Upper Airway-Related Symptoms According to Mental Illness and Sleep Disorders among Workers Employed by a Large Non-Profit Organization in the Mountain West Region of the United States
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Statistical Techniques
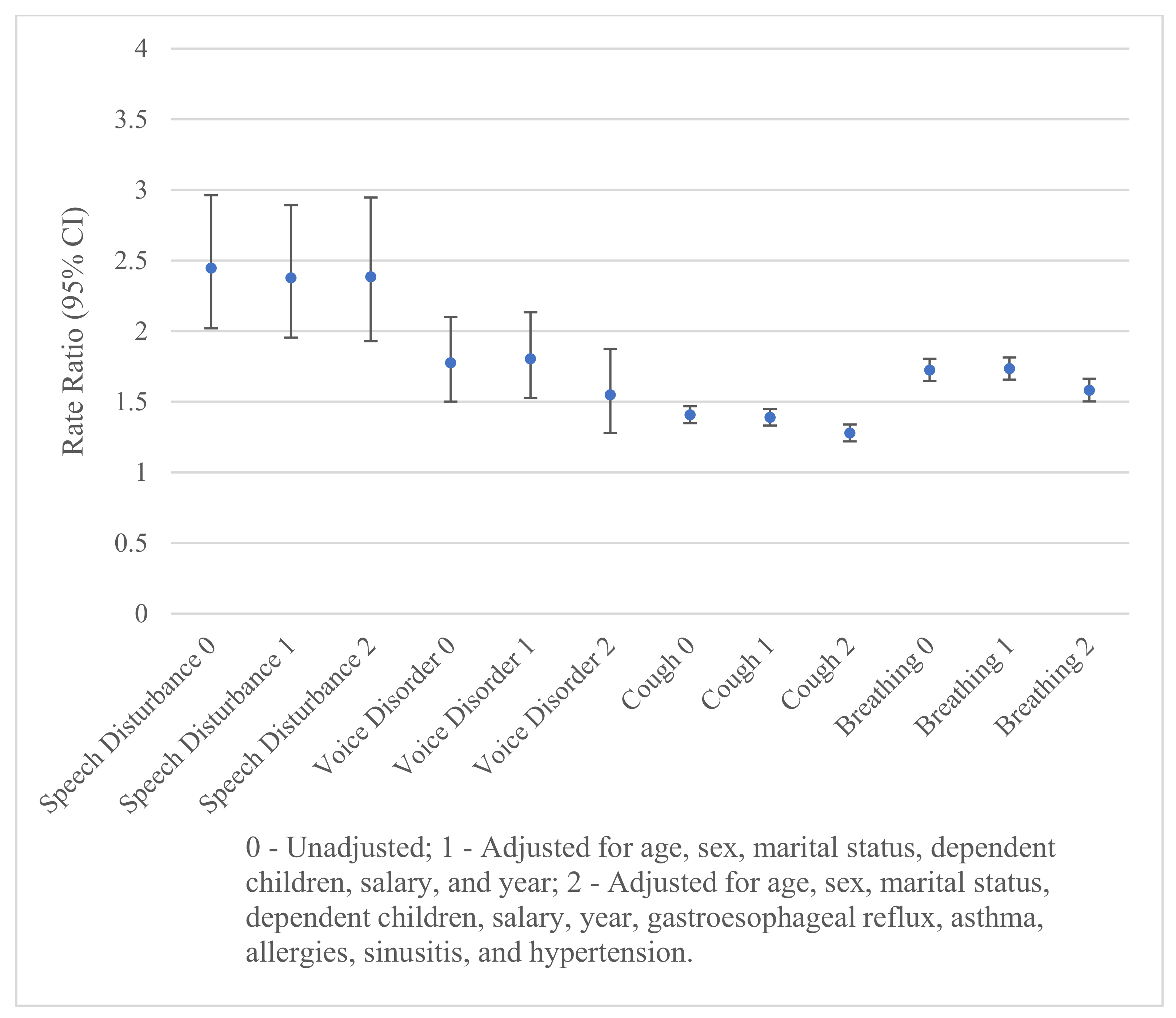
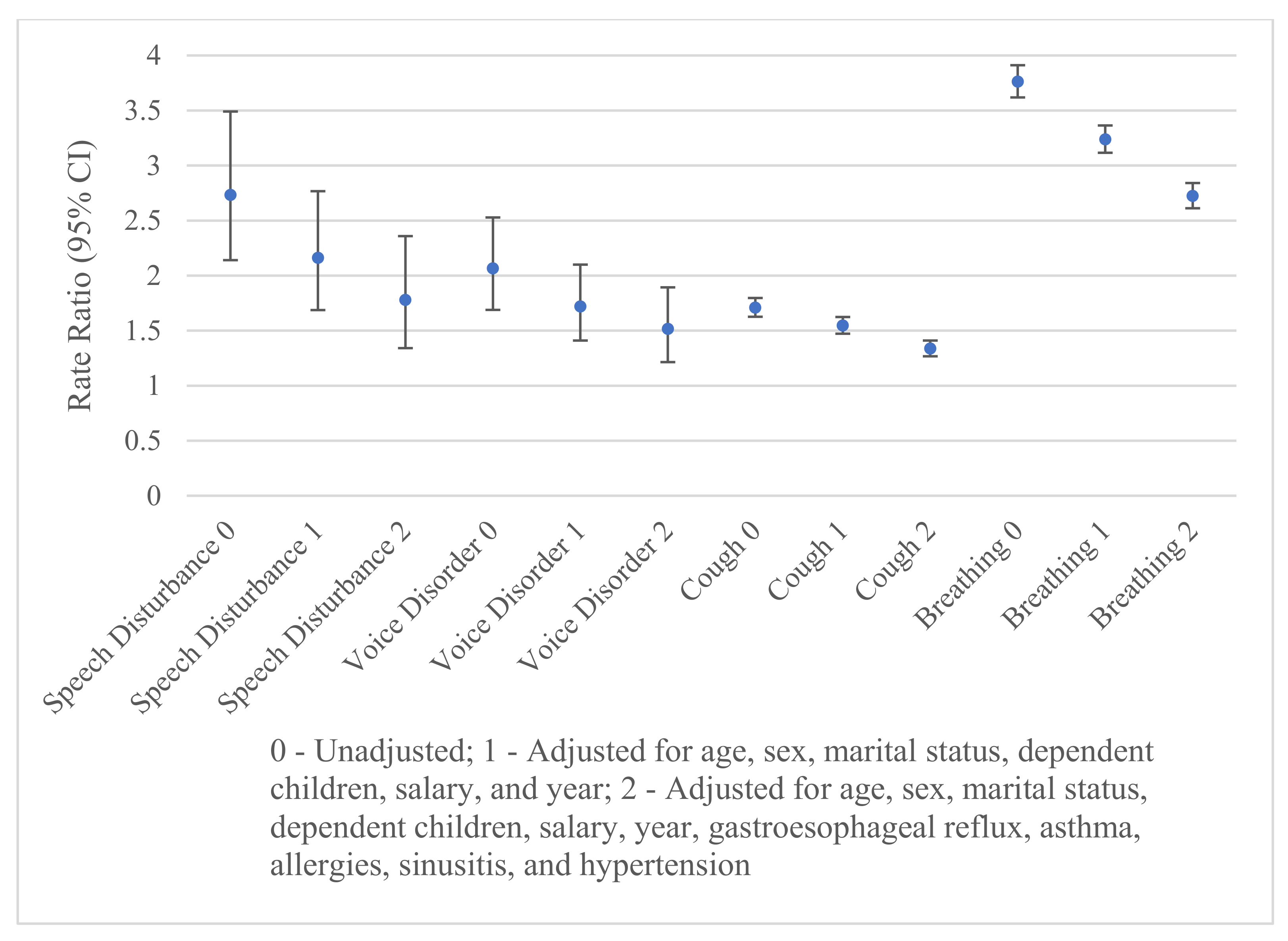
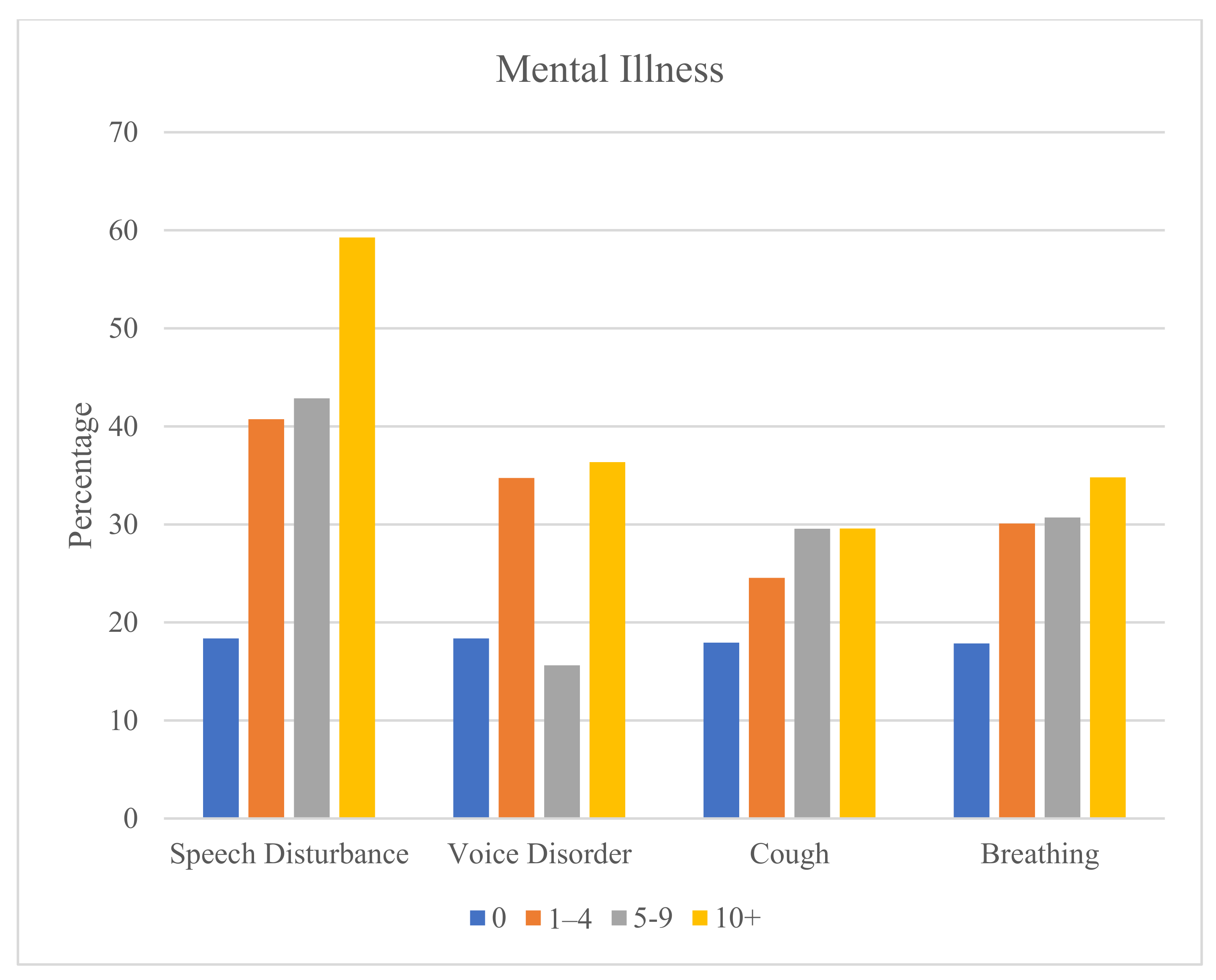
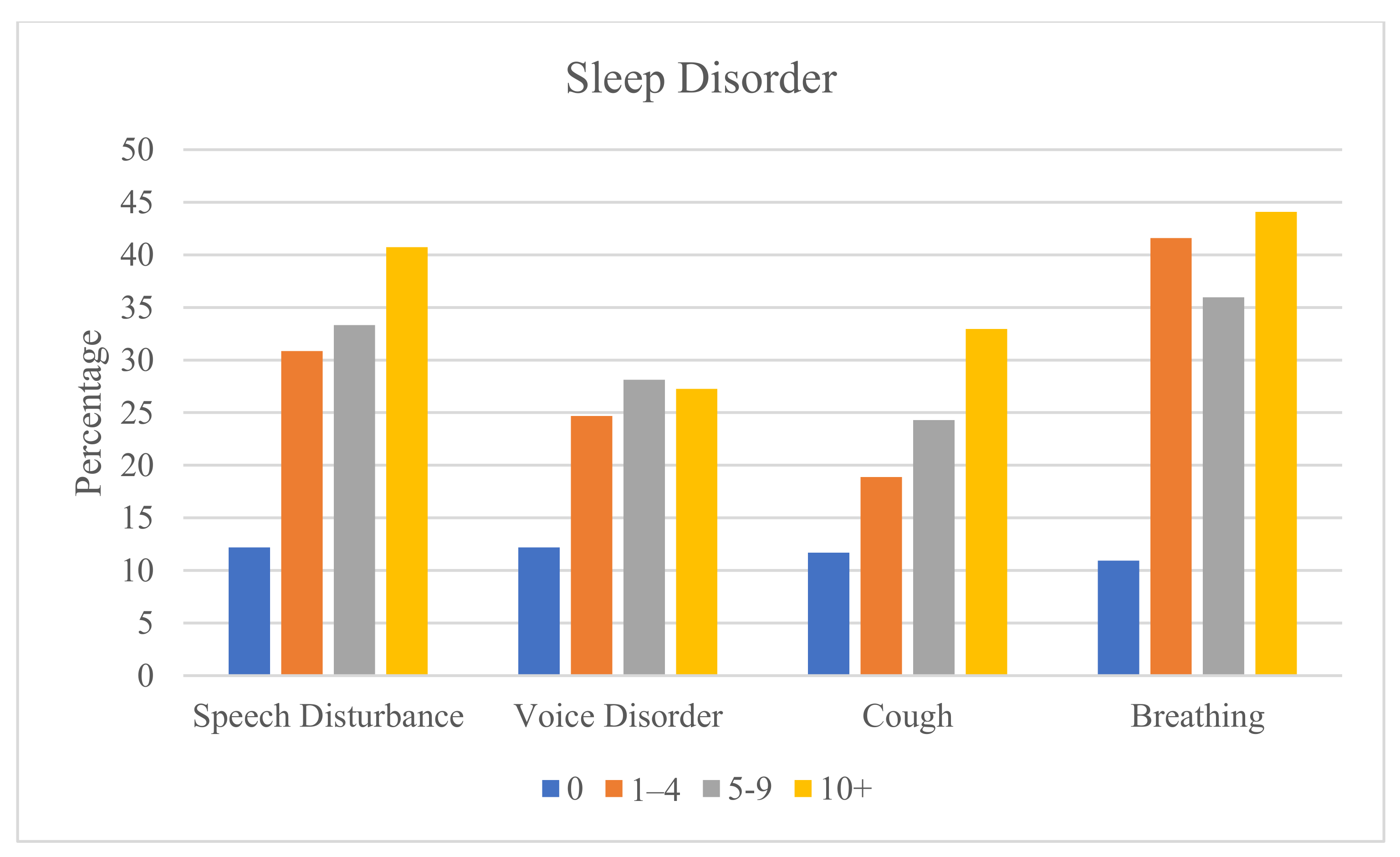
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vasenina, E.E.; Levin, O.S. Narushenie rechi i trevoga: Mekhanizmy vzaimodeistviya i vozmozhnosti terapii [Speech disorders and anxiety: Interaction mechanisms and therapy potential]. Zh. Nevrol. Psikhiatr. Im. SS Korsakova 2020, 120, 136–144. [Google Scholar] [CrossRef]
- Nerrière, E.; Vercambre, M.N.; Gilbert, F.; Kovess-Masféty, V. Voice disorders and mental health in teachers: A cross-sectional nationwide study. BMC Public Health 2009, 9, 370. [Google Scholar] [CrossRef]
- Barbosa, I.K.; Behlau, M.; Lima-Silva, M.F.; Almeida, L.N.; Farias, H.; Almeida, A.A. Voice symptoms, perceived voice control, and common mental disorders in elementary school teachers. J. Voice 2021, 35, 158.e1–158.e7. [Google Scholar] [CrossRef]
- Adams, R.J.; Appleton, S.L.; Wilson, D.H.; Taylor, A.W.; Ruffin, R.E. Associations of physical and mental health problems with chronic cough in a representative population cohort. Cough 2009, 5, 10. [Google Scholar] [CrossRef]
- Worsham, C.M.; Banzett, R.B.; Schwartzstein, R.M. Abnormalities of breathing, acute respiratory failure, psychological trauma, and post-ICU mental health: A caution and a call for research. Chest 2021, 159, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Mukerji, V. Abnormalities of breathing, orthopnea, and paroxysmal nocturnal abnormalities of breathing. In Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd ed.; Walker, H.K., Hall, W.D., Hurst, J.W., Eds.; Butterworths: Boston, MA, USA, 1990; Chapter 11. [Google Scholar]
- Jones, K.; Harrison, Y. Frontal lobe function, sleep loss and fragmented sleep. Sleep Med. Rev. 2001, 5, 463–475. [Google Scholar] [CrossRef] [PubMed]
- Rocha, B.R.; Behlau, M. The influence of sleep disorders on voice quality. J. Voice 2018, 32, 771.e1–771.e13. [Google Scholar] [CrossRef]
- Lee, K.K.; Birring, S.S. Cough and sleep. Lung 2010, 188, S91–S94. [Google Scholar] [CrossRef]
- Aihara, K.; Oga, T.; Yoshimura, C.; Hitomi, T.; Chihara, Y.; Harada, Y.; Murase, K.; Toyama, Y.; Tanizawa, K.; Handa, T.; et al. Measurement of dyspnea in patients with obstructive sleep apnea. Sleep Breath. 2013, 17, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, D.; Park, V.; Bogaardt, H.; Docking, K. The impact of childhood obstructive sleep apnea on speech and oral language development: A systematic review. Sleep Med. 2021, 81, 144–153. [Google Scholar] [CrossRef]
- Birring, S.S.; Ing, A.J.; Chan, K.; Cossa, G.; Matos, S.; Morgan, M.D.L.; Pavord, I.D. Obstructive sleep apnoea: A cause of chronic cough. Cough 2007, 3, 7. [Google Scholar] [CrossRef]
- Roy, N.; Merrill, R.M.; Pierce, J.; Sundar, K.M. Evidence of possible irritable larynx syndrome in obstructive sleep apnea: An epidemiologic approach. J Voice 2021, 35, 932.e29–932.e38. [Google Scholar] [CrossRef]
- Merrill, R.M.; Roy, N.; Pierce, J.; Sundar, K.M. Impact of voice, cough, and diurnal breathing problems on quality of life in obstructive sleep apnea. Do they matter? AOHNS 2020, 4, 3. [Google Scholar] [CrossRef]
- Sereg-Bahar, M.; Jansa, R.; Hocevar-Boltezar, I. Voice disorders and gastroesophageal reflux. Logoped. Phoniatr. Vocol. 2005, 30, 120–124. [Google Scholar] [CrossRef]
- Kahrilas, P.J.; Altman, K.W.; Chang, A.B.; Field, S.K.; Harding, S.M.; Lane, A.P.; Lim, K.; McGarvery, L.; Smith, J.; Irwin, R.S. Chronic cough due to gastroesophageal reflux in adults: CHEST guideline and expert panel report. Chest 2016, 150, 1341–1360. [Google Scholar] [CrossRef]
- Clarrett, D.M.; Hachem, C. Gastroesophageal reflux disease (GERD). Mo. Med. 2018, 115, 214–218. [Google Scholar]
- Hassen, H.E.; Abo Hasseba, A.M. Voice evaluation in asthma patients using inhaled corticosteroids. Kulak Burun Bogaz Ihtis. Derg. 2016, 26, 101–108. [Google Scholar] [CrossRef]
- Turcotte, S.E.; Lougheed, M.D. Cough in asthma. Curr. Opin. Pharmacol. 2011, 11, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Scano, G.; Stendardi, L. Dyspnea and asthma. Curr. Opin. Pulm. Med. 2006, 12, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Dicpinigaitis, P.V. Chronic cough due to asthma: ACCP evidence-based clinical practice guidelines. Chest 2006, 129, 75S–79S. [Google Scholar] [CrossRef] [PubMed]
- Ohlsson, A.C.; Drevsäter, A.; Brynnel, M.; Johansson, I. Allergic rhinitis and voice change. Logoped. Phoniatr. Vocol. 2016, 41, 143–148. [Google Scholar] [CrossRef]
- Simberg, S.; Sala, E.; Tuomainen, J.; Rönnemaa, A.M. Vocal symptoms and allergy–A pilot study. J. Voice 2009, 23, 136–139. [Google Scholar] [CrossRef] [PubMed]
- Gawchik, S.; Goldstein, S.; Prenner, B.; John, A. Relief of cough and nasal symptoms associated with allergic rhinitis by mometasone furoate nasal spray. Ann. Allergy Asthma Immunol. 2003, 90, 416–421. [Google Scholar] [CrossRef]
- Cleveland Clinic: Dyspnea. Available online: https://my.clevelandclinic.org/health/symptoms/16942-dyspnea (accessed on 24 August 2023).
- Willis, J.; Michael, D.D.; Boyer, H.; Misono, S. Prevalence and severity of dysphonia in patients with cystic fibrosis: A pilot study. Otolaryngol. Head Neck Surg. 2015, 153, 88–93. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tatar, M.; Plevkova, J.; Brozmanova, M.; Pecova, R.; Kollarik, M. Mechanisms of the cough associated with rhinosinusitis. Pulm. Pharmacol. Ther. 2009, 22, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Budhwar, N.; Syed, Z. Chronic abnormalities of breathing: Diagnosis and evaluation. Am. Fam. Physician. 2020, 101, 542–548. [Google Scholar] [PubMed]
- Bainbridge, K.E.; Roy, N.; Losonczy, K.G.; Hoffman, H.J.; Cohen, S.M. Voice disorders and associated risk markers among young adults in the United States. Laryngoscope 2017, 127, 2093–2099. [Google Scholar] [CrossRef]
- Dockry, R.; Gibbard, C.; Mitchell, J.; Holt, K.; Corfield, D.; Smith, J. Chronic cough is associated with an increased risk of hypertension. Eur. Respir. J. 2018, 52, PA814. [Google Scholar]
- Dumitrescu, D.; Sitbon, O.; Weatherald, J.; Howard, L.S. Exertional dyspnoea in pulmonary arterial hypertension. Eur. Respir. Rev. 2017, 26, 170039. [Google Scholar] [CrossRef]
- Zeng, Y.; Cao, S.; Yang, H. The causal role of gastroesophageal reflux disease in anxiety disorders and depression: A bidirectional Mendelian randomization study. Front. Psychiatry 2023, 14, 1135923. [Google Scholar] [CrossRef]
- Zhu, Z.; Zhu, X.; Liu, C.L.; Shi, H.; Shen, S.; Yang, Y.; Hasegawa, K.; Camargo, C.A., Jr.; Liang, L. Shared genetics of asthma and mental health disorders: A large-scale genome-wide cross-trait analysis. Eur. Respir. J. 2019, 54, 1901507. [Google Scholar] [CrossRef]
- Scott, K.M.; Von Korff, M.; Ormel, J.; Zhang, M.Y.; Bruffaerts, R.; Alonso, J.; Kessler, R.C.; Tachimori, H.; Karam, E.; Levinson, D.; et al. Mental disorders among adults with asthma: Results from the World Mental Health Survey. Gen. Hosp. Psychiatry 2007, 29, 123–133. [Google Scholar] [CrossRef]
- Aberle, D.; Wu, S.E.; Oklu, R.; Erinjeri, J.; Deipolyi, A.R. Association between allergies and psychiatric disorders in patients undergoing invasive procedures. Psychosomatics 2017, 58, 490–495. [Google Scholar] [CrossRef]
- Oh, H.; Koyanagi, A.; DeVylder, J.E.; Stickley, A. Seasonal allergies and psychiatric disorders in the United States. Int. J. Environ. Res. Public Health 2018, 15, 1965. [Google Scholar] [CrossRef] [PubMed]
- Schlosser, R.J.; Storck, K.; Cortese, B.M.; Uhde, T.W.; Rudmik, L.; Soler, Z.M. Depression in chronic rhinosinusitis: A controlled cohort study. Am. J. Rhinol. Allergy 2016, 30, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Stein, D.J.; Aguilar-Gaxiola, S.; Alonso, J.; Bruffaerts, R.; de Jonge, P.; Liu, Z.; Caldas-de-Almeida, J.M.; O’Neill, S.; Viana, M.C.; Al-Hamzawi, A.O.; et al. Associations between mental disorders and subsequent onset of hypertension. Gen. Hosp. Psychiatry 2014, 36, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Fujiwara, Y.; Arakawa, T.; Fass, R. Gastroesophageal reflux disease and sleep disturbances. J. Gastroenterol. 2012, 47, 760–769. [Google Scholar] [CrossRef]
- Cukic, V.; Lovre, V.; Dragisic, D. Sleep disorders in patients with bronchial asthma. Mater. Sociomed. 2011, 23, 235–237. [Google Scholar] [CrossRef] [PubMed]
- Koinis-Mitchell, D.; Craig, T.; Esteban, C.A.; Klein, R.B. Sleep and allergic disease: A summary of the literature and future directions for research. J. Allergy Clin. Immunol. 2012, 130, 1275–1281. [Google Scholar] [CrossRef] [PubMed]
- Papagiannopoulos, P.; Kuan, E.C.; Tajudeen, B.A. Chronic rhinosinusitis and sleep quality. Curr. Opin. Otolaryngol. Head Neck Surg. 2020, 28, 11–13. [Google Scholar] [CrossRef]
- Li, C.; Shang, S. Relationship between sleep and hypertension: Findings from the NHANES (2007–2014). Int. J. Environ. Res. Public Health 2021, 18, 7867. [Google Scholar] [CrossRef] [PubMed]
- International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). Available online: https://www.cdc.gov/nchs/icd/icd-10-cm.htm (accessed on 10 September 2023).
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; Text Revision; American Psychiatric Association Publishing: Washington, DC, USA, 2022. [Google Scholar] [CrossRef]
- Bai, H.; Sha, B.; Xu, X.; Yu, L. Gender difference in chronic cough: Are women more likely to cough? Front. Physiol. 2021, 12, 654797. [Google Scholar] [CrossRef] [PubMed]
- Lowery, E.M.; Brubaker, A.L.; Kuhlmann, E.; Kovacs, E.J. The aging lung. Clin. Interv. Aging 2013, 8, 1489–1496. [Google Scholar] [PubMed]
- Hippisley-Cox, J.; Coupland, C.; Pringle, M.; Crown, N.; Hammersley, V. Married couples’ risk of same disease: Cross sectional study. BMJ 2002, 325, 636. [Google Scholar] [CrossRef] [PubMed]
- ENT Health: Hoarseness. Available online: https://www.enthealth.org/conditions/hoarseness/ (accessed on 23 October 2023).
- Rattay, P.; von der Lippe, E. Association between living with children and the health and health behavior of women and men. Are there differences by age? Results of the “German Health Update” (GEDA) Study. Int. J. Environ. Res. Public Health 2020, 17, 3180. [Google Scholar] [CrossRef] [PubMed]
- Sahni, S.; Talwar, A.; Khanijo, S.; Talwar, A. Socioeconomic status and its relationship to chronic respiratory disease. Adv. Respir. Med. 2017, 85, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Abouzgheib, W.; Pratter, M.R.; Bartter, T. Cough and asthma. Curr. Opin. Pulm. Med. 2007, 13, 44–48. [Google Scholar] [CrossRef]
- Li, Y.; Cao, C.; Ji, Y.; Xu, S. Anxiety and depression are associated with reduced quality of life and increased cough severity in chronic cough. Asian Pac. J. Allergy Immunol. 2022. Online ahead of print. [Google Scholar]
- Weiner, L.; Doignon-Camus, N.; Bertschy, G.; Giersch, A. Thought and language disturbance in bipolar disorder quantified via process-oriented verbal fluency measures. Sci. Rep. 2019, 9, 14282. [Google Scholar] [CrossRef]
- Ragin, A.B.; Oltmanns, T.F. Communicability and thought disorder in schizophrenics and other diagnostic groups. A follow-up study. Br. J. Psychiatry 1987, 150, 494–500. [Google Scholar] [CrossRef]
- France, D.J.; Shiavi, R.G.; Silverman, S.; Silverman, M.; Wilkes, D.M. Acoustical properties of speech as indicators of depression and suicidal risk. IEEE Trans. Biomed. Eng. 2000, 47, 829–837. [Google Scholar] [CrossRef] [PubMed]
- Zdanowicz, T.; Turowski, K.; Celej-Szuster, J.; Lorencowicz, R.; Przychodzka, E. Insomnia, sleepiness, and fatigue among polish nurses. Workplace Health Saf. 2020, 68, 272–278. [Google Scholar] [CrossRef] [PubMed]
| No. | % | Speech Disturbances | Voice Disorders | Cough | Breathing Abnormalities | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rate Ratio † | 95% LCL † | 95% UCL † | Rate Ratio † | 95% LCL † | 95% UCL † | Rate Ratio † | 95% LCL † | 95% UCL † | Rate Ratio † | 95% LCL † | 95% UCL † | |||
| Sex | ||||||||||||||
| Men | 73,446 | 68.76 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Women | 33,363 | 31.24 | 1.30 | 0.86 | 1.96 | 1.13 | 0.83 | 1.54 | 1.25 | 1.18 | 1.32 | 0.99 | 0.92 | 1.06 |
| Age | ||||||||||||||
| 18–29 | 12,143 | 11.37 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 30–39 | 22,967 | 21.50 | 1.58 | 0.39 | 6.38 | 1.69 | 0.82 | 3.50 | 1.37 | 1.21 | 1.54 | 1.45 | 1.24 | 1.71 |
| 40–49 | 27,495 | 25.74 | 4.47 | 1.22 | 16.33 | 3.53 | 1.69 | 7.41 | 1.64 | 1.46 | 1.85 | 2.22 | 1.91 | 2.59 |
| 50–59 | 28,323 | 26.52 | 5.54 | 1.43 | 21.44 | 4.15 | 1.97 | 8.74 | 2.00 | 1.79 | 2.24 | 2.38 | 2.05 | 2.76 |
| 60–64 | 15,881 | 14.87 | 15.97 | 4.26 | 59.90 | 4.80 | 2.15 | 10.73 | 2.25 | 1.99 | 2.55 | 2.78 | 2.37 | 3.25 |
| Married | ||||||||||||||
| No | 22,808 | 21.35 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Yes | 84,001 | 78.65 | 0.70 | 0.42 | 1.15 | 1.00 | 0.69 | 1.46 | 1.20 | 1.11 | 1.29 | 1.20 | 1.10 | 1.31 |
| Dependent Children | ||||||||||||||
| No | 37,806 | 35.4 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Yes | 69,003 | 64.6 | 2.01 | 1.25 | 3.23 | 0.90 | 0.66 | 1.22 | 0.94 | 0.88 | 1.00 | 0.90 | 0.83 | 0.97 |
| Annual Salary | ||||||||||||||
| <50 K | 30,448 | 28.51 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 50–<100 K | 41,964 | 39.29 | 0.93 | 0.59 | 1.48 | 1.08 | 0.78 | 1.51 | 1.10 | 1.03 | 1.17 | 0.87 | 0.81 | 0.94 |
| ≥100 K | 29,892 | 27.99 | 0.65 | 0.37 | 1.16 | 1.15 | 0.75 | 1.77 | 1.06 | 0.98 | 1.14 | 0.82 | 0.75 | 0.90 |
| Missing | 4505 | 4.22 | 1.51 | 0.87 | 2.64 | 1.11 | 0.61 | 2.04 | 0.93 | 0.82 | 1.06 | 1.18 | 1.03 | 1.35 |
| Year | ||||||||||||||
| 2017 | 21,360 | 20.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 2018 | 21,835 | 20.44 | 0.87 | 0.51 | 1.49 | 1.07 | 0.74 | 1.54 | 0.98 | 0.90 | 1.05 | 0.97 | 0.89 | 1.07 |
| 2019 | 21,663 | 20.28 | 0.97 | 0.58 | 1.62 | 1.14 | 0.79 | 1.64 | 1.00 | 0.93 | 1.08 | 1.10 | 1.00 | 1.20 |
| 2020 | 20,891 | 19.56 | 1.03 | 0.61 | 1.74 | 0.80 | 0.53 | 1.20 | 1.53 | 1.42 | 1.64 | 1.25 | 1.14 | 1.37 |
| 2021 | 21,060 | 19.72 | 0.56 | 0.30 | 1.05 | 1.13 | 0.78 | 1.63 | 1.17 | 1.09 | 1.26 | 1.12 | 1.02 | 1.23 |
| Stress | Anx | Dep | ADHD | Bipolar | OCD | Schizo | Suicidal Ideation | Insomnia | Hypersomnia | Sleep Apnea | Other Sleep | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | % | % | % | % | % | % | % | % | % | % | % | % | |
| All Employed | 106,809 | 100 | 2.24 | 9.46 | 8.46 | 2.05 | 0.65 | 0.41 | 0.09 | 0.14 | 2.25 | 1.07 | 10.18 | 0.80 |
| Speech Disturb | 129 | 0.12 | 6.98 | 21.71 | 20.16 | 2.33 | 1.55 | --- | 0.78 | 1.55 | 10.08 | 3.88 | 24.81 | 4.65 |
| Voice Disorders | 282 | 0.26 | 6.03 | 18.09 | 17.02 | 2.84 | 0.71 | 1.06 | 0.35 | 0.71 | 5.67 | 2.84 | 21.28 | 1.42 |
| Cough | 7010 | 6.56 | 3.62 | 13.47 | 12.01 | 2.57 | 1.11 | 0.61 | 0.11 | 0.19 | 3.98 | 2.01 | 16.90 | 1.26 |
| Breathing | 4570 | 4.28 | 3.96 | 17.55 | 15.54 | 2.63 | 1.05 | 0.55 | 0.15 | 0.33 | 5.40 | 6.13 | 36.81 | 4.27 |
| Speech Disturbances | Voice Disorders | Cough | Breathing Abnormalities | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | Rate Ratio† | 95% LCL † | 95% UCL † | Odds Ratio † | 95% LCL † | 95% UCL † | Rate Ratio † | 95% LCL † | 95% UCL † | Rate Ratio † | 95% LCL † | 95% UCL † | |
| Gastroesophageal Reflux | 4637 | 4.34 | 2.89 | 1.76 | 4.75 | 7.65 | 5.90 | 9.91 | 2.10 | 1.95 | 2.26 | 2.44 | 2.24 | 2.66 |
| Asthma | 3505 | 3.28 | 2.37 | 1.32 | 4.26 | 4.20 | 2.96 | 5.95 | 3.65 | 3.42 | 3.90 | 4.54 | 4.21 | 4.90 |
| Allergies | 4032 | 3.77 | 1.44 | 0.68 | 3.08 | 3.95 | 2.83 | 5.51 | 2.44 | 2.26 | 2.63 | 2.48 | 2.25 | 2.73 |
| Chronic Sinusitis | 3147 | 2.95 | 1.44 | 0.63 | 3.28 | 2.02 | 1.25 | 3.26 | 2.54 | 2.35 | 2.76 | 2.12 | 1.89 | 2.37 |
| Hypertension | 14,519 | 13.59 | 2.90 | 2.00 | 4.23 | 1.23 | 0.91 | 1.66 | 1.48 | 1.40 | 1.57 | 2.29 | 2.14 | 2.44 |
| Stress | Anx | Dep | ADHD | Bipolar | OCD | Schizo | Suicidal Ideation | Insomnia | HypersSomnia | Sleep Apnea | Other Sleep | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rate Ratio † | ||||||||||||
| Gastroesophageal Reflux | 1.93 | 1.76 | 1.72 | 1.44 | 1.90 | 1.58 | 1.82 | 3.29 | 1.77 | 2.07 | 1.73 | 2.29 |
| Asthma | 1.69 | 1.51 | 1.66 | 1.93 | 2.03 | 0.90 | 3.67 | 2.45 | 1.71 | 2.32 | 2.24 | 1.74 |
| Allergies | 1.56 | 1.52 | 1.48 | 1.71 | 1.44 | 2.28 | 2.07 | 1.64 | 1.79 | 1.74 | 1.77 | 1.47 |
| Chronic Sinusitis | 1.21 | 1.52 | 1.50 | 1.53 | 1.86 | 1.35 | 1.13 | 2.75 | 1.73 | 1.60 | 1.57 | 1.99 |
| Hypertension | 1.07 | 1.30 | 1.43 | 1.56 | 1.32 | 1.00 | 1.14 | 1.50 | 1.30 | 1.91 | 2.38 | 1.42 |
| Stress | Anx | Dep | ADHD | Bipolar | OCD | Schizo | Suicidal Ideation | Insomnia | Hypersomnia | Sleep Apnea | Other Sleep | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rate Ratio † | ||||||||||||
| Speech Disturb | 2.70 | 2.30 | 2.20 | 1.33 | 2.58 | --- | 1.90 | 7.47 | 3.29 | 3.46 | 1.94 | 5.28 |
| Voice Disorders | 2.75 | 1.99 | 1.97 | 1.62 | 1.05 | 3.41 | 4.72 | 6.86 | 2.14 | 2.36 | 1.73 | 1.63 |
| Cough | 1.63 | 1.46 | 1.43 | 1.33 | 1.91 | 1.73 | 1.26 | 1.54 | 1.69 | 1.87 | 1.57 | 1.58 |
| Breathing | 1.83 | 1.98 | 1.89 | 1.40 | 1.60 | 1.56 | 1.32 | 2.76 | 2.24 | 6.69 | 3.48 | 6.21 |
| Rate Ratio ‡ | ||||||||||||
| Speech Disturb | 2.87 | 2.61 | 2.08 | 1.62 | 1.80 | --- | 4.44 | 3.23 | 3.18 | 2.62 | 1.46 | 6.27 |
| Voice Disorders | 2.95 | 1.60 | 1.81 | 1.54 | 1.13 | 4.11 | 1.48 | 5.46 | 2.05 | 1.42 | 1.48 | 0.81 |
| Cough | 1.59 | 1.36 | 1.30 | 1.20 | 1.78 | 1.69 | 1.00 | 1.31 | 1.50 | 1.62 | 1.34 | 1.54 |
| Breathing | 1.61 | 1.82 | 1.69 | 1.24 | 1.43 | 1.48 | 1.21 | 1.87 | 2.00 | 5.66 | 2.89 | 5.60 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Merrill, R.M.; Gibbons, I.S.; Barker, C.J. Upper Airway-Related Symptoms According to Mental Illness and Sleep Disorders among Workers Employed by a Large Non-Profit Organization in the Mountain West Region of the United States. Int. J. Environ. Res. Public Health 2023, 20, 7173. https://doi.org/10.3390/ijerph20247173
Merrill RM, Gibbons IS, Barker CJ. Upper Airway-Related Symptoms According to Mental Illness and Sleep Disorders among Workers Employed by a Large Non-Profit Organization in the Mountain West Region of the United States. International Journal of Environmental Research and Public Health. 2023; 20(24):7173. https://doi.org/10.3390/ijerph20247173
Chicago/Turabian StyleMerrill, Ray M., Ian S. Gibbons, and Christian J. Barker. 2023. "Upper Airway-Related Symptoms According to Mental Illness and Sleep Disorders among Workers Employed by a Large Non-Profit Organization in the Mountain West Region of the United States" International Journal of Environmental Research and Public Health 20, no. 24: 7173. https://doi.org/10.3390/ijerph20247173
APA StyleMerrill, R. M., Gibbons, I. S., & Barker, C. J. (2023). Upper Airway-Related Symptoms According to Mental Illness and Sleep Disorders among Workers Employed by a Large Non-Profit Organization in the Mountain West Region of the United States. International Journal of Environmental Research and Public Health, 20(24), 7173. https://doi.org/10.3390/ijerph20247173







