Dr. Google: Physicians—The Web—Patients Triangle: Digital Skills and Attitudes towards e-Health Solutions among Physicians in South Eastern Poland—A Cross-Sectional Study in a Pre-COVID-19 Era
Abstract
:1. Introduction
2. Theoretical Background and Literature Review
2.1. Physicians’ Attitude and Acceptance of e-Health
2.2. Research Questions
- Q.1 How do physicians evaluate their digital skills and digital literacy, and what variables determine this?
- Q.2. How do physicians perceive the quality and usefulness of online health information for their patients, and what variables determine this?
- Q.3. How do physicians evaluate e-health solutions in general, and what variables determine this?
- Q.4. Do physicians recommend e-health solutions to their patients, and what variables determine this?
3. Materials and Methods
3.1. Study Design
3.2. Questionnaires
- “Digital Literacy” section on self-assessment of the ability to use digital devices and solutions, and evaluation the frequency of using digital devices and solutions in private and professional life (smartphone, computer, e-mail, mobile applications, and tablet);
- “The impact of the Internet/new technologies on healthcare and modern life” section concerning the general assessment and opinion on the use of the search engine/Internet in the context of health;
- “Recommendation of e-Health solutions” section containing statements regarding the present/future recommending or not recommending e-health solutions to the patients,
- “Evaluation of e-Health solutions” section with self-assessment of the relevance of the proposed e-health solutions;
3.3. Ethics
3.4. Data Analysis
4. Results
4.1. The Reliability and Validity of Questionnaires
- Digital literacy: the Cronbach’s alpha: 0.571, PCA: two components (“Own skills”, and “Need for training”), explaining 61.6% of the variance;
- The impact of the Internet/new technologies on healthcare and modern life: the Cronbach’s alpha: 0.462, PCA: one variable explaining 65.0% of the variance;
- Recommendation of e-health solutions: the Cronbach’s alpha: 0.865, PCA: one component explaining 52.1% of the variance;
- Evaluation of e-health solutions: the Cronbach’s alpha: 0.928, PCA: two components (“Patients” and “Medical facility”), explaining 69.0% of the variance.
4.2. Characteristics of the Study Group
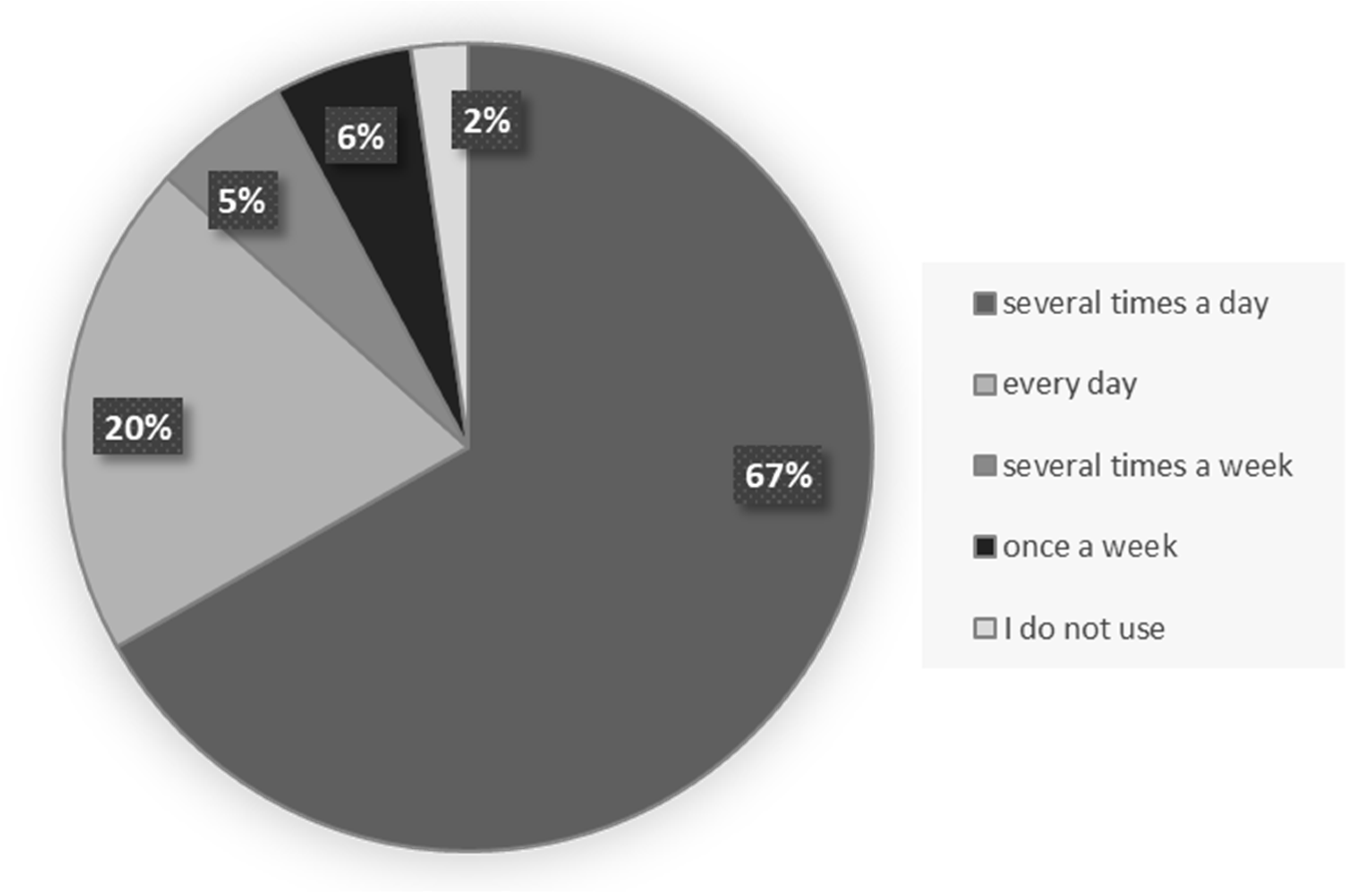
4.3. Physicians’ Digital Literacy and e-Health Indicators
4.4. Physicians’ Opinion about Online Health Information (Dr. Google)
4.5. Dr. Google and Physicians’ Digital Literacy Indicators
4.6. Recommendation of e-Health Solutions
4.7. Evaluation of e-Health Solutions
4.8. Correlation Matrix of All Digital Indicators
5. Discussion
6. Conclusions
7. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Digital 2022. Global Overview Report. Hootsuite, We Are Social. Available online: https://www.hootsuite.com/resources/digital-trends (accessed on 26 September 2022).
- Wald, H.; Dube, C.; Anthony, D. Untangling the Web: The impact of Internet use on health care and the physician–patient relationship. Patient Educ. Couns. 2007, 68, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Huisman, M.; Joye, S.; Biltereyst, D. Searching for Health: Doctor Google and the Shifting Dynamics of the Middle-Aged and Older Adult Patient–Physician Relationship and Interaction. J. Aging Health 2020, 32, 998–1007. [Google Scholar] [CrossRef]
- Davis, J.K. Dr. Google and Premature Consent: Patients Who Trust the Internet More Than They Trust Their Provider. HEC Forum 2018, 30, 253–265. [Google Scholar] [CrossRef] [PubMed]
- Sbaffi, L.; Rowley, J. Trust and Credibility in Web-Based Health Information: A Review and Agenda for Future Research. J. Med. Internet Res. 2017, 19, e218. [Google Scholar] [CrossRef] [PubMed]
- Pitt, M.B.; Hendrickson, M.A. Providing a Second Opinion to Dr. Google with the WWW Framework. J. Gen. Intern. Med. 2022, 37, 222–224. [Google Scholar] [CrossRef]
- Cacciamani, G.E.; Dell’Oglio, P.; Cocci, A.; Russo, G.I.; De Castro Abreu, A.; Gill, I.S.; Briganti, A.; Artibani, W. Asking “Dr. Google” for a Second Opinion: The Devil Is in the Details. Eur. Urol. Focus 2021, 7, 479–481. [Google Scholar] [CrossRef] [Green Version]
- Van Riel, N.; Auwerx, K.; Debbaut, P.; Van Hees, S.; Schoenmakers, B. The effect of Dr Google on doctor-patient encounters in primary care: A quantitative, observational, cross-sectional study. BJGP Open 2017, 1, bjgpopen17X100833. [Google Scholar] [CrossRef]
- Tustin, N. The role of patient satisfaction in online health information seeking. J. Health Commun. 2010, 15, 3–17. [Google Scholar] [CrossRef]
- Chambers, D.; Cantrell, A.J.; Johnson, M.; Preston, L.; Baxter, S.K.; Booth, A.; Turner, J. Digital and online symptom checkers and health assessment/triage services for urgent health problems: Systematic review. BMJ Open 2019, 9, e027743. [Google Scholar] [CrossRef] [Green Version]
- Fox, S.; Duggan, M.; Pew Research Center. Health Online. 2013. Available online: https://www.pewinternet.org/wp-content/uploads/sites/9/media/Files/Reports/PIP_HealthOnline.pdf (accessed on 26 September 2022).
- Attfield, S.J.; Adams, A.; Blandford, A. Patient information needs: Pre- and post-consultation. Health Informatics J. 2006, 12, 165–177. [Google Scholar] [CrossRef]
- Murray, E.; Lo, B.; Pollack, L.; Donelan, K.; Catania, J.; White, M.; Turner, R. The impact of health information on the internet on the physician-patient relationship: Patient perceptions. Arch. Intern. Med. 2003, 163, 1727–1734. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, K.; Hoti, K.; Hughes, J.D.; Emmerton, L. Dr Google Is Here to Stay but Health Care Professionals Are Still Valued: An Analysis of Health Care Consumers’ Internet Navigation Support Preferences. J. Med. Internet Res. 2017, 19, e210. [Google Scholar] [CrossRef]
- Giunti, G.; Guisado-Fernandez, E.; Belani, H.; Lacalle-Remigio, J.R. Mapping the Access of Future Doctors to Health Information Technologies Training in the European Union: Cross-Sectional Descriptive Study. J. Med. Internet Res. 2019, 21, e14086. [Google Scholar] [CrossRef] [PubMed]
- NHS. Preparing the Healthcare Workforce to Deliver the Digital Future. 2018. Available online: https://topol.hee.nhs.uk/wp-content/uploads/HEE-Topol-Review-2019.pdf (accessed on 20 November 2022).
- Woodward-Kron, R.; Connor, M.; Schulz, P.J.; Elliott, K. Educating the Patient for Health Care Communication in the Age of the World Wide Web: A Qualitative Study. Acad. Med. 2014, 89, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Powell, J.; Inglis, N.; Ronnie, J.; Large, S. The Characteristics and Motivations of Online Health Information Seekers: Cross-Sectional Survey and Qualitative Interview Study. J. Med. Internet Res. 2011, 13, e20. [Google Scholar] [CrossRef] [PubMed]
- Caiata-Zufferey, M.; Abraham, A.; Sommerhalder, K.; Schulz, P.J. Online health information seeking in the context of the medical consultation in Switzerland. Qual. Health Res. 2010, 20, 1050–1061. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.J.; Longo, D.L. The Precision of Evidence Needed to Practice. N Engl. J. Med. 2019, 380, 2472–2474. [Google Scholar] [CrossRef]
- Mesko, B.; Győrffy, Z. The Rise of the Empowered Physician in the Digital Health Era: Viewpoint. J. Med. Internet Res. 2019, 21, e12490. [Google Scholar] [CrossRef]
- Bates, D.W.; Cohen, M.; Leape, L.L.; Overhage, J.M.; Shabot, M.M.; Sheridan, T. Reducing the frequency of errors in medicine using information technology. J. Am. Med. Inform. Assoc. 2001, 8, 299–308. [Google Scholar] [CrossRef] [Green Version]
- Elbert, N.J.; van Os-Medendorp, H.; van Renselaar, W.; Ekeland, A.G.; Hakkaart-van Roijen, L.; Raat, H.; Nijsten, T.E.; Pasmans, S.G. Effectiveness and cost-effectiveness of ehealth interventions in somatic diseases: A systematic review of systematic reviews and meta-analyses. J. Med. Internet Res. 2014, 16, e110. [Google Scholar] [CrossRef]
- European Commission. European Skills Agenda for Sustainable Competitiveness, Social Fairness and Resilience. 2020. Available online: https://www.europarl.europa.eu/doceo/document/TA-9-2021-0051_EN.html (accessed on 26 September 2022).
- CPME Policy on Digital Competencies for Doctors’ (CPME 2020/100 FINAL). 2020. Available online: https://www.cpme.eu/api/documents/adopted/2020/11/CPME_AD_Board_21112020_100.FINAL_.CPME_.Policy.Digital.Competencies.for_.Doctors.pdf (accessed on 26 September 2022).
- European Commission. Flash Eurobarometer 404 (European Citizens’ Digital Health Literacy), Genesis Data Archive 2015, v.1. Available online: http://ec.europa.eu/commfrontoffice/publicopinion/flash/fl_404_sum_en.pdf (accessed on 26 September 2022).
- Bawden, D. Information and digital literacies: A review of concepts. J. Doc. 2001, 57, 218–259. [Google Scholar] [CrossRef] [Green Version]
- European Commission. e-Health—Making Healthcare Better for European Citizens: An Action Plan for a European e-Health Area. 2004. Available online: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=COM:2004:0356:FIN:EN:PDF (accessed on 10 November 2022).
- Global Health Survey. Experiences & Perceptions in 28 Countries. International Research Institudes. 2011. Available online: https://www.arc.com.pl/download.php?id=2 (accessed on 10 November 2022).
- Kummervold, P.E.; Chronaki, C.; Lausen, B.; Prokosch, H.-U.; Rasmussen, J.; Santana, S.; Staniszewski, A.; Wangberg, S. eHealth Trends in Europe 2005-2007: A Population-Based Survey. J. Med. Internet Res. 2008, 10, e42. [Google Scholar] [CrossRef] [PubMed]
- Czerwińska, M. Postawy wobec e-zdrowia i opinie na jego temat w grupie studentów kierunku zdrowie publiczne. Rocz. Kol. Anal. Ekon. 2013, 29, 539–551. [Google Scholar]
- Borek, E.; Greser, J.; Kilijanek-Cieślik, A.; Perendyk, T.; Pruszko, A.; Sitek, A.; Wojtaszczyk, K. e-Zdrowie. Czego Oczekują Pacjenci; Fundacja My Pacjenci: Warszawa, Poland, 2017. [Google Scholar]
- Ajami, S.; Ketabi, S.; Saghaeiannejad, S.; Heidari, A. Requirements and areas associated with readiness assessment of electronic health records implementation. J. Health Admin. 2011, 14, 71–78. [Google Scholar]
- Dikomitis, L.; Green, T.; Macleod, U. Embedding electronic decision-support tools for suspected cancer in primary care: A qualitative study of GPs’ experiences. Prim. Health Care Res. Dev. 2015, 16, 548–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brooks, E.; Turvey, C.; Augusterfer, E. Provider barriers to telemental health: Obstacles overcome, obstacles remaining. Telemed. J. eHealth. 2013, 19, 433–437. [Google Scholar] [CrossRef] [PubMed]
- de Grood, C.; Raissi, A.; Kwon, Y.; Santana, M.J. Adoption of e-health technology by physicians: A scoping review. J. Multidiscip. Healthc. 2016, 9, 335–344. [Google Scholar] [CrossRef] [Green Version]
- Vedel, I.; Lapointe, L.; Lussier, M.-T.; Richard, C.; Goudreau, J.; Lalonde, L.; Turcotte, A. Healthcare professionals’ adoption and use of a clinical information system (CIS) in primary care: Insights from the Da Vinci study. Int. J. Med. Inform. 2012, 81, 73–87. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Hsiao, J. An investigation on physicians’ acceptance of hospital information systems: A case study. Int. J. Med. Inform. 2012, 81, 810–820. [Google Scholar] [CrossRef]
- Dunnebeil, S.; Sunyaev, A.; Blohm, I.; Leimeister, J.M.; Krcmar, H. Determinants of physicians’ technology acceptance for e-health in ambulatory care. Int. J. Med. Inform. 2012, 81, 746–760. [Google Scholar] [CrossRef] [Green Version]
- Legris, P.; John, I.; Pierre, C. Why do people use information technology? A critical review of the technology acceptance model. Inf. Manag. 2003, 40, 191–204. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. Manag. Inf. Syst. Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Portz, J.D.; Bayliss, E.A.; Bull, S.; Boxer, R.S.; Bekelman, D.B.; Gleason, K.; Czaja, S. Using the Technology Acceptance Model to Explore User Experience, Intent to Use, and Use Behavior of a Patient Portal Among Older Adults With Multiple Chronic Conditions: Descriptive Qualitative Study. J. Med. Internet Res. 2019, 21, e11604. [Google Scholar] [CrossRef]
- Scott, P.J.; de Keizer, N.; Georgiou, A. (Eds.) Applied interdisciplinary theory in health informatics: A knowledge base for practitioners. In Studies in Health Technology and Informatics; IOS Press: Amsterdam, The Netherlands, 2019; Volume 263. [Google Scholar]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User acceptance of information technology: Toward a unified view. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef] [Green Version]
- Parlakkılıç, A. Evaluation of Physicians’ Information Technology Readiness. Eurasian J. Fam. Med. 2020, 9, 170–175. [Google Scholar] [CrossRef]
- Yarbrough, A.K.; Smith, T.B. Technology acceptance among physicians: A new take on TAM. Med. Care Res. Rev. 2007, 64, 650–672. [Google Scholar] [CrossRef]
- Główny Urząd Statystyczny. Oddział Rzeszów. Mniej Lekarzy, Więcej Pielęgniarek. 2019. Available online: https://rzeszow.stat.gov.pl/dla-mediow/informacje-prasowe/mniej-lekarzy-wiecej-pielegniarek,220,1.html (accessed on 19 December 2022).
- Bartosiewicz, A.; Burzyńska, J.; Januszewicz, P. Polish Nurses’ Attitude to e-Health Solutions and Self-Assessment of Their IT Competence. J. Clin. Med. 2021, 10, 4799. [Google Scholar] [CrossRef] [PubMed]
- Zdrowa Przyszłość. Ramy Strategiczne Rozwoju Systemu Ochrony Zdrowia Na Lata 2021–2027, z Perspektywą Do 2030 r. Ministerstwo Zdrowia. Available online: https://www.gov.pl/web/zdrowie/zdrowa-przyszlosc-ramy-strategiczne-rozwoju-systemu-ochrony-zdrowia-na-lata-2021-2027-z-perspektywa-do-2030 (accessed on 26 September 2022).
- Liu, L.; Wei, K.; Zhang, X.; Wen, D.; Gao, L.; Lei, J. The Current Status and a New Approach for Chinese Doctors to Obtain Medical Knowledge Using Social Media: A Study of WeChat. Wirel. Commun. Mob. Comput. 2018, 2018, 2329876. [Google Scholar] [CrossRef] [Green Version]
- Internet in the life of Poles. Ministry of Digitization. 2019. Available online: https://www.gov.pl/web/cyfryzacja/internet-ulatwia-zycie-polakom (accessed on 22 August 2022).
- European Health Parliament. Committee on Digital Skills for Health Professionals. 2020. Available online: https://www.healthparliament.eu/wp-content/uploads/2017/09/Digital-skills-for-health-professionals.pdf (accessed on 22 August 2022).
- Han, E.R.; Yeo, S.; Kim, M.J.; Lee, Y.H.; Park, K.H.; Roh, H. Medical education trends for future physicians in the era of advanced technology and artificial intelligence: An integrative review. BMC Med. Educ. 2019, 19, 460. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nazeha, N.; Pavagadhi, D.; Kyaw, B.M.; Car, J.; Jimenez, G.; Car, L.T. A digitally competent health workforce: Scoping review of educational frameworks. J. Med. Internet Res. 2020, 22, e22706. [Google Scholar] [CrossRef]
- Foadi, N.; Varghese, J. Digital competence—A Key Competence for Todays and Future Physicians. J. Eur. CME 2022, 11, 2015200. [Google Scholar] [CrossRef] [PubMed]
- Thapa, D.K.; Visentin, D.C.; Kornhaber, R.; West, S.; Cleary, M. The influence of online health information on health decisions: A systematic review. Patient Educ. Couns. 2021, 104, 770–784. [Google Scholar] [CrossRef] [PubMed]
- Chu, J.T.; Wang, M.P.; Shen, C.; Viswanath, K.; Lam, T.H.; Chan, S.S.C. How, When and Why People Seek Health Information Online: Qualitative Study in Hong Kong. Interact. J. Med. Res. 2017, 6, e24. [Google Scholar] [CrossRef] [Green Version]
- Cocco, A.M.; Zordan, R.; Taylor, D.M.; Weiland, T.J.; Dilley, S.J.; Kant, J.; Dombagolla, M.; Hendarto, A.; Lai, F.; Hutton, J. Dr Google in the ED: Searching for online health information by adult emergency department patients. Med. J. Aust. 2018, 209, 342–347. [Google Scholar] [CrossRef]
- Doroszewska, A. Wpływ Internetu na zachowania w zdrowiu i chorobie. In Zdrowie i Choroba w Kontekście Psychospołecznym; Popielski, K., Skrzypek, M., Albińska, E., Eds.; Wydawnictwo KUL: Lublin, Poland, 2010; pp. 299–311. [Google Scholar]
- Potts, H.W.W.; Wyatt, J.C. Survey of Doctors’ Experience of Patients Using the Internet. J. Med. Internet Res. 2002, 4, e5. [Google Scholar] [CrossRef] [PubMed]
- Lewis, S.P.; Mahdy, J.C.; Michal, N.J.; Arbuthnott, A.E. Googling Self-injury: The state of health information obtained through online searches for self-injury. JAMA Pediatr. 2014, 168, 443–449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niedźwiedziński, M.; Klepacz, H. The Digitization of Health Care as a Weapon in the Fight against the COVID-19 Pandemic. Przedsiębiorczość I Zarządzanie 2021, 12, 81–99. [Google Scholar]
- Abd-Alrazaq, A.; Alajlani, M.; Alhuwail, D.; Schneider, J.; Al-Kuwari, S.; Shah, Z.; Hamdi, M.; Househ, M. Artificial Intelligence in the Fight Against COVID-19: Scoping Review. J. Med. Internet Res. 2020, 22, 12. [Google Scholar] [CrossRef] [PubMed]
- Deloitte. Digital Transformation: Shaping the Future of European Healthcare. 2020. Available online: https://www2.deloitte.com/pl/pl/pages/life-sciences-and-healthcare/articles/raport-Digital-transformation-Shaping-the-future-of-European-healthcare.html (accessed on 22 August 2022).
| Type of Electronic Device | Often | Sometimes | Never | N/A | ||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| Private usage | ||||||||
| Smartphone | 256 | 83.4 | 23 | 7.5 | 24 | 7.8 | 4 | 1.3 |
| Computer | 202 | 65.8 | 94 | 30.6 | 8 | 2.6 | 3 | 1.0 |
| 217 | 70.7 | 59 | 19.2 | 20 | 6.5 | 11 | 3.6 | |
| Mobile apps | 173 | 56.4 | 80 | 26.1 | 44 | 14.3 | 10 | 3.3 |
| Tablet | 70 | 22.8 | 104 | 33.9 | 107 | 34.9 | 26 | 8.5 |
| At work | ||||||||
| Smartphone | 146 | 47.6 | 75 | 24.4 | 65 | 21.2 | 21 | 6.8 |
| Computer | 261 | 85.0 | 31 | 10.1 | 14 | 4.6 | 1 | 0.3 |
| 95 | 30.9 | 116 | 37.8 | 82 | 26.7 | 14 | 4.6 | |
| Mobile apps | 76 | 24.8 | 103 | 33.6 | 103 | 33.6 | 25 | 8.1 |
| Tablet | 16 | 5.2 | 21 | 6.8 | 224 | 73.0 | 46 | 15.0 |
| Item | Yes | Rather Yes | No Opinion | Rather No | No | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |
| I feel prepared to use e-Health solutions in my work | 77 | 25.1 | 139 | 45.3 | 40 | 13.0 | 48 | 15.6 | 3 | 1.0 |
| I would use training courses to improve my digital literacy | 97 | 31.6 | 161 | 52.4 | 28 | 9.1 | 20 | 6.5 | 1 | 0.3 |
| Current physician education keeps pace with the digital challenges of the 21st century | 45 | 14.7 | 50 | 16.3 | 80 | 26.1 | 116 | 37.8 | 16 | 5.2 |
| There should be more subjects that shape digital literacy in medical studies | 80 | 26.1 | 153 | 49.8 | 43 | 14.0 | 30 | 9.8 | 1 | 0.3 |
| The Internet will revolutionize healthcare in the near future | 123 | 40.1 | 116 | 37.8 | 52 | 16.9 | 12 | 3.9 | 4 | 1.3 |
| Digital Literacy—Own Skills | Digital Literacy—The Need for Training | The Impact of the Internet/New Technologies on Healthcare and Modern Life | Recommendation of e-Health Solutions | Evaluation of e-Health Solutions—The Patient | Evaluation of e-Health Solutions—Medical Facility | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| The frequency of Internet use | ||||||||||||
| several times a day | −0.09 | 0.93 | 0.20 | 0.91 | −0.14 | 0.97 | −0.17 | 0.92 | −0.25 | 0.66 | 0.02 | 0.92 |
| everyday | −0.22 | 0.76 | −0.10 | 0.95 | −0.07 | 0.93 | 0.17 | 1.05 | −0.06 | 0.96 | 0.14 | 0.99 |
| several times a week | 0.11 | 0.60 | −0.86 | 0.99 | 0.31 | 0.67 | 0.22 | 1.02 | 0.67 | 1.24 | 0.21 | 1.34 |
| once a week | 1.27 | 1.19 | −0.58 | 1.14 | 0.91 | 0.54 | 0.88 | 0.89 | 1.66 | 1.08 | −0.79 | 0.91 |
| no use | 1.36 | 1.83 | −1.48 | 0.89 | 1.70 | 1.28 | 0.81 | 1.43 | 2.22 | 1.66 | −0.22 | 1.76 |
| F | p | F | p | F | p | F | p | F | p | F | p | |
| 13.167 | 0.0000 | 12.133 | 0.0000 | 11.448 | 0.0000 | 7.045 | 0.0000 | 37.800 | 0.0000 | 3.343 | 0.0107 | |
| The number of patients seen on average per month | ||||||||||||
| <50 | 0.01 | 1.09 | −0.05 | 1.02 | −0.35 | 0.89 | −0.34 | 1.22 | 0.07 | 1.29 | −0.42 | 0.65 |
| 50–100 | −0.04 | 0.95 | 0.21 | 0.64 | −0.23 | 0.85 | 0.28 | 0.75 | −0.05 | 0.72 | 0.11 | 0.87 |
| 100–200 | 0.07 | 0.91 | −0.04 | 1.34 | 0.17 | 1.00 | 0.23 | 1.01 | 0.40 | 1.15 | 0.44 | 1.22 |
| >200 | 0.01 | 1.03 | −0.10 | 1.06 | 0.19 | 1.06 | −0.13 | 1.02 | −0.08 | 1.00 | −0.06 | 1.05 |
| F | p | F | p | F | p | F | p | F | p | F | p | |
| 0.102 | 0.9587 | 1.873 | 0.1341 | 5.371 | 0.0013 | 5.432 | 0.0012 | 2.371 | 0.0705 | 5.163 | 0.0017 | |
| In Private Life | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Computer | Tablet | Smartphone | Mobile Apps | |||||||
| F | p | F | p | F | p | F | p | F | p | |
| Digital literacy—own skills | 9.480 | 0.0000 | 7.406 | 0.0001 | 3.506 | 0.0158 | 6.276 | 0.0004 | 8.420 | 0.0000 |
| Digital literacy—the need for training | 9.817 | 0.0000 | 1.580 | 0.1941 | 27.609 | 0.0000 | 14.514 | 0.0000 | 21.495 | 0.0000 |
| The impact of the Internet/new technologies on healthcare and modern life | 8.357 | 0.0000 | 9.068 | 0.0000 | 10.420 | 0.0000 | 11.179 | 0.0000 | 26.757 | 0.0000 |
| Recommendation of e-Health solutions | 9.241 | 0.0000 | 8.609 | 0.0000 | 6.229 | 0.0004 | 12.670 | 0.0000 | 10.941 | 0.0000 |
| Evaluation of e-Health solutions—the patient | 20.095 | 0.0000 | 16.166 | 0.0000 | 22.946 | 0.0000 | 43.822 | 0.0000 | 30.692 | 0.0000 |
| Evaluation of e-Health solutions—medical facility | 0.540 | 0.6550 | 2.606 | 0.0519 | 1.766 | 0.1536 | 5.141 | 0.0018 | 2.764 | 0.0421 |
| At work | ||||||||||
| Digital literacy—own skills | 17.886 | 0.0000 | 11.169 | 0.0000 | 5.831 | 0.0007 | 19.753 | 0.0000 | 6.240 | 0.0004 |
| Digital literacy—the need for training | 7.165 | 0.0001 | 2.059 | 0.1057 | 10.942 | 0.0000 | 12.404 | 0.0000 | 16.157 | 0.0000 |
| The impact of the Internet/new technologies on healthcare and modern life | 19.639 | 0.0000 | 2.606 | 0.0519 | 11.731 | 0.0000 | 8.553 | 0.0000 | 6.962 | 0.0002 |
| Recommendation of e-Health solutions | 6.141 | 0.0005 | 3.878 | 0.0096 | 10.026 | 0.0000 | 12.827 | 0.0000 | 8.529 | 0.0000 |
| Evaluation of e-Health solutions—the patient | 26.764 | 0.0000 | 2.533 | 0.0571 | 16.946 | 0.0000 | 28.404 | 0.0000 | 10.060 | 0.0000 |
| Evaluation of e-Health solutions—medical facility | 2.396 | 0.0683 | 2.172 | 0.0913 | 0.491 | 0.6890 | 1.795 | 0.1481 | 0.875 | 0.4543 |
| Digital Literacy—Own Skills | Digital literacy—The Need for Training | Assessment of the Impact of the Internet/New Technologies on Healthcare and Modern Life | Recommendation of e-Health Solutions | Evaluation of e-Health Solutions—The Patient | Evaluation of e-Health Solutions—Medical Facility | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| % of patients accessing online health information within a month | ||||||||||||
| <1% | −0.08 | 1.62 | 0.55 | 1.20 | −0.31 | 0.83 | −0.48 | 1.28 | −0.38 | 0.69 | −0.04 | 0.59 |
| 1–2% | −0.02 | 1.15 | 0.03 | 1.05 | 0.12 | 0.72 | −0.15 | 1.51 | 0.48 | 1.30 | −0.01 | 1.34 |
| 3–5% | −0.10 | 1.08 | −0.15 | 0.70 | −0.06 | 0.87 | −0.01 | 0.95 | −0.07 | 0.76 | 0.15 | 0.88 |
| 6–10% | 0.03 | 0.89 | −0.04 | 1.02 | 0.12 | 0.99 | 0.12 | 0.99 | 0.15 | 1.18 | 0.11 | 1.32 |
| >10% | −0.14 | 0.70 | 0.27 | 0.91 | −0.18 | 1.02 | −0.07 | 0.84 | −0.31 | 0.76 | −0.09 | 0.77 |
| it is difficult to estimate | 0.25 | 1.15 | −0.32 | 1.12 | 0.22 | 1.11 | 0.14 | 1.03 | 0.30 | 1.13 | −0.03 | 1.11 |
| Opinion about the general quality of online health information | ||||||||||||
| reliable | −1.00 | 1.07 | 0.06 | 0.93 | −0.82 | 0.43 | −1.52 | 1.15 | −0.85 | 0.44 | −0.16 | 0.76 |
| usually reliable | −0.08 | 1.08 | −0.28 | 0.87 | −0.04 | 0.72 | −0.29 | 0.89 | −0.14 | 0.79 | 0.01 | 0.91 |
| sometimes reliable | −0.07 | 0.83 | 0.10 | 0.95 | −0.05 | 1.04 | 0.04 | 0.98 | −0.07 | 0.79 | 0.15 | 1.03 |
| unreliable | 0.19 | 1.10 | 0.13 | 1.22 | 0.13 | 0.97 | 0.18 | 0.92 | 0.19 | 1.30 | −0.23 | 0.90 |
| no opinion | 0.74 | 1.18 | −0.44 | 0.94 | 0.54 | 1.31 | 0.67 | 0.68 | 0.75 | 1.59 | −0.53 | 1.11 |
| Opinion on patients’ experience of health benefits as a result of access to online health information | ||||||||||||
| often | −1.06 | 0.83 | 0.18 | 0.86 | −0.50 | 0.57 | −1.53 | 0.86 | −0.84 | 0.39 | −0.23 | 0.81 |
| sometimes | 0.00 | 0.64 | 0.04 | 0.98 | −0.16 | 0.86 | −0.30 | 0.79 | −0.27 | 0.72 | −0.05 | 0.94 |
| seldom | −0.14 | 0.93 | 0.13 | 1.13 | 0.07 | 1.15 | 0.13 | 0.95 | −0.06 | 1.08 | 0.03 | 1.05 |
| never | 0.65 | 1.10 | 0.98 | 1.08 | 0.57 | 0.89 | 1.05 | 0.59 | 0.73 | 1.14 | −0.27 | 0.84 |
| no opinion | 0.19 | 1.23 | −0.29 | 0.82 | 0.12 | 1.04 | 0.34 | 0.94 | 0.37 | 1.06 | 0.10 | 1.08 |
| An assessment of patients’ use of online health knowledge | ||||||||||||
| very positive | −0.62 | 1.30 | −0.10 | 0.99 | −0.52 | 0.89 | −1.51 | 1.14 | −0.72 | 0.59 | −0.11 | 0.77 |
| positive | 0.09 | 1.00 | −0.09 | 0.66 | 0.13 | 0.95 | −0.23 | 0.91 | −0.12 | 0.66 | −0.21 | 0.70 |
| meaningless | −0.24 | 0.99 | −0.01 | 1.08 | −0.31 | 0.98 | −0.21 | 1.10 | −0.20 | 1.06 | −0.17 | 0.97 |
| negative | 0.02 | 0.92 | 0.21 | 1.03 | −0.01 | 0.82 | 0.19 | 0.85 | 0.04 | 0.96 | 0.21 | 1.08 |
| very negative | 0.31 | 1.07 | −0.44 | 1.01 | 0.42 | 1.35 | 0.34 | 0.96 | 0.46 | 1.23 | −0.05 | 1.07 |
| % of Patients Accessing Online Health Information within a Month | An Opinion on the Overall Quality of Online Health Information | An Opinion on Patients’ Health Benefits Related to Online Health Information | An Assessment of Patients’ Use of Online Health Knowledge | |||||
|---|---|---|---|---|---|---|---|---|
| F | p | F | p | F | p | F | p | |
| Digital literacy—own skills | 1.541 | 0.1769 | 6.709 | 0.0000 | 7.845 | 0.0000 | 3.167 | 0.0143 |
| Digital literacy—the need for training | 4.262 | 0.0009 | 2.781 | 0.0270 | 6.066 | 0.0001 | 3.985 | 0.0036 |
| The impact of the Internet/new technologies on healthcare and modern life | 1.891 | 0.0956 | 3.776 | 0.0052 | 3.309 | 0.0113 | 4.754 | 0.0010 |
| Recommendation of e-Health solutions | 1.173 | 0.3225 | 11.079 | 0.0000 | 24.239 | 0.0000 | 10.246 | 0.0000 |
| Assessment of e-Health solutions—the patient | 5.193 | 0.0001 | 6.130 | 0.0001 | 11.394 | 0.0000 | 4.726 | 0.0010 |
| Assessment of e-Health solutions—medical facility | 0.517 | 0.7635 | 3.358 | 0.0104 | 0.760 | 0.5520 | 2.546 | 0.0396 |
| e-Health Solution | I Have Already Recommended | I Would Recommend | I Do Not Recommend | |||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Remote monitoring of basic parameters (pressure, heart rate, temperature, glucose level) | 45 | 14.7 | 127 | 41.4 | 135 | 44.0 |
| Obtaining laboratory test results via the Internet | 99 | 32.2 | 163 | 53.1 | 45 | 14.7 |
| Arranging medical appointments via the Internet | 83 | 27.0 | 143 | 46.6 | 81 | 26.4 |
| Using a mobile application—the analysis of tests results | 47 | 15.3 | 110 | 35.8 | 150 | 48.9 |
| Using the mobile application—a knowledge base on health-related topics | 41 | 13.4 | 151 | 49.2 | 115 | 37.5 |
| Using the mobile application—a mobile drug database | 48 | 15.6 | 146 | 47.6 | 113 | 36.8 |
| Using a mobile application—reminder to take medication | 41 | 13.4 | 222 | 72.3 | 44 | 14.3 |
| Using a video consultation with the doctor /nurse /midwife to support the treatment process | 33 | 10.7 | 132 | 43.0 | 142 | 46.3 |
| Very Important | Important | Not very Important | Insignificant | No Opinion | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |
| Quick and easy access to the patient’s medical records in electronic form | 129 | 42.0 | 127 | 41.4 | 31 | 10.1 | 6 | 2.0 | 14 | 4.6 |
| The possibility to write electronic prescriptions | 112 | 36.5 | 132 | 43.0 | 33 | 10.7 | 6 | 2.0 | 24 | 7.8 |
| The possibility to write out electronic sick leaves | 137 | 44.6 | 132 | 43.0 | 18 | 5.9 | 11 | 3.6 | 9 | 2.9 |
| The possibility to write electronic referrals | 112 | 36.5 | 141 | 45.9 | 31 | 10.1 | 8 | 2.6 | 15 | 4.9 |
| Using the electronic database of medicines | 148 | 48.2 | 128 | 41.7 | 13 | 4.2 | 2 | 0.7 | 16 | 5.2 |
| The ability to remotely route patients to other specialists or hospitals | 106 | 34.5 | 129 | 42.0 | 38 | 12.4 | 9 | 2.9 | 25 | 8.1 |
| The solutions to streamline the sending/sharing clinical results | 143 | 46.6 | 113 | 36.8 | 24 | 7.8 | 8 | 2.6 | 19 | 6.2 |
| Solutions enabling remote patient care | 87 | 28.3 | 84 | 27.4 | 44 | 14.3 | 45 | 14.7 | 47 | 15.3 |
| More digital solutions supporting the treatment and self-monitoring of the patient’s health | 70 | 22.8 | 143 | 46.6 | 46 | 15.0 | 13 | 4.2 | 35 | 11.4 |
| The possibility to exercise comprehensive control over facilities, tracking generated costs, managing staff (schedules, schedules) | 72 | 23.5 | 131 | 42.7 | 46 | 15.0 | 15 | 4.9 | 43 | 14.0 |
| The possibility to conduct scientific research | 96 | 31.3 | 120 | 39.1 | 26 | 8.5 | 18 | 5.9 | 47 | 15.3 |
| Digital Literacy—Need for Training | The Impact of the Internet/New Technologies on Healthcare and Modern Life | Recommendation of e-Health Solutions | Assessment of e-Health Solutions—the Patient | Assessment of e-Health Solutions—Medical Facility | ||
|---|---|---|---|---|---|---|
| Digital literacy—own skills | r | 0.000 | 0.447 | 0.413 | 0.449 | −0.105 |
| p | 1.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0673 | |
| Digital literacy—need for training | r | −0.239 | −0.131 | −0.250 | 0.040 | |
| p | 0.0000 | 0.0220 | 0.0000 | 0.4883 | ||
| The impact of the Internet/new technologies on healthcare and modern life | r | 0.369 | 0.457 | 0.022 | ||
| p | 0.0000 | 0.0000 | 0.7029 | |||
| Recommendation of e-Health solutions | r | 0.588 | 0.140 | |||
| p | 0.0000 | 0.0144 | ||||
| Assessment of e-Health solutions—the patient | r | 0.000 | ||||
| p | 1.0000 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burzyńska, J.; Bartosiewicz, A.; Januszewicz, P. Dr. Google: Physicians—The Web—Patients Triangle: Digital Skills and Attitudes towards e-Health Solutions among Physicians in South Eastern Poland—A Cross-Sectional Study in a Pre-COVID-19 Era. Int. J. Environ. Res. Public Health 2023, 20, 978. https://doi.org/10.3390/ijerph20020978
Burzyńska J, Bartosiewicz A, Januszewicz P. Dr. Google: Physicians—The Web—Patients Triangle: Digital Skills and Attitudes towards e-Health Solutions among Physicians in South Eastern Poland—A Cross-Sectional Study in a Pre-COVID-19 Era. International Journal of Environmental Research and Public Health. 2023; 20(2):978. https://doi.org/10.3390/ijerph20020978
Chicago/Turabian StyleBurzyńska, Joanna, Anna Bartosiewicz, and Paweł Januszewicz. 2023. "Dr. Google: Physicians—The Web—Patients Triangle: Digital Skills and Attitudes towards e-Health Solutions among Physicians in South Eastern Poland—A Cross-Sectional Study in a Pre-COVID-19 Era" International Journal of Environmental Research and Public Health 20, no. 2: 978. https://doi.org/10.3390/ijerph20020978
APA StyleBurzyńska, J., Bartosiewicz, A., & Januszewicz, P. (2023). Dr. Google: Physicians—The Web—Patients Triangle: Digital Skills and Attitudes towards e-Health Solutions among Physicians in South Eastern Poland—A Cross-Sectional Study in a Pre-COVID-19 Era. International Journal of Environmental Research and Public Health, 20(2), 978. https://doi.org/10.3390/ijerph20020978







