Self-Myofascial Release of the Foot Plantar Surface: The Effects of a Single Exercise Session on the Posterior Muscular Chain Flexibility after One Hour
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
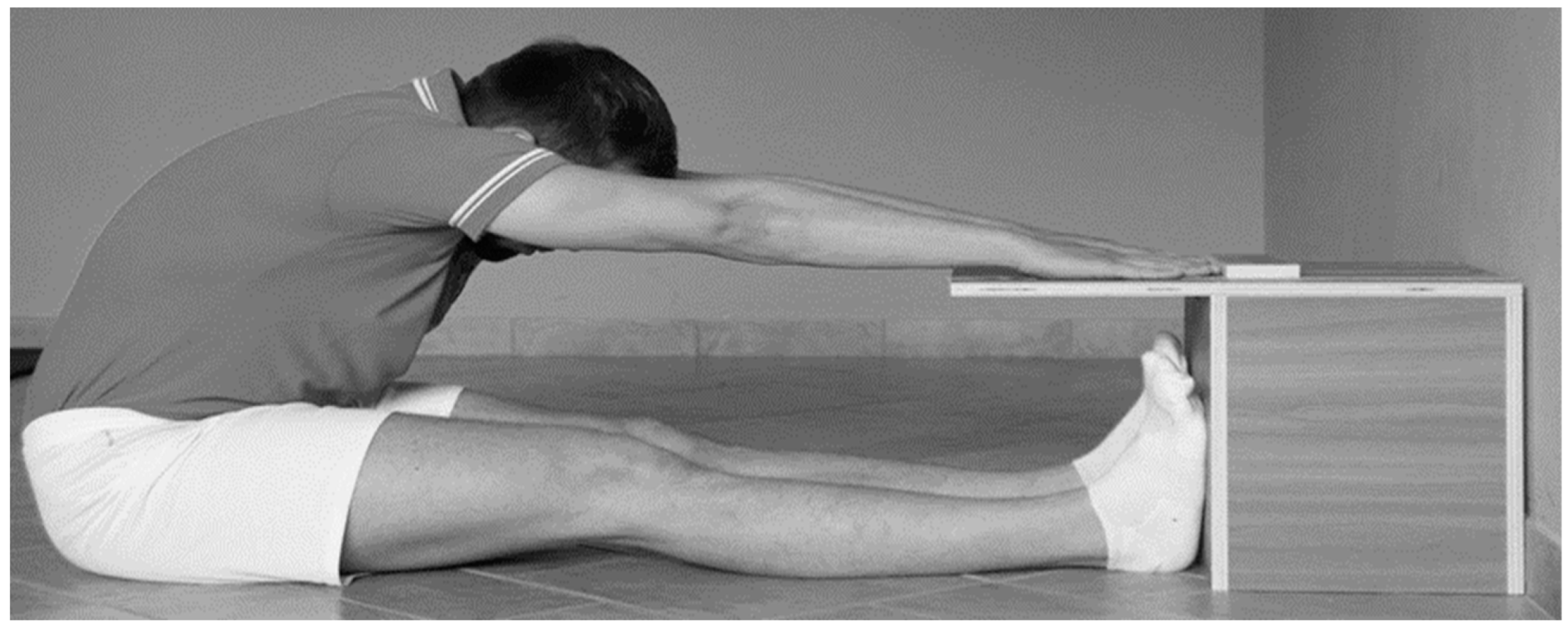
2.2. Instrumentation
2.3. Procedure and Data Collection
- T0: corresponding to the first S&R test carried out on the participants;
- T1: corresponding to the second S&R test on the participants immediately after the SMR technique;
- T2: corresponding to the third test of the S&R, carried out 30 min after T1;
- T3: corresponding the fourth test of the S&R, carried out 60 min after T1.
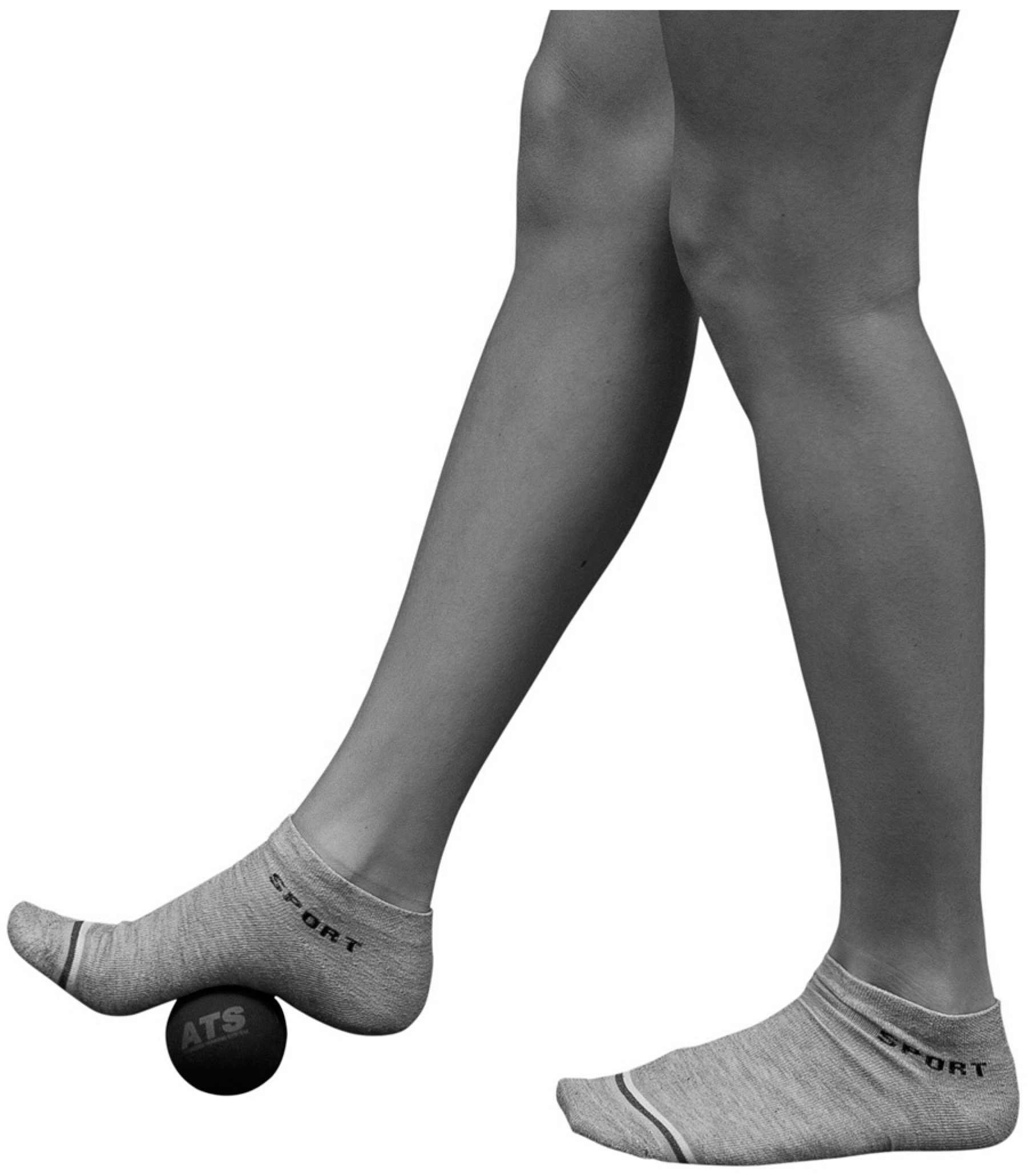
2.4. Intervention
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Posterior Muscular Chain Flexibility, Changes in the Whole Sample
4.2. Posterior Muscular Chain Flexibility, Changes for Subgroups
4.3. Musculoskeletal and Fascial Aspects
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Junker, D.; Stöggl, T. The Training Effects of Foam Rolling on Core Strength Endurance, Balance, Muscle Performance and Range of Motion: A Randomized Controlled Trial. J. Sports Sci. Med. 2019, 18, 229–238. [Google Scholar] [PubMed]
- Shariat, A.; Anastasio, A.T.; Soheili, S.; Rostad, M. Home-based fundamental approach to alleviate low back pain using myofascial release, stretching, and spinal musculature strengthening during the COVID-19 pandemic. Work 2020, 67, 11–19. [Google Scholar] [CrossRef]
- Shalamzari, M.H.; Minoonejad, H.; Seidi, F. The Effects of a Self-Myofascial Release Program on Isokinetic Hamstrings-to-Quadriceps Strength Ratio and Range of Motion of the Knee Joint Among Athletes With Hamstring Shortness. J. Sport Rehabil. 2022, 31, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Sulowska-Daszyk, I.; Skiba, A. The Influence of Self-Myofascial Release on Muscle Flexibility in Long-Distance Runners. Int. J. Environ. Res. Public Health 2022, 19, 457. [Google Scholar] [CrossRef] [PubMed]
- Russo, L.; Montagnani, E.; Buttari, D.; Ardigò, L.P.; Melenco, I.; Larion, A.; Migliaccio, G.M.; Padulo, J. Track Running Shoes: A Case Report of the Transition from Classical Spikes to “Super Spikes” in Track Running. Appl. Sci. 2022, 12, 10195. [Google Scholar] [CrossRef]
- Cheatham, S.W.; Stull, K.R. Knowledge of self-myofascial release among allied health students in the United States: A descriptive survey. J. Bodyw. Mov. Ther. 2018, 22, 713–717. [Google Scholar] [CrossRef]
- Ughreja, R.A.; Venkatesan, P.; Balebail Gopalakrishna, D.; Singh, Y.P. Effectiveness of myofascial release on pain, sleep, and quality of life in patients with fibromyalgia syndrome: A systematic review. Complement. Ther. Clin. Pract. 2021, 45, 101477. [Google Scholar] [CrossRef]
- López-Torres, O.; Mon-López, D.; Gomis-Marzá, C.; Lorenzo, J.; Guadalupe-Grau, A. Effects of myofascial release or self-myofascial release and control position exercises on lower back pain in idiopathic scoliosis: A systematic review. J. Bodyw. Mov. Ther. 2021, 27, 16–25. [Google Scholar] [CrossRef]
- Beardsley, C.; Škarabot, J. Effects of self-myofascial release: A systematic review. J. Bodyw. Mov. Ther. 2015, 19, 747–758. [Google Scholar] [CrossRef]
- Kalichman, L.; Ben David, C. Effect of self-myofascial release on myofascial pain, muscle flexibility, and strength: A narrative review. J. Bodyw. Mov. Ther. 2017, 21, 446–451. [Google Scholar] [CrossRef]
- McKenney, K.; Elder, A.S.; Elder, C.; Hutchins, A. Myofascial release as a treatment for orthopaedic conditions: A systematic review. J. Athl. Train. 2013, 48, 522–527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaitow, L. Research in water and fascia. Micro-tornadoes, hydrogenated diamonds and nanocrystals. Massage Today 2009, 9, 1–3. [Google Scholar]
- Aguilera, F.J.; Martin, D.P.; Masanet, R.A.; Botella, A.C.; Soler, L.B.; Morell, F.B. Immediate effect of ultrasound and ischemic compression techniques for the treatment of trapezius latent myofascial trigger points in healthy subjects: A randomized controlled study. J. Manip. Physiol. Ther. 2009, 32, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Lavelle, E.D.; Lavelle, W.; Smith, H.S. Myofascial trigger points. Anesthesiol. Clin. 2007, 25, 841–851. [Google Scholar] [CrossRef]
- Montañez-Aguilera, F.J.; Valtueña-Gimeno, N.; Pecos-Martín, D.; Arnau-Masanet, R.; Barrios-Pitarque, C.; Bosch-Morell, F. Changes in a patient with neck pain after application of ischemic compression as a trigger point therapy. J. Back Musculoskelet. Rehabil. 2010, 23, 101–104. [Google Scholar] [CrossRef]
- MacDonald, G.Z.; Penney, M.D.; Mullaley, M.E.; Cuconato, A.L.; Drake, C.D.; Behm, D.G.; Button, D.C. An acute bout of self-myofascial release increases range of motion without a subsequent decrease in muscle activation or force. J. Strength Cond. Res. 2013, 27, 812–821. [Google Scholar] [CrossRef] [Green Version]
- Schleip, R.; Müller, D.G. Training principles for fascial connective tissues: Scientific foundation and suggested practical applications. J. Bodyw. Mov. Ther. 2013, 17, 103–115. [Google Scholar] [CrossRef]
- Behm, D.G.; Wilke, J. Do Self-Myofascial Release Devices Release Myofascia? Rolling Mechanisms: A Narrative Review. Sports Med. 2019, 49, 1173–1181. [Google Scholar] [CrossRef]
- Cornell, D.J.; Ebersole, K.T. Influence of an acute bout of self-myofascial release on knee extension force output and electro-mechanical activation of the quadriceps. Int. J. Sports Phys. Ther. 2020, 15, 732–743. [Google Scholar] [CrossRef]
- Ferreira, R.M.; Martins, P.N.; Goncalves, R.S. Effects of Self-myofascial Release Instruments on Performance and Recovery: An Umbrella Review. Int. J. Exerc. Sci. 2022, 15, 861–883. [Google Scholar]
- Russo, L.; Palermi, S.; Dhahbi, W.; Kalinski, S.D.; Bragazzi, N.L.; Padulo, J. Selected components of physical fitness in rhythmic and artistic youth gymnast. Sport Sci. Health 2021, 17, 415–421. [Google Scholar] [CrossRef]
- Maniar, N.; Shield, A.J.; Williams, M.D.; Timmins, R.G.; Opar, D.A. Hamstring strength and flexibility after hamstring strain injury: A systematic review and meta-analysis. Br. J. Sports Med. 2016, 50, 909–920. [Google Scholar] [CrossRef] [PubMed]
- Sadler, S.G.; Spink, M.J.; Ho, A.; de Jonge, X.J.; Chuter, V.H. Restriction in lateral bending range of motion, lumbar lordosis, and hamstring flexibility predicts the development of low back pain: A systematic review of prospective cohort studies. BMC Musculoskelet. Disord. 2017, 18, 179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hori, M.; Hasegawa, H.; Takasaki, H. Comparisons of hamstring flexibility between individuals with and without low back pain: Systematic review with meta-analysis. Physiother. Theory Pract. 2021, 37, 559–582. [Google Scholar] [CrossRef] [PubMed]
- Thomas, E.; Bianco, A.; Paoli, A.; Palma, A. The Relation Between Stretching Typology and Stretching Duration: The Effects on Range of Motion. Int. J. Sports Med. 2018, 39, 243–254. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Trama, R.; Fouré, A.; Hautier, C.A. The Immediate Effects of Self-Myofacial Release on Flexibility, Jump Performance and Dynamic Balance Ability. J. Hum. Kinet. 2020, 75, 139–148. [Google Scholar] [CrossRef]
- Kasahara, K.; Konrad, A.; Yoshida, R.; Murakami, Y.; Sato, S.; Aizawa, K.; Koizumi, R.; Thomas, E.; Nakamura, M. Comparison between 6-week foam rolling intervention program with and without vibration on rolling and non-rolling sides. Eur. J. Appl. Physiol. 2022, 122, 2061–2070. [Google Scholar] [CrossRef]
- Beier, Z.; Earp, I.; Korak, J.A. Self-Myofascial Release Does Not Improve Back Squat Range of Motion, Alter Muscle Activation, or Aid in Perceived Recovery 24-Hours Following Lower Body Resistance Training. Int. J. Exerc. Sci. 2019, 12, 839–846. [Google Scholar]
- Grieve, R.; Goodwin, F.; Alfaki, M.; Bourton, A.J.; Jeffries, C.; Scott, H. The immediate effect of bilateral self myofascial release on the plantar surface of the feet on hamstring and lumbar spine flexibility: A pilot randomised controlled trial. J. Bodyw. Mov. Ther. 2015, 19, 544–552. [Google Scholar] [CrossRef]
- Williams, W.; Selkow, N.M. Self-Myofascial Release of the Superficial Back Line Improves Sit-and-Reach Distance. J. Sport Rehabil. 2019, 29, 400–404. [Google Scholar] [CrossRef]
- Fauris, P.; López-de-Celis, C.; Canet-Vintró, M.; Martin, J.C.; Llurda-Almuzara, L.; Rodríguez-Sanz, J.; Labata-Lezaun, N.; Simon, M.; Pérez-Bellmunt, A. Does Self-Myofascial Release Cause a Remote Hamstring Stretching Effect Based on Myofascial Chains? A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 12356. [Google Scholar] [CrossRef] [PubMed]
- Prabu Raja, G.; Shyamasunder Bhat, N.; Marie Cruz, A.; Prabhu, A.; Fernandes, S.; Naaz, N. The anatomical myofascial continuum between the neck and eyes. Clin. Anat. 2022, 35, 340–346. [Google Scholar] [CrossRef]
- Hamaoui, A.; le Bozec, S.; Poupard, L.; Bouisset, S. Does postural chain muscular stiffness reduce postural steadiness in a sitting posture? Gait Posture 2007, 25, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Russo, L.; Giustino, V.; Toscano, R.E.; Secolo, G.; Secolo, I.; Iovane, A.; Messina, G. Can tongue position and cervical ROM affect postural oscillations? A pilot and preliminary study. J. Hum. Sport Exerc. 2020, 15, S840–S847. [Google Scholar] [CrossRef]
- Halperin, I.; Aboodarda, S.J.; Button, D.C.; Andersen, L.L.; Behm, D.G. Roller massager improves range of motion of plantar flexor muscles without subsequent decreases in force parameters. Int. J. Sports Phys. Ther. 2014, 9, 92–102. [Google Scholar] [PubMed]
- Jay, K.; Sundstrup, E.; Søndergaard, S.D.; Behm, D.; Brandt, M.; Særvoll, C.A.; Jakobsen, M.D.; Andersen, L.L. Specific and cross over effects of massage for muscle soreness: Randomized controlled trial. Int. J. Sports Phys. Ther. 2014, 9, 82–91. [Google Scholar] [PubMed]
- Liemohn, W.; Sharpe, G.L.; Wasserman, J.F. Criterion related validity of the sit-and-reach test. J. Strength Cond Res. 1994, 8, 91–94. [Google Scholar] [CrossRef]
- Russo, L.; Benis, R.; Livi, S.; Falcone, A.; Ragalmuto, N.; Bartolucci, P.; Barni, L. Esercizio Correttivo® Postura Salute Perfomance; ATS—Giacomo Catalani Editore: Arezzo, Italy, 2016; p. 226. [Google Scholar]
- Russo, L.; Di Capua, R.; Arnone, B.; Borrelli, M.; Coppola, R.; Esposito, F.; Padulo, J. Shoes and Insoles: The Influence on Motor Tasks Related to Walking Gait Variability and Stability. Int. J. Environ. Res. Public Health 2020, 17, 4569. [Google Scholar] [CrossRef]
- Ardigò, L.P.; Buglione, A.; Russo, L.; Cular, D.; Esposito, F.; Doria, C.; Padulo, J. Marathon shoes vs. track spikes: A crossover pilot study on metabolic demand at different speeds in experienced runners. Res. Sports Med. 2021, 1–8. [Google Scholar] [CrossRef]
- Atkinson, G.; Reilly, T. Circadian variation in sports performance. Sports Med. 1996, 21, 292–312. [Google Scholar] [CrossRef]
- Mayorga-Vega, D.; Merino-Marban, R.; Viciana, J. Criterion-Related Validity of Sit-and-Reach Tests for Estimating Hamstring and Lumbar Extensibility: A Meta-Analysis. J. Sports Sci. Med. 2014, 13, 1–14. [Google Scholar] [PubMed]
- Lemmink, K.A.P.M.; Greef, M.H.G.; Rispens, P.; Kemper, H.C.G.; Stevens, M. The validity of the sit-and-reach test and the modified sit-and-reach test in middle-aged to older men and women. Res. Q. Exerc. Sport 2003, 74, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Kaminsky, L.A.; Bonzheim, K.A. American College of Sports Medicine (ACSM) Resource Manual for Guidelines for Exercise Testing and Prescription, 5th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006. [Google Scholar]
- Gonzalez-Suarez, C.B.; Caralipio, N.; Gambito, E.; Reyes, J.J.; Espino, R.V.; Macatangay, R. The association of physical fitness with body mass index and waist circumference in Filipino preadolescents. Asia Pac. J. Public Health 2013, 25, 74–83. [Google Scholar] [CrossRef]
- Joshi, D.G.; Balthillaya, G.; Prabhu, A. Effect of remote myofascial release on hamstring flexibility in asymptomatic individuals—A randomized clinical trial. J. Bodyw. Mov. Ther. 2018, 22, 832–837. [Google Scholar] [CrossRef]
- Wilke, J.; Kalo, K.; Niederer, D.; Vogt, L.; Banzer, W. Gathering Hints for Myofascial Force Transmission under In Vivo Conditions: Are Remote Exercise Effects Age Dependent? J. Sport Rehabil. 2019, 28, 758–763. [Google Scholar] [CrossRef]
- Štefan, L.; Kasović, M.; Culej, M. Normative Values for Health-Related Physical Fitness in First-Year Police Officers. J. Strength Cond. Res. 2022, 36, 2530–2535. [Google Scholar] [CrossRef]
- Wilke, J.; Krause, F.; Vogt, L.; Banzer, W. What Is Evidence-Based About Myofascial Chains: A Systematic Review. Arch. Phys. Med. Rehabil. 2016, 97, 454–461. [Google Scholar] [CrossRef]
- Krause, F.; Wilke, J.; Vogt, L.; Banzer, W. Intermuscular force transmission along myofascial chains: A systematic review. J. Anat. 2016, 228, 910–918. [Google Scholar] [CrossRef]
- Gabriel, A.; Konrad, A.; Roidl, A.; Queisser, J.; Schleip, R.; Horstmann, T.; Pohl, T. Myofascial Treatment Techniques on the Plantar Surface Influence Functional Performance in the Dorsal Kinetic Chain. J. Sports Sci. Med. 2022, 21, 13–22. [Google Scholar] [CrossRef]
- Seiler, S. What is best practice for training intensity and duration distribution in endurance athletes? Int. J. Sports Physiol. Perform 2010, 5, 276–291. [Google Scholar] [CrossRef]
- La Greca, S.; Rapali, M.; Ciaprini, G.; Russo, L.; Vinciguerra, M.G.; Di Giminiani, R. Acute and Chronic Effects of Supervised Flexibility Training in Older Adults: A Comparison of Two Different Conditioning Programs. Int. J. Environ. Res. Public Health 2022, 19, 16974. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.M. Running economy is negatively related to sit-and-reach test performance in international-standard distance runners. Int. J. Sports Med. 2022, 23, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Trehearn, T.L.; Buresh, R.J. Sit-and-reach flexibility and running economy of men and women collegiate distance runners. J. Strength Cond. Res. 2009, 23, 158–162. [Google Scholar] [CrossRef]
- Hunter, G.R.; Katsoulis, K.; McCarthy, J.P.; Ogard, W.K.; Bamman, M.M.; Wood, D.S.; Den Hollander, J.A.; Blaudeau, T.E.; Newcomer, B.R. Tendon length and joint flexibility are related to running economy. Med. Sci. Sports Exerc. 2011, 43, 1492–1499. [Google Scholar] [CrossRef] [PubMed]
- Stroiney, D.A.; Herrick, S.L.; Paolone, V.J.; Matthews, T.D. The Effects of an Acute Bout of Self-Myofascial Release on the Physiological Parameters of Running. Int. J. Exerc. Sci. 2020, 13, 113–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giovanelli, N.; Vaccari, F.; Floreani, M.; Rejc, E.; Copetti, J.; Garra, M.; Biasutti, L.; Lazzer, S. Short-Term Effects of Rolling Massage on Energy Cost of Running and Power of the Lower Limbs. Int. J. Sports Physiol. Perform. 2018, 13, 1337–1343. [Google Scholar] [CrossRef]
- Höög, S.; Andersson, E.P. Sex and Age-Group Differences in Strength, Jump, Speed, Flexibility, and Endurance Performances of Swedish Elite Gymnasts Competing in TeamGym. Front. Sports Act. Living 2021, 3, 653503. [Google Scholar] [CrossRef]
- Lopes, T.J.A.; Simic, M.; Alves, D.S.; Bunn, P.D.S.; Rodrigues, A.I.; Terra, B.S.; Lima, M.D.S.; Ribeiro, F.M.; Vilão, P.; Pappas, E. Physical Performance Measures of Flexibility, Hip Strength, Lower Limb Power, and Trunk Endurance in Healthy Navy Cadets: Normative Data and Differences Between Sex and Limb Dominance. J. Strength Cond. Res. 2021, 35, 458–464. [Google Scholar] [CrossRef]
- Phillips, J.; Diggin, D.; King, D.L.; Sforzo, G.A. Effect of Varying Self-myofascial Release Duration on Subsequent Athletic Performance. J. Strength Cond. Res. 2021, 35, 746–753. [Google Scholar] [CrossRef]
- Agopyan, A.; Tekin, D.; Unal, M.; Kurtel, H.; Turan, G.; Ersoz, A. Acute effects of static stretching on isokinetic thigh strength on modern dancers. J. Sports Med. Phys. Fitness 2013, 53, 538–550. [Google Scholar]
- Pavan, P.G.; Stecco, A.; Stern, R.; Stecco, C. Painful connections: Densification versus fibrosis of fascia. Curr. Pain Headache Rep. 2014, 18, 441. [Google Scholar] [CrossRef]
- Stecco, C.; Porzionato, A.; Macchi, V.; Tiengo, C.; Parenti, A.; Aldegheri, R.; Delmas, V.; De Caro, R. Histological characteristics of the deep fascia of the upper limb. Ital. J. Anat. Embryol. 2006, 111, 105–110. [Google Scholar] [PubMed]
- Stecco, C.; Gagey, O.; Belloni, A.; Pozzuoli, A.; Porzionato, A.; Macchi, V.; Aldegheri, R.; De Caro, R.; Delmas, V. Anatomy of the deep fascia of the upper limb. Second part: Study of innervation. Morphologie 2007, 91, 38–43. [Google Scholar] [CrossRef]
- Stecco, C.; Porzionato, A.; Lancerotto, L.; Stecco, A.; Macchi, V.; Day, J.A.; De Caro, R. Histological study of the deep fasciae of the limbs. J. Bodyw. Mov. Ther. 2008, 12, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Stecco, A.; Gesi, M.; Stecco, C.; Stern, R. Fascial components of the myofascial pain syndrome. Curr. Pain Headache Rep. 2013, 17, 352. [Google Scholar] [CrossRef]



| S&R (cm) | |||||||
|---|---|---|---|---|---|---|---|
| Group (n) | T0 | T1 | T2 | T3 | F | η2 | p Value |
| Entire sample (36) | 4.3 ± 8.7 | 5.7 ± 9.1 * | 6.4 ± 8.4 * | 7.0 ± 8.7 *# | 9.374 | 0.460 | 0.000 |
| Males (17) | 0.5 ± 9.3 | 1.4 ± 9.7 | 2.4 ± 8.8 | 2.6 ± 9.4 | 1.975 | 0.297 | 0.164 |
| Females (19) | 7.7 ± 6.6 | 9.5 ± 6.5 * | 10.1 ± 6.1 * | 11.0 ± 5.8 *# | 10.457 | 0.662 | 0.000 |
| FG (10) | 13.7 ± 2.7 | 14.6 ± 3.4 | 14.5 ± 4.4 | 15.5 ± 4.1 | 1.198 | 0.339 | 0.378 |
| AG (15) | 5.9 ± 3.6 | 8.1 ± 4.1 * | 8.6 ± 4.3 * | 9.0 ± 4.7 * | 8.838 | 0.688 | 0.002 |
| SG (11) | −6.5 ± 4.3 | −5.8 ± 4.5 | −3.8 ± 3.9 *# | −3.4 ± 4.6 | 4.992 | 0.649 | 0.032 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Russo, L.; Montagnani, E.; Pietrantuono, D.; D’Angona, F.; Fratini, T.; Di Giminiani, R.; Palermi, S.; Ceccarini, F.; Migliaccio, G.M.; Lupu, E.; et al. Self-Myofascial Release of the Foot Plantar Surface: The Effects of a Single Exercise Session on the Posterior Muscular Chain Flexibility after One Hour. Int. J. Environ. Res. Public Health 2023, 20, 974. https://doi.org/10.3390/ijerph20020974
Russo L, Montagnani E, Pietrantuono D, D’Angona F, Fratini T, Di Giminiani R, Palermi S, Ceccarini F, Migliaccio GM, Lupu E, et al. Self-Myofascial Release of the Foot Plantar Surface: The Effects of a Single Exercise Session on the Posterior Muscular Chain Flexibility after One Hour. International Journal of Environmental Research and Public Health. 2023; 20(2):974. https://doi.org/10.3390/ijerph20020974
Chicago/Turabian StyleRusso, Luca, Eleonora Montagnani, Davide Pietrantuono, Fabiola D’Angona, Tommaso Fratini, Riccardo Di Giminiani, Stefano Palermi, Francesco Ceccarini, Gian Mario Migliaccio, Elena Lupu, and et al. 2023. "Self-Myofascial Release of the Foot Plantar Surface: The Effects of a Single Exercise Session on the Posterior Muscular Chain Flexibility after One Hour" International Journal of Environmental Research and Public Health 20, no. 2: 974. https://doi.org/10.3390/ijerph20020974
APA StyleRusso, L., Montagnani, E., Pietrantuono, D., D’Angona, F., Fratini, T., Di Giminiani, R., Palermi, S., Ceccarini, F., Migliaccio, G. M., Lupu, E., & Padulo, J. (2023). Self-Myofascial Release of the Foot Plantar Surface: The Effects of a Single Exercise Session on the Posterior Muscular Chain Flexibility after One Hour. International Journal of Environmental Research and Public Health, 20(2), 974. https://doi.org/10.3390/ijerph20020974












