Abstract
Research has shown a protective association between social support and depression, depression among stroke patients, and health impacts of depression. Despite this, not much is known about the effect of social support on depression among stroke patients. This review aims to summarize the current research examining the association between social support and depression among stroke patients. A literature search was performed in PubMed to find original peer-reviewed journal articles from 2016 to 12 March 2023 that examined the association between social support and depression among stroke patients. The search terms were depression and “social support” and stroke, which lead to 172 articles. After abstract review, seven observational studies that studied the target association among stroke patients were selected. One additional study was found using PsycINFO as a complementary source with the same search strategy and criteria. Overall, a negative association was found between social support and depression among stroke patients in eight studies, with more social support leading to lower rates of depression post-stroke. The other study did not find a statistically significant association. Overall, the results of recent studies suggest that social support is negatively associated with depression among stroke patients. In most studies, this association was statistically significant. The findings suggest the importance of improving social support perceived by stroke patients in the prevention of depression after the occurrence of stroke.
1. Introduction
Stroke is an abrupt neurological outburst following impaired blood perfusion to the brain or bleeding due to rupture of a blood vessel [1,2]. The impaired blood perfusion causes the central nervous system to suffer from an acute focal injury, which can then lead to a neurological deficit [3]; in the bleeding case, a hematoma is formed that causes compression to the brain tissue and increase of the intracranial pressure [2,3]. Stroke is the second leading cause of death worldwide as of 2019 [4]. The global mortality rate of stroke is about 5.5 million, and about half of stroke survivors suffer from some level of long-term disability [4]. In the United States (USA), stroke remains the 5th cause of death [5]. A stroke occurs every 40 s, and death from stroke every 4 min in the USA [6]. Based on the mechanisms, stroke typically consists of three types—ischemic stroke, hemorrhagic stroke, and transient ischemic attack (TIA) [1]. Post-stroke complications are multiple—post-stroke seizures, partial paralysis, bladder dysfunction, bowl dysfunction, and sleep disturbance may start immediately after stroke onset and can last for years [1,7]. Apart from the physical complications, psychosocial complications occur as well. Depression is one of the major mental problems following stroke [1,7,8,9]. Depression is a mental disorder that leads to constant sad feelings and loss of interest [10]. In addition to sad feelings and loss of interest, people with depression may typically experience somatic symptoms, including changes in appetite, sleeping disorder, chronic pain in joints, the back and limbs, fatigue, and gastrointestinal problems [11,12]. Changes in appetite and gastrointestinal problems may then result in other health problems such as diabetes [13]. Besides, depressive symptoms are associated with increased social isolation [14]. Even worse, depressed patients may think about and attempt suicidal behavior [15]. The prevalence of post-stroke depression (PSD) occurs in 18–31% of stroke patients, according to results of several meta-analysis studies [16,17,18]. Worldwide, depression affects approximately 3.8% of the total population, and around 5.0% among adults (18 years or older) [19]. Additionally, PSD is highly associated with post-stroke physical complications [1,7]. For example, bladder dysfunction leads to urine incontinence, which is highly associated with an increased risk of depression [20,21]. Even more concerning, depression has been found associated with decreased adherence to medication treatment for stroke, leading to increased risks of stroke recurrence and mortality [22,23,24].
As introduced above, depression does not just impact mental health, but also introduces somatic symptoms and problems in daily life [11,12,13,14,15,25,26]. However, what makes depression worse is that 69% of patients who met the criteria of depression reported only somatic symptoms when they paid a visit to health professionals, according to a study by Simon et al. [27]. Patients reporting only somatic symptoms instead of psychological symptoms such as depressed mood can lead to undiagnosed depression [27,28]. This, among other factors, including concerns of being recommended antidepressants and being referred to a psychiatrist, often hinders early diagnosis and treatment of depression [27,28,29,30,31]. The underreporting is a particularly serious problem among stroke survivors, whose depression is often co-morbid with physical ailments and associated with the recurrence and mortality [22,23,24]. The underdiagnosis also indicates that depression is in fact more prevalent among the populations than indicated by the observed numbers, including among stroke patients [32]. It is essential to examine the modifiable factors associated with depression for the purpose of prevention and treatment.
The presence of high social support is thought to be particularly helpful in PSD. Social support is a psychological construct that refers to the provision of assistance or comfort that are provided and are accessible to individuals, typically thought to help individuals deal with biological and psycho-social stressors [33]. Social support has multiple operationalized meanings, which can include structural components such as social integration, which means being a part of and participating in social networks [34,35]. Social support can also refer to functional components, such as types of interactions between individuals [36]. In most studies, social support is conceptualized as perceived social support, which is typically measured by psychological scales that cover the components above [37,38,39,40].
By affecting coping strategies, meeting daily social needs, and encouraging community participation, social support has been found to be an important factor for both the acute recovery and daily life of stroke patients [41,42,43,44,45]. Despite this, little is known about the association between social support and depression/depressiveness among stroke patients, either at the acute phase or in a longer period. Multiple studies have evaluated the association between social support and mental health among various populations, such as the elderly or the general population [46,47,48,49,50,51]. Findings of most existing studies indicated that those with better social support were expected to have a lower risk of depression and less severe depression/depressive symptoms [46,47,48,49,50,51,52]. Nevertheless, most of these studies do not particularly target stroke patients, who have the health conditions that are related to depression [46,47,48,49,50,51,52]. Given the distinct challenges that arise from stroke—long rehabilitation process, difficulties to perform daily activities, loneliness, cost of medical needs and so forth–social support and depression might be associated differently among stroke patients than other populations or might be associated [15,53]. Moreover, most review articles and meta-analyses on relevant topics either broadly describe psycho-social factors or are more focused on intervention programs in clinical settings, which were fundamentally different from social support that is perceived in daily life [54,55,56,57]. Summary and evaluation of studies are crucial to understand what is known regarding social support and depression among stroke patients.
This literature review aims to evaluate the current research studying the association between social support and depression, specifically among stroke patients.
2. Materials and Methods
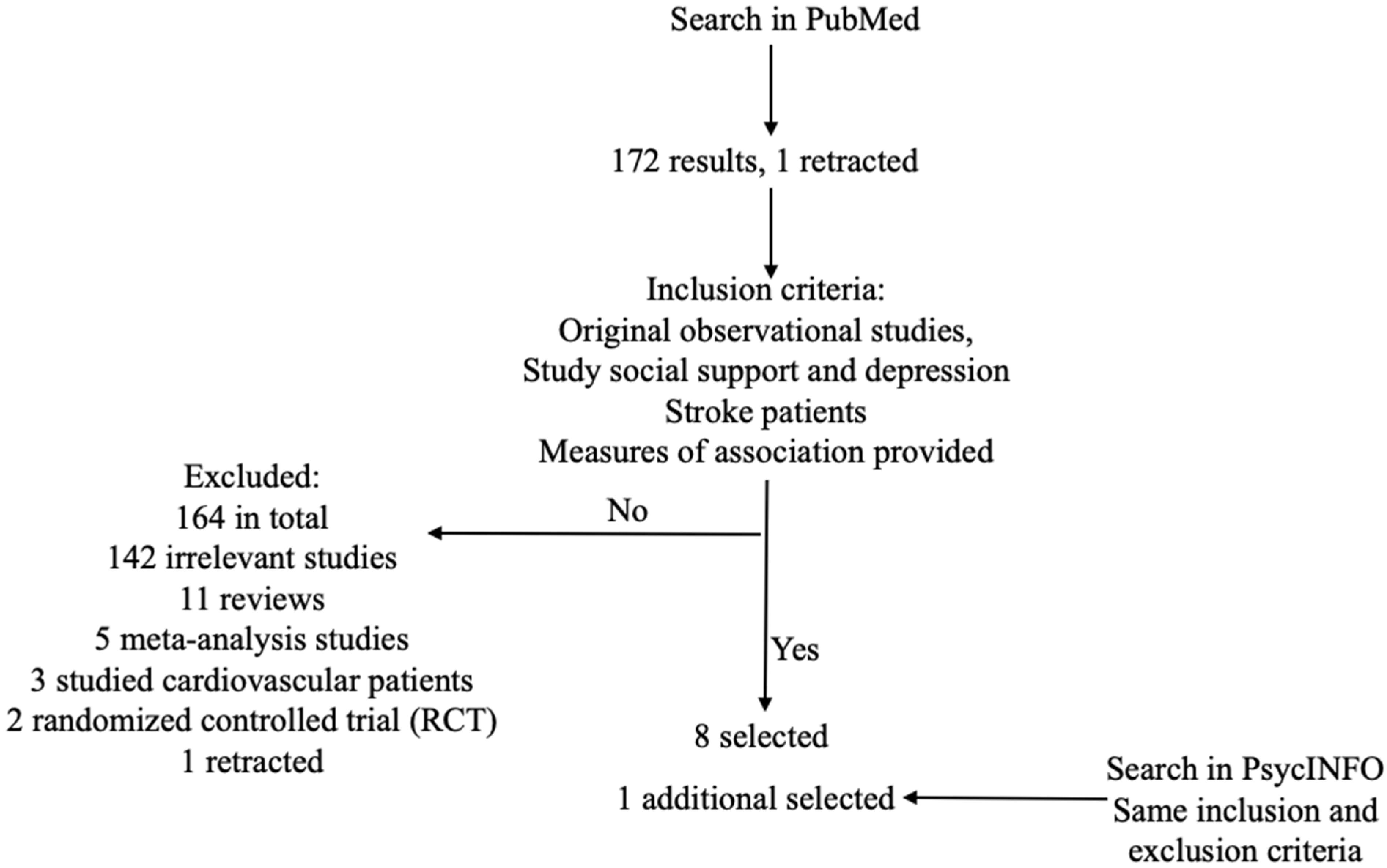
This literature review includes peer-reviewed journal articles that examined the association between social support and depression among stroke patients. PubMed was used to search for the terms “depression and ‘social support’ and stroke”. “Social support” was quoted in the search box to exclude irrelevant results. The most recent search date was 12 March 2023, and this review includes papers published up to that date. The year range was restricted to between 2016 and 2023 (including 2016 and 2023) so that only recent studies were included. According to the History and Search Details of Pubmed, the search terms were automatically mapped to MeSH terms, which were translated as following: depression: “depressed”[All Fields] OR “depression”[MeSH Terms] OR “depression”[All Fields] OR “depressions”[All Fields] OR “depression’s”[All Fields] OR “depressive disorder”[MeSH Terms] OR (“depressive”[All Fields] AND “disorder”[All Fields]) OR “depressive disorder”[All Fields] OR “depressivity”[All Fields] OR “depressive”[All Fields] OR “depressively”[All Fields] OR “depressiveness”[All Fields] OR “depressives”[All Fields]; stroke: “stroke”[MeSH Terms] OR “stroke”[All Fields] OR “strokes”[All Fields] OR “stroke’s”[All Fields]. More specific terms such as “hemorrhagic stroke”, “ischemic stroke”, or “ischemia attack” were unnecessary because the Mesh Term “stroke” already covered all the specific situations below “stroke” in the MeSH term tree structure. Thus, although only the above search terms were used, the search results included all the studies that might meet the inclusion criteria for this literature review in the PubMed database. This search resulted in 172 articles, of which one article was retracted. Figure 1 shows the steps of searching and selection of articles.
Figure 1.
Search and selection of articles.
Abstracts of the remaining 172 articles were read for selection based on inclusion and exclusion rules. For a study to be included, it must be an original observational study, for the exposure of interest was social support that can only be perceived from daily life. Cohort studies, cross-sectional studies, and case-control studies were acceptable. The exposure and the outcome of interest must be specifically defined with explicit operationalization. Social support/perceived social support must be the primary exposure or one of the primary exposures, and depression/depressive symptoms/depressiveness must be the primary outcome or one of the primary outcomes. The target population had to be stroke patients. There was no restriction on specific types of stroke—ischemic stroke, hemorrhagic stroke, and transient ischemic attack (TIA) [58]. Measures of association must be provided for a study to be included, regardless of the statistical significance level.
Among the 172 articles found by search terms, 11 studies were literature reviews or systematic reviews; four studies were meta-analyses; 142 studies were identified as irrelevant ones that did not study the target association—social support and depression, or targeted other populations than stroke patients. Besides the fact that the article types did not meet our inclusion criteria, the literature reviews and meta-analyses did not study the association of interest among stroke patients although these 15 articles showed up in the search results. One experimental study designed and implemented social support interventions and compared depression levels between the intervention group and the control group [59]. Excluding experimental studies had a conceptual reason: the exposure differed from the one that the topic review focuses on—the social support status perceived by subjects in their daily life instead of a social support intervention. After all criteria were applied, eight studies were left for this topical review, including five prospective cohort studies, and three cross-sectional studies [60,61,62,63,64,65,66,67].
APA PsycINFO was used as a complementary database. The same search strategies and inclusion and exclusion criteria were used to find if there were additional appropriate papers. The same search terms resulted in 83 papers (the last search date: 12 March 2023), including two prospective cohort studies that met all the criteria [62,66]. One of the cohort studies overlapped with the selected papers from PubMed [66]. The other study was selected [62]. Thus, nine studies were selected for the final review [60,61,62,63,64,65,66,67,68].
3. Results
3.1. Samples and Populations
The main characteristics of the selected studies are listed in Table 1. The studies included five prospective cohort studies and three cross-sectional studies. Additionally, the study by Ladwig et al. analyzed data from two cohort studies [68]. All the studies except Ladwig et al. enrolled adults (age ≥ 18 years) that had been diagnosed with stroke [60,61,62,63,64,65,66,67,68]. The average age of eight studies ranged from 56.4 to 70.8 years [61,62,63,64,65,66,67,68]. The gender distribution was roughly balanced in six studies, where neither gender exceeded 60% [61,63,65,66,67,68]. The most unbalanced gender distribution (29.1% females) appeared in the study by Wei et al. [62]. One article did not reveal mean age or gender distribution [60]. The sample size of respondents ranged from 33 in a prospective cohort study to 710 in a cross-sectional study [60,61,62,63,64,65,66,67]. The mean sample size was 230.0, the median 160.5, and the standard deviation 224.0. Eight studies focused on inpatients from hospitals, rehabilitation centers, and/or clinics [61,62,63,64,65,66,67,68]. One study recruited stroke patients, of which the source was not specified in the article [60].

Table 1.
Characteristics of Selected Studies.
The population of interest in this review was stroke patients, regardless of stroke types and lengths of time between the occurrence of stroke and data collection or enrollment. The cross-sectional study by Olibamoyo et al. specified that stroke must have occurred in the six months prior to enrollment [56]. Six studies had restrictions on specific types or the status of stroke that participants had [60,61,62,66,67,68]. The cohort study by Volz et al. restricted the participants to only patients with a first ischemic stroke diagnosed over four weeks prior to enrollment [66]. Schöttke et al. only enrolled patients with either acute cerebral infarction or intracerebral hemorrhage over 24 h prior [67]. The cross-sectional study by Ahmed et al. included only patients with a history of acute ischemic stroke confirmed with neuroimage evidence [61]. Villain et al. limited their sample to adult patients with first ischemic stroke diagnosed by a neurologist with clinical evidence and magnetic resonance image (MRI) [60]. The two samples in the study by Ladwig et al. only included ischemic stroke patients; clinical evidence was unspecified in the paper [59]. Wei et al. excluded those with hemorrhagic stroke [62]. The other two studies did not add restrictions on a time duration from the stroke occurrence or stroke types [63,64].
3.2. Social Support and Depression Measurements
The study by Olibamoyo et al. measured social support using only one question in a demographic questionnaire [65]. The eight other studies measured social support with validated psychological scales [60,61,62,63,64,67,68]. The scales used to assess social support included the Multidimensional Scale of Perceived Social Support (MSPSS), the Perceived Social Support Questionnaire (F-SozU, both the 22-item version F-SozU K-22 and the 14-item version F-SozU K-14), Social Support Rating Scale (SSRS), and the MOS Social Support Survey (MOS-SSS) [69,70,71,72,73,74]. For depression, the outcome of interest, one study confirmed subjects’ depression using diagnostic evaluations at three time points [75]. One study diagnosed depression based on Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) [76]. Seven studies assessed depression using other scales, which included the Mini-International Neuropsychiatric Interview (MINI), the Hospital Anxiety and Depression Scale (HADS), Cornell Scale for Depression (CDS), the Hamilton Depression Rating Scale (HDRS-17), the Center for Epidemiologic Studies Depression Scale (CES-D), the Patient Health Questionnaire-9 (PHQ-9), and Geriatric Depression Scale (GDS) [77,78,79,80,81,82,83].
3.3. Main Findings
Despite the differences in sample sizes, study design, and analytical methods that existed across the studies, there was one consistent facet in the findings: eight studies found negative associations between social support and depression among stroke patients [60,61,62,63,64,65,67,68]. The association estimates in eight of the nine studies indicated that stroke patients with poorer social support were more likely to suffer from depression or were expected to have worse depression status [60,61,62,63,64,65,67,68]. Due to the different parameterizations of social support and depression, the estimates could not be compared directly between studies on ischemic-stroke patients and those on patients with any type of stroke. Nevertheless, both types of studies reported odds ratios (ORs) greater than 1.3 (absolute value) [61,67].
As the only selected study that measured social support with one single item, the study by Olibamoyo et al. categorized social support into “poor”, “fair”, and “good” [56]. They found the adjusted OR that was the furthest from the null: OR (fair vs. good) = 7.6, 95% CI: (0.96, 59.614), OR (poor vs. good) = 92.4, 95% CI: (3.71, 2296.83) among patients with any type of stroke [65]. The article did not address the possible reasons for the extreme estimates. To measure social support as a construct, using only one item is likely to yield low reliability. The OR of categorized social support is not comparable with the ORs in other studies, where social support was represented by a scale score in regression models. Besides this, the extremely wide confidence intervals were not informative.
In the studies that measured social support with psychological scales and applied logistic regression models, the adjusted OR furthest from the null was in the study by Ahmed et al.: 0.66, 95% CI: (0.47, 0.94) for a one-unit increase in the MSPSS scale, the OR closest to the null in the study by Volz et al.: 0.95 (p = 0.03) for a one-unit increase in the F-SozU scale [61,62,66,67]. Ahmed et al. recruited 68 ischemic-stroke patients and adjusted for the fewest covariates in the models: stroke severity at admission, poststroke disability after 3 months, and discontinuation of rehabilitation. No demographics were included in the models, while five other studies included several, although not identical, demographic covariates [60,61,63,64,65,67]. The study by Wei et al. had a larger sample size (368 adult patients with any type of stroke except hemorrhagic stroke) than the study by Ahmed et al., and did not adjust for demographic covariates [62]. The association between social support at baseline and depression three months afterwards (adjusted OR = 0.57, p = 0.001) was found close to that in the study by Ahmed et al. [61,62].
Four studies measured social support with psychological scales and fitted linear regression models [60,63,64,68]. Among the four studies, both the study by Wang et al. and the study by Babkair et al. were cross-sectional studies and recruited stroke patients through convenient sampling [63,64]. The sample sizes were 800 and 135 adult stroke patients, respectively [63,64]. The estimated coefficients in linear models were β = −0.111 (p < 0.01) and β = −0.31 (p < 0.001) [63,64], respectively, meaning that a single-unit increase in the scores measured by their selected social support scales was respectively associated with decreases of 0.111 and 0.31 in the depression scales. Both studies adjusted for demographics and variables measuring the subjects’ physical health at baseline [63,64]. The main difference in the two studies that might lead to the difference in effect estimates was the measurement instruments used; Wang et al. used the PSSS scale to measure social support, and assessed depression with CES-D while Babkair et al. used MOS-SSS for social support and PHQ-9 for depression [63,64,69,72,81,82]. Villain et al. broke down perceived social support at admission, the exposure, into multiple components: medical attention from medical staff, moral support from medical staff, moral support from family and friends, and material support from family and friends [60]. The ischemic stroke patients had these four components assessed through ecological momentary assessment (EMA) [60,84]. The estimated coefficients in the models adjusting for age, sex, anxiety, and depression levels at hospital admission were medical attention from medical staff: γ = −0.019 (SE = 0.055, t ratio = −0.357), moral support from medical staff: γ = −0.051 (SE = 0.043, t ratio = −1.191), moral support from family and friends: γ = −0.097 (SE = 0.046, t ratio = −2.141), and material support from family and friends: γ = 0.008 (SE = 0.055, t ratio = 0.161) adjusting for age, sex, and baseline depression levels [60]. All the four components of social support were found to be negatively related with depression three months after hospital discharge in the cohort study. The effect of moral support from family and friends was the strongest and statistically significant. The sample size of this study was 33 after dropping those lost to follow-up, the smallest among the eight studies. Both cohort studies in the article of Ladwig et al. recruited only ischemic stroke patients [68]. They treated social support scores (one by F-SozU K-22, and one by F-SozU K-14) as continuous variables [68]. Depression was also a continuous variable in both studies; one used the GDS score and one used the PHQ-9 score [68]. Consistent with Wang et al., Babkair et al., and Villain et al., Ladwig et al. found that social support was negatively associated with the risk of poststroke depression six months later (Study A: social support measured by F-SozU K22, depression measured by GDS-15, β = −1.91, 95% CI: (−2.71, −1.11), Study B: social support measured by F-SozU K14, depression measured by PHQ-9, β = −2.69, 95% CI: (−3.92, −1.47)) [68]. Besides the association of different social support levels between individuals and depression, Ladwig et al. also found a protective effect of within-person change in social support six months after the acute phase on depression (β = −0.14, 95% CI: (−0.22, −0.05)) [68].
Eight of the selected studies found statistically significant associations, but one did not. The prospective cohort study conducted by Schöttke et al. had a sample of 78 patients with any type of stroke after a 3-year follow-up [67]. The study looked into the association between perceived social support at baseline and depression three years after stroke onset [67]. The adjusted covariates in the study included sex, age, functional impairment, depression at the acute phase of stroke, and estimated the association with (adjusted OR = 1.825 (95% CI 0.593, 5.617)) and without the interaction (adjusted OR = 1.355 (95% CI 0.516, 3.560), p = 0.537) between functional impairment and perceived social support at the acute phase [67]. The point estimates of OR were greater than 1, which conflicted with the findings in all the other seven studies. This study did not adjust for stroke severity, which was an important covariate in multiple other studies [61,65,66]. Besides, Schöttke et al. measured depression both at enrollment and three years afterwards at follow up (the longest duration between the baseline when social support was measured and the measurement of depression) [67]. The final model predicting depression three years after enrollment included the depression level at baseline as a predictor, which was unique in all the selected studies except for the study by Villain et al. [60,61,62,63,64,65,66,67,68].
Six studies adjusted for demographics, among which five studies adjusted for age, and four adjusted for sex review [60,63,64,65,67,68]. Other demographic covariates were not shared by most studies. Besides demographics, variables related to physical health conditions, particularly stroke severity and physical disability, were important covariates as seven studies included at least one of the two variables in the final model [61,62,63,64,65,66,67,68].
4. Discussion
The primary purpose of this literature review was to examine recent literature on social support and depression among stroke patients. PSD is a common condition that leads to suffering of patients and is a key problem to address in stroke treatment. Eight studies consistently found that depression was negatively associated with social support and the association was statistically significant. In total, four studies recruited stroke patients without restriction on the stroke types; four were based on only ischemic-stroke patients and one excluded hemorrhagic stroke patients. Another difference across the eight studies was the restriction on time of measuring the variables. Of the eight studies with significant results, all cohort studies took measurements at baseline (hospital admission), but follow-up time varied from 90 days to 6.1 months; one cross-sectional study was restricted to patients with a stroke history at least 6 months prior [61,65,66]. There was no substantive distinction in the findings on different stroke patients in terms of what type of stroke and when PSD and social support were measured relative to stroke onset. Social support appeared consistently associated with lower depression severity or risk of having depression. This is also consistent with the association of social support and depression among other populations and under other scenarios, such as individuals at the time of social isolation and social distancing due to the COVID-19 pandemic [85], and among elderly people [86,87,88].
The only study that had a discrepancy with the others regarding the target association was that by Schöttke et al., which did not restrict stroke types [67]. The prospective cohort study by Schöttke et al. did not find a statistically significant association and the direction of the association conflicted with the other seven studies [67]. This discrepancy might be caused by a variety of factors: the covariates selected biasing the estimate, selection bias caused by a high proportion of loss to follow-up, and uncontrolled confounding especially given the long interval between the baseline and the follow-up three years after stroke. The other eight studies observed statistically significant associations within a shorter period after stroke onset [60,61,62,63,64,65,66,68]. Assuming that the findings of Schöttke et al. are unbiased, the discrepancy might indicate that social support plays a weaker role in the later phase of stroke [67]. Schöttke et al. recruited patients from three rehabilitation clinics; the target population for inference was not exactly the same as the other studies in this review [67]. The inclusion criteria also varied across studies. For example, the study by Schöttke et al. restricted the participants to stroke patients with acute cerebral infarction and those with intracerebral hemorrhage [67]. In addition, the study required that the documentation of neurological symptoms must have exceeded 24 h prior to the study enrollment [67]. The other studies used different inclusion and exclusion criteria, which yielded different source populations in terms of stroke conditions. Another potential reason for the discrepancy might be the varying measures for social support and depression, which lead to an undeniable fact that the selected studies, in essence, evaluated associations slightly different from each other even if regardless of the covariates and populations.
Based on the comparison of the studies, including demographics did not systematically improve or reduce effect estimates of social support [60,61,62,63,64,65,66,67,68]. Neither the study with the OR furthest from the null nor the study with the OR closest to the null included adjustment for demographics [61,66]. The main difference in estimated effect sizes appears to be more affected by sample size and measuring instruments for social support and depression. The study by Ahmed et al. found the largest effect size (as OR), which measured social support with MSPSS and assessed depression with HADS [52,60,69]. The study by Volz et al. reported the smallest effect size (as OR), where social support was measured with HDRS-17 and depression with DSM-IV [66,76,89]. The nine studies were not enough to present patterns such as which combination of the scales would yield stronger or weaker effect estimates of social support on depression.
Five of the selected studies were prospective cohort studies, three were cross-sectional studies, and one was a secondary analysis based on longitudinal data [60,61,62,63,64,65,66,67,68]. All the cohort studies investigated the association between social support at baseline and depression after a follow-up period. The secondary analysis examined the effect of change in social support on depression after follow-up. Thus, temporality was clear in the data analysis of the cohort studies as well as the secondary analysis, which is an essential prerequisite for causality. Given the consistent findings, it is plausible to conclude that social support has a protective effect against PSD, which is itself a serious mental problem and is associated with poor treatment adherence and increased probabilities of bad health outcomes including stroke recurrence and death.
4.1. Limitations
Several limitations must be carefully considered regarding the selected studies. First, only one study explicitly explained that it used a probability sampling method, which was good for the representativeness of the sample. The other studies either used convenient sampling or did not introduce the sampling method. This weakness rendered a potential concern to the external validity of the study findings. Second, some of the studies had moderate sample sizes, the smallest of which was 44 enrolled and 33 followed up [60]. It is plausible to worry about random errors that might have biased the results. Third, none of the selected studies conducted sensitivity analysis [60,61,62,63,64,65,66,67,68]. Unlike randomized controlled trials, an essential concern in observational studies is always uncontrolled confounding that may explain away the association [90]. Thus, it is crucial to conduct sensitivity analysis in observational studies, which is lacking in all the selected studies. The robustness of the study findings to uncontrolled confounding remains unknown. This limitation also makes it impossible to identify which study built the most efficient model that estimated the association with the least necessary covariates while adjusting for confounders adequately. An essential piece of evidence, though not a necessary condition, is missing for drawing causal conclusions due to this fact. Fourth, the three cross-sectional studies could not provide temporality of social support and depression. Thus, the association estimates provided by these three studies, either adjusted or unadjusted, could not infer causality.
Other limitations included but were not limited to: (1) One study had a 45% dropout rate, potentially impairing the representativeness and introducing bias, the direction of which could be either away from the null or towards the null [67]; (2) patients with severe functional impairment or extremely poor cognitive status were excluded from some studies, which also limited the generalizability and transportability and could bias the results if the targeted population was not adjusted to those that did not include the severe patients in interpretation. Existing studies have found worse stroke severity to predict more severe depression [17,91]. Despite this, no evidence was found on the association between stroke severity at baseline (at onset or at hospital admission) and social support. The direction of bias caused by exclusion remains unknown; (3) Hospital setting also might have lowered the generalizability of study findings, for more of the stroke patients were still at the acute phase at the time of study or more severe than patients at home [92].
4.2. Strengths
The selected studies had noticeable strengths despite the limitations listed above: (1) Temporality of social support and depression, a necessary but insufficient condition for causality, was clear in the five prospective cohort studies; (2) The relatively large sample sizes of several studies rendered their effect estimates less prone to random error than those with small sample sizes. The largest sample size was 710 in the study by Wang et al. where the linear coefficient of social support score was −0.111 (p < 0.01), adding to the power of the study and the strength of our conclusion on social support and depression [63]; (3) Although covariates adjusted for varied across the studies, eight of the studies reported statistically significant associations and six of them were strong associations. This was evidence in favor of causality despite the absence of sensitivity analysis. (4) Different measuring instruments for social support and depression yielded the same direction of the targeted association, the only difference of which was the magnitude of the effect estimates. This fact further supports the robustness of the observed protective effect of social support against depression among stroke patients.
4.3. Future Research Directions
Several advancements should be made in future studies. First, add sensitivity analysis to observational studies on the association between social support and depression among stroke patients. This is due to the nature of observational studies, of which the purpose is to measure the robustness of effect estimates to uncontrolled confounding and provide evidence of causality [90,93,94]. The research question of this literature review by itself eliminates the possibility of experimental study designs because the exposure of interest is social support perceived by subjects in their life. In an experimental study, the exposure would become a support intervention, which is different from the exposure of interest. One experimental study was excluded in article selection because of this reason. Second, more combinations of covariates both as potential confounders and potential effect modifiers should be tested out in regression analysis. Variables measuring or reflecting the physical health conditions of stroke patients could make good covariates, such as NIHSS score and Barthel Index that measure stroke severity and activities of daily life. These two variables were included as covariates (confounders) in multiple selected studies, but not all of them. It has not yet been tested as to whether these two variables are effect modifiers. Using these variables as a base, researchers can try adding other covariates to regression models. Third, it might be more informative if future studies explicitly explain the sampling method (i.e., whether probability sampling or nonprobability sampling such as convenient sampling). Fourth, in order to increase sample sizes and avoid a high dropout rate, certain solutions need to be taken such as increasing the number of hospitals to recruit patients from, adding incentives for enrollment and responses during the follow-up period, and shortening the observation period if feasible and not conflicting with research questions. Lastly, researchers are encouraged to implement qualitative studies, cross-sectional studies, or even short-term cohort studies if feasible given the resources, to explore psycho-social factors that affect the association between social support and depression, such as prior diagnosis of depression or other mental conditions before the stroke onset.
5. Conclusions
Overall, social support appears to be negatively associated with depression among stroke patients. Stroke patients with better social support conditions are expected to have a lower risk of depression or less severe depression. The association is statistically significant and supported by most recent studies. Multiple methodological improvements can still be made to accumulate valid evidence of causality on this association.
From the perspective of clinical practice, this review examined the quantitative importance of social support, particularly the support perceived by stroke patients, in lowering the risk and severity of post-stroke depression, which then may improve treatment adherence and reduce poor health outcomes including stroke recurrences and deaths. Care providers are encouraged to evaluate the depression/depressive level and social support of stroke patients as a routine and help address factors that hinder the reception and perception of social support.
Author Contributions
H.Z. developed the research objectives and methods, implemented the searching procedure, and summarized the articles. E.R.K. was responsible for guidance throughout the development of the topical review and provided feedback on all the sections. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank Rick Lezenby for his assistance with the search strategy for this topical review.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kuriakose, D.; Xiao, Z. Pathophysiology and Treatment of Stroke: Present Status and Future Perspectives. Int. J. Mol. Sci. 2020, 21, 7609. [Google Scholar] [CrossRef] [PubMed]
- Unnithan, A.K.A.; Das, J.M.; Mehta, P. Hemorrhagic Stroke; StatPearls: St. Petersburg, FL, USA, 2023. [Google Scholar]
- Sacco, R.L.; Kasner, S.E.; Broderick, J.P.; Caplan, L.R.; Connors, J.J.; Culebras, A.; Elkind, M.S.V.; George, M.G.; Hamdan, A.D.; Higashida, R.T.; et al. An Updated Definition of Stroke for the 21st Century: A Statement for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2013, 44, 2064–2089. [Google Scholar] [CrossRef] [PubMed]
- Donkor, E.S. Stroke in the 21(St) Century: A Snapshot of the Burden, Epidemiology, and Quality of Life. Stroke Res. Treat. 2018, 2018, 3238165. [Google Scholar] [CrossRef] [PubMed]
- American Stroke Association About Stroke. Available online: https://www.stroke.org/en/about-stroke (accessed on 24 May 2023).
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P. Heart Disease and Stroke Statistic—2020 Update: A Report from the American Heart Association. Am. Hear. Assoc. 2020, 141, e139–e596. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Selim, M.H.; Caplan, L.R. Medical Complications after Stroke. Lancet Neurol. 2010, 9, 105–118. [Google Scholar] [CrossRef]
- Medeiros, G.C.; Roy, D.; Kontos, N.; Beach, S.R. Post-Stroke Depression: A 2020 Updated Review. Gen. Hosp. Psychiatry 2020, 66, 70–80. [Google Scholar] [CrossRef]
- Guo, J.; Wang, J.; Sun, W.; Liu, X. The Advances of Post-Stroke Depression: 2021 Update. J. Neurol. 2022, 269, 1236–1249. [Google Scholar] [CrossRef]
- Chand, S.P.; Arif, H. Depression; StatPearls: St. Petersburg, FL, USA, 2023. [Google Scholar]
- Trivedi, M.H. The Link between Depression and Physical Symptoms. Prim. Care Companion J. Clin. Psychiatry 2004, 6, 12–16. [Google Scholar]
- Raič, M. Depression and Heart Diseases: Leading Health Problems. Psychiatr. Danub. 2017, 29 (Suppl. S4), 770–777. [Google Scholar] [PubMed]
- Graham, E.; Watson, T.; Deschênes, S.S.; Filion, K.B.; Henderson, M.; Harper, S.; Rosella, L.C.; Schmitz, N. Depression-Related Weight Change and Incident Diabetes in a Community Sample. Sci. Rep. 2021, 11, 13575. [Google Scholar] [CrossRef]
- Elmer, T.; Stadtfeld, C. Depressive Symptoms Are Associated with Social Isolation in Face-to-Face Interaction Networks. Sci. Rep. 2020, 10, 1444. [Google Scholar] [CrossRef]
- Garrett-Jones, E.C.; Anakor, E.A.; Mamin, F.A.; Fatema, U.K.; Das, S.K. The Long-Term Challenges Faced by Stroke Survivors and Their Caregivers Following a Stroke in Bangladesh: A Qualitative Study. J. Glob. Health Rep. 2019, 3, e2019053. [Google Scholar] [CrossRef]
- Hackett, M.L.; Pickles, K. Part I: Frequency of Depression after Stroke: An Updated Systematic Review and Meta-Analysis of Observational Studies. Int. J. Stroke Off. J. Int. Stroke Soc. 2014, 9, 1017–1025. [Google Scholar] [CrossRef] [PubMed]
- Ayerbe, L.; Ayis, S.; Wolfe, C.D.A.; Rudd, A.G. Natural History, Predictors and Outcomes of Depression after Stroke: Systematic Review and Meta-Analysis. Br. J. Psychiatry 2013, 202, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, A.J.; Sheth, B.; Gill, J.; Yadegarfar, M.; Stubbs, B.; Yadegarfar, M.; Meader, N. Prevalence and Predictors of Post-Stroke Mood Disorders: A Meta-Analysis and Meta-Regression of Depression, Anxiety and Adjustment Disorder. Gen. Hosp. Psychiatry 2017, 47, 48–60. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Depression. Available online: https://www.who.int/news-room/fact-sheets/detail/depression (accessed on 27 March 2022).
- Thomas, L.H.; Coupe, J.; Cross, L.D.; Tan, A.L.; Watkins, C.L. Interventions for Treating Urinary Incontinence after Stroke in Adults. Cochrane Database Syst. Rev. 2019, 2, CD004462. [Google Scholar] [CrossRef]
- Limampai, P.; Wongsrithep, W.; Kuptniratsaikul, V. Depression after Stroke at 12-Month Follow-up: A Multicenter Study. Int. J. Neurosci. 2017, 127, 887–892. [Google Scholar] [CrossRef]
- Srithumsuk, W.; Chaleoykitti, S.; Jaipong, S.; Pattayakorn, P.; Podimuang, K. Association between Depression and Medication Adherence in Stroke Survivor Older Adults. Jpn. J. Nurs. Sci. 2021, 18, e12434. [Google Scholar] [CrossRef]
- Cai, W.; Mueller, C.; Li, Y.-J.; Shen, W.-D.; Stewart, R. Post Stroke Depression and Risk of Stroke Recurrence and Mortality: A Systematic Review and Meta-Analysis. Ageing Res. Rev. 2019, 50, 102–109. [Google Scholar] [CrossRef]
- Sibolt, G.; Curtze, S.; Melkas, S.; Pohjasvaara, T.; Kaste, M.; Karhunen, P.J.; Oksala, N.K.J.; Vataja, R.; Erkinjuntti, T. Post-Stroke Depression and Depression-Executive Dysfunction Syndrome Are Associated with Recurrence of Ischaemic Stroke. Cerebrovasc. Dis. 2013, 36, 336–343. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- Belmaker, R.H.; Agam, G. Major Depressive Disorder. N. Engl. J. Med. 2008, 358, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Simon, G.E.; VonKorff, M.; Piccinelli, M.; Fullerton, C.; Ormel, J. An International Study of the Relation between Somatic Symptoms and Depression. N. Engl. J. Med. 1999, 341, 1329–1335. [Google Scholar] [CrossRef] [PubMed]
- Dafsari, F.S.; Jessen, F. Late life depression—Diagnosis, pathophysiology and therapeutic strategies. Fortschr. Neurol. Psychiatr. 2018, 86, 242–255. [Google Scholar] [CrossRef] [PubMed]
- Bell, R.A.; Franks, P.; Duberstein, P.R.; Epstein, R.M.; Feldman, M.D.; Garcia, E.F.; Kravitz, R.L. Suffering in Silence: Reasons for Not Disclosing Depression in Primary Care. Ann. Fam. Med. 2011, 9, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Halfin, A. Depression: The Benefits of Early and Appropriate Treatment. Am. J. Manag. Care 2007, 13, S92–S97. [Google Scholar] [PubMed]
- Cacheda, F.; Fernandez, D.; Novoa, F.J.; Carneiro, V. Early Detection of Depression: Social Network Analysis and Random Forest Techniques. J. Med. Internet Res. 2019, 21, e12554. [Google Scholar] [CrossRef] [PubMed]
- Khedr, E.M.; Abdelrahman, A.A.; Desoky, T.; Zaki, A.F.; Gamea, A. Post-Stroke Depression: Frequency, Risk Factors, and Impact on Quality of Life among 103 Stroke Patients—Hospital-Based Study. Egypt. J. Neurol. Psychiatry Neurosurg. 2020, 56, 66. [Google Scholar] [CrossRef]
- American Psychological Association Social Support—APA Dictionary of Psychology. Available online: https://dictionary.apa.org/social-support (accessed on 5 November 2021).
- Reblin, M.; Uchino, B.N. Social and Emotional Support and Its Implication for Health. Curr. Opin. Psychiatry 2008, 21, 201–205. [Google Scholar] [CrossRef]
- Rodríguez-Artalejo, F.; Guallar-Castillón, P.; Herrera, M.C.; Otero, C.M.; Chiva, M.O.; Ochoa, C.C.; Banegas, J.R.; Pascual, C.R. Social Network as a Predictor of Hospital Readmission and Mortality among Older Patients with Heart Failure. J. Card. Fail. 2006, 12, 621–627. [Google Scholar] [CrossRef]
- Piferi, R.L.; Lawler, K.A. Social Support and Ambulatory Blood Pressure: An Examination of Both Receiving and Giving. Int. J. Psychophysiol. Off. J. Int. Organ. Psychophysiol. 2006, 62, 328–336. [Google Scholar] [CrossRef]
- Lyyra, T.-M.; Heikkinen, R.-L. Perceived Social Support and Mortality in Older People. J. Gerontol. B Psychol. Sci. Soc. Sci. 2006, 61, S147–S152. [Google Scholar] [CrossRef] [PubMed]
- Usta, Y.Y. Importance of Social Support in Cancer Patients. Asian Pac. J. Cancer Prev. 2012, 13, 3569–3572. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Mann, F.; Lloyd-Evans, B.; Ma, R.; Johnson, S. Associations between Loneliness and Perceived Social Support and Outcomes of Mental Health Problems: A Systematic Review. BMC Psychiatry 2018, 18, 156. [Google Scholar] [CrossRef] [PubMed]
- Falak, S.; Safdar, F. Nuzhat-Ul-Ain Perceived Discrimination, Social Support, and Psychological Distress in Transgender Individuals. PsyCh J. 2020, 9, 682–690. [Google Scholar] [CrossRef]
- Erler, K.S.; Sullivan, V.; Mckinnon, S.; Inzana, R. Social Support as a Predictor of Community Participation after Stroke. Front. Neurol. 2019, 10, 1013. [Google Scholar] [CrossRef] [PubMed]
- Hartford, W.; Lear, S.; Nimmon, L. Stroke Survivors’ Experiences of Team Support along Their Recovery Continuum. BMC Health Serv. Res. 2019, 19, 723. [Google Scholar] [CrossRef] [PubMed]
- Lehnerer, S.; Hotter, B.; Padberg, I.; Knispel, P.; Remstedt, D.; Liebenau, A.; Grittner, U.; Wellwood, I.; Meisel, A. Social Work Support and Unmet Social Needs in Life after Stroke: A Cross-Sectional Exploratory Study. BMC Neurol. 2019, 19, 220. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.-Y.; Wan, L.-H. Posttraumatic Growth of Stroke Survivors and Its Correlation with Rumination and Social Support. J. Neurosci. Nurs. J. Am. Assoc. Neurosci. Nurs. 2018, 50, 252–257. [Google Scholar] [CrossRef]
- Robinson-Smith, G.; Mahoney, C. Coping and Marital Equilibrium after Stroke. J. Neurosci. Nurs. J. Am. Assoc. Neurosci. Nurs. 1995, 27, 83–89. [Google Scholar] [CrossRef]
- Recto, P.; Champion, J.D. Social Support and Perinatal Depression: The Perspectives of Mexican-American Adolescent Mothers. Issues Ment. Health Nurs. 2020, 41, 932–939. [Google Scholar] [CrossRef]
- Domènech-Abella, J.; Lara, E.; Rubio-Valera, M.; Olaya, B.; Moneta, M.V.; Rico-Uribe, L.A.; Ayuso-Mateos, J.L.; Mundó, J.; Haro, J.M. Loneliness and Depression in the Elderly: The Role of Social Network. Soc. Psychiatry Psychiatry Epidemiol. 2017, 52, 381–390. [Google Scholar] [CrossRef]
- Gariépy, G.; Honkaniemi, H.; Quesnel-Vallée, A. Social Support and Protection from Depression: Systematic Review of Current Findings in Western Countries. Br. J. Psychiatry 2016, 209, 284–293. [Google Scholar] [CrossRef]
- Nakić Radoš, S.; Tadinac, M.; Herman, R. Anxiety During Pregnancy and Postpartum: Course, Predictors and Comorbidity with Postpartum Depression. Acta Clin. Croat. 2018, 57, 39–51. [Google Scholar] [CrossRef]
- Shih, T.-Y.; Cheng, S.-L.; Chang, S.-H.; Sun, H.-F. Perceived Social Support and Depression Symptoms in Patients with Major Depressive Disorder in Taiwan: An Association Study. Arch. Psychiatr. Nurs. 2020, 34, 384–390. [Google Scholar] [CrossRef] [PubMed]
- Hefner, J.; Eisenberg, D. Social Support and Mental Health among College Students. Am. J. Orthopsychiatry 2009, 79, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Ioannou, M.; Kassianos, A.P.; Symeou, M. Coping with Depressive Symptoms in Young Adults: Perceived Social Support Protects against Depressive Symptoms Only under Moderate Levels of Stress. Front. Psychol. 2019, 9, 2780. [Google Scholar] [CrossRef] [PubMed]
- Chohan, S.A.; Venkatesh, P.K.; How, C.H. Long-Term Complications of Stroke and Secondary Prevention: An Overview for Primary Care Physicians. Singap. Med. J. 2019, 60, 616–620. [Google Scholar] [CrossRef] [PubMed]
- Cheong, M.J.; Kang, Y.; Kang, H.W. Psychosocial Factors Related to Stroke Patients’ Rehabilitation Motivation: A Scoping Review and Meta-Analysis Focused on South Korea. Healthcare 2021, 9, 1211. [Google Scholar] [CrossRef] [PubMed]
- Aarnes, R.; Stubberud, J.; Lerdal, A. A Literature Review of Factors Associated with Fatigue after Stroke and a Proposal for a Framework for Clinical Utility. Neuropsychol. Rehabil. 2020, 30, 1449–1476. [Google Scholar] [CrossRef] [PubMed]
- Bartholomé, L.; Winter, Y. Quality of Life and Resilience of Patients With Juvenile Stroke: A Systematic Review. J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2020, 29, 105129. [Google Scholar] [CrossRef]
- Sun, X.; Deng, L.; Qiu, S.; Tu, X.; Wang, D.; Liu, M. Pharmacological and Psychotherapeutic Interventions for Management of Poststroke Depression: A Bayesian Network Meta-Analysis of Randomized Controlled Trials. Medicine 2017, 96, e6100. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention Types of Stroke | Cdc.Gov. Available online: https://www.cdc.gov/stroke/types_of_stroke.htm (accessed on 4 November 2021).
- Lin, F.-H.; Yih, D.N.; Shih, F.-M.; Chu, C.-M. Effect of Social Support and Health Education on Depression Scale Scores of Chronic Stroke Patients. Medicine 2019, 98, e17667. [Google Scholar] [CrossRef] [PubMed]
- Villain, M.; Sibon, I.; Renou, P.; Poli, M.; Swendsen, J. Very Early Social Support Following Mild Stroke Is Associated with Emotional and Behavioral Outcomes Three Months Later. Clin. Rehabil. 2017, 31, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, Z.M.; Khalil, M.F.; Kohail, A.M.; Eldesouky, I.F.; Elkady, A.; Shuaib, A. The Prevalence and Predictors of Post-Stroke Depression and Anxiety During COVID-19 Pandemic. J. Stroke Cerebrovasular Dis. 2020, 29, 105315. [Google Scholar] [CrossRef] [PubMed]
- Wei, C.; Gao, J.; Chen, L.; Zhang, F.; Ma, X.; Zhang, N.; Zhang, W.; Xue, R.; Luo, L.; Hao, J. Factors Associated with Post-Stroke Depression and Emotional Incontinence: Lesion Location and Coping Styles. Int. J. Neurosci. 2016, 126, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Shang, S.; Yang, H.; Ai, H.; Wang, Y.; Chang, S.; Sha, X.; Wang, L.; Jiang, X. Associations of Psychological Distress with Positive Psychological Variables and Activities of Daily Living among Stroke Patients: A Cross-Sectional Study. BMC Psychiatry 2019, 19, 381. [Google Scholar] [CrossRef]
- Babkair, L.A.; Chyun, D.; Vaughan, V.; Mohammed, D. The Effect of Psychosocial Factors and Functional Independence on Poststroke Depressive Symptoms: A Cross-Sectional Study. J. Nurs. Res. 2021, 30, e189. [Google Scholar] [CrossRef]
- Olibamoyo, O.; Adewuya, A.; Ola, B.; Coker, O.; Atilola, O. Prevalence and Correlates of Depression among Nigerian Stroke Survivors. South. Afr. J. Psychiatry 2019, 25, 1252. [Google Scholar] [CrossRef]
- Volz, M.; Möbus, J.; Letsch, C.; Werheid, K. The Influence of Early Depressive Symptoms, Social Support and Decreasing Self-Efficacy on Depression 6 Months Post-Stroke. J. Affect. Disord. 2016, 206, 252–255. [Google Scholar] [CrossRef]
- Schöttke, H.; Gerke, L.; Düsing, R.; Möllmann, A. Post-Stroke Depression and Functional Impairments—A 3-Year Prospective Study. Compr. Psychiatry 2020, 99, 152171. [Google Scholar] [CrossRef]
- Ladwig, S.; Werheid, K.; Südmeyer, M.; Volz, M. Predictors of Post-Stroke Depression: Validation of Established Risk Factors and Introduction of a Dynamic Perspective in Two Longitudinal Studies. Front. Psychiatry 2023, 14, 1093918. [Google Scholar] [CrossRef]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Pers. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Kliem, S.; Mößle, T.; Rehbein, F.; Hellmann, D.F.; Zenger, M.; Brähler, E. A Brief Form of the Perceived Social Support Questionnaire (F-SozU) Was Developed, Validated, and Standardized. J. Clin. Epidemiol. 2015, 68, 551–562. [Google Scholar] [CrossRef]
- Xiao, S. The Theoretical Basis and Applications of Social Support Rating Scale. J. Clin. Psychiatry 1994, 02, 98–100. [Google Scholar]
- Sherbourne, C.D.; Stewart, A.L. The MOS Social Support Survey. Soc. Sci. Med. 1991, 32, 705–714. [Google Scholar] [CrossRef]
- Fydrich, T.; Geyer, M.A.; Hessel, A.; Sommer, G.; Brähler, E. Fragebogen Zur Sozialen Unterstützung (F-SozU): Normierung an Einer Repräsentativen Stichprobe. Diagnostica 1999, 45, 212–216. [Google Scholar] [CrossRef]
- Fydrich, T.; Sommer, G.; Tydecks, S.; Brähler, E. Fragebogen Zur Sozialen Unterstützung (F-SozU): Normierung Der Kurzform (K-14) Social Support Questionnaire (F-SozU): Standardization of Short Form (K-14). Z. Für Med. Psychol. 2009, 18, 43–48. [Google Scholar]
- Liu, R.; Yue, Y.; Jiang, H.; Lu, J.; Wu, A.; Geng, D.; Wang, J.; Lu, J.; Li, S.; Tang, H.; et al. A Risk Prediction Model for Post-Stroke Depression in Chinese Stroke Survivors Based on Clinical and Socio-Psychological Features. Oncotarget 2017, 8, 62891–62899. [Google Scholar] [CrossRef]
- Bell, C.C. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. JAMA 1994, 272, 828–829. [Google Scholar] [CrossRef]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The Development and Validation of a Structured Diagnostic Psychiatric Interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59, 22–33. [Google Scholar]
- Snaith, R.P. The Hospital Anxiety and Depression Scale. Health Qual. Life Outcomes 2003, 1, 6–9. [Google Scholar] [CrossRef]
- Alexopoulos, G.S.; Abrams, R.C.; Young, R.C.; Shamoian, C. The Cornell Scale for Depression in Dementia: Administration & Scoring Guidelines. Biol. Psychiatry 1988, 23, 271–284. [Google Scholar] [PubMed]
- Hamilton, M. A Rating Scale of Depression. J. Neurol. Neurosurg. Psychiatry 1969, 23, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Radloff, L.S. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Stone, L.; Granier, K.; Segal, D.L. Geriatric Depression Scale. Encycl. Gerontol. Popul. Aging 2019, 1, 709–711. [Google Scholar]
- Neff, A.J.; Lee, Y.; Metts, C.L.; Wong, A.W.K. Ecological Momentary Assessment of Social Interactions: Associations With Depression, Anxiety, Pain, and Fatigue in Individuals With Mild Stroke. Physiol. Behav. 2021, 102, 395–405. [Google Scholar] [CrossRef] [PubMed]
- Grey, I.; Arora, T.; Thomas, J.; Saneh, A.; Tohme, P.; Abi-Habib, R. The Role of Perceived Social Support on Depression and Sleep during the COVID-19 Pandemic. Psychiatry Res. 2020, 293, 113452. [Google Scholar] [CrossRef]
- Wang, J.; Xue, J.; Jiang, Y.; Zhu, T.; Chen, S. Mediating Effects of Depressive Symptoms on Social Support and Quality of Life among Rural Older Chinese. Health Qual. Life Outcomes 2020, 18, 242. [Google Scholar] [CrossRef]
- Patra, P.; Alikari, V.; Fradelos, E.C.; Sachlas, A.; Kourakos, M.; Rojas Gil, A.P.; Babatsikou, F.; Zyga, S. Assessment of Depression in Elderly. Is Perceived Social Support Related? A Nursing Home Study: Depression and Social Support in Elderly. Adv. Exp. Med. Biol. 2017, 987, 139–150. [Google Scholar] [CrossRef]
- Tang, L.; Wang, D.; Bai, Z.; Zhu, Y.; Chen, R. Relationship between Social Support and Depression among Older People from Elderly Care Social Organizations in Anhui Province, China. Rev. Epidemiol. Sante Publique 2022, 70, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M. A Rating Scale for Depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef] [PubMed]
- VanderWeele, T.J.; Ding, P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann. Intern. Med. 2017, 167, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Ilut, S.; Stan, A.; Blesneag, A.; Vacaras, V.; Vesa, S.; Fodoreanu, L. Factors That Influence the Severity of Post-Stroke Depression. J. Med. Life 2017, 10, 167–171. [Google Scholar]
- Powers, W.J.; Derdeyn, C.P.; Biller, J.; Coffey, C.S.; Hoh, B.L.; Jauch, E.C.; Johnston, K.C.; Johnston, S.C.; Khalessi, A.A.; Kidwell, C.S.; et al. 2015 American Heart Association/American Stroke Association Focused Update of the 2013 Guidelines for the Early Management of Patients with Acute Ischemic Stroke Regarding Endovascular Treatment: A Guideline for Healthcare Professionals from the American. Stroke 2015, 46, 3020–3035. [Google Scholar] [CrossRef]
- Ding, P.; VanderWeele, T.J. Sensitivity Analysis without Assumptions. Epidemiology 2016, 27, 368–377. [Google Scholar] [CrossRef]
- Trinquart, L.; Erlinger, A.L.; Petersen, J.M.; Fox, M.; Galea, S. Applying the e Value to Assess the Robustness of Epidemiologic Fields of Inquiry to Unmeasured Confounding. Am. J. Epidemiol. 2019, 188, 1174–1180. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).