Modelling the Predictors of Mobile Health (mHealth) Adoption among Healthcare Professionals in Low-Resource Environments
Abstract
:1. Introduction
1.1. Mobile Health Applications
1.2. Theoretical Framework and the Process of Hypotheses Development
1.2.1. Performance Expectancy (PE)
1.2.2. Effort Expectancy (EE)
1.2.3. Social Influence (SI)
1.2.4. Self-Concept (SC)
1.2.5. Facilitating Conditions (FCs)
1.2.6. Behavioral Intention (BI)
1.3. Objectives of the Study
2. Materials and Methods
2.1. Participants and Procedure
2.2. Research Tool
2.3. Data Collection and Analysis Procedure
3. Results
3.1. Demographic Information
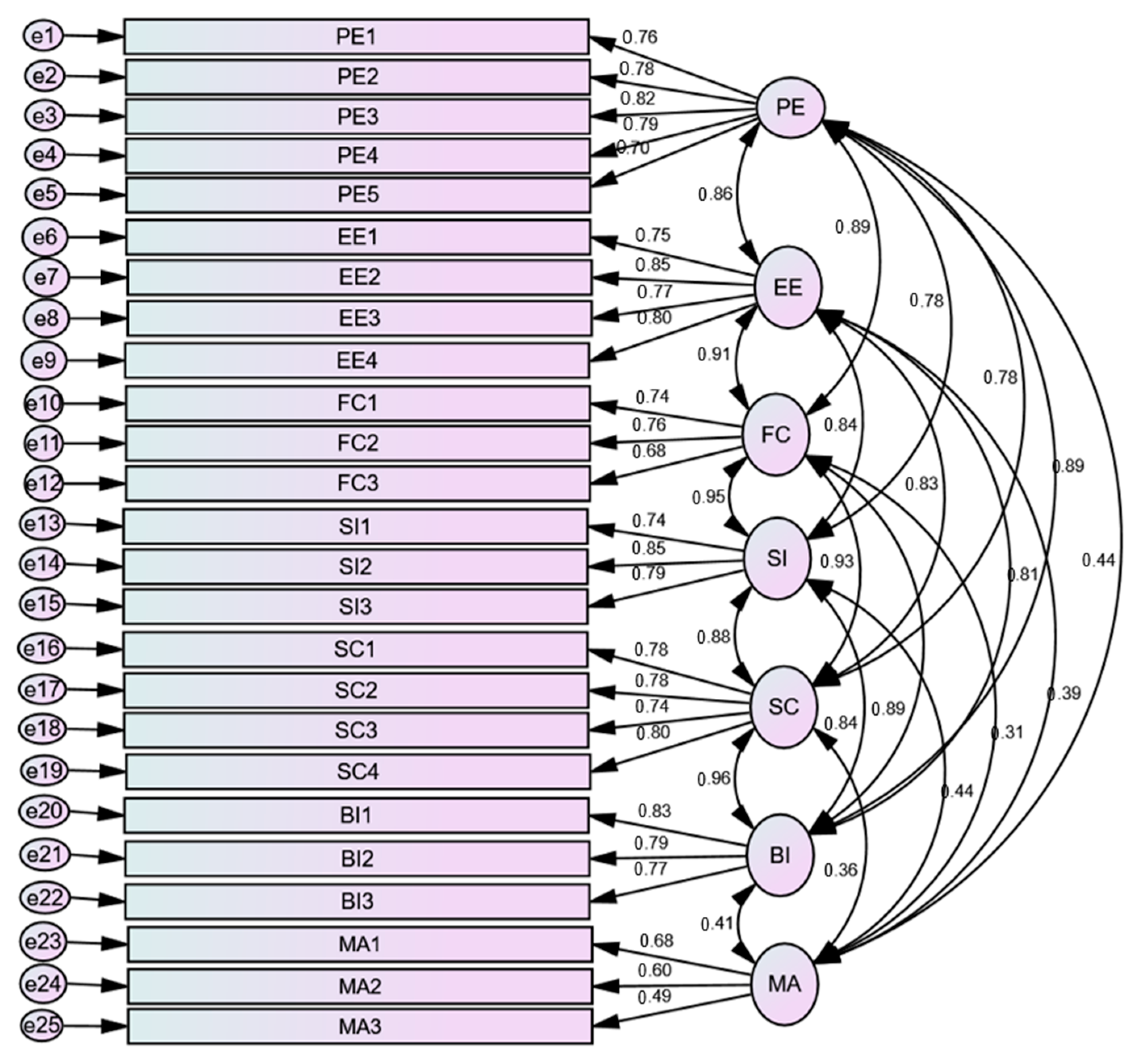
3.2. Confirmatory Factor Analysis
3.2.1. Regression Weights
3.2.2. Estimation of Correlation
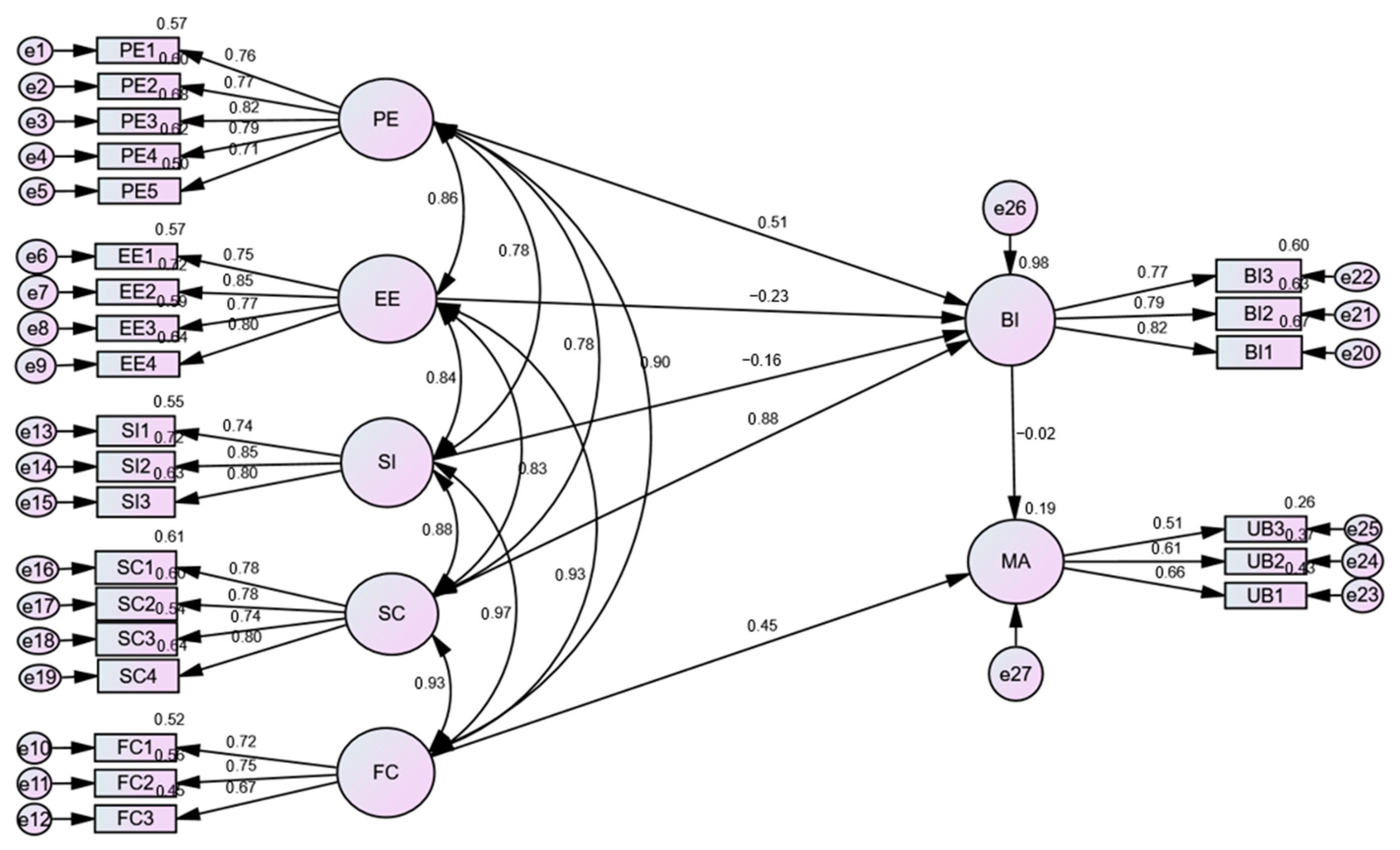
3.3. Structural Equation Model
3.3.1. Multiple Squared Correlations
3.3.2. Standardized Direct, Indirect, and Total Effects
3.3.3. Model Fit Indices
3.4. Moderating Effect of Gender, Age, and Experience
3.4.1. Moderating Effect of Age
3.4.2. Moderating Effect of Gender
3.4.3. Moderating Effect of Experience
3.5. Estimation of Regression Weights and Validation of the Hypotheses
4. Discussion
4.1. Moderating Effect of Gender, Age, and Experience
4.2. Limitations of the Study
4.3. Implications of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Items under Seven Constructs of the UTAUT
| Construct | Items | Measure | Sources |
| Performance Expectancy (PE) | PE1 | I find mHealth useful in my daily life. | [26,29,77] |
| PE2 | I think mHealth can help in providing timely medical advice to patients | ||
| PE3 | I think mHealth can help in accomplishing daily tasks more quickly. | ||
| PE4 | I think adopting mHealth can increase my clinical performance. | ||
| PE5 | I think mHealth can reduce a considerable amount of hospital expenses on the provision of healthcare | ||
| PE6 | I think mHealth application allows healthcare professionals to be easily accessible and thereby enhances patient experience. | ||
| Effort Expectancy (EE) | EE1 | I think learning how to monitor health issues through mHealth is easy | [33] |
| EE2 | I think my interaction with patients through mHealth app is clear and understandable | ||
| EE3 | I think mHealth apps are easy to use | ||
| EE4 | I think I do not need any effort to use mHealth for patient care | ||
| EE5 | I think it is easy to learn how to use mHealth to receive, track, and evaluate medical data | ||
| Social Influence (SI) | SI1 | People who influence my behavior think that I should use mHealth for clinical practice | [42] |
| SI2 | People whose opinions that I value prefer that I use mHealth for clinical practice | ||
| SI3 | Professionals in my community who use mHealth are more informed and active than those who do not | ||
| SI4 | My mentors and senior professionals encourage me to use mHealth for providing patient care. | ||
| Self-Concept (SC) | SC1 | I think the application of mHealth is necessary for clinical practice | [64] |
| SC2 | I think there is strong evidence that supports the use of mHealth in order to improve the quality of patient care | ||
| SC3 | I feel adherence to mHealth characteristics. | ||
| SC4 | I think my personal behavior is compatible with the mHealth image. | ||
| SC5 | I think mHealth can help in monitoring patients, issuing diagnoses, and treating diseases. | ||
| Facilitating Conditions (FCs) | FC1 | I think I have access to the secured and trusted resources necessary to practice mHealth. | [27,77,78] |
| FC2 | I think I have gathered the knowledge necessary to use mHealth. | ||
| FC3 | I think I can get help from my colleagues when I have difficulties using mHealth. | ||
| FC4 | I think our hospital encourages and facilitates the use of mHealth | ||
| Behavioral Intention (BI) | BI1 | I intend to use mHealth in the future | [79] |
| BI2 | I am interested in r improving the skills necessary to incorporate mHealth into clinical practice | ||
| BI3 | If I need to check patients from rural areas for health-related issue, I intend to use mHealth. | ||
| BI4 | If mHealth brings convenience to my patients, I am willing to continue using it | ||
| BI5 | I intend to inform my colleagues and other healthcare professionals to use mHealth | ||
| mHealth Adoption for Healthcare | AD1 | I think adopting mHealth service will be a pleasant experience | [63,65,67,80] |
| AD2 | I think mHealth can provide an opportunity to respond patients more quickly | ||
| AD3 | I spend a lot of time on using mHealth applications | ||
| AD4 | I think adapting mHealth can enable faster access to patient data. | ||
| AD5 | I frequently use mHealth services. |
References
- Handayani, P.W.; Hidayanto, A.N.; Budi, I. User Acceptance Factors of Hospital Information Systems and Related Technologies: Systematic Review. Inform. Health Soc. Care 2018, 43, 401–426. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Available online: https://www.who.int/ (accessed on 23 August 2023).
- Nacinovich, M. Defining MHealth. J. Commun. Healthc. 2013, 4, 1–3. [Google Scholar] [CrossRef]
- Silva, B.M.C.; Rodrigues, J.J.P.C.; de la Torre Díez, I.; López-Coronado, M.; Saleem, K. Mobile-Health: A Review of Current State in 2015. J. Biomed. Inform. 2015, 56, 265–272. [Google Scholar] [CrossRef]
- Akter, S.; Ray, P. MHealth—An Ultimate Platform to Serve the Unserved. Yearb. Med. Inform. 2010, 19, 94–100. [Google Scholar] [CrossRef]
- O’Donnell, O. Access to Health Care in Developing Countries: Breaking down Demand Side Barriers. Cad. Saude Publica 2007, 23, 2820–2834. [Google Scholar] [CrossRef] [PubMed]
- Latif, S.; Rana, R.; Qadir, J.; Ali, A.; Imran, M.A.; Younis, M.S. Mobile Health in the Developing World: Review of Literature and Lessons from a Case Study. IEEE Access 2017, 5, 11540–11556. [Google Scholar] [CrossRef]
- Mackert, M.; Ball, J.; Lopez, N. Health Literacy Awareness Training for Healthcare Workers: Improving Knowledge and Intentions to Use Clear Communication Techniques. Patient Educ. Couns. 2011, 85, e225–e228. [Google Scholar] [CrossRef] [PubMed]
- Ivatury, G.; Moore, J.; Bloch, A. A Doctor in Your Pocket: Health Hotlines in Developing Countries. Innov. Technol. Gov. Glob. 2009, 4, 119–153. [Google Scholar] [CrossRef]
- Hall, C.S.; Fottrell, E.; Wilkinson, S.; Byass, P. Assessing the Impact of MHealth Interventions in Low- and Middle-Income Countries—What Has Been Shown to Work? Glob. Health Action 2014, 7, 25606. [Google Scholar] [CrossRef] [PubMed]
- Andrade, R.; von Wangenheim, A.; Bortoluzzi, M.K. Wireless and PDA: A Novel Strategy to Access DICOM-Compliant Medical Data on Mobile Devices. Int. J. Med. Inform. 2003, 71, 157–163. [Google Scholar] [CrossRef]
- Castaño, P.M.; Westhoff, C.; Martínez, R.A.; Lara, M. The Effect of Daily Text Message Reminders on Adolescent Oral Contraceptive Pill Continuation. J. Adolesc. Health 2009, 44, S23. [Google Scholar] [CrossRef]
- Ali, R.; Zhang, Z.; Soomro, M.B. Smoking-Cessation Acceptance Via Mobile Health and Quick Response Code Technologies: Empirical Evidence of a Pilot Study from China and Pakistan. Curr. Psychol. 2021, 40, 6085–6097. [Google Scholar] [CrossRef]
- Lee, S.; Chib, A.; Kim, J.N. Midwives’ Cell Phone Use and Health Knowledge in Rural Communities. J. Health Commun. 2011, 16, 1006–1023. [Google Scholar] [CrossRef] [PubMed]
- Kaunda-Khangamwa, B.N.; Steinhardt, L.C.; Rowe, A.K.; Gumbo, A.; Moyo, D.; Nsona, H.; Troell, P.; Zurovac, D.; Mathanga, D. The Effect of Mobile Phone Text Message Reminders on Health Workers’ Adherence to Case Management Guidelines for Malaria and Other Diseases in Malawi: Lessons from Qualitative Data from a Cluster-Randomized Trial. Malar. J. 2018, 17, 481. [Google Scholar] [CrossRef] [PubMed]
- PATIL, D.D.A. Mobile for Health (MHealth) in Developing Countries: Application of 4 Ps of Social Marketing. J. Health Inform. Dev. Ctries. 2011, 5, 317–326. [Google Scholar]
- Ehsanur Rahman, A.; Mhajabin, S.; Dockrell, D.; Nair, H.; El Arifeen, S.; Campbell, H. Managing Pneumonia through Facility-Based Integrated Management of Childhood Management (IMCI) Services: An Analysis of the Service Availability and Readiness among Public Health Facilities in Bangladesh. BMC Health Serv. Res. 2021, 1, 667. [Google Scholar] [CrossRef]
- Albabtain, A.F.; Almulhim, D.A.; Yunus, F.; Househ, M.S. The Role of Mobile Health in the Developing World: A Review of Current Knowledge and Future Trends. J. Sel. Areas Health Informatics 2014, 4, 10–15. [Google Scholar]
- El-Rashidy, N.; El-Sappagh, S.; Riazul Islam, S.M.; El-Bakry, H.M.; Abdelrazek, S. Mobile Health in Remote Patient Monitoring for Chronic Diseases: Principles, Trends, and Challenges. Diagnostics 2021, 11, 607. [Google Scholar] [CrossRef]
- Sidney, K.; Antony, J.; Rodrigues, R.; Arumugam, K.; Krishnamurthy, S.; D’Souza, G.; De Costa, A.; Shet, A. Supporting Patient Adherence to Antiretrovirals Using Mobile Phone Reminders: Patient Responses from South India. AIDS Care–Psychol. Socio-Medical Asp. AIDS/HIV 2012, 24, 612–617. [Google Scholar] [CrossRef]
- Cole-Lewis, H.; Kershaw, T. Text Messaging as a Tool for Behavior Change in Disease Prevention and Management. Epidemiol. Rev. 2010, 32, 56–69. [Google Scholar] [CrossRef]
- Fjeldsoe, B.S.; Marshall, A.L.; Miller, Y.D. Behavior Change Interventions Delivered by Mobile Telephone Short-Message Service. Am. J. Prev. Med. 2009, 36, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Krishna, S.; Boren, S.A.; Balas, E.A. Healthcare via Cell Phones: A Systematic Review. Telemed e-Health 2009, 15, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Lim, M.S.C.; Hocking, J.S.; Hellard, M.E.; Aitken, C.K. SMS STI: A Review of the Uses of Mobile Phone Text Messaging in Sexual Health. Int. J. STD AIDS 2008, 19, 287–290. [Google Scholar] [CrossRef] [PubMed]
- Mohammadzadeh, N.; Safdari, R. Patient Monitoring in Mobile Health: Opportunities and Challenges. Med. Arh. 2014, 68, 57–60. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The Theory of Planned Behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Rogers, E.M. Diffuison of Innovations; Free Press: New York, NY, USA, 1995; pp. 1–20. [Google Scholar]
- Bandura, A. Social Cognitive Theory of Self-Regulation. Organ. Behav. Hum. Decis. Process. 1991, 50, 248–287. [Google Scholar] [CrossRef]
- MASLOW, A.H. Preface to Motivation Theory. Psychosom. Med. 1943, 5, 85–92. [Google Scholar] [CrossRef]
- Thompson, R.L.; Higgins, C.A.; Howell, J.M. Personal Computing: Toward a Conceptual Model of Utilization. MIS Q. 1991, 15, 125–143. [Google Scholar] [CrossRef]
- Ryan, B.; Gross, N.C. The Diffusion of Hybrid Seed Corn in Two Iowa Communities. Rural Sociol. 1943, 8, 15. [Google Scholar]
- Ajzen, I.; Fishbein, M. Attitude-Behavior Relations: A Theoretical Analysis and Review of Empirical Research. Psychol. Bull. 1977, 84, 888–918. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. Manag. Inf. Syst. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Williams, M.; Rana, N.; Dwivedi, Y.; Lal, B. Is Utaut Really Used Or Just Cited For The Sake Of It? A Systematic Review Of Citations Of Utaut’s Originating Article. In Proceedings of the European Conference on Information Systems, Helsinki, Finland, 9–10 June 2011; Available online: https://aisel.aisnet.org/ecis2011/231 (accessed on 20 April 2023).
- Alharbi, S.T. Trust and Acceptance of Cloud Computing: A Revised UTAUT Model. In Proceedings of the 2014 International Conference on Computational Science and Computational Intelligence, Las Vegas, NV, USA, 10–13 March 2014; pp. 131–134. [Google Scholar] [CrossRef]
- Wu, Y.L.; Tao, Y.H.; Yang, P.C. Using UTAUT to Explore the Behavior of 3G Mobile Communication Users. In Proceedings of the IEEE International Conference on Industrial Engineering and Engineering Management, Singapore, 2–4 December 2007; pp. 199–203. [Google Scholar] [CrossRef]
- Chib, A.; Van Velthoven, M.H.; Car, J. MHealth Adoption in Low-Resource Environments: A Review of the Use of Mobile Healthcare in Developing Countries. J. Health Commun. 2015, 20, 4–34. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.L.; Higgins, C.A.; Howell, J.M. Influence of Experience on Personal Computer Utilization: Testing a Conceptual Model. J. Manag. Inf. Syst. 1994, 11, 167–187. [Google Scholar] [CrossRef]
- Alaiad, A.; Alsharo, M.; Alnsour, Y. The Determinants of M-Health Adoption in Developing Countries: An Empirical Investigation. Appl. Clin. Inform. 2019, 10, 820–840. [Google Scholar] [CrossRef]
- Hoque, R.; Sorwar, G. Understanding Factors Influencing the Adoption of MHealth by the Elderly: An Extension of the UTAUT Model. Int. J. Med. Inform. 2017, 101, 75–84. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. Dead or Alive? The Development, Trajectory and Future of Technology Adoption Research. J. AIS 2003, 8, 267–286. [Google Scholar] [CrossRef]
- Gao, Y.; Li, H.; Luo, Y. An Empirical Study of Wearable Technology Acceptance in Healthcare. Ind. Manag. Data Syst. 2015, 115, 1704–1723. [Google Scholar] [CrossRef]
- Bandura, A. Social Cognitive Theory: An Agentic Perspective. Annu. Rev. Psychol. 2003, 52, 1–26. [Google Scholar] [CrossRef]
- Bawack, R.E.; Kala Kamdjoug, J.R. Adequacy of UTAUT in Clinician Adoption of Health Information Systems in Developing Countries: The Case of Cameroon. Int. J. Med. Inform. 2018, 109, 15–22. [Google Scholar] [CrossRef]
- Liang, Y.; Qi, G.; Wei, K.; Chen, J. Exploring the Determinant and Influence Mechanism of E-Government Cloud Adoption in Government Agencies in China. Gov. Inf. Q. 2017, 34, 481–495. [Google Scholar] [CrossRef]
- Chau, P.Y.K.; Tam, K.Y. Factors Affecting the Adoption of Open Systems: An Exploratory Study. MIS Q. Manag. Inf. Syst. 1997, 21, 1–20. [Google Scholar] [CrossRef]
- Ramdani, B.; Chevers, D.; Williams, D.A. SMEs’ Adoption of Enterprise Applications: A Technology-Organisation-Environment Model. J. Small Bus. Enterp. Dev. 2013, 20, 735–753. [Google Scholar] [CrossRef]
- Zhu, K.; Dong, S.; Xu, S.X.; Kraemer, K.L. Innovation Diffusion in Global Contexts: Determinants of Post-Adoption Digital Transformation of European Companies. Eur. J. Inf. Syst. 2006, 15, 601–616. [Google Scholar] [CrossRef]
- Nadri, H.; Rahimi, B.; Afshar, H.L.; Samadbeik, M.; Garavand, A. Factors Affecting Acceptance of Hospital Information Systems Based on Extended Technology Acceptance Model: A Case Study in Three Paraclinical Departments. Appl. Clin. Inform. 2018, 9, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, C.H.; Tang, K.Y. Explaining Undergraduates’ Behavior Intention of e-Textbook Adoption: Empirical Assessment of Five Theoretical Models. Libr. Hi Tech. 2014, 32, 139–163. [Google Scholar] [CrossRef]
- Nkosi, M.T.; Mekuria, F. Cloud Computing for Enhanced Mobile Health Applications. In Proceedings of the2010 IEEE Second International Conference on Cloud Computing Technology and Science, Indianapolis, IN, USA, 30 November–3 December 2010; pp. 629–633. [Google Scholar] [CrossRef]
- Chiu, C.M.; Wang, E.T.G. Understanding Web-Based Learning Continuance Intention: The Role of Subjective Task Value. Inf. Manag. 2008, 45, 194–201. [Google Scholar] [CrossRef]
- Heselmans, A.; Aertgeerts, B.; Donceel, P.; Geens, S.; Van De Velde, S.; Ramaekers, D. Family Physicians’ Perceptions and Use of Electronic Clinical Decision Support during the First Year of Implementation. J. Med. Syst. 2012, 36, 3677–3684. [Google Scholar] [CrossRef]
- Yi, M.Y.; Jackson, J.D.; Park, J.S.; Probst, J.C. Understanding Information Technology Acceptance by Individual Professionals: Toward an Integrative View. Inf. Manag. 2006, 43, 350–363. [Google Scholar] [CrossRef]
- Burney, A.; Abbas, Z.; Mahmood, N.; Arifeen, Q. Prospects for Mobile Health in Pakistan and Other Developing Countries. Adv. Internet Things 2013, 3, 27–32. [Google Scholar] [CrossRef]
- Nishtar, S.; Bhutta, Z.A.; Jafar, T.H.; Ghaffar, A.; Akhtar, T.; Bengali, K.; Isa, Q.A.; Rahim, E. Health Reform in Pakistan: A Call to Action. Lancet 2013, 381, 2291–2297. [Google Scholar] [CrossRef]
- Hair, J.; Black, W.; Babin, B.; Anderson, R.; Tatham, R. Multivariate Data Analysis, 6th ed.; Pearson Prentice Hall: Upper Saddle River, NJ, USA, 2006; Available online: https://www.scirp.org/(S(351jmbntvnsjt1aadkposzje))/reference/ReferencesPapers.aspx?ReferenceID=1385913 (accessed on 30 August 2023).
- Sun, Y.; Wang, N.; Guo, X.; Peng, Z. Understanding the Acceptance of Mobile Health Services: A Comparison and Integration of Alternative Models. J. Electron. Commer. Res. 2013, 14, 183–200. [Google Scholar]
- Petersen, F.; Jacobs, M.; Pather, S. Barriers for User Acceptance of Mobile Health Applications for Diabetic Patients: Applying the UTAUT Model. In Conference on e-Business, e-Services and e-Society; Springer International Publishing: Cham, Switzerland, 2020; Volume 12067, pp. 61–72. [Google Scholar] [CrossRef]
- Tian, X.F.; Wu, R.Z. Determinants of the Mobile Health Continuance Intention of Elders with Chronic Diseases: An Integrated Framework of ECM-ISC and UTAUT. Int. J. Environ. Res. Public Health 2022, 19, 9980. [Google Scholar] [CrossRef] [PubMed]
- Garavand, A.; Samadbeik, M.; Nadri, H.; Rahimi, B.; Asadi, H. Effective Factors in Adoption of Mobile Health Applications between Medical Sciences Students Using the UTAUT Model. Methods Inf. Med. 2019, 58, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Semiz, B.B.; Semiz, T. Examining Consumer Use of Mobile Health Applications by the Extended UTAUT Model. Bus. Manag. Stud. An Int. J. 2021, 9, 267–281. [Google Scholar] [CrossRef]
- Ndayizigamiye, P.; Maharaj, M. Mobile Health Adoption in Burundi: A UTAUT Perspective. In Proceedings of the 2016 IEEE Global Humanitarian Technology Conference (GHTC), Seattle, WA, USA, 13–16 October 2016; pp. 613–623. [Google Scholar] [CrossRef]
- Dwivedi, Y.K.; Shareef, M.A.; Simintiras, A.C.; Lal, B.; Weerakkody, V. A Generalised Adoption Model for Services: A Cross-Country Comparison of Mobile Health (m-Health). Gov. Inf. Q. 2016, 33, 174–187. [Google Scholar] [CrossRef]
- Cao, J.; Kurata, K.; Lim, Y.; Sengoku, S.; Kodama, K. Social Acceptance of Mobile Health among Young Adults in Japan: An Extension of the UTAUT Model. Int. J. Environ. Res. Public Health 2022, 19, 15156. [Google Scholar] [CrossRef]
- Alam, M.Z.; Hu, W.; Hoque, M.R.; Kaium, M.A. Adoption Intention and Usage Behavior of MHealth Services in Bangladesh and China: A Cross-Country Analysis. Int. J. Pharm. Healthc. Mark. 2020, 14, 37–60. [Google Scholar] [CrossRef]
- Zhao, Y.; Ni, Q.; Zhou, R. What Factors Influence the Mobile Health Service Adoption? A Meta-Analysis and the Moderating Role of Age. Int. J. Inf. Manag. 2018, 43, 342–350. [Google Scholar] [CrossRef]
- Ifinedo, P. Technology Acceptance by Health Professionals in Canada: An Analysis with a Modified UTAUT Model. In Proceedings of the 2012 45th Hawaii International Conference on System Sciences, Maui, HI, USA, 4–7 January 2012; pp. 2937–2946. [Google Scholar] [CrossRef]
- Ami-Narh, J.T.; Williams, P.A.H. Journal of Computing::A Revised UTAUT Model to Investigate E-Health Acceptance of Health Professionals in Africa. J. Emerg. Trends Comput. Inf. Sci. 2012, 3, 1383–1391. [Google Scholar]
- Phichitchaisopa, N.; Naenna, T. Factors Affecting the Adoption of Healthcare Information Technology. EXCLI J. 2013, 12, 413. [Google Scholar]
- Hennington, A.; Janz, B.D.; And Janz, B.D.; Hennington, A.H. Information Systems and Healthcare XVI: Physician Adoption of Electronic Medical Records: Applying the UTAUT Model in a Healthcare Context. Commun. Assoc. Inf. Syst. 2007, 19, 60–80. [Google Scholar] [CrossRef]
- Kruger, J.; Dunning, D. Unskilled and Unaware of It: How Difficulties in Recognizing One’s Own Incompetence Lead to Inflated Self-Assessments. J. Pers. Soc. Psychol. 1999, 77, 1121–1134. [Google Scholar] [CrossRef] [PubMed]
- Canady, B.E.; Larzo, M. Overconfidence in Managing Health Concerns: The Dunning–Kruger Effect and Health Literacy. J. Clin. Psychol. Med. Settings 2023, 30, 460–468. [Google Scholar] [CrossRef] [PubMed]
- Hassanaly, P.; Dufour, J.C. Analysis of the Regulatory, Legal, and Medical Conditions for the Prescription of Mobile Health Applications in the United States, the European Union, and France. Med. Devices Evid. Res. 2021, 14, 389–409. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.A.; Tsuji, K. Bridging Digital Divide in Bangladesh: Study on Community Information Centers. Electron. Libr. 2011, 29, 506–522. [Google Scholar] [CrossRef]
- Jacob, C.; Sanchez-Vazquez, A.; Ivory, C. Understanding Clinicians’ Adoption of Mobile Health Tools: A Qualitative Review of the Most Used Frameworks. JMIR mHealth uHealth 2020, 8, e18072. [Google Scholar] [CrossRef]
- Kijsanayotin, B.; Pannarunothai, S.; Speedie, S.M. Factors Influencing Health Information Technology Adoption in Thailand’s Community Health Centers: Applying the UTAUT Model. Int. J. Med. Inform. 2009, 78, 404–416. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Miguel Cruz, A.; Rios Rincon, A.; Buttar, V.; Ranson, Q.; Goertzen, D. What Factors Determine Therapists’ Acceptance of New Technologies for Rehabilitation-a Study Using the Unified Theory of Acceptance and Use of Technology (UTAUT). Disabil. Rehabil. 2015, 37, 447–455. [Google Scholar] [CrossRef]
- Taylor, S.; Todd, P.A. Understanding Information Technology Usage: A Test of Competing Models. Inf. Syst. Res. 1995, 6, 144–176. [Google Scholar] [CrossRef]
- Dou, K.; Yu, P.; Deng, N.; Liu, F.; Guan, Y.; Li, Z.; Ji, Y.; Du, N.; Lu, X.; Duan, H. Patients’ Acceptance of Smartphone Health Technology for Chronic Disease Management: A Theoretical Model and Empirical Test. JMIR mHealth uHealth 2017, 5, e177. [Google Scholar] [CrossRef]

| Types of Service | Description |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
| Types of App | Description |
|---|---|
| Marham | The healthcare application Marham allows communication between patients and physicians. The app’s users can use it to locate doctors, make appointments, and obtain medical guidance. It also provides information about hospitals and medical specialties. It has over one million users. https://play.google.com/store/apps/details?id=controllers.marham.marhammed&pcampaignid=web_share (accessed on 16 November 2023) |
| MyDoctor.pk | The MyDoctor.pk app gives access to a network of doctors and enables them to schedule appointments, communicate with doctors, and examine their medical records. It has over ten thousand users. https://play.google.com/store/apps/details?id=com.doctor.findmydoctor&pcampaignid=web_share (accessed on 16 November 2023) |
| Oladoc | The Oladoc platform allows users to search for and schedule appointments with doctors, dentists, and other healthcare providers. It has over one million users. https://play.google.com/store/apps/details?id=com.mediconnect.oladoc&pcampaignid=web_share (accessed on 16 November 2023) |
| Pak Blood | Pak Blood helps people in finding nearby blood donors during emergencies. Through the app, users may connect with potential donors and request blood donations. It has over ten thousand users. https://play.google.com/store/apps/details?id=com.bloodbank.bloodbankpakistan&pcampaignid=web_share (accessed on 16 November 2023) |
| Pregnancy Week by Week | Pregnancy Week by Week provides counseling, health information, and a week-by-week pregnancy tracker to help pregnant women have a healthy pregnancy. It has over ten million users https://play.google.com/store/apps/details?id=com.hp.pregnancy.lite&pcampaignid=web_share (accessed on 16 November 2023) |
| Pharmapedia Pakistan | Pharmapedia is a medical app that provides information about medicines that are available in Pakistan, including uses, dosages, and adverse effects. It has over one million users. https://play.google.com/store/apps/details?id=com.binops.pharma.pk&pcampaignid=web_share (accessed on 16 November 2023) |
| Dawaai.pk | The Dawaai.pk app allows users to buy prescription medicines, healthcare products, and supplements along with additional information regarding medications and their substitutes. It has over one million users. https://play.google.com/store/apps/details?id=com.dawaai.app&pcampaignid=web_share (accessed on 16 November 2023) |
| Hypotheses | Estimate | S.E. | C.R. | p | Results | |||
|---|---|---|---|---|---|---|---|---|
| H1 | PE | → | BI | 0.504 | 0.099 | 5.064 | *** | Accepted |
| H2 | EE | → | BI | −0.198 | 0.104 | −1.900 | 0.057 | Rejected |
| H3 | SI | → | BI | −0.134 | 0.121 | −1.109 | 0.267 | Rejected |
| H4 | SC | → | BI | 0.860 | 0.144 | 5.968 | *** | Accepted |
| H5 | FCs | → | MA | 0.219 | 0.114 | 1.916 | 0.055 | Rejected |
| H6 | BI | → | MA | −0.008 | 0.153 | −0.054 | 0.957 | Rejected |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Azam, M.; Bin Naeem, S.; Kamel Boulos, M.N.; Faiola, A. Modelling the Predictors of Mobile Health (mHealth) Adoption among Healthcare Professionals in Low-Resource Environments. Int. J. Environ. Res. Public Health 2023, 20, 7112. https://doi.org/10.3390/ijerph20237112
Azam M, Bin Naeem S, Kamel Boulos MN, Faiola A. Modelling the Predictors of Mobile Health (mHealth) Adoption among Healthcare Professionals in Low-Resource Environments. International Journal of Environmental Research and Public Health. 2023; 20(23):7112. https://doi.org/10.3390/ijerph20237112
Chicago/Turabian StyleAzam, Mehreen, Salman Bin Naeem, Maged N. Kamel Boulos, and Anthony Faiola. 2023. "Modelling the Predictors of Mobile Health (mHealth) Adoption among Healthcare Professionals in Low-Resource Environments" International Journal of Environmental Research and Public Health 20, no. 23: 7112. https://doi.org/10.3390/ijerph20237112
APA StyleAzam, M., Bin Naeem, S., Kamel Boulos, M. N., & Faiola, A. (2023). Modelling the Predictors of Mobile Health (mHealth) Adoption among Healthcare Professionals in Low-Resource Environments. International Journal of Environmental Research and Public Health, 20(23), 7112. https://doi.org/10.3390/ijerph20237112







