Not Getting Vaccinated? It Is a Matter of Problem-Solving Abilities and Socio-Cognitive Polarization
Abstract
1. Introduction
2. Materials and Methods
2.1. Procedure
2.2. Measures
2.2.1. Demographics
2.2.2. Vaccine Acceptance
2.2.3. Socio-Cognitive Polarization (SCP)
2.2.4. Creative Problem Solving
2.3. Participants
2.4. Statistical Plan
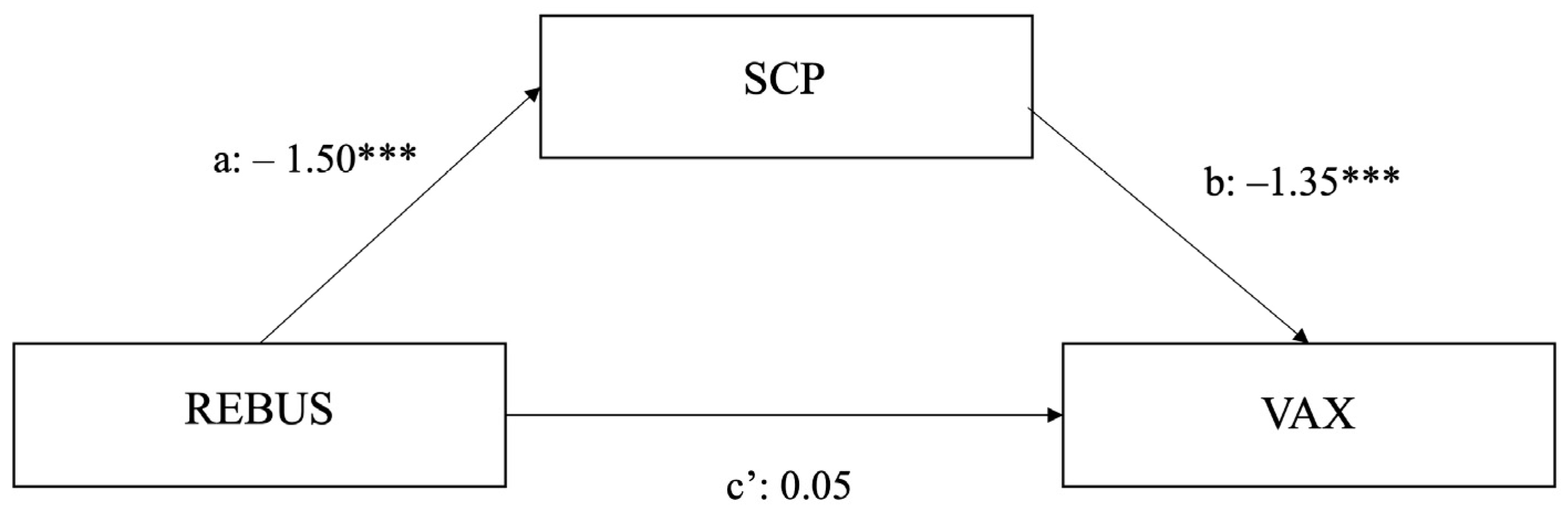
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Beltekian, D.; Dattani, S.; et al. Coronavirus Pandemic (COVID-19). Our World in Data. 2020–2022. Available online: https://ourworldindata.org/covid-vaccinations?country=JPN~USA (accessed on 13 December 2022).
- Thomas, K.; Weiland, N.; LaFraniere, S.F.D.A. Advisory Panel Gives Green Light to Pfizer Vaccine. The New York Times. 10 December 2020.
- Centers for Disease Control and Prevention. Vaccines for COVID-19. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/index.html (accessed on 13 December 2022).
- Benveniste, A. New York City Will Require Vaccines for Entry to Restaurants and Gyms. 3 August 2021. Available online: https://web.archive.org/web/20210803163022/https://www.cnn.com/2021/08/03/business/new-york-city-vaccine-requirements/index.html (accessed on 13 August 2021).
- Iannello, P.; Colautti, L.; Magenes, S.; Antonietti, A.; Cancer, A. Black-and-white Thinking and Conspiracy Beliefs Prevent Parents from Vaccinating Their Children against COVID-19. Appl. Cogn. Psychol. 2022, 36, 1177–1187. [Google Scholar] [CrossRef] [PubMed]
- Shi, R.; Qi, W.; Ding, Y.; Liu, C.; Shen, W. Under What Circumstances Is Helping an Impulse? Emergency and Prosocial Traits Affect Intuitive Prosocial Behavior. Personal. Individ. Differ. 2020, 159, 109828. [Google Scholar] [CrossRef]
- De Dreu, C.K.W.; Baas, M.; Nijstad, B.A. Hedonic Tone and Activation Level in the Mood-Creativity Link: Toward a Dual Pathway to Creativity Model. J. Personal. Soc. Psychol. 2008, 94, 739–756. [Google Scholar] [CrossRef] [PubMed]
- Perry-Smith, J.E.; Mannucci, P.V. From Creativity to Innovation: The Social Network Drivers of the Four Phases of the Idea Journey. AMR 2017, 42, 53–79. [Google Scholar] [CrossRef]
- Salvi, C.; Cristofori, I.; Grafman, J.; Beeman, M. Rapid Communication: The Politics of Insight. Q. J. Exp. Psychol. 2016, 69, 1064–1072. [Google Scholar] [CrossRef]
- Salvi, C.; Iannello, P.; Cancer, A.; McClay, M.; Rago, S.; Dunsmoor, J.E.; Antonietti, A. Going Viral: How Fear, Socio-Cognitive Polarization and Problem-Solving Influence Fake News Detection and Proliferation during COVID-19 Pandemic. Front. Commun. 2021, 5, 562588. [Google Scholar] [CrossRef]
- Zmigrod, L. The Role of Cognitive Rigidity in Political Ideologies: Theory, Evidence, and Future Directions. Curr. Opin. Behav. Sci. 2020, 34, 34–39. [Google Scholar] [CrossRef]
- Salvi, C.; Barr, N.; Dunsmoor, J.E.; Grafman, J. Insight Problem Solving Ability Predicts Reduced Susceptibility to Fake News, Bullshit, and Overclaiming. Think. Reason. 2022, 1–25. [Google Scholar] [CrossRef]
- Salvi, C.; Iannello, P.; Cancer, A.; Cooper, S.E.; McClay, M.; Antonietti, A.; Dunsmoor, J.E. Does Social Rigidity Predict Cognitive Rigidity? Profiles of Socio-Cognitive Polarization. 2022. [Google Scholar] [CrossRef]
- Stanovich, K.E.; West, R.F. Discrepancies Between Normative and Descriptive Models of Decision Making and the Understanding/Acceptance Principle. Cogn. Psychol. 1999, 38, 349–385. [Google Scholar] [CrossRef]
- MacDonald, N.E. SAGE Working Group on Vaccine Hesitancy. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Romer, D.; Jamieson, K.H. Conspiracy Theories as Barriers to Controlling the Spread of COVID-19 in the U.S. Soc. Sci. Med. 2020, 263, 113356. [Google Scholar] [CrossRef]
- Dodd, R.H.; Cvejic, E.; Bonner, C.; Pickles, K.; McCaffery, K.J.; Ayre, J.; Batcup, C.; Copp, T.; Cornell, S.; Dakin, T.; et al. Willingness to Vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2021, 21, 318–319. [Google Scholar] [CrossRef]
- Peretti-Watel, P.; Alleaume, C.; Léger, D.; Beck, F.; Verger, P. Anxiety, Depression and Sleep Problems: A Second Wave of COVID-19. Gen. Psychiatry 2020, 33, e100299. [Google Scholar] [CrossRef]
- Holeva, V.; Parlapani, E.; Nikopoulou, V.A.; Nouskas, I.; Diakogiannis, I. COVID-19 Vaccine Hesitancy in a Sample of Greek Adults. Psychol. Health Med. 2022, 27, 113–119. [Google Scholar] [CrossRef]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine Hesitancy: The next Challenge in the Fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
- Palamenghi, L.; Barello, S.; Boccia, S.; Graffigna, G. Mistrust in Biomedical Research and Vaccine Hesitancy: The Forefront Challenge in the Battle against COVID-19 in Italy. Eur. J. Epidemiol. 2020, 35, 785–788. [Google Scholar] [CrossRef]
- Doherty, I.A.; Pilkington, W.; Brown, L.; Billings, V.; Hoffler, U.; Paulin, L.; Kimbro, K.S.; Baker, B.; Zhang, T.; Locklear, T.; et al. COVID-19 Vaccine Hesitancy in Underserved Communities of North Carolina. PLoS ONE 2021, 16, e0248542. [Google Scholar] [CrossRef]
- Baumgaertner, B.; Carlisle, J.E.; Justwan, F. The Influence of Political Ideology and Trust on Willingness to Vaccinate. PLoS ONE 2018, 13, e0191728. [Google Scholar] [CrossRef]
- Bilewicz, M.; Soral, W. The Politics of Vaccine Hesitancy: An Ideological Dual-Process Approach. Soc. Psychol. Personal. Sci. 2022, 13, 1080–1089. [Google Scholar] [CrossRef]
- Hagger, M.S.; Hamilton, K. Predicting COVID-19 Booster Vaccine Intentions. Appl. Psychol. Health Well-Being 2022, 14, 819–841. [Google Scholar] [CrossRef] [PubMed]
- Litman, L.; Robinson, J.; Abberbock, T. TurkPrime.Com: A Versatile Crowdsourcing Data Acquisition Platform for the Behavioral Sciences. Behav. Res. 2017, 49, 433–442. [Google Scholar] [CrossRef] [PubMed]
- Robinson, J.P.; Shaver, P.R.; Wrightsman, L.S. Measures of Political Attitudes; Academic Press: San Diego, CA, USA, 1999; ISBN 978-0-12-590242-7. [Google Scholar]
- Lauriola, M.; Foschi, R.; Mosca, O.; Weller, J. Attitude Toward Ambiguity: Empirically Robust Factors in Self-Report Personality Scales. Assessment 2016, 23, 353–373. [Google Scholar] [CrossRef] [PubMed]
- van der Veer, K.; Ommundsen, R.; Yakushko, O.; Higler, L.; Woelders, S.; Hagen, K.A. Psychometrically and Qualitatively Validating a Cross-National Cumulative Measure of Fear-Based Xenophobia. Qual. Quant. 2013, 47, 1429–1444. [Google Scholar] [CrossRef]
- Salvi, C.; Costantini, G.; Bricolo, E.; Perugini, M.; Beeman, M. Validation of Italian Rebus Puzzles and Compound Remote Associate Problems. Behav. Res. 2016, 48, 664–685. [Google Scholar] [CrossRef]
- Salvi, C.; Bricolo, E.; Kounios, J.; Bowden, E.; Beeman, M. Insight Solutions Are Correct More Often than Analytic Solutions. Think. Reason. 2016, 22, 443–460. [Google Scholar] [CrossRef]
- Salvi, C.; Costantini, G.; Pace, A.; Palmiero, M. Validation of the Italian Remote Associate Test. J. Creat. Behav. 2020, 54, 62–74. [Google Scholar] [CrossRef]
- MacGregor, J.N.; Cunningham, J.B. Rebus Puzzles as Insight Problems. Behav. Res. 2008, 40, 263–268. [Google Scholar] [CrossRef]
- Cancer, A.; Iannello, P.; Salvi, C.; Antonietti, A. Executive Functioning and Divergent Thinking Predict Creative Problem-Solving in Young Adults and Elderlies. Psychol. Res. 2022, 1–9. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 3rd ed.; Methodology in the Social Sciences; The Guilford Press: New York, NY, USA, 2022; ISBN 978-1-4625-4903-0. [Google Scholar]
- Adams, K.; Rhoads, J.P.; Surie, D.; Gaglani, M.; Ginde, A.A.; McNeal, T.; Talbot, H.K.; Casey, J.D.; Zepeski, A.; Shapiro, N.I.; et al. Vaccine Effectiveness of Primary Series and Booster Doses against COVID-19 Associated Hospital Admissions in the United States: Living Test Negative Design Study. BMJ 2022, 379, e072065. [Google Scholar] [CrossRef]
- Boehner, C.W.; Howe, S.R.; Bernstein, D.I.; Rosenthal, S.L. Viral Sexually Transmitted Disease Vaccine Acceptability among College Students. Sex. Transm. Dis. 2003, 30, 774–778. [Google Scholar] [CrossRef]
- Gottschling, J.; Krieger, F.; Greiff, S. The Fight against Infectious Diseases: The Essential Role of Higher-Order Thinking and Problem-Solving. J. Intell. 2022, 10, 14. [Google Scholar] [CrossRef]
- Burki, T. COVID-19 Vaccine Mandates in Europe. Lancet Infect. Dis. 2022, 22, 27–28. [Google Scholar] [CrossRef]
- Banker, C.C.; Leary, M.R. Hypo-Egoic Nonentitlement as a Feature of Humility. Personal. Soc. Psychol. Bull. 2020, 46, 738–753. [Google Scholar] [CrossRef]
- Huynh, H.P.; Senger, A.R. A Little Shot of Humility: Intellectual Humility Predicts Vaccination Attitudes and Intention to Vaccinate against COVID-19. J. Appl. Soc. Psychol. 2021, 51, 449–460. [Google Scholar] [CrossRef]
- Zmigrod, L.; Rentfrow, P.J.; Robbins, T.W. Cognitive Underpinnings of Nationalistic Ideology in the Context of Brexit. Proc. Natl. Acad. Sci. USA 2018, 115, E4532–E4540. [Google Scholar] [CrossRef]
- Zmigrod, L.; Rentfrow, P.J.; Robbins, T.W. Cognitive Inflexibility Predicts Extremist Attitudes. Front. Psychol. 2019, 10, 989. [Google Scholar] [CrossRef]
- McCoy, C.A. The Social Characteristics of Americans Opposed to Vaccination: Beliefs about Vaccine Safety versus Views of U.S. Vaccination Policy. Crit. Public Health 2020, 30, 4–15. [Google Scholar] [CrossRef]
- Sturm, T.; Albrecht, T. Constituent COVID-19 Apocalypses: Contagious Conspiracism, 5G, and Viral Vaccinations. Anthropol. Med. 2021, 28, 122–139. [Google Scholar] [CrossRef]
- Bertin, P.; Nera, K.; Delouvée, S. Conspiracy Beliefs, Rejection of Vaccination, and Support for Hydroxychloroquine: A Conceptual Replication-Extension in the COVID-19 Pandemic Context. Front. Psychol. 2020, 11, 565128. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.C.; Reiss, D.R. Digging the Rabbit Hole, COVID-19 Edition: Anti-Vaccine Themes and the Discourse around COVID-19. Microbes Infect. 2020, 22, 608–610. [Google Scholar] [CrossRef]
- Burki, T. Outbreak of Coronavirus Disease 2019. Lancet Infect. Dis. 2020, 20, 292–293. [Google Scholar] [CrossRef] [PubMed]
- Puri, N.; Coomes, E.A.; Haghbayan, H.; Gunaratne, K. Social Media and Vaccine Hesitancy: New Updates for the Era of COVID-19 and Globalized Infectious Diseases. Hum. Vaccines Immunother. 2020, 16, 2586–2593. [Google Scholar] [CrossRef] [PubMed]
| n (%) | |
|---|---|
| Age1 | 34.32 (7.63) |
| Gender | |
| Male | 103 (37.2) |
| Female | 168 (60.6) |
| Other | 6 (2.2) |
| Marital status | |
| Married | 107 (38.6) |
| Partnered | 81 (29.2) |
| Single | 89 (32.1) |
| Highest educational level | |
| Middle School | 1 (0.4) |
| High School | 100 (36.1) |
| Bachelor’s degree | 105 (37.9) |
| Graduate/Master | 28 (10.1) |
| MD/PhD | 38 (13.7) |
| Other 2 | 5 (1.8) |
| Vaccine acceptance | |
| Provax | 197 (71.1) |
| Antivax | 80 (28.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cancer, A.; Salvi, C.; Antonietti, A.; Iannello, P. Not Getting Vaccinated? It Is a Matter of Problem-Solving Abilities and Socio-Cognitive Polarization. Int. J. Environ. Res. Public Health 2023, 20, 1721. https://doi.org/10.3390/ijerph20031721
Cancer A, Salvi C, Antonietti A, Iannello P. Not Getting Vaccinated? It Is a Matter of Problem-Solving Abilities and Socio-Cognitive Polarization. International Journal of Environmental Research and Public Health. 2023; 20(3):1721. https://doi.org/10.3390/ijerph20031721
Chicago/Turabian StyleCancer, Alice, Carola Salvi, Alessandro Antonietti, and Paola Iannello. 2023. "Not Getting Vaccinated? It Is a Matter of Problem-Solving Abilities and Socio-Cognitive Polarization" International Journal of Environmental Research and Public Health 20, no. 3: 1721. https://doi.org/10.3390/ijerph20031721
APA StyleCancer, A., Salvi, C., Antonietti, A., & Iannello, P. (2023). Not Getting Vaccinated? It Is a Matter of Problem-Solving Abilities and Socio-Cognitive Polarization. International Journal of Environmental Research and Public Health, 20(3), 1721. https://doi.org/10.3390/ijerph20031721








