Effects of Aircraft Noise on Sleep: Federal Aviation Administration National Sleep Study Protocol
Abstract
1. Introduction
1.1. Effects of Nocturnal Noise Exposure on Sleep and Health
1.2. Field Studies on the Effects of Aircraft Noise on Sleep
1.3. Regulatory Relevance
1.4. Objectives
2. Methodology and Materials
2.1. Study Design
2.1.1. Overview
2.1.2. Study Target Population
2.1.3. Airport Selection and Study Simulation
- Awakening probability attributable to noise at the highest noise levels experienced in the bedroom is typically around 10%. Airports in Germany (Leipzig–Halle) [17] and Canada (Montreal) [27] use one additional awakening induced by nighttime aircraft noise per night as a criterion for limiting or assessing the effects of aircraft noise on sleep. Thus, minimally 10 events per night (50 events per five nights) are needed to reach this threshold. We used the median number of observed aircraft noise events during the five simulated nights for classification.
- For statistical efficiency, instances in which investigated subjects are not exposed to a single aircraft noise event throughout the whole measurement period should be rare in the actual study. Runway ends where >5% of subjects had zero observed events were classified as low-traffic runway ends.
- Low-Traffic Runway Ends: 0 ANEs in the 5th percentile or median of less than 50 ANEs (464 runway ends fell into this category; all runway ends were classified as low traffic at 34 airports)
- Medium-Traffic Runway Ends: More than 0 ANEs in the 5th percentile and a median of 50–99 ANEs (119 runway ends fell into this category; at least one runway end was classified as medium traffic at 44 airports)
- High-Traffic Runway Ends: More than 0 ANEs in the 5th percentile and a median of at least 100 ANEs (83 runway ends fell into this category; at least one runway end was classified as high traffic at 33 airports)
2.2. Sample Size and Power Calculations
2.2.1. Primary Outcome and Assumptions
2.2.2. Simulation Studies to Determine Statistical Power
- Traffic class (all airports, medium and high traffic airports only, high traffic airports only)
- Variance of random effects (type 1: empirical average of all pilot studies, type 2: theoretically set person-specific variance inflation of 20%, type 3: theoretically set person-specific variance inflation of 50%)
- Sampling scheme (uniform, population density by household units)
- Sample size (250, 300, 350, 400, 500)
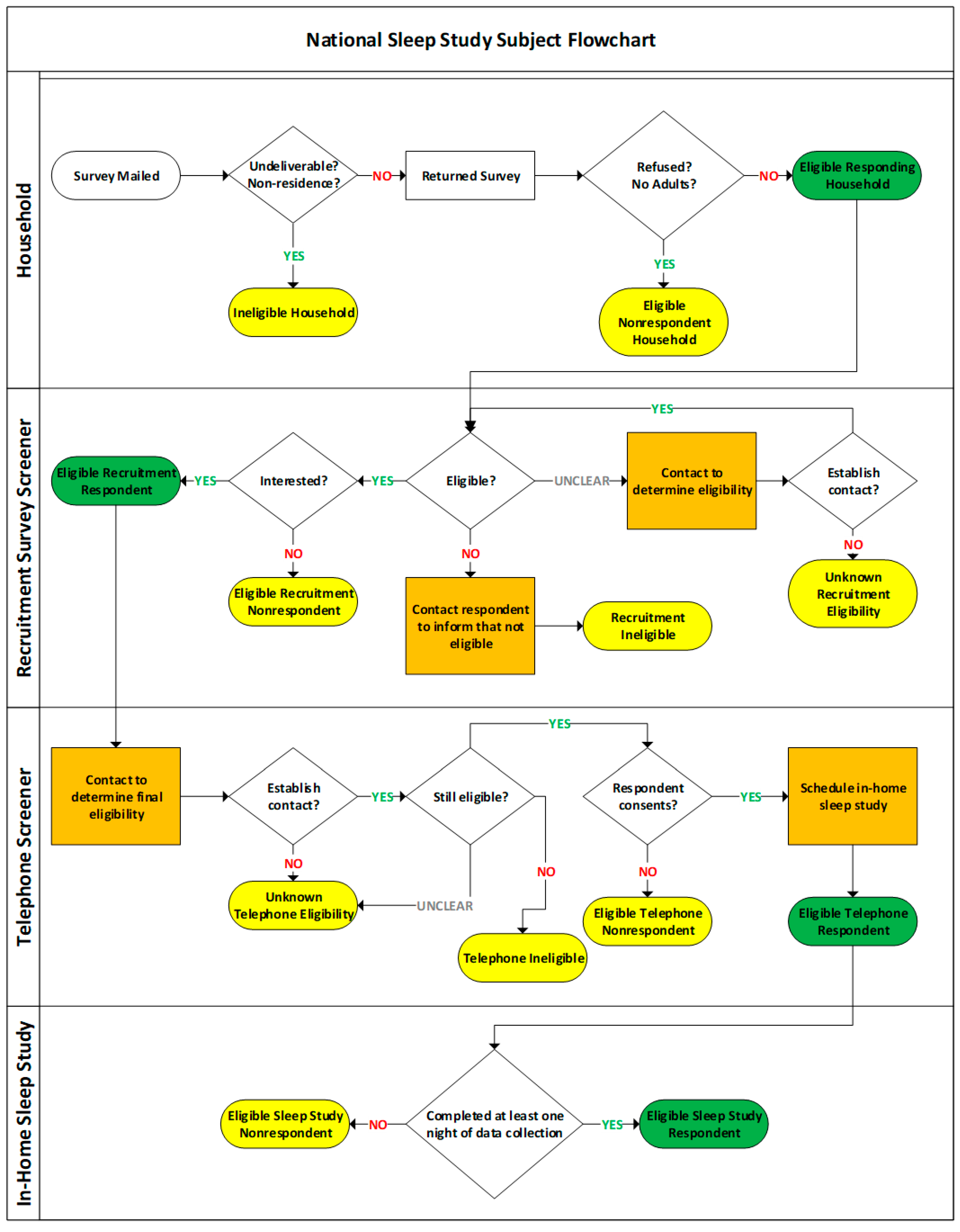
2.3. Subject Enrollment
2.3.1. Eligible Household Selection
2.3.2. Participant Recruitment
2.3.3. Eligibility Criteria
2.4. Field Study
2.4.1. Field Study Data Collection Procedures
- Morningness–Eveningness Questionnaire (MEQ), a standardized method of measuring chronotype [33];
- Pittsburgh Sleep Quality Index (PSQI), a standardized method of measuring sleep quality over the past month [34];
- Additional questions considered relevant but not included in the Recruitment Survey. The questions address noise countermeasures; sleep disturbance by road, rail, industry, construction, neighbors, and air conditioning over the past 12 months; whether the residence received sound proofing treatment; and whether participants use air conditioning in their bedroom. Questions on sleep disturbance are formulated according to standard guidelines described by the International Commission on the Biological Effects of Noise (ICBEN) [37].
2.4.2. Field Study Equipment
Sound Recorder
ECG and Body Movement Monitor
Time Synchronization
2.4.3. Incentives
2.4.4. Ethics
3. Data Analysis
3.1. Processing of Returned Equipment and Field Study Data
3.1.1. Processing of ECG and Movement Data
3.1.2. Processing of Sound Recorder Data
3.2. Aircraft Noise Exposure Metrics
3.3. Statistical Analysis
3.3.1. Primary Outcome
3.3.2. Secondary Outcome
3.3.3. Exploratory Analyses
3.3.4. Weighting
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
Appendix A
- Q1.
- During the last month or so, how would you rate your sleep quality overall?5-point Likert scale with answer categories very good; fairly good; neither good nor bad; fairly bad; very bad
- Q2.
- Select the response that best reflects how often you have taken medicine (prescribed or “over the counter”) to help you sleep during the last month or so.4-point Likert scale with answer categories not during the past month; less than once a week; once or twice a week; three or more times a week
- Q3.
- How strongly do you agree or disagree with the statement “I am sensitive to noise”?5-point Likert scale with answer categories strongly disagree; somewhat disagree; neither agree nor disagree; somewhat agree; strongly agree
- Q4.
- Thinking about the last 12 months or so, when you are here at home, how much does noise from aircraft bother, disturb or annoy you?5-point Likert scale with answer categories not at all; slightly; moderately; very, extremely
- Q5.
- Thinking about the last 12 months or so, when you are here at home, how much does noise from aircraft disturb your sleep?5-point Likert scale with answer categories not at all; slightly; moderately; very, extremely
- Q6.
- Now considering how you feel about everything in your neighborhood, how would you rate your neighborhood as a place to live on a scale from 1 to 5?5-point Likert scale with anchors best (1) and worst (5)
- Q7.
- In general, would you say your health is…?5-point Likert scale with answer categories excellent; very goof; good; fair; poor
- Q8.
- Have you ever been diagnosed by a health professional with any of the following sleep disorders? (Mark all that apply.)Response options: sleep apnea; narcolepsy; restless legs syndrome; periodic limb movement syndrome; insomnia; none; other (please specify)
- Q9.
- Do you have any problems or difficulties with your sense of hearing?Response options: yes; no
- Q10.
- Have you ever been diagnosed by a health professional with any of the following conditions? (Mark all that apply.)Response options: hypertension/high blood pressure; arrhythmia/irregular heart beat; heart disease; diabetes; cancer; none
- Q11.
- What is your current employment status? (Mark one.)Response options: employed (working mostly from home ); employed (working mostly away from home; unemployed/searching for a job; student; retired; homemaker; other
- Q12.
- What is the highest degree or level of school you have completed?Response options: less than high school; high school graduate, including equivalency; some college credit, including Associate’s degree; Bachelor’s degree; graduate or professional degree
- Q13.
- What was your total household income last year?Response options: less than $10,000; $10,000 to $14,999; $15,000 to $24,999; $25,000 to $34,999; $35,000 to $49,999; $50,000 to $74,999; $75,000 to $99,999; $100,000 to $149,999; $150,000 or more
- Q14.
- If currently employed, does your job require overnight shift work? (Overnight shift work refers to work for at least 4 h between 12 midnight to 6 a.m. in the morning.)Response options: yes; no
- Q15.
- What is your ethnicity?Response options: Hispanic or Latino; not Hispanic or Latino
- Q16.
- What is your race? (Mark all that apply.)Response options: American Indian or Alaska Native; Asian; Black or African American; Native Hawaiian or Other Pacific Islander; White; prefer not to answer; other (please specify)
- Q17.
- How long have you lived at your current residence?Response options: less than 1 year; 1 year or more but less than 5 years; 5 to 10 years; more than 10 years
- Q18.
- How many people 21 years of age or older (including yourself) reside in this household?2-digit entry box for age
- Q19.
- Is there someone living in your home that frequently requires your care during the night?Response options: yes; no
- Q20.
- What is your sex?Response options: male; female
- Q21.
- What is your age?2-digit entry box for age
- Q22.
- What is your height?1-digit entry box for feet and 2-digit entry box for inches
- Q23.
- What is your weight?3-digit entry box for pounds (lbs)
- Q24.
- Any other commentsOpen question
- Q25.
- Are you interested in taking part in the in-home sleep study, and do you give your permission for the study team to contact you either by phone or email?Response options: yes; no (input fields for first name, last name, email address, phone # [landline] and phone # [cell] are also provided).
Appendix B
- Study performed around Cologne Bonn airport (STRAIN) in 2001 and 2002 [17]
- Study performed around Frankfurt airport (NORAH) in 2013 [41]
- NSS pilot study performed around Philadelphia International Airport (PHL) in 2014 and 2015 [23]
- NSS pilot study performed around Hartsfield–Jackson Atlanta International Airport (ATL) in 2016 and 2017 [24]
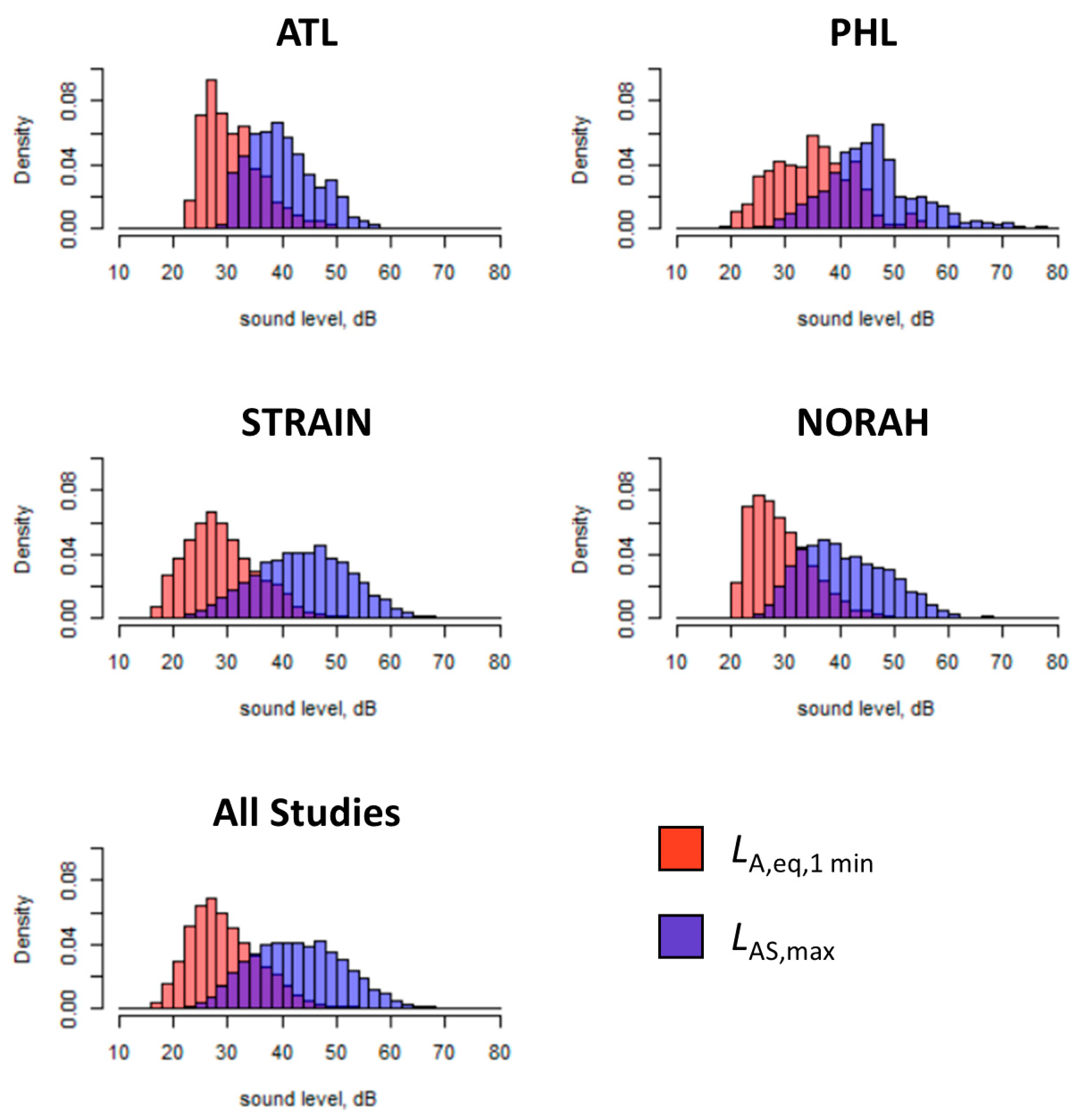
| Pilot | Number of ANEs | Number of Individuals |
|---|---|---|
| STRAIN | 17,058 | 63 |
| NORAH | 8979 | 164 |
| PHL | 2010 | 32 |
| ATL | 1667 | 22 |
| Total | 29,714 | 282 |
| Average | 7428 | 70 |
Appendix C
- Determine the fixed effects coefficients (beta = (β0, β1)) and airport-specific random effects
- Fit Model 0 to ANE data from four pilot studies: ATL, PHL, STRAIN, NORAH. Each pilot study has a beta vector of (β0, β1).
- The distribution of the beta coefficients across the four pilot studies is used to estimate the Model 2 parameters for the sampled airports in the simulation study. For the simulations, each airport will have a set of fixed effect coefficients for Model 2 drawn from a normal distribution, where the mean and covariance matrix are set to be the average value and covariance of those parameters across the four pilot studies.
- The average beta parameter vector is (−4.2586, 0.0434), with estimated SD (0.6328, 0.0134) and covariance(beta) = −0.008430 defining the between-airport random effects. The variance for the (normal) distribution of beta parameters for individuals within an airport is determined by the random effects described in step 2.
- Determine the individual random effects (b = (b0, b1))
- Fit Model 0 to ANE data from four pilot studies: ATL, PHL, STRAIN, NORAH. Each pilot has random effects for intercept (b0) and slope (b1) for each individual. We define varRE to be the covariance matrix for individual random effects (b0,b1)
- The true varRE used for simulations is calculated by using:
- Type 1: the unweighted empirical average of varRE over all pilots The SD for (b0,b1) are (1.6376,0.0363), with covariance −0.0573.
- Type 2: theoretically set variance inflated by 20% of type 1
- Type 3: theoretically set variance inflated by 50% of type 1
- LAS,max was left as a continuous variable and in its original scale.
- Randomly draw (Nind) participants according to one of two sampling strategies:
- Uniform sampling: Sample with replacement Nind rows from the airport/runway sleep study simulation data file (nRWY∗50 weeks∗10 people) to determine the airport, runway, and number of ANEs (nevent) for each of the Nind participants
- Population density-based sampling: Sample Nind runways with each unique runway’s probability of being selected based on its population household unit density. For each of the Nind selected runway, sample from the corresponding airport/runway’s sleep study simulation data file to determine the number of ANEs. Note that population sampling is only available for medium and high traffic runways.
- For each airport in the sample, draw coefficients from the model distribution for the airport-specific coefficients (B0,B1)
- c.
- Mean and variance of this distribution determined by the analysis of the pilot data, as described in step 1 of modeling steps above.
- For each airport in the sample, randomly select which pilot airport the noise profiles will come from.
- d.
- For each person in this airport, sample with replacement a given profile of noise events by randomly sampling a person from the chosen pilot airport data; then sample their nevent_i noise levels from this profile.
- For each person in the sample, generate random effects for b0 and b1.
- e.
- Random effects have a mean of 0 and variance is determined by the selected varRE type: Type 1 (empirical average of all pilot data), Type 2 (theoretically inflated by 20% variance), Type 3 (theoretically inflated by 50% variance), as described in step 2 of modeling steps above.
- Generate the logistic awakening outcome (1 for awakening, 0 otherwise) by flipping a coin with probability determined by Model 2.
- Reduce simulated data by randomly selecting 30%, then randomly delete 5% of Nind subjects to account for potential missing data.
- Fit Model 1 to the remaining dataset to obtain estimated coefficients.
- Save coefficients and other relevant output (e.g., number of ANEs, which airports and runways were selected)}
References
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the american academy of sleep medicine and sleep research society. Sleep 2015, 38, 843–844. [Google Scholar] [CrossRef]
- Muzet, A. Environmental noise, sleep and health. Sleep Med. Rev. 2007, 11, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Fritschi, L.; Brown, A.L.; Kim, R.; Schwela, D.H.; Kephalopoulos, S. Burden of Disease from Environmental Noise; World Health Organization (WHO): Bonn, Germany, 2011. [Google Scholar]
- Kempen, E.V.; Casas, M.; Pershagen, G.; Foraster, M. Who environmental noise guidelines for the european region: A systematic review on environmental noise and cardiovascular and metabolic effects: A summary. Int. J. Environ. Res. Public Health 2018, 15, 379. [Google Scholar] [CrossRef]
- Munzel, T.; Sorensen, M.; Daiber, A. Transportation noise pollution and cardiovascular disease. Nat. Rev. Cardiol. 2021, 18, 619–636. [Google Scholar] [CrossRef] [PubMed]
- Jarup, L.; Babisch, W.; Houthuijs, D.; Pershagen, G.; Katsouyanni, K.; Cadum, E.; Dudley, M.L.; Savigny, P.; Seiffert, I.; Swart, W.; et al. Hypertension and exposure to noise near airports: The hyena study. Environ. Health Perspect. 2008, 116, 329–333. [Google Scholar] [CrossRef]
- Herzog, J.; Schmidt, F.P.; Hahad, O.; Mahmoudpour, S.H.; Mangold, A.K.; Garcia Andreo, P.; Prochaska, J.; Koeck, T.; Wild, P.S.; Sørensen, M.; et al. Acute exposure to nocturnal train noise induces endothelial dysfunction and pro-thromboinflammatory changes of the plasma proteome in healthy subjects. Basic Res. Cardiol. 2019, 114, 46. [Google Scholar] [CrossRef]
- Schmidt, F.P.; Basner, M.; Kroger, G.; Weck, S.; Schnorbus, B.; Muttray, A.; Sariyar, M.; Binder, H.; Gori, T.; Warnholtz, A.; et al. Effect of nighttime aircraft noise exposure on endothelial function and stress hormone release in healthy adults. Eur. Heart J. 2013, 34, 3508–3514. [Google Scholar] [CrossRef]
- Schmidt, F.; Kolle, K.; Kreuder, K.; Schnorbus, B.; Wild, P.; Hechtner, M.; Binder, H.; Gori, T.; Munzel, T. Nighttime aircraft noise impairs endothelial function and increases blood pressure in patients with or at high risk for coronary artery disease. Clin. Res. Cardiol. 2015, 104, 23–30. [Google Scholar] [CrossRef]
- Eriksson, C.; Hilding, A.; Pyko, A.; Bluhm, G.; Pershagen, G.; Ostenson, C.G. Long-term aircraft noise exposure and body mass index, waist circumference, and type 2 diabetes: A prospective study. Environ. Health Perspect. 2014, 122, 687–694. [Google Scholar] [CrossRef]
- Abbott, S.M.; Videnovic, A. Chronic sleep disturbance and neural injury: Links to neurodegenerative disease. Nat. Sci. Sleep 2016, 8, 55–61. [Google Scholar] [PubMed]
- Andersen, Z.J.; Jorgensen, J.T.; Elsborg, L.; Lophaven, S.N.; Backalarz, C.; Laursen, J.E.; Pedersen, T.H.; Simonsen, M.K.; Brauner, E.V.; Lynge, E. Long-term exposure to road traffic noise and incidence of breast cancer: A cohort study. Breast Cancer Res. 2018, 20, 119. [Google Scholar] [CrossRef] [PubMed]
- Roswall, N.; Bidstrup, P.E.; Reaschou-Nielsen, O.; Jensen, S.S.; Overvad, K.; Halkjaer, J.; Sorensen, M. Residential road traffic noise exposure and colorectal cancer survival—A danish cohort study. PLoS ONE 2017, 12, e0187161. [Google Scholar] [CrossRef]
- Roswall, N.; Raaschou-Nielsen, O.; Ketzel, M.; Overvad, K.; Halkjaer, J.; Sorensen, M. Modeled traffic noise at the residence and colorectal cancer incidence: A cohort study. Cancer Causes Control 2017, 28, 745–753. [Google Scholar] [CrossRef] [PubMed]
- Kroller-Schon, S.; Daiber, A.; Steven, S.; Oelze, M.; Frenis, K.; Kalinovic, S.; Heimann, A.; Schmidt, F.P.; Pinto, A.; Kvandova, M.; et al. Crucial role for nox2 and sleep deprivation in aircraft noise-induced vascular and cerebral oxidative stress, inflammation, and gene regulation. Eur. Heart J. 2018, 39, 3528–3539. [Google Scholar] [CrossRef]
- Saucy, A.; Schaffer, B.; Tangermann, L.; Vienneau, D.; Wunderli, J.M.; Roosli, M. Does night-time aircraft noise trigger mortality? A case-crossover study on 24 886 cardiovascular deaths. Eur. Heart J. 2021, 42, 835–843. [Google Scholar] [CrossRef]
- Basner, M.; Isermann, U.; Samel, A. Aircraft noise effects on sleep: Application of the results of a large polysomnographic field study. J. Acoust. Soc. Am. 2006, 119, 2772–2784. [Google Scholar] [CrossRef] [PubMed]
- Passchier-Vermeer, W.; Vos, H.; Steenbekkers, J.H.M.; Van der Ploeg, F.D.; Groothuis-Oudshoorn, K. Sleep Disturbance and Aircraft Noise Exposure—Exposure Effect Relationships; Report 2002.027; TNO: Leiden, The Netherlands, 2002; pp. 1–245. [Google Scholar]
- Fidell, S.; Pearsons, K.; Tabachnick, B.G.; Howe, R. Effects on sleep disturbance of changes in aircraft noise near three airports. J. Acoust. Soc. Am. 2000, 107, 2535–2547. [Google Scholar] [CrossRef]
- Basner, M.; Brink, M.; Elmenhorst, E.M. Critical appraisal of methods for the assessment of noise effects on sleep. Noise Health 2012, 14, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Basner, M.; Griefahn, B.; Müller, U.; Plath, G.; Samel, A. An ecg-based algorithm for the automatic identification of autonomic activations associated with cortical arousal. Sleep 2007, 30, 1349–1361. [Google Scholar] [CrossRef]
- McGuire, S.; Müller, U.; Plath, G.; Basner, M. Refinement and Validation of An Ecg Based Algorithm for Detecting Awakenings. In Proceedings of the 11th International Congress on Noise as a Public Health Problem, Nara, Japan, 1–5 June 2014; International Commission of Biological Effects of Noise (ICBEN): Nara, Japan, 2014. [Google Scholar]
- Basner, M.; Witte, M.; McGuire, S. Aircraft noise effects on sleep—Results of a pilot study near philadelphia international airport. Int. J. Environ. Res. Public Health 2019, 16, 3178. [Google Scholar] [CrossRef]
- Smith, M.G.; Rocha, S.; Witte, M.; Basner, M. On the feasibility of measuring physiologic and self-reported sleep disturbance by aircraft noise on a national scale: A pilot study around atlanta airport. Sci. Total Environ. 2020, 718, 137368. [Google Scholar] [CrossRef] [PubMed]
- Federal Interagency Committee on Noise (FICON). Federal Agency Review of Selected Airport Noise Analysis Issues; FICON: Washington, DC, USA, 1992. [Google Scholar]
- Miller, N.P.; Czech, J.J.; Hellauer, K.M.; Bradley, N.L.; Lohr, S.; Jodts, E.; Broene, P.; Morganstein, D.; Kali, J.; Zhu, X.; et al. Analysis of the Neighborhood Environmental Survey; DOT/FAA/TC-21/4; Federal Aviation Administration; William, J., Ed.; Hughes Technical Center: Springfield, VA, USA, 2021; pp. 1–451. [Google Scholar]
- Tetreault, L.F.; Plante, C.; Perron, S.; Goudreau, S.; King, N.; Smargiassi, A. Risk assessment of aircraft noise on sleep in montreal. Can. J. Public Health 2012, 103, e293–e296. [Google Scholar] [CrossRef] [PubMed]
- Brink, M.; Basner, M.; Schierz, C.; Spreng, M.; Scheuch, K.; Bauer, G.; Stahel, W. Determining physiological reaction probabilities to noise events during sleep. Somnologie 2009, 13, 236–243. [Google Scholar] [CrossRef]
- Weisberg, S. Applied Linear Regression, 3rd ed.; Wiley-Interscience: Hoboken, NJ, USA, 2005; p. p. 310. [Google Scholar]
- Dillman, D.A.; Smyth, J.D.; Christian, L.M. Internet, Phone, Mail, and Mixed-Mode Surveys: The Tailored Design Method, 4th ed.; Wiley: Hoboken, NJ, USA, 2014; p. p. 509. [Google Scholar]
- Smith, M.G.; Witte, M.; Rocha, S.; Basner, M. Effectiveness of incentives and follow-up on increasing survey response rates and participation in field studies. BMC Med. Res. Methodol. 2019, 19, 230. [Google Scholar] [CrossRef]
- Akerstedt, T.; Gillberg, M. Subjective and objective sleepiness in the active individual. Int. J. Neurosci. 1990, 52, 29–37. [Google Scholar] [CrossRef]
- Horne, J.A.; Ostberg, O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int. J. Chronobiol. 1976, 4, 97–110. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Schutte, M.; Marks, A.; Wenning, E.; Griefahn, B. The development of the noise sensitivity questionnaire. Noise Health 2007, 9, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Griefahn, B. Determination of noise sensitivity within an internet survey using a reduced version of the noise sensitivity questionnaire. J. Acoust. Soc. Am. 2008, 123, 3449. [Google Scholar] [CrossRef]
- Fields, J.M.; De Jong, R.G.; Gjestland, T.; Flindell, I.H.; Job, R.F.S.; Kurra, S.; Lercher, P.; Vallet, M.; Yano, T.; Guski, R.; et al. Standardized general-purpose noise reaction questions for community noise surveys: Research and a recommendation. J. Sound Vib. 2001, 242, 641–679. [Google Scholar] [CrossRef]
- Kwon, O.; Jeong, J.; Kim, H.B.; Kwon, I.H.; Park, S.Y.; Kim, J.E.; Choi, Y. Electrocardiogram sampling frequency range acceptable for heart rate variability analysis. Healthc. Inform. Res. 2018, 24, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Edwards, P.J.; Roberts, I.; Clarke, M.J.; DiGuiseppi, C.; Wentz, R.; Kwan, I.; Cooper, R.; Felix, L.M.; Pratap, S. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst. Rev. 2009. [Google Scholar] [CrossRef] [PubMed]
- Church, A.H. Estimating the effect of incentives on mail survey response rates—A metaanalysis. Public Opin. Q. 1993, 57, 62–79. [Google Scholar] [CrossRef]
- Schreckenberg, D.; Eikmann, T.; Faulbaum, F.; Haufe, E.; Herr, C.; Klatte, M.; Meis, M.; Möhler, U.; Müller, U.; Schmitt, J.; et al. Norah—Study on Noise Related Annoyance, Cognition and Health: A Transportation Noise Effects Monitoring Program in Germany; ICBEN: London, UK; International Commission of Biological Effects of Noise: London, UK, 2011. [Google Scholar]



| Traffic | Sampling | Variance | Sample Size | ||||
|---|---|---|---|---|---|---|---|
| 250 | 300 | 350 | 400 | 500 | |||
| L, M, H | U | 1 | 0.0197 | 0.0189 | 0.0166 | 0.0161 | 0.0146 |
| M, H | U | 1 | 0.0149 | 0.0138 | 0.0127 | 0.0125 | 0.0106 |
| H | U | 1 | 0.0142 | 0.0132 | 0.0127 | 0.0113 | 0.0109 |
| M, H | P | 1 | 0.0153 | 0.0146 | 0.0132 | 0.0127 | 0.0111 |
| H | P | 1 | 0.0147 | 0.0145 | 0.0131 | 0.0124 | 0.0119 |
| M, H | P | 2 | 0.0161 | 0.0147 | 0.0142 | 0.0135 | 0.0121 |
| H | P | 2 | 0.0155 | 0.0151 | 0.0140 | 0.0139 | 0.0123 |
| M, H | P | 3 | 0.0168 | 0.0158 | 0.0151 | 0.0143 | 0.0129 |
| H | P | 3 | 0.0176 | 0.0162 | 0.0149 | 0.0149 | 0.0131 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Basner, M.; Barnett, I.; Carlin, M.; Choi, G.H.; Czech, J.J.; Ecker, A.J.; Gilad, Y.; Godwin, T.; Jodts, E.; Jones, C.W.; et al. Effects of Aircraft Noise on Sleep: Federal Aviation Administration National Sleep Study Protocol. Int. J. Environ. Res. Public Health 2023, 20, 7024. https://doi.org/10.3390/ijerph20217024
Basner M, Barnett I, Carlin M, Choi GH, Czech JJ, Ecker AJ, Gilad Y, Godwin T, Jodts E, Jones CW, et al. Effects of Aircraft Noise on Sleep: Federal Aviation Administration National Sleep Study Protocol. International Journal of Environmental Research and Public Health. 2023; 20(21):7024. https://doi.org/10.3390/ijerph20217024
Chicago/Turabian StyleBasner, Mathias, Ian Barnett, Michele Carlin, Grace H. Choi, Joseph J. Czech, Adrian J. Ecker, Yoni Gilad, Thomas Godwin, Eric Jodts, Christopher W. Jones, and et al. 2023. "Effects of Aircraft Noise on Sleep: Federal Aviation Administration National Sleep Study Protocol" International Journal of Environmental Research and Public Health 20, no. 21: 7024. https://doi.org/10.3390/ijerph20217024
APA StyleBasner, M., Barnett, I., Carlin, M., Choi, G. H., Czech, J. J., Ecker, A. J., Gilad, Y., Godwin, T., Jodts, E., Jones, C. W., Kaizi-Lutu, M., Kali, J., Opsomer, J. D., Park-Chavar, S., Smith, M. G., Schneller, V., Song, N., & Shaw, P. A. (2023). Effects of Aircraft Noise on Sleep: Federal Aviation Administration National Sleep Study Protocol. International Journal of Environmental Research and Public Health, 20(21), 7024. https://doi.org/10.3390/ijerph20217024







