic-search.php accessed on 12 July 2022.
- Guidelines:
- Dutch guidelines: Richtlijnen Koninklijk Nederlands Genootschap voor Fysiotherapie: https://www.kngf.nl/kennisplatform/richtlijnen accessed on 12 July 2022.
- Guidelines International Network: https://guidelines.ebmportal.com/guidelines-international-network accessed on 12 July 2022.
Appendix C. Results Search
| Database | Articles Found |
|---|---|
| PubMed | 191 |
| Embase | 237 |
| CINAHL + ERIC | 99 |
| Total | 527 |
| Deduplicated | 381 |
| Grey Literature Source | Sources Found |
|---|---|
| DART Europe | 8 |
| KNGF guideline | 0 |
| Guidel. Int. Netw. | 17 |
| Total | 25 |
References
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abdelalim, A.; Abdollahi, M.; Abdollahpour, I.; Abegaz, K.H.; et al. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Nicholas, M.; Vlaeyen, J.W.S.; Rief, W.; Barke, A.; Aziz, Q.; Benoliel, R.; Cohen, M.; Evers, S.; Giamberardino, M.A.; Goebel, A.; et al. The IASP Classification of Chronic Pain for ICD-11: Chronic Primary Pain. Pain 2019, 160, 28–37. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Kamper, S.J.; French, S.D. Low-Value Care in Musculoskeletal Health Care: Is There a Way Forward? Pain Pract. 2022, 22, 65–70. [Google Scholar] [CrossRef]
- Swart, N.M.; Apeldoorn, A.T.; Conijn, D.; Meerhoff, G.A.; Ostelo, R.W.J.G. KNGF Guideline Low Back Pain and Lumbosacral Radiculair Syndrome; KNGF: Amersfoort, The Netherlands, 2021. [Google Scholar]
- Edwards, R.R.; Dworkin, R.H.; Turk, D.C.; Angst, M.S.; Dionne, R.; Freeman, R.; Hansson, P.; Haroutounian, S.; Arendt-Nielsen, L.; Attal, N.; et al. Patient Phenotyping in Clinical Trials of Chronic Pain Treatments: IMMPACT Recommendations. Pain 2016, 157, 1851–1871. [Google Scholar] [CrossRef]
- Bruehl, S. Personalized Pain Medicine: Pipe Dream or Reality? Anesthesiology 2015, 122, 967–968. [Google Scholar] [CrossRef] [Green Version]
- Kamper, S.J.; Apeldoorn, A.T.; Chiarotto, A.; Smeets, R.J.E.M.; Ostelo, R.W.J.G.; Guzman, J.; Tulder, M.W.V. Multidisciplinary Biopsychosocial Rehabilitation for Chronic Low Back Pain: Cochrane Systematic Review and Meta-Analysis. BMJ 2015, 350, h444. [Google Scholar] [CrossRef] [Green Version]
- Smeets, R.J.E.M. How to Sustain and Improve Client Centred (Matched) Care in Chronic Musculoskeletal Pain? Start by Changing the Way Policy Makers Select and Judge the Large Amount of Available Data, and Get Rid of the Dogma of Stepped Care. Eur. J. Physiother. 2021, 23, 66–67. [Google Scholar] [CrossRef]
- Nicholas, M.K.; Linton, S.J.; Watson, P.J.; Main, C.J. Early Identification and Management of Psychological Risk Factors (“yellow Flags”) in Patients with Low Back Pain: A Reappraisal. Phys. Ther. 2011, 91, 737–753. [Google Scholar] [CrossRef]
- Simpson, P.; Holopainen, R.; Schütze, R.; O’Sullivan, P.; Smith, A.; Linton, S.J.; Nicholas, M.; Kent, P. Training of Physical Therapists to Deliver Individualized Biopsychosocial Interventions to Treat Musculoskeletal Pain Conditions: A Scoping Review. Phys. Ther. 2021, 101, pzab188. [Google Scholar] [CrossRef]
- Synnott, A.; O’Keeffe, M.; Bunzli, S.; Dankaerts, W.; O’Sullivan, P.; O’Sullivan, K. Physiotherapists May Stigmatise or Feel Unprepared to Treat People with Low Back Pain and Psychosocial Factors That Influence Recovery: A Systematic Review. J. Physiother. 2015, 61, 68–76. [Google Scholar] [CrossRef]
- Alexanders, J.; Anderson, A.; Henderson, S. Musculoskeletal Physiotherapists’ Use of Psychological Interventions: A Systematic Review of Therapists’ Perceptions and Practice. Physiotherapy 2015, 101, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Ng, W.; Slater, H.; Starcevich, C.; Wright, A.; Mitchell, T.; Beales, D. Barriers and Enablers Influencing Healthcare Professionals’ Adoption of a Biopsychosocial Approach to Musculoskeletal Pain: A Systematic Review and Qualitative Evidence Synthesis. Pain 2021, 162, 2154–2185. [Google Scholar] [CrossRef] [PubMed]
- Toye, F.; Seers, K.; Barker, K.L. Meta-Ethnography to Understand Healthcare Professionals’ Experience of Treating Adults with Chronic Non-Malignant Pain. BMJ Open 2017, 7, e018411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arksey, H.; O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. Theory Pract. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping Studies: Advancing the Methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [Green Version]
- Peters, M.D.J.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for Conducting Systematic Scoping Reviews. Int. J. Evid. Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef] [Green Version]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Cane, J.; O’Connor, D.; Michie, S. Validation of the Theoretical Domains Framework for Use in Behaviour Change and Implementation Research. Implement. Sci. 2012, 7, 37. [Google Scholar] [CrossRef] [Green Version]
- Atkins, L.; Francis, J.; Islam, R.; O’Connor, D.; Patey, A.; Ivers, N.; Foy, R.; Duncan, E.M.; Colquhoun, H.; Grimshaw, J.M.; et al. A Guide to Using the Theoretical Domains Framework of Behaviour Change to Investigate Implementation Problems. Implement. Sci. 2017, 12, 77. [Google Scholar] [CrossRef] [Green Version]
- Beissner, K.; Henderson, C.R., Jr.; Papaleontiou, M.; Olkhovskaya, Y.; Wigglesworth, J.; Reid, M.C. Physical Therapists’ Use of Cognitive-Behavioral Therapy for Older Adults With Chronic Pain: A Nationwide Survey. Phys. Ther. 2009, 89, 456–469. [Google Scholar] [CrossRef]
- Verwoerd, M.J.; Wittink, H.; Goossens, M.E.J.B.; Maissan, F.; Smeets, R.J.E.M. Physiotherapists’ Knowledge, Attitude and Practice Behavior to Prevent Chronification in Patients with Non-Specific, Non-Traumatic, Acute- and Subacute Neck Pain: A Qualitative Study. Musculoskelet. Sci. Pract. 2022, 57, 102493. [Google Scholar] [CrossRef]
- Sandelowski, M.; Barroso, J. Classifying the Findings in Qualitative Studies. Qual. Health Res. 2003, 13, 905–923. [Google Scholar] [CrossRef]
- Holopainen, R.; Piirainen, A.; Karppinen, J.; Linton, S.J.; O’Sullivan, P. An Adventurous Learning Journey. Physiotherapists’ Conceptions of Learning and Integrating Cognitive Functional Therapy into Clinical Practice. Physiother. Theory Pract. 2022, 38, 309–326. [Google Scholar] [CrossRef] [PubMed]
- Al Zoubi, F.M.; French, S.D.; Patey, A.M.; Mayo, N.E.; Bussières, A.E. Professional Barriers and Facilitators to Using Stratified Care Approaches for Managing Non-Specific Low Back Pain: A Qualitative Study with Canadian Physiotherapists and Chiropractors. Chiropr. Man. Ther. 2019, 27, 68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cowell, I.; O’Sullivan, P.; O’Sullivan, K.; Poyton, R.; McGregor, A.; Murtagh, G. Perceptions of Physiotherapists towards the Management of Non-Specific Chronic Low Back Pain from a Biopsychosocial Perspective: A Qualitative Study. Musculoskelet. Sci. Pract. 2018, 38, 113–119. [Google Scholar] [CrossRef]
- Denneny, D.; Frijdal Nee Klapper, A.; Bianchi-Berthouze, N.; Greenwood, J.; McLoughlin, R.; Petersen, K.; Singh, A.; C de C Williams, A. The Application of Psychologically Informed Practice: Observations of Experienced Physiotherapists Working with People with Chronic Pain. Physiotherapy 2020, 106, 163–173. [Google Scholar] [CrossRef] [Green Version]
- Fritz, J.; Söderbäck, M.; Söderlund, A.; Sandborgh, M. The Complexity of Integrating a Behavioral Medicine Approach into Physiotherapy Clinical Practice. Physiother. Theory Pract. 2019, 35, 1182–1193. [Google Scholar] [CrossRef]
- Vervaeke, R. Prospect of Direct-Access Management of Low-Back Pain: Survey of Subjective Examination Practices of French Physiotherapists in Private Practice. Exploratory Study. Kinesitherapie 2019, 19, 44–49. [Google Scholar] [CrossRef]
- Zangoni, G.; Thomson, O.P. ‘I Need to Do Another Course’—Italian Physiotherapists’ Knowledge and Beliefs When Assessing Psychosocial Factors in Patients Presenting with Chronic Low Back Pain. Musculoskelet. Sci. Pract. 2017, 27, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.; Foster, N.E.; Bishop, A.; Ong, B.N. Biopsychosocial Care and the Physiotherapy Encounter: Physiotherapists’ Accounts of Back Pain Consultations. BMC Musculoskelet. Disord. 2013, 14, 65. [Google Scholar] [CrossRef]
- Schröder, K.; Öberg, B.; Enthoven, P.; Kongsted, A.; Abbott, A. Confidence, Attitudes, Beliefs and Determinants of Implementation Behaviours among Physiotherapists towards Clinical Management of Low Back Pain before and after Implementation of the BetterBack Model of Care. BMC Health Serv. Res. 2020, 20, 443. [Google Scholar] [CrossRef] [PubMed]
- Richmond, H.; Hall, A.M.; Hansen, Z.; Williamson, E.; Davies, D.; Lamb, S.E. Exploring Physiotherapists’ Experiences of Implementing a Cognitive Behavioural Approach for Managing Low Back Pain and Identifying Barriers to Long-Term Implementation. Physiotherapy 2018, 104, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Oostendorp, R.A.B.; Elvers, H.; Mikołajewska, E.; Laekeman, M.; Van Trijffel, E.; Samwel, H.; Duquet, W. Manual Physical Therapists’ Use of Biopsychosocial History Taking in the Management of Patients with Back or Neck Pain in Clinical Practice. Sci. World J. 2015, 2015, 170463. [Google Scholar] [CrossRef] [PubMed]
- Jeffrey, J.E.; Foster, N.E. A Qualitative Investigation of Physical Therapists’ Experiences and Feelings of Managing Patients with Nonspecific Low Back Pain. Phys. Ther. 2012, 92, 266–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- França, A.A.; dos Santos, V.; Filho, R.L.; Pires, K.F.; Lagoa, K.F.; Martins, W.R. ‘It’s Very Complicated’: Perspectives and Beliefs of Newly Graduated Physiotherapists about the Biopsychosocial Model for Treating People Experiencing Non-Specific Low Back Pain in Brazil. Musculoskelet. Sci. Pract. 2019, 42, 84–89. [Google Scholar] [CrossRef]
- Singla, M.; Jones, M.; Edwards, I.; Kumar, S. Physiotherapists’ Assessment of Patients’ Psychosocial Status: Are We Standing on Thin Ice? A Qualitative Descriptive Study. Man. Ther. 2015, 20, 328–334. [Google Scholar] [CrossRef]
- Caeiro, C.; Canhão, H.; Paiva, S.; Gomes, L.A.; Fernandes, R.; Rodrigues, A.M.; Sousa, R.; Pimentel-Santos, F.; Branco, J.; Fryxell, A.C.; et al. Interdisciplinary Stratified Care for Low Back Pain: A Qualitative Study on the Acceptability, Potential Facilitators and Barriers to Implementation. PLoS ONE 2019, 14, e0225336. [Google Scholar] [CrossRef] [Green Version]
- Demmelmaier, I.; Denison, E.; Lindberg, P.; Åsenlöf, P. Tailored Skills Training for Practitioners to Enhance Assessment of Prognostic Factors for Persistent and Disabling Back Pain: Four Quasi-Experimental Single-Subject Studies. Physiother. Theory Pract. 2012, 28, 359–372. [Google Scholar] [CrossRef]
- Fritz, J.; Wallin, L.; Söderlund, A.; Almqvist, L.; Sandborgh, M. Implementation of a Behavioral Medicine Approach in Physiotherapy: Impact and Sustainability. Disabil. Rehabil. 2020, 42, 3467–3474. [Google Scholar] [CrossRef] [Green Version]
- Matthews, J.; Hall, A.M.; Hernon, M.; Murray, A.; Jackson, B.; Taylor, I.; Toner, J.; Guerin, S.; Lonsdale, C.; Hurley, D.A. A Brief Report on the Development of a Theoretically-Grounded Intervention to Promote Patient Autonomy and Self-Management of Physiotherapy Patients: Face Validity and Feasibility of Implementation. BMC Health Serv. Res. 2015, 15, 260. [Google Scholar] [CrossRef]
- Nielsen, M.; Keefe, F.J.; Bennell, K.; Jull, G.A. Physical Therapist-Delivered Cognitive-Behavioral Therapy: A Qualitative Study of Physical Therapists Perceptions and Experiences. Phys. Ther. 2014, 94, 197–209. [Google Scholar] [CrossRef] [PubMed]
- Man, I.; Kumar, S.; Jones, M.; Edwards, I. An Exploration of Psychosocial Practice within Private Practice Musculoskeletal Physiotherapy: A Cross-Sectional Survey. Musculoskelet. Sci. Pract. 2019, 43, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Emilson, C.; Åsenlöf, P.; Pettersson, S.; Bergman, S.; Sandborgh, M.; Martin, C.; Demmelmaier, I. Physical Therapists’ Assessments, Analyses and Use of Behavior Change Techniques in Initial Consultations on Musculoskeletal Pain: Direct Observations in Primary Health Care. BMC Musculoskelet. Disord. 2016, 17, 316. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T. Implementing Change in Physiotherapy: Professions, Contexts and Interventions. J. Health Organ. Manag. 2014, 28, 96–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cowell, I.; McGregor, A.; O’Sullivan, P.; O’Sullivan, K.; Poyton, R.; Schoeb, V.; Murtagh, G. How do physiotherapists solicit and explore patients’ concerns in back pain consultations: A conversation analytic approach. Physiother Theory Pract. 2021, 37, 693–709. [Google Scholar] [CrossRef]
- Driver, C.; Kean, B.; Oprescu, F.; Lovell, G.P. Knowledge, Behaviors, Attitudes and Beliefs of Physiotherapists towards the Use of Psychological Interventions in Physiotherapy Practice: A Systematic Review. Disabil. Rehabil. 2017, 39, 2237–2249. [Google Scholar] [CrossRef]
- Synnott, A.; O’Keeffe, M.; Bunzli, S.; Dankaerts, W.; O’Sullivan, P.; Robinson, K.; O’Sullivan, K. Physiotherapists Report Improved Understanding of and Attitude toward the Cognitive, Psychological and Social Dimensions of Chronic Low Back Pain after Cognitive Functional Therapy Training: A Qualitative Study. J. Physiother. 2016, 62, 215–221. [Google Scholar] [CrossRef] [Green Version]
- O’Keeffe, M.; Cullinane, P.; Hurley, J.; Leahy, I.; Bunzli, S.; O’Sullivan, P.B.; O’Sullivan, K. What Influences Patient-Therapist Interactions in Musculoskeletal Physical Therapy? Qualitative Systematic Review and Meta-Synthesis. Phys. Ther. 2016, 96, 609–622. [Google Scholar] [CrossRef] [Green Version]
- Guerrero, A.V.S.; Maujean, A.; Campbell, L.; Sterling, M. A Systematic Review and Meta-Analysis of the Effectiveness of Psychological Interventions Delivered by Physiotherapists on Pain, Disability and Psychological Outcomes in Musculoskeletal Pain Conditions. Clin. J. Pain 2018, 34, 838–857. [Google Scholar] [CrossRef]
- Gardner, T.; Refshauge, K.; Smith, L.; McAuley, J.; Hübscher, M.; Goodall, S. Physiotherapists’ Beliefs and Attitudes Influence Clinical Practice in Chronic Low Back Pain: A Systematic Review of Quantitative and Qualitative Studies. J. Physiother. 2017, 63, 132–143. [Google Scholar] [CrossRef]
- Thompson, K.; Johnson, M.I.; Milligan, J.; Briggs, M. Rethinking Pain Education from the Perspectives of People Experiencing Pain: A Meta-Ethnography to Inform Physiotherapy Training. BMJ Open 2022, 12, e046363. [Google Scholar] [CrossRef] [PubMed]
- Bee, P.; McBeth, J.; MacFarlane, G.J.; Lovell, K. Managing Chronic Widespread Pain in Primary Care: A Qualitative Study of Patient Perspectives and Implications for Treatment Delivery. BMC Musculoskelet. Disord. 2016, 17, 354. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suman, A.; Bostick, G.P.; Schopflocher, D.; Russell, A.S.; Ferrari, R.; Battié, M.C.; Hu, R.; Buchbinder, R.; Gross, D.P. Long-Term Evaluation of a Canadian Back Pain Mass Media Campaign. Eur. Spine J. 2017, 26, 2467–2474. [Google Scholar] [CrossRef] [PubMed]
- Petit, A.; Begue, C.; Richard, I.; Roquelaure, Y. Factors Influencing Physiotherapists’ Attitudes and Beliefs toward Chronic Low Back Pain: Impact of a Care Network Belonging. Physiother. Theory Pract. 2019, 35, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Hall, A.; Richmond, H.; Bursey, K.; Hansen, Z.; Williamson, E.; Copsey, B.; Albury, C.; Asghari, S.; Curran, V.; Pike, A.; et al. Evaluating the Impact of a Champion on Implementation of the Back Skills Training (BeST) Programme in Canada: A Mixed Methods Feasibility Study Protocol. BMJ Open 2020, 10, e040834. [Google Scholar] [CrossRef] [PubMed]
- Thompson, K.; Johnson, M.I.; Milligan, J.; Briggs, M. Twenty-Five Years of Pain Education Research-What Have We Learned? Findings from a Comprehensive Scoping Review of Research into Pre-Registration Pain Education for Health Professionals. Pain 2018, 159, 2146–2158. [Google Scholar] [CrossRef]
| Themes Identified |
|---|
| Knowledge, Skills, and Attitudes |
| Confidence |
| Role clarity |
| Environmental context and resources |
| Patient expectations, beliefs and attitudes |
| Therapeutic alliance |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Dijk, H.; Köke, A.J.A.; Elbers, S.; Mollema, J.; Smeets, R.J.E.M.; Wittink, H. Physiotherapists Using the Biopsychosocial Model for Chronic Pain: Barriers and Facilitators—A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 1634. https://doi.org/10.3390/ijerph20021634
van Dijk H, Köke AJA, Elbers S, Mollema J, Smeets RJEM, Wittink H. Physiotherapists Using the Biopsychosocial Model for Chronic Pain: Barriers and Facilitators—A Scoping Review. International Journal of Environmental Research and Public Health. 2023; 20(2):1634. https://doi.org/10.3390/ijerph20021634
Chicago/Turabian Stylevan Dijk, Han, Albère J. A. Köke, Stefan Elbers, Jurgen Mollema, Rob J. E. M. Smeets, and Harriët Wittink. 2023. "Physiotherapists Using the Biopsychosocial Model for Chronic Pain: Barriers and Facilitators—A Scoping Review" International Journal of Environmental Research and Public Health 20, no. 2: 1634. https://doi.org/10.3390/ijerph20021634
APA Stylevan Dijk, H., Köke, A. J. A., Elbers, S., Mollema, J., Smeets, R. J. E. M., & Wittink, H. (2023). Physiotherapists Using the Biopsychosocial Model for Chronic Pain: Barriers and Facilitators—A Scoping Review. International Journal of Environmental Research and Public Health, 20(2), 1634. https://doi.org/10.3390/ijerph20021634





