A Single Session of a Digital Health Tool-Delivered Exercise Intervention May Provide Immediate Relief from Pelvic Pain in Women with Endometriosis: A Pilot Randomized Controlled Study
Abstract
:1. Introduction
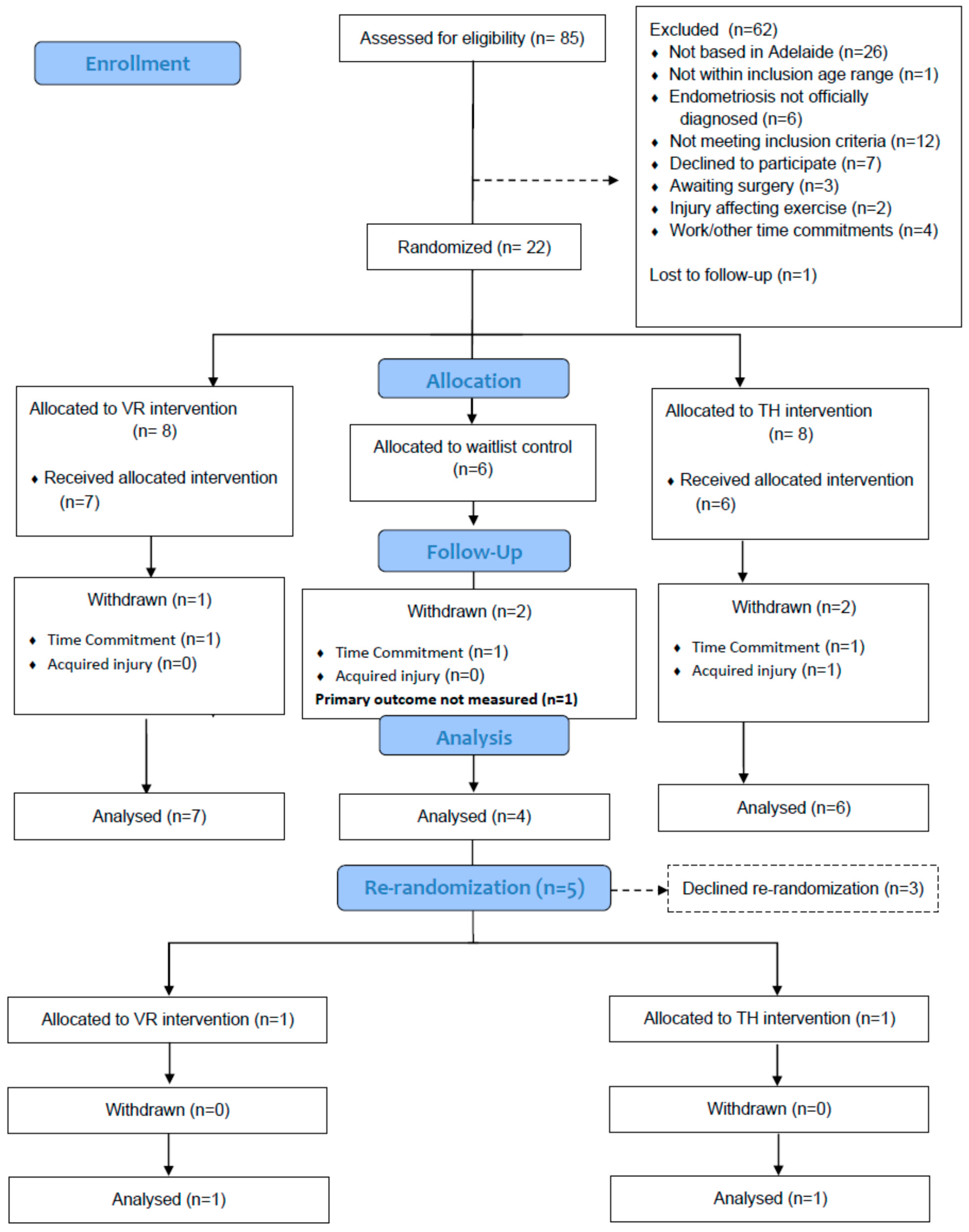
2. Materials and Methods
2.1. Acute Pelvic Pain
2.2. Cardiorespiratory Fitness
2.3. Telehealth Session
2.4. Virtual Reality Session
2.5. Statistical Analysis
3. Results
Pelvic Pain
4. Discussion
4.1. Practical Considerations
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oats, J.; Abraham, S. Llewellyn-Jones Fundamentals of Obstetrics and Gynaecology E-Book; Elsevier Health Sciences: Berlin/Heidelberg, Germany, 2015. [Google Scholar]
- Shafrir, A.L.; Farland, L.; Shah, D.; Harris, H.; Kvaskoff, M.; Zondervan, K.; Missmer, S. Risk for and consequences of endometriosis: A critical epidemiologic review. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 51, 1–15. [Google Scholar] [CrossRef]
- Young, E. The cost of endometriosis in Australia: A report for EndoActive by Ernst & Young. EndoActive 2019, 6. unpublished. [Google Scholar]
- Nnoaham, K.E.; Hummelshoj, L.; Webster, P.; d’Hooghe, T.; de Cicco Nardone, F.; de Cicco Nardone, C.; Jenkinson, C.; Kennedy, S.H.; Zondervan, K.T.; World Endometriosis Research Foundation Global Study of Women’s Health consortium. Impact of endometriosis on quality of life and work productivity: A multicenter study across ten countries. Fertil. Steril. 2011, 96, 366–373.e8. [Google Scholar] [CrossRef] [Green Version]
- Valle, R.F.; Sciarra, J.J. Endometriosis: Treatment strategies. Ann. N. Y. Acad. Sci. 2003, 997, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Bulletti, C.; Coccia, M.E.; Battistoni, S.; Borini, A. Endometriosis and infertility. J. Assist. Reprod. Genet. 2010, 27, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Mira, T.A.; Buen, M.M.; Borges, M.G.; Yela, D.A.; Benetti-Pinto, C.L. Systematic review and meta-analysis of complementary treatments for women with symptomatic endometriosis. Int. J. Gynecol. Obstet. 2018, 143, 2–9. [Google Scholar] [CrossRef]
- Ambrose, K.R.; Golightly, Y.M. Physical exercise as non-pharmacological treatment of chronic pain: Why and when. Best Pract. Res. Clin. Rheumatol. 2015, 29, 120–130. [Google Scholar] [CrossRef] [Green Version]
- Gill, S.D.; McBurney, H.; Schulz, D.L. Land-based versus pool-based exercise for people awaiting joint replacement surgery of the hip or knee: Results of a randomized controlled trial. Arch. Phys. Med. Rehabil. 2009, 90, 388–394. [Google Scholar] [CrossRef]
- Awad, E.; Ahmed, H.A.H.; Yousef, A.; Abbas, R. Efficacy of exercise on pelvic pain and posture associated with endometriosis: Within subject design. J. Phys. Ther. Sci. 2017, 29, 2112–2115. [Google Scholar] [CrossRef] [Green Version]
- Kabani, Z.; Ramos-Nino, M.E.; Ramdass, P.V. Endometriosis and COVID-19: A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2022, 23, 12951. [Google Scholar] [CrossRef]
- Adamse, C.; Dekker-Van Weering, M.G.; van Etten-Jamaludin, F.S.; Stuiver, M.M. The effectiveness of exercise-based telemedicine on pain, physical activity and quality of life in the treatment of chronic pain: A systematic review. J. Telemed. Telecare 2018, 24, 511–526. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, M.; Horne, A.W.; Armour, M.; Missmer, S.A.; Roman, H.; Rombauts, L.; Hummelshoj, L.; Wattiez, A.; Condous, G.; Johnson, N.P. Endometriosis and the coronavirus (COVID-19) pandemic: Clinical advice and future considerations. Front. Reprod. Health 2020, 2, 5. [Google Scholar] [CrossRef] [PubMed]
- Wittkopf, P.G.; Lloyd, D.M.; Coe, O.; Yacoobali, S.; Billington, J. The effect of interactive virtual reality on pain perception: A systematic review of clinical studies. Disabil. Rehabil. 2020, 42, 3722–3733. [Google Scholar] [CrossRef] [PubMed]
- Merlot, B.; Dispersyn, G.; Husson, Z.; Chanavaz-Lacheray, I.; Dennis, T.; Greco-Vuilloud, J.; Fougère, M.; Potvin, S.; Cotty-Eslous, M.; Roman, H. Pain Reduction with an Immersive Digital Therapeutic Tool in Women Living with Endometriosis-Related Pelvic Pain: Randomized Controlled Trial. J. Med. Internet Res. 2022, 24, e39531. [Google Scholar] [CrossRef]
- Schröder, J.; Van Criekinge, T.; Embrechts, E.; Celis, X.; Van Schuppen, J.; Truijen, S.; Saeys, W. Combining the benefits of tele-rehabilitation and virtual reality-based balance training: A systematic review on feasibility and effectiveness. Disabil. Rehabil. Assist. Technol. 2019, 14, 2–11. [Google Scholar] [CrossRef] [PubMed]
- McGeary, D.D.; McGeary, C.A.; Gatchel, R.J.; Allison, S.; Hersh, A. Assessment of research quality of telehealth trials in pain management: A meta-analysis. Pain Pract. 2013, 13, 422–431. [Google Scholar] [CrossRef]
- Bourdel, N.; Alves, J.; Pickering, G.; Ramilo, I.; Roman, H.; Canis, M. Systematic review of endometriosis pain assessment: How to choose a scale? Hum. Reprod. Update 2015, 21, 136–152. [Google Scholar] [CrossRef]
- Chen, M.J.; Fan, X.; Moe, S.T. Criterion-related validity of the Borg ratings of perceived exertion scale in healthy individuals: A meta-analysis. J. Sport. Sci. 2002, 20, 873–899. [Google Scholar] [CrossRef]
- Spiegel, B.; Fuller, G.; Lopez, M.; Dupuy, T.; Noah, B.; Howard, A.; Albert, M.; Tashjian, V.; Lam, R.; Ahn, J. Virtual reality for management of pain in hospitalized patients: A randomized comparative effectiveness trial. PLoS ONE 2019, 14, e0219115. [Google Scholar] [CrossRef] [Green Version]
- Vacha-Haase, T.; Thompson, B. How to estimate and interpret various effect sizes. J. Couns. Psychol. 2004, 51, 473. [Google Scholar] [CrossRef] [Green Version]
- Jin, W.; Choo, A.; Gromala, D.; Shaw, C.; Squire, P. A virtual reality game for chronic pain management: A randomized, controlled clinical study. In Medicine Meets Virtual Reality 22; IOS Press: Amsterdam, The Netherlands, 2016; pp. 154–160. [Google Scholar]
- Bennell, K.L.; Lawford, B.J.; Keating, C.; Brown, C.; Kasza, J.; Mackenzie, D.; Metcalf, B.; Kimp, A.J.; Egerton, T.; Spiers, L. Comparing video-based, telehealth-delivered exercise and weight loss programs with online education on outcomes of knee osteoarthritis: A randomized trial. Ann. Intern. Med. 2022, 175, 198–209. [Google Scholar] [CrossRef] [PubMed]
- Galiano-Castillo, N.; Cantarero-Villanueva, I.; Fernández-Lao, C.; Ariza-García, A.; Díaz-Rodríguez, L.; Del-Moral-Ávila, R.; Arroyo-Morales, M. Telehealth system: A randomized controlled trial evaluating the impact of an internet-based exercise intervention on quality of life, pain, muscle strength, and fatigue in breast cancer survivors. Cancer 2016, 122, 3166–3174. [Google Scholar] [CrossRef] [PubMed]
- Melzack, R.; Wall, P.D. Pain Mechanisms: A New Theory: A gate control system modulates sensory input from the skin before it evokes pain perception and response. Science 1965, 150, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Melzack, R. From the gate to the neuromatrix. Pain 1999, 82, S121–S126. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.H. How does distraction work in the management of pain? Curr. Pain Headache Rep. 2005, 9, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Bantick, S.J.; Wise, R.G.; Ploghaus, A.; Clare, S.; Smith, S.M.; Tracey, I. Imaging how attention modulates pain in humans using functional MRI. Brain 2002, 125, 310–319. [Google Scholar] [CrossRef] [Green Version]
- Ghione, S. Hypertension-associated hypalgesia: Evidence in experimental animals and humans, pathophysiological mechanisms, and potential clinical consequences. Hypertension 1996, 28, 494–504. [Google Scholar] [CrossRef]
- Randich, A.; Maixner, W. Interactions between cardiovascular and pain regulatory systems. Neurosci. Biobehav. Rev. 1984, 8, 343–367. [Google Scholar] [CrossRef]
- Koltyn, K.F. Exercise-induced hypoalgesia and intensity of exercise. Sport. Med. 2002, 32, 477–487. [Google Scholar] [CrossRef]
- Jones, G.; Jenkinson, C.; Kennedy, S. The impact of endometriosis upon quality of life: A qualitative analysis. J. Psychosom. Obstet. Gynecol. 2004, 25, 123–133. [Google Scholar] [CrossRef]
- Jennett, P.A.; Hall, L.A.; Hailey, D.; Ohinmaa, A.; Anderson, C.; Thomas, R.; Young, B.; Lorenzetti, D.; Scott, R.E. The socio-economic impact of telehealth: A systematic review. J. Telemed. Telecare 2003, 9, 311–320. [Google Scholar] [CrossRef] [PubMed]

| Variables | Telehealth (n = 7) | VR (n = 8) | Control (n = 4) |
|---|---|---|---|
| Age (years) | 29 ± 7 | 27 ± 7 | 25 ± 4 |
| BMI (kg/m2) | 25 ± 4 | 23 ± 4 | 26 ± 2 |
| Height (cm) | 168 ± 10 | 169 ± 5 | 167 ± 6 |
| Weight (kg) | 70 ± 12 | 66 ± 12 | 72 ± 6 |
| Time since laparoscopy | |||
| More than 12 months (no. of participants) | 3 | 4 | 3 |
| Medications | |||
| NSAIDS, (no. of participants) | 2 | 2 | 2 |
| Progestins (no. of participants) | 4 | 5 | 4 |
| Androgens (no. of participants) | 1 | 1 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lutfi, M.; Dalleck, L.C.; Drummond, C.; Drummond, M.; Paparella, L.; Keith, C.E.; Kirton, M.; Falconer, L.; Gebremichael, L.; Phelan, C.; et al. A Single Session of a Digital Health Tool-Delivered Exercise Intervention May Provide Immediate Relief from Pelvic Pain in Women with Endometriosis: A Pilot Randomized Controlled Study. Int. J. Environ. Res. Public Health 2023, 20, 1665. https://doi.org/10.3390/ijerph20031665
Lutfi M, Dalleck LC, Drummond C, Drummond M, Paparella L, Keith CE, Kirton M, Falconer L, Gebremichael L, Phelan C, et al. A Single Session of a Digital Health Tool-Delivered Exercise Intervention May Provide Immediate Relief from Pelvic Pain in Women with Endometriosis: A Pilot Randomized Controlled Study. International Journal of Environmental Research and Public Health. 2023; 20(3):1665. https://doi.org/10.3390/ijerph20031665
Chicago/Turabian StyleLutfi, Muhammad, Lance C. Dalleck, Claire Drummond, Murray Drummond, Liana Paparella, Caitlin E. Keith, Michael Kirton, Laura Falconer, Lemlem Gebremichael, Caroline Phelan, and et al. 2023. "A Single Session of a Digital Health Tool-Delivered Exercise Intervention May Provide Immediate Relief from Pelvic Pain in Women with Endometriosis: A Pilot Randomized Controlled Study" International Journal of Environmental Research and Public Health 20, no. 3: 1665. https://doi.org/10.3390/ijerph20031665





