Is Positive Affect as a Trait Related to Higher Heart Rate Variability in a Stressful Situation?
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Materials
2.2.1. PANAS
2.2.2. Cognitive Tests
2.2.3. VAS
2.2.4. NASA-TLX Questionnaire
2.2.5. Stress Test
2.2.6. Equipment
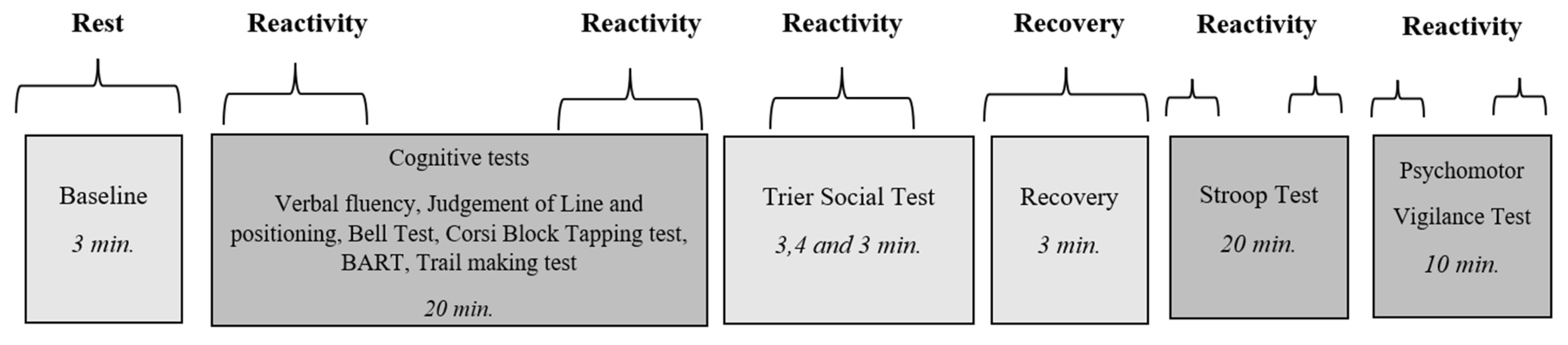
2.3. Procedure
2.4. Recording of HRV
2.5. Statistical Analysis
3. Results
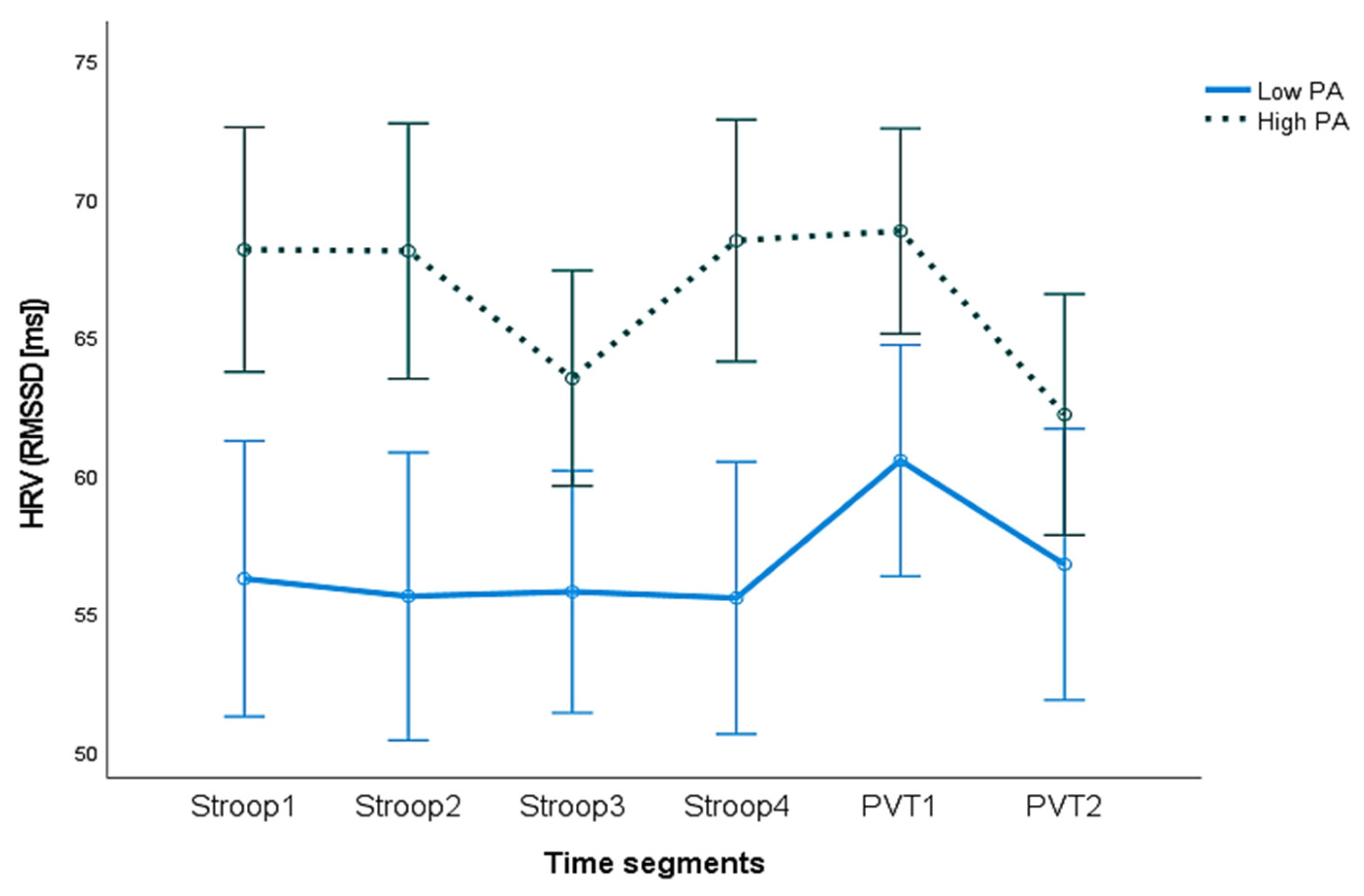
3.1. HRV and Trait PA
3.2. IBI, HR, and Trait PA
3.3. Subjective Assessment of Stress and Workload
4. Discussion
4.1. Trait PA as a Buffer against Harmful Effects
4.2. HRV for PNS Activity and Trait PA
4.3. HRV, PA, and Emotional Regulation
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chida, Y.; Steptoe, A. Positive psychological well-being and mortality: A quantitative review of prospective observational studies. Psychosom. Med. 2008, 70, 741–756. [Google Scholar] [CrossRef] [PubMed]
- Diener, E.; Chan, M.Y. Happy people live longer: Subjective well-being contributes to health and longevity. Appl. Psychol. Health Well-Being 2011, 3, 1–43. [Google Scholar] [CrossRef]
- Zhang, Y.; Han, B. Positive affect and mortality risk in older adults: A meta-analysis. PsyCh J. 2016, 5, 125–138. [Google Scholar] [CrossRef] [PubMed]
- Boehm, J.K.; Kubzansky, L.D. The heart’s content: The association between positive psychological well-being and cardiovascular health. Psychol. Bull. 2012, 138, 655. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, R.; Bassett, S.M.; Boughton, S.W.; Schuette, S.A.; Shiu, E.W.; Moskowitz, J.T. Psychological well-being and physical health: Associations, mechanisms, and future directions. Emot. Rev. 2018, 10, 18–29. [Google Scholar] [CrossRef]
- Pressman, S.D.; Cross, M.P. Moving beyond a one-size-fits-all view of positive affect in health research. Curr. Dir. Psychol. Sci. 2018, 27, 339–344. [Google Scholar] [CrossRef]
- Marsland, A.L.; Pressman, S.A.; Cohen, S. Positive affect and immune function. Psychoneuroimmunology 2007, 2, 761–779. [Google Scholar]
- Pressman, S.D.; Jenkins, B.N.; Moskowitz, J.T. Positive affect and health: What do we know and where next should we go? Annu. Rev. Psychol. 2019, 70, 627–650. [Google Scholar] [CrossRef]
- Brummett, B.H.; Boyle, S.H.; Kuhn, C.M.; Siegler, I.C.; Williams, R.B. Positive affect is associated with cardiovascular reactivity, norepinephrine level, and morning rise in salivary cortisol. Psychophysiology 2009, 46, 862–869. [Google Scholar] [CrossRef]
- Pressman, S.D.; Cohen, S. Does positive affect influence health? Psychol. Bull. 2005, 131, 925–971. [Google Scholar] [CrossRef]
- Tugade, M.M.; Fredrickson, B.L. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J. Personal. Soc. Psychol. 2004, 86, 320–333. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Gibson, E.L.; Hamer, M.; Wardle, J. Neuroendocrine and cardiovascular correlates of positive affect measured by ecological momentary assessment and by questionnaire. Psychoneuroendocrinology 2007, 32, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Papousek, I.; Nauschnegg, K.; Paechter, M.; Lackner, H.K.; Goswami, N.; Schulter, G. Trait and state positive affect and cardiovascular recovery from experimental academic stress. Biol. Psychol. 2010, 83, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Dowd, H.; Zautra, A.; Hogan, M. Emotion, stress, and cardiovascular response: An experimental test of models of positive and negative affect. Int. J. Behav. Med. 2010, 17, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Chida, Y.; Steptoe, A. Response to stress reactivity and its association with increased cardiovascular risk: A role for the sympathetic nervous system? Hypertension 2010, 55, e21. [Google Scholar] [CrossRef]
- Schwartz, A.R.; Gerin, W.; Davidson, K.W.; Pickering, T.G.; Brosschot, J.F.; Thayer, J.F.; Christenfeld, N.; Linden, W. Toward a causal model of cardiovascular responses to stress and the development of cardiovascular disease. Psychosom. Med. 2003, 65, 22–35. [Google Scholar] [CrossRef] [PubMed]
- Treiber, F.A.; Kamarck, T.; Schneiderman, N.; Sheffield, D.; Kapuku, G.; Taylor, T. Cardiovascular reactivity and development of preclinical and clinical disease states. Psychosom. Med. 2003, 65, 46–62. [Google Scholar] [CrossRef]
- Gump, B.B.; Matthews, K.A. Do background stressors influence reactivity to and recovery from acute stressors? J. Appl. Soc. Psychol. 1999, 29, 469–494. [Google Scholar] [CrossRef]
- Steptoe, A.; Feldman, P.J.; Kunz, S.; Owen, N.; Willemsen, G.; Marmot, M. Stress responsivity and socioeconomic status. A mechanism for increased cardiovascular disease risk? Eur. Heart J. 2002, 23, 1757–1763. [Google Scholar] [CrossRef]
- Schneider, G.M.; Jacobs, D.W.; Gevirtz, R.N.; O’Connor, D.T. Cardiovascular hemodynamic response to repeated mental stress in normotensive subjects at genetic risk of hypertension: Evidence of enhanced reactivity, blunted adaptation, and delayed recovery. J. Hum. Hypertens. 2003, 17, 829–840. [Google Scholar] [CrossRef]
- Lovallo, W.R. Stress and Health: Biological and Psychological Interactions, 2nd ed.; Sage: Thousand Oaks, CA, USA, 2004. [Google Scholar]
- Brosschot, J.F.; Thayer, J.F. Anger inhibition, cardiovascular recovery, and vagal function: A model of the link between hostility and cardiovascular disease. Ann. Behav. Med. 1998, 20, 326–332. [Google Scholar] [CrossRef]
- Saul, J.P. Beat-to-beat variations of heart rate reflect modulation of cardiac autonomic outflow. Physiology 1990, 5, 32–37. [Google Scholar] [CrossRef]
- Fredrickson, B.L.; Levenson, R.W. Positive emotions speed recovery from the cardiovascular sequelae of negative emotions. Cogn. Emot. 1998, 12, 191–220. [Google Scholar] [CrossRef] [PubMed]
- Gendolla, G.H.; Krüsken, J. Mood state and cardiovascular response in active coping with an affect-regulative challenge. Int. J. Psychophysiol. 2001, 41, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Dockray, S.; Steptoe, A. Positive affect and psychobiological processes. Neurosci. Biobehav. Rev. 2010, 35, 69–75. [Google Scholar] [CrossRef]
- Thayer, J.F.; Lane, R.D. A model of neurovisceral integration in emotion regulation and dysregulation. J. Affect. Disord. 2000, 61, 201–216. [Google Scholar] [CrossRef]
- Bostock, S.; Hamer, M.; Wawrzyniak, A.J.; Mitchell, E.S.; Steptoe, A. Positive emotional style and subjective, cardiovascular, and cortisol responses to acute laboratory stress. Psychoneuroendocrinology 2011, 36, 1175–1183. [Google Scholar] [CrossRef]
- Laborde, S.; Mosley, E.; Thayer, J.F. Heart rate variability and cardiac vagal tone in psychophysiological research–recommendations for experiment planning, data analysis, and data reporting. Front. Psychol. 2017, 8, 213. [Google Scholar] [CrossRef]
- Malik, M. Task force of the European society of cardiology and the north American society of pacing and electrophysiology. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Eur. Heart J. 1996, 17, 354–381. [Google Scholar] [CrossRef]
- Pomeranz, B.; Macaulay, R.J.; Caudill, M.A.; Kutz, I.; Adam, D.; Gordon, D.; Kilborn, K.M.; Barger, A.C.; Shannon, D.C.; Cohen, R.J.; et al. Assessment of autonomic function in humans by heart rate spectral analysis. Am. J. Physiol.-Heart Circ. Physiol. 1985, 248, H151–H153. [Google Scholar] [CrossRef]
- Shaffer, F.; Venner, J. Heart rate variability anatomy and physiology. Biofeedback 2013, 41, 13–25. [Google Scholar] [CrossRef]
- Acharya, U.R.; Joseph, K.P.; Kannathal, N.; Lim, C.M.; Suri, J.S. Heart rate variability: A review. Med. Biol. Eng. Comput. 2006, 44, 1031–1051. [Google Scholar] [CrossRef]
- Pham, T.; Lau, Z.J.; Chen, S.H.; Makowski, D. Heart Rate Variability in Psychology: A Review of HRV Indices and an Analysis Tutorial. Sensors 2021, 21, 3998. [Google Scholar] [CrossRef] [PubMed]
- Trimmel, M. Relationship of heart rate variability (HRV) parameters including pNNxx with the subjective experience of stress, depression, well-being, and every-day trait moods (TRIM-T): A pilot study. Ergon. Open J. 2015, 8, 32–37. [Google Scholar] [CrossRef]
- Schwerdtfeger, A.R.; Gerteis, A.K.S. The manifold effects of positive affect on heart rate variability in everyday life: Distinguishing within-person and between-person associations. Health Psychol. 2014, 33, 1065–1073. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Lü, W.; Qin, R. Respiratory sinus arrhythmia is associated with trait positive affect and positive emotional expressivity. Biol. Psychol. 2013, 93, 190–196. [Google Scholar] [CrossRef]
- Kok, B.E.; Fredrickson, B.L. Upward spirals of the heart: Autonomic flexibility, as indexed by vagal tone, reciprocally and prospectively predicts positive emotions and social connectedness. Biol. Psychol. 2010, 85, 432–436. [Google Scholar] [CrossRef]
- Oveis, C.; Cohen, A.B.; Gruber, J.; Shiota, M.N.; Haidt, J.; Keltner, D. Resting respiratory sinus arrhythmia is associated with tonic positive emotionality. Emotion 2009, 9, 265. [Google Scholar] [CrossRef]
- Bhattacharyya, M.R.; Whitehead, D.L.; Rakhit, R.; Steptoe, A. Depressed mood, positive affect, and heart rate variability in patients with suspected coronary artery disease. Psychosom. Med. 2008, 70, 1020–1027. [Google Scholar] [CrossRef]
- Grol, M.; De Raedt, R. The link between resting heart rate variability and affective flexibility. Cogn. Affect. Behav. Neurosci. 2020, 20, 746–756. [Google Scholar] [CrossRef]
- Park, G.; Thayer, J.F. From the heart to the mind: Cardiac vagal tone modulates top-down and bottom-up visual perception and attention to emotional stimuli. Front. Psychol. 2014, 5, 278. [Google Scholar] [CrossRef] [PubMed]
- Appelhans, B.M.; Luecken, L.J. Heart rate variability as an index of regulated emotional responding. Rev. Gen. Psychol. 2006, 10, 229–240. [Google Scholar] [CrossRef]
- Balzarotti, S.; Biassoni, F.; Colombo, B.; Ciceri, M.R. Cardiac vagal control as a marker of emotion regulation in healthy adults: A review. Biol. Psychol. 2017, 130, 54–66. [Google Scholar] [CrossRef]
- Ruiz-Padial, E.; Sollers, J.J.; Vila, J.; Thayer, J.F. The rhythm of the heart in the blink of an eye: Emotion-modulated startle magnitude covaries with heart rate variability. Psychophysiology 2003, 40, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Thayer, J.F.; Brosschot, J.F. Psychosomatics and psychopathology: Looking up and down from the brain. Psychoneuroendocrinology 2005, 30, 1050–1058. [Google Scholar] [CrossRef] [PubMed]
- Geisler, F.C.; Vennewald, N.; Kubiak, T.; Weber, H. The impact of heart rate variability on subjective well-being is mediated by emotion regulation. Personal. Andin. Differ. 2010, 49, 723–728. [Google Scholar] [CrossRef]
- Steptoe, A.; Wardle, J. Positive affect and biological function in everyday life. Neurobiol. Aging 2005, 26, 108–112. [Google Scholar] [CrossRef]
- Dreisbach, G.; Goschke, T. How positive affect modulates cognitive control: Reduced perseveration at the cost of increased distractibility. J. Exp. Psychol. Learn. Mem. Cogn. 2004, 30, 343. [Google Scholar] [CrossRef]
- Tugade, M.M.; Fredrickson, B.L.; Feldman Barrett, L. Psychological resilience and positive emotional granularity: Examining the benefits of positive emotions on coping and health. J. Personal. 2004, 72, 1161–1190. [Google Scholar] [CrossRef]
- Cavanagh, C.E.; Larkin, K.T. A critical review of the “undoing hypothesis”: Do positive emotions undo the effects of stress? Appl. Psychophysiol. Biofeedback 2018, 43, 259–273. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Personal. Soc. Psychol. 1988, 54, 1063–1070. [Google Scholar] [CrossRef] [PubMed]
- Watson, D.; Walker, L.M. The long-term stability and predictive validity of trait measures of affect. J. Personal. Soc. Psychol. 1996, 70, 567–577. [Google Scholar] [CrossRef] [PubMed]
- Halldórsson, Á. Athugun á próffræðilegum eiginleikum íslenskrar útgáfu PANAS-kvarðans [Assessing the Psychometric Properties of the Icelandic Publication of PANAS Scale]. Bachelor’s Thesis, Faculty of Psychology, University of Iceland, Reykjavík, Iceland, 2007. [Google Scholar]
- Crawford, J.R.; Henry, J.D. The positive and negative affect schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2004, 43, 245–265. [Google Scholar] [CrossRef]
- Schonberg, T.; Fox, C.R.; Mumford, J.A.; Congdon, E.; Trepel, C.; Poldrack, R.A. Decreasing ventromedial prefrontal cortex activity during sequential risk-taking: An fMRI investigation of the balloon analog risk task. Front. Neurosci. 2012, 6, 80. [Google Scholar] [CrossRef]
- Helfinstein, S.M.; Schonberg, T.; Congdon, E.; Karlsgodt, K.H.; Mumford, J.A.; Sabb, F.W.; Cannon, T.D.; London, E.D.; Bilder, R.M.; Poldrack, R.A. Predicting risky choices from brain activity patterns. Proc. Natl. Acad. Sci. USA 2014, 111, 2470–2475. [Google Scholar] [CrossRef]
- Lejuez, C.W.; Read, J.P.; Kahler, C.W.; Richards, J.B.; Ramsey, S.E.; Stuart, G.L.; Strong, D.R.; Brown, R.A. Evaluation of a behavioral measure of risk taking: The Balloon Analogue Risk Task (BART). J. Exp. Psychol. Appl. 2002, 8, 75–84. [Google Scholar] [CrossRef]
- Escovar Paiva, S.C.; Viapiana, V.F.; de Oliveira Cardoso, C.; Fonseca, R.P. Bells Test: Are there differences in performance between adult groups aged 40–59 and 60–75? Dement. Neuropsychol. 2017, 11, 40–47. [Google Scholar] [CrossRef][Green Version]
- Vanier, M.; Gauthier, L.; Lambert, J.; Pepin, E.P.; Robillard, A.; Dubouloz, C.J.; Gagnon, R.; Joannette, Y. Evaluation of left visuospatial neglect: Norms and discrimination power of two tests. Neuropsychology 1990, 4, 87–96. [Google Scholar] [CrossRef]
- Ferber, S.; Karnath, H.O. How to assess spatial neglect—Line bisection or cancellation tests? J. Clin. Exp. Neuropsychol. 2001, 23, 599–607. [Google Scholar] [CrossRef]
- Gauthier, L.; Dehaut, F.; Joanette, Y. The Bells Test: A quantitative and qualitative test for visual neglect. Int. J. Clin. Neuropsychol. 1989, 11, 49–54. [Google Scholar]
- Corsi, P.M. Human Memory and the Medial Temporal Region of the Brain. Doctoral Thesis, McGill University, Montréal, QC, USA, 1972. Available online: https://bit.ly/3xZlORh (accessed on 15 October 2021).
- Kessels, R.P.; van Zandvoort, M.J.; Postma, A.; Kappelle, L.J.; de Haan, E.H. The Corsi Block-Tapping Task: Standardization and normative data. Appl. Neuropsychol. 2000, 7, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Collaer, M.L.; Reimers, S.; Manning, J.T. Visuospatial performance on an internet line judgment task and potential hormonal markers: Sex, sexual orientation, and 2D: 4D. Arch. Sex. Behav. 2007, 36, 177–192. [Google Scholar] [CrossRef] [PubMed]
- Collaer, M.L. Judgment of Line Angle and Position Test-15 Line Version (JLAP-15); Unpublished Test; Middlebury College: Middlebury, VT, USA, 2001. [Google Scholar]
- Dinges, D.F.; Powell, J.W. Microcomputer analyses of performance on a portable, simple visual RT task during sustained operations. Behav. Res. Methods Instrum. Comput. 1985, 17, 652–655. [Google Scholar] [CrossRef]
- Dorian, J.; Rogers, N.L.; Dinges, D.F. Psychomotor Vigilance Performance: Neurocognitive Assay Sensitive to Sleep Loss; Marcel Dekker: New York, NY, USA, 2005. [Google Scholar]
- Drummond, S.P.; Bischoff-Grethe, A.; Dinges, D.F.; Ayalon, L.; Mednick, S.C.; Meloy, M.J. The neural basis of the psychomotor vigilance task. Sleep 2005, 28, 1059–1068. [Google Scholar] [CrossRef]
- Basner, M.; Dinges, D.F. Maximizing sensitivity of the psychomotor vigilance test (PVT) to sleep loss. Sleep 2011, 34, 581–591. [Google Scholar] [CrossRef]
- Stroop, J.R. Studies of interference in serial verbal reactions. J. Exp. Psychol. 1935, 18, 643–662. [Google Scholar] [CrossRef]
- Jensen, A.R.; Rohwer, W.D., Jr. The Stroop color-word test: A review. Acta Psychol. 1966, 25, 36–93. [Google Scholar] [CrossRef]
- Vazan, R.; Filcikova, D.; Mravec, B. Effect of the Stroop test performed in supine position on the heart rate variability in both genders. Autonomic Neuroscience: Basic Clin. 2017, 208, 156–160. [Google Scholar] [CrossRef]
- Johannsdottir, K.R.; Magnúsdóttir, E.H.; Sigurjónsdóttir, S.; Guðnason, J. The role of working memory capacity in cardiovascular monitoring of cognitive workload. Biol. Psychol. 2018, 132, 154–163. [Google Scholar] [CrossRef]
- Reitan, R.M.; Wolfson, D. The Halstead-Reitan Neuropsychological Test Battery: Theory and Clinical Interpretation; Neuropsychological Press: Tuscon, AZ, USA, 1985. [Google Scholar]
- Reitan, R.M. Validity of the Trail-Making Test as an indicator of organic brain damage. Percept. Mot. Ski. 1958, 8, 271–276. [Google Scholar] [CrossRef]
- Chan, E.; MacPherson, S.E.; Robinson, G.; Turner, M.; Lecce, F.; Shallice, T.; Cipolotti, L. Limitations of the Trail Making Test Part-B in assessing frontal executive dysfunction. J. Int. Neuropsychol. Soc. 2015, 21, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Dikmen, S.S.; Heaton, R.K.; Grant, I.; Temkin, N.R. Test-retest reliability and practice effects of expanded Halstead–Reitan Neuropsychological Test Battery. J. Int. Neuropsychol. Soc. 1999, 5, 346–356. [Google Scholar] [CrossRef] [PubMed]
- Lezak, M.D.; Howieson, D.B.; Loring, D.W. Neuropsychological Assessment, 5th ed.; Oxford University Press: Oxford, UK, 2012. [Google Scholar]
- Strauss, E.; Sherman, E.M.S.; Spreen, O. A Compendium of Neuropsychological Tests: Administration, Norms, and Commentary, 3rd ed.; Oxford University Press: Oxford, UK, 2006. [Google Scholar]
- Benton, A.L.; Hamsher, K.; Rey, G.L.; Sivan, A.B. Multilingual Aphasia Examination, 3rd ed.; AJA Associates: Iowa City, IA, USA, 1994. [Google Scholar]
- Ratcliff, G.; Ganguli, M.; Chandra, V.; Sharma, S.; Belle, S.; Seaberg, E.; Pandav, R. Effects of literacy and education on measures of word fluency. Brain Lang. 1998, 61, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Tucha, O.; Smely, C.; Lange, K.W. Verbal and figural fluency in patients with mass lesions of the left or right frontal lobes. J. Clin. Exp. Neuropsychol. 1999, 21, 229–236. [Google Scholar] [CrossRef]
- Delis, D.C.; Kaplan, E.; Kramer, J.H. Delis-Kaplan Executive Function System: Technical Manual; The Psychological Corporation: San Antonio, TX, USA, 2001. [Google Scholar]
- Magnúsdóttir, E.H. Cognitive Workload Classification with Psychophysiological Signals for Monitoring in Safety Critical Situations. Doctoral Dissertation, University of Reykjavik, Reykjavík, Iceland, 2019. [Google Scholar]
- Gould, D.; Kelly, D.; Goldstone, L.; Gammon, J. Examining the validity of pressure ulcer risk assessment scales: Developing and using illustrated patient simulations to collect the data. J. Clin. Nurs. 2001, 10, 697–706. [Google Scholar] [CrossRef]
- Paul-Dauphin, A.; Guillemin, F.; Virion, J.M.; Briançon, S. Bias and precision in visual analogue scales: A randomized controlled trial. Am. J. Epidemiol. 1999, 150, 1117–1127. [Google Scholar] [CrossRef]
- Jensen, M.P.; Chen, C.; Brugger, A.M. Interpretation of visual analog scale ratings and change scores: A reanalysis of two clinical trials of postoperative pain. J. Pain 2003, 4, 407–414. [Google Scholar] [CrossRef]
- Hart, S.G. NASA-task load index (NASA-TLX); 20 years later. In Proceedings of the Human Factors and Ergonomics Society Annual Meeting; Sage publications: Los Angeles, CA, USA, 2006; Volume 50, pp. 904–908. [Google Scholar] [CrossRef]
- Brookings, J.B.; Wilson, G.F.; Swain, C.R. Psychophysiological responses to changes in workload during simulated air traffic control. Biol. Psychol. 1996, 42, 361–377. [Google Scholar] [CrossRef]
- Casali, J.G.; Wierwille, W.W. On the measurement of pilot perceptual workload: A comparison of assessment techniques addressing sensitivity and intrusion issues. Ergonomics 1984, 27, 1033–1050. [Google Scholar] [CrossRef]
- Verwey, W.B.; Veltman, H.A. Detecting short periods of elevated workload: A comparison of nine workload assessment techniques. J. Exp. Psychol. Appl. 1996, 2, 270–285. [Google Scholar] [CrossRef]
- Kirschbaum, C.; Pirke, K.M.; Hellhammer, D.H. The ‘Trier Social Stress Test’—A tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology 1993, 28, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Caretaker Medical. What Can Caretaker Monitor? 2020. Available online: https://caretakermedical.net (accessed on 10 February 2021).
- Kwon, Y.; Stafford, P.L.; Enfield, K.; Mazimba, S.; Baruch, M.C. Continuous noninvasive blood pressure monitoring of beat-by-beat blood pressure and heart rate using caretaker compared with invasive arterial catheter in the intensive care unit. J. Cardiothorac. Vasc. Anesth. 2022, 36, 2012–2021. [Google Scholar] [CrossRef] [PubMed]
- Gray, C.D.; Kinnear, P.R. IBM SPSS Statistics 19 Made Simple; Psychology Press: Hove, UK, 2012. [Google Scholar]
- Ashby, F.G.; Isen, A.M.; Turken, A.U. A neuropsychological theory of positive affect and its influence on cognition. Psychol. Rev. 1999, 106, 529–550. [Google Scholar] [CrossRef]
- Isen, A.M. A role for neuropsychology in understanding the facilitating influence of positive affect on social behavior and cognitive processes. In Oxford Handbook of Positive Psychology, 2nd ed.; Lopez, S., Snyder, C.R., Eds.; Oxford University Press: New York, NY, USA, 2009; pp. 503–518. [Google Scholar]
- Kok, B.E.; Coffey, K.A.; Cohn, M.A.; Catalino, L.I.; Vacharkulksemsuk, T.; Algoe, S.B.; Brantley, M.; Fredrickson, B.L. How positive emotions build physical health: Perceived positive social connections account for the upward spiral between positive emotions and vagal tone. Psychol. Sci. 2013, 24, 1123–1132. [Google Scholar] [CrossRef]
- Fredrickson, B.L. The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. Am. Psychol. 2001, 56, 218. [Google Scholar] [CrossRef]
- Fredrickson, B.L.; Mancuso, R.A.; Branigan, C.; Tugade, M.M. The undoing effect of positive emotions. Motiv. Emot. 2000, 24, 237–258. [Google Scholar] [CrossRef]
- Waugh, C.E.; Muhtadie, L.; Thompson, R.J.; Joormann, J.; Gotlib, I.H. Affective and physiological responses to stress in girls at elevated risk for depression. Dev. Psychopathol. 2012, 24, 661–666. [Google Scholar] [CrossRef]
- Kline, J.P.; Blackhart, G.C.; Williams, W.C. Anterior EEG asymmetries and opponent process theory. Int. J. Psychophysiol. 2007, 63, 302–307. [Google Scholar] [CrossRef]
- Jackson, D.C.; Mueller, C.J.; Dolski, I.; Dalton, K.M.; Nitschke, J.B.; Urry, H.L.; Rosenkranz, M.A.; Ryff, C.D.; Singer, B.H.; Davidson, R.J. Now you feel it, now you don’t: Frontal brain electrical asymmetry and individual differences in emotion regulation. Psychol. Sci. 2003, 14, 612–617. [Google Scholar] [CrossRef]
- Thayer, J.F.; Åhs, F.; Fredrikson, M.; Sollers, J.J.; Wager, T.D. A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health. Neurosci. Biobehav. Rev. 2012, 36, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Thayer, J.F.; Hansen, A.L.; Saus-Rose, E.; Johnsen, B.H. Heart rate variability, prefrontal neural function, and cognitive performance: The neurovisceral integration perspective on self-regulation, adaptation, and health. Ann. Behav. Med. A Publ. Soc. Behav. Med. 2009, 37, 141–153. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sveinsdóttir, S.Þ.; Jóhannsdóttir, K.R. Is Positive Affect as a Trait Related to Higher Heart Rate Variability in a Stressful Situation? Int. J. Environ. Res. Public Health 2023, 20, 6919. https://doi.org/10.3390/ijerph20206919
Sveinsdóttir SÞ, Jóhannsdóttir KR. Is Positive Affect as a Trait Related to Higher Heart Rate Variability in a Stressful Situation? International Journal of Environmental Research and Public Health. 2023; 20(20):6919. https://doi.org/10.3390/ijerph20206919
Chicago/Turabian StyleSveinsdóttir, Sigrún Þóra, and Kamilla Rún Jóhannsdóttir. 2023. "Is Positive Affect as a Trait Related to Higher Heart Rate Variability in a Stressful Situation?" International Journal of Environmental Research and Public Health 20, no. 20: 6919. https://doi.org/10.3390/ijerph20206919
APA StyleSveinsdóttir, S. Þ., & Jóhannsdóttir, K. R. (2023). Is Positive Affect as a Trait Related to Higher Heart Rate Variability in a Stressful Situation? International Journal of Environmental Research and Public Health, 20(20), 6919. https://doi.org/10.3390/ijerph20206919




