Impacts of Wildfire Smoke and Air Pollution on a Pediatric Population with Asthma: A Population-Based Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Study Population and Associated Data
2.2.1. Population and Data Linkage
2.2.2. Clinical and Pharmaceutical Data
2.3. Air Pollution Data
2.4. Statistical Analysis and Modeling
2.5. Ethics Statement
3. Results
3.1. Population Characteristics
3.2. Air Pollution Characteristics
3.3. Relationship between Air Pollution, Wildfire Smoke and Asthma Exacerbation
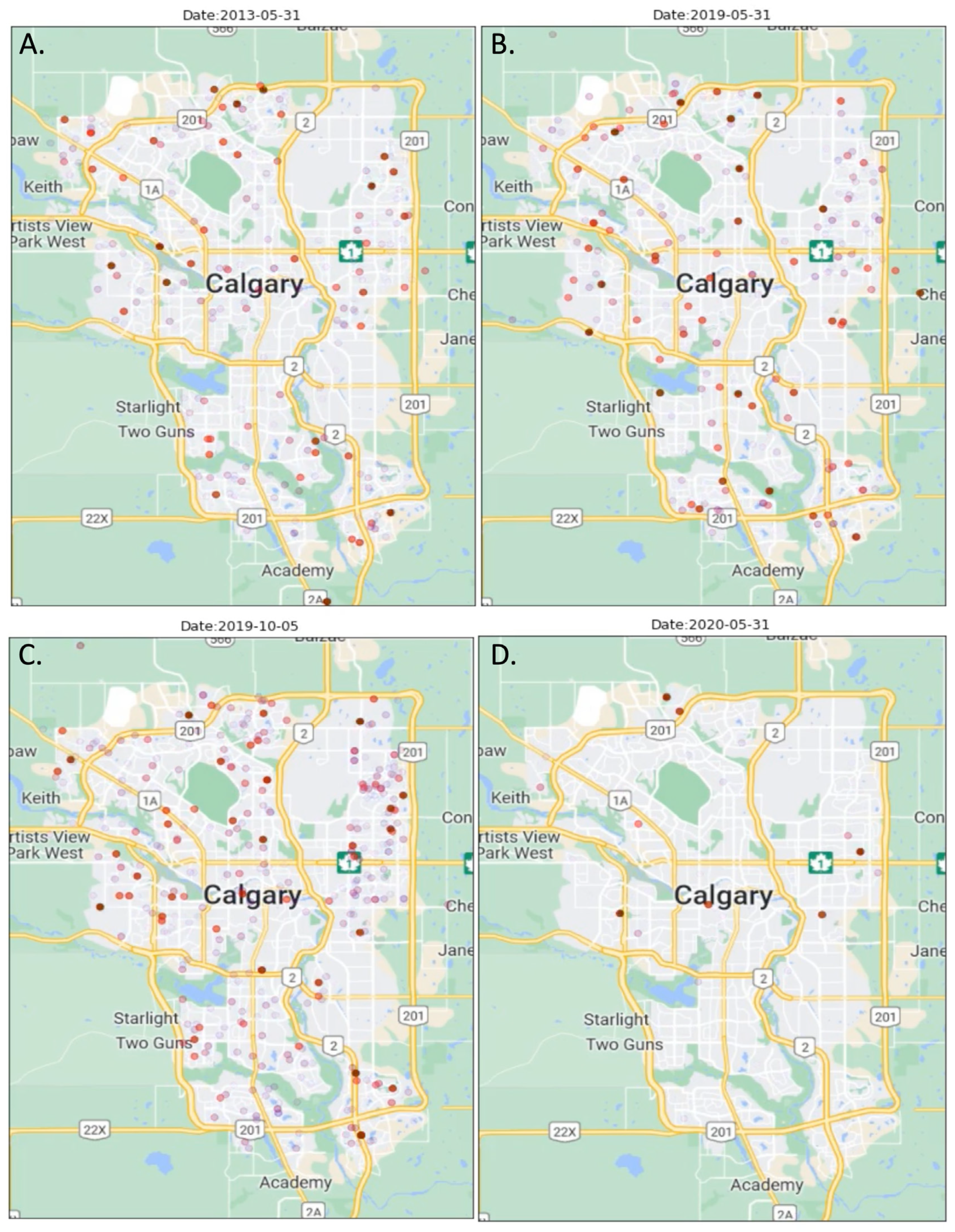
3.4. COVID-19 Public Health Precautions and Asthma Exacerbations

4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ismaila, A.S.; Sayani, A.P.; Marin, M.; Su, Z. Clinical, economic, and humanistic burden of asthma in Canada: A systematic review. BMC Pulm. Med. 2013, 13, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sears, M.R. Trends in the Prevalence of Asthma. Chest 2014, 145, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Lu, F.; Xu, D.; Cheng, Y.; Dong, S.; Guo, C.; Jiang, X.; Zheng, X. Systematic review and meta-analysis of the adverse health effects of ambient PM2.5 and PM10 pollution in the Chinese population. Environ. Res. 2015, 136, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Guarnieri, M.; Balmes, J.R. Outdoor air pollution and asthma. Lancet 2014, 383, 1581–1592. [Google Scholar] [CrossRef] [Green Version]
- Watts, N.; Amann, M.; Ayeb-Karlsson, S.; Belesova, K.; Bouley, T.; Boykoff, M.; Byass, P.; Cai, W.; Campbell-Lendrum, D.; Chambers, J.; et al. The Lancet Countdown on health and climate change: From 25 years of inaction to a global transformation for public health. Lancet 2018, 391, 581–630. [Google Scholar] [CrossRef]
- Pechony, O.; Shindell, D.T. Driving forces of global wildfires over the past millennium and the forthcoming century. Proc. Natl. Acad. Sci. USA 2010, 107, 19167–19170. [Google Scholar] [CrossRef] [Green Version]
- Dupuy, J.-L.; Fargeon, H.; Martin-StPaul, N.; Pimont, F.; Ruffault, J.; Guijarro, M.; Hernando, C.; Madrigal, J.; Fernandes, P. Climate change impact on future wildfire danger and activity in southern Europe: A review. Ann. For. Sci. 2020, 77, 35. [Google Scholar] [CrossRef]
- Wang, X.; Parisien, M.-A.; Taylor, S.W.; Candau, J.-N.; Stralberg, D.; Marshall, G.A.; Little, J.M.; Flannigan, M.D. Projected changes in daily fire spread across Canada over the next century. Environ. Res. Lett. 2017, 12, 025005. [Google Scholar] [CrossRef]
- Westerling, A.L.; Hidalgo, H.G.; Cayan, D.R.; Swetnam, T.W. Warming and Earlier Spring Increase Western U.S. Forest Wildfire Activity. Science 2006, 313, 940–943. [Google Scholar] [CrossRef] [Green Version]
- Abatzoglou, J.T.; Kolden, C.A. Climate Change in Western US Deserts: Potential for Increased Wildfire and Invasive Annual Grasses. Rangel. Ecol. Manag. 2011, 64, 471–478. [Google Scholar] [CrossRef]
- Liu, J.C.; Peng, R.D. The impact of wildfire smoke on compositions of fine particulate matter by ecoregion in the Western US. J. Expo. Sci. Environ. Epidemiol. 2018, 29, 765–776. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Lin, M.; Horowitz, L.W. Summer PM 2.5 Pollution Extremes Caused by Wildfires Over the Western United States During 2017–2018. Geophys. Res. Lett. 2020, 47, e2020GL089429. [Google Scholar] [CrossRef]
- Shi, H.; Jiang, Z.; Zhao, B.; Li, Z.; Chen, Y.; Gu, Y.; Jiang, J.H.; Lee, M.; Liou, K.; Neu, J.L.; et al. Modeling Study of the Air Quality Impact of Record-Breaking Southern California Wildfires in December 2017. J. Geophys. Res. Atmos. 2019, 124, 6554–6570. [Google Scholar] [CrossRef] [PubMed]
- Künzli, N.; Avol, E.; Wu, J.; Gauderman, W.J.; Rappaport, E.; Millstein, J.; Bennion, J.; McConnell, R.; Gilliland, F.D.; Berhane, K.; et al. Health Effects of the 2003 Southern California Wildfires on Children. Am. J. Respir. Crit. Care Med. 2006, 174, 1221–1228. [Google Scholar] [CrossRef] [Green Version]
- Vicedo-Cabrera, A.M.; Esplugues, A.; Iñíguez, C.; Estarlich, M.; Ballester, F. Health effects of the 2012 Valencia (Spain) wildfires on children in a cohort study. Environ. Geochem. Health 2015, 38, 703–712. [Google Scholar] [CrossRef]
- Delfino, R.J.; Brummel, S.; Wu, J.; Stern, H.; Ostro, B.; Lipsett, M.; Winer, A.; Street, D.H.; Zhang, L.; Tjoa, T.; et al. The relationship of respiratory and cardiovascular hospital admissions to the southern California wildfires of 2003. Occup. Environ. Med. 2009, 66, 189–197. [Google Scholar] [CrossRef] [Green Version]
- Henry, S.; Ospina, M.B.; Dennett, L.; Hicks, A. Assessing the Risk of Respiratory-Related Healthcare Visits Associated with Wildfire Smoke Exposure in Children 0–18 Years Old: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 8799. [Google Scholar] [CrossRef]
- Mirabelli, M.C.; Künzli, N.; Avol, E.; Gilliland, F.D.; Gauderman, W.J.; McConnell, R.; Peters, J.M. Respiratory Symptoms Following Wildfire Smoke Exposure: Airway Size as a Susceptibility Factor. Epidemiology 2009, 20, 451–459. [Google Scholar] [CrossRef] [Green Version]
- Johnston, F.H.; Webby, R.J.; Pilotto, L.S.; Bailie, R.S.; Parry, D.L.; Halpin, S.J. Vegetation fires, particulate air pollution and asthma: A panel study in the Australian monsoon tropics. Int. J. Environ. Health Res. 2006, 16, 391–404. [Google Scholar] [CrossRef]
- Hanigan, I.C.; Johnston, F.H.; Morgan, G.G. Vegetation fire smoke, indigenous status and cardio-respiratory hospital admissions in Darwin, Australia, 1996–2005: A time-series study. Environ. Health 2008, 7, 42. [Google Scholar] [CrossRef]
- Leibel, S.; Nguyen, M.; Brick, W.; Parker, J.; Ilango, S.; Aguilera, R.; Gershunov, A.; Benmarhnia, T. Increase in Pediatric Respiratory Visits Associated with Santa Ana Wind–Driven Wildfire Smoke and PM2.5 Levels in San Diego County. Ann. Am. Thorac. Soc. 2020, 17, 313–320. [Google Scholar] [CrossRef] [PubMed]
- To, T.; Dell, S.; Dick, P.T.; Cicutto, L.; Harris, J.K.; MacLusky, I.B.; Tassoudji, M. Case verification of children with asthma in Ontario. Pediatr. Allergy Immunol. 2005, 17, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Asthma Incidence among Alberta Children—Asthma Incidence among Alberta Children—Open Government. Available online: https://open.alberta.ca/dataset/asthma-incidence-among-alberta-children/resource/c1d7f0ba-28fc-4615-9df7-8bf187107e23 (accessed on 29 November 2022).
- Wentworth, G.R.; Aklilu, Y.-A.; Landis, M.S.; Hsu, Y.-M. Impacts of a large boreal wildfire on ground level atmospheric concentrations of PAHs, VOCs and ozone. Atmos. Environ. 2018, 178, 19–30. [Google Scholar] [CrossRef] [PubMed]
- Holm, S.M.; Miller, M.D.; Balmes, J.R. Health effects of wildfire smoke in children and public health tools: A narrative review. J. Expo. Sci. Environ. Epidemiol. 2021, 31, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Alberta Regional Dashboard—Calgary—Population. Available online: https://regionaldashboard.alberta.ca/region/calgary/population/#/?from=2001&to=2021 (accessed on 6 December 2022).
- Statistics Canaada Population 2016 Calgary. Available online: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page.cfm?Lang=E&Geo1=CMACA&Code1=825&Geo2=PR&Code2=48&Data=Count&SearchText=calgary&SearchType=Begins&SearchPR=01&B1=All&TABID=1 (accessed on 6 December 2022).
- Alberta Health Services Data Access. Available online: https://www.albertahealthservices.ca/research/Page16074.aspx (accessed on 6 December 2022).
- ICD-9/CCP and ICD-9-CM|CIHI. Available online: https://www.cihi.ca/en/icd-9ccp-and-icd-9-cm (accessed on 6 December 2022).
- Information (CIHI), C.I. for H. Canadian Coding Standards for ICD-10-CA and CCI. Available online: https://secure.cihi.ca/estore/productSeries.htm?pc=PCC189 (accessed on 6 December 2022).
- Canadian Triage and Acuity Scale. Available online: https://ctas-phctas.ca/ (accessed on 28 November 2022).
- Access Air Quality and Deposition Data|Alberta.ca. Available online: https://www.alberta.ca/access-air-quality-and-deposition-data.aspx (accessed on 28 November 2022).
- Stieb, D.M.; Judek, S.; Van Donkelaar, A.; Martin, R.V.; Brand, K.; Shin, H.H.; Burnett, R.T.; Smith-Doiron, M.H. Estimated public health impacts of changes in concentrations of fine particle air pollution in Canada, 2000 to 2011. Can. J. Public Health 2015, 106, e362–e368. [Google Scholar] [CrossRef]
- NASA Wordview Service Home Page. Available online: https://worldview.earthdata.nasa.gov (accessed on 28 November 2021).
- Henderson, S.B.; Brauer, M.; Macnab, Y.C.; Kennedy, S.M. Three Measures of Forest Fire Smoke Exposure and Their Associations with Respiratory and Cardiovascular Health Outcomes in a Population-Based Cohort. Environ. Health Perspect. 2011, 119, 1266–1271. [Google Scholar] [CrossRef]
- Zhang, R. Map of Calgary Video with Pediatric Asthma Cases Marked, 2010–2021. 2022. Available online: https://doc-0s-50-docs.googleusercontent.com/docs/securesc/3gbe91disrkilhquf5uo1vl3f3n0k62h/02su1eut9uiie9k33oa6oa7g0deidgps/1669242750000/10880086360861761895/12751004392703094166/1vJcUu925ZTDeNqR9bXqHGLOV8cy5rt53?e=down-load&ax=AEKYgyRoU-kH6fVz7IWmAs9-E4rYh_VNUegGmjP8D2nNQ-V2apm-jAFKdTRCBsQE8kuxvLU6RibdkB-jknJsLcwD_iTh9H2z7DirMbQ9scnM3q9FKirjulxzdlGtuyl-X99qnELyF8V6xuv_8JxfvYRq0-b_g1h3pOFul0Pgvq_e6ziN9Vna_ThxcUqxtCd789xYUH70SBF4aJGZiVZt6rmyfahSKO7a2cdM0amecYAkmOO8ShttTME2EjbIoOSCFDo527rZxgq2rRfO6Q_Sbos2hsyvFuD5TFRnAkAhelC7TOPJkgRhAeaPIVHIY7fO_POJlIwjLXJtICb72Hg93JFZjNvjVg3kvQJDhQEjsP3tgqgGqbAxrCqXKSoRK5gntG7YaiWob_oAncW2Vx3U6Towy_1GpRNnLSHPU--4Thae-Zk75RdOl_-O3ujNlLReFklHU_tKNRTqPDGwYMjFcz2aqzeSWFzO_SafZ_lf-zLvKyREhsqNKv5gqHFlZlBenKoYuMuMoAl42K4NCyB6F_s4gMw6e3xDuUbi0XrZGEWO3Hl2eVqqCv1pzmq06QOpDSK_UD_X3FP3HrwfM8bUDZPMxM5p6zMfHAtAWedg_ziV8fn2N0zkjGqhhkICjSZ5Gd56k0-ajYlfQ4vBVjKxSIYthgqlM03iYELWeyq-7BbKTYeEASdPYXadxLCd10y0myTaLzvJySprcuKYQL8o6oAtbrmTH5eFbVLzB8-v_kFmvSD87RzfqMfxMWiP-CbNOtysBGh-CQSEQiH775Y0_45y07LeiXGeMZqRO4XvPAosw2wwWTqlFftRLJxr8jrYFjwclbCIrC7OSSNaG5T3_LoZJ1SiS1Kp69bNcTp8NdhrnJkEf_N5ObkGZXWAHVCL7qw8Gd6IGgKJbs-QI6gKTT3_6RSexbhCBRWfe-wKVl0zOZV5bArSc6Vi0UV3ovkS3xFE3Bw&uuid=8dba3997-3ad8-445b-b3ff-35d618cc65ce&authuser=0 (accessed on 23 November 2022).
- Pandas Development. Pandas-Dev/Pandas: Pandas. 2022. Available online: https://zenodo.org/record/7344967#.Y8kcbHbMJPY (accessed on 23 November 2022).
- Hunter, J.D. Matplotlib: A 2D graphics environment. Comput. Sci. Eng. 2007, 9, 90–95. [Google Scholar] [CrossRef]
- Harris, C.R.; Millman, K.J.; van der Walt, S.J.; Gommers, R.; Virtanen, P.; Cournapeau, D.; Wieser, E.; Taylor, J.; Berg, S.; Smith, N.J.; et al. Array programming with NumPy. Nature 2020, 585, 357–362. [Google Scholar] [CrossRef]
- Kluyver, T.; Ragan-Kelley, B.; Pérez, F.; Granger, B.E.; Bussonnier, M.; Frederic, J.; Kelley, K.; Hamrick, J.; Grout, J.; Corlay, S.; et al. Jupyter Notebooks—A publishing format for reproducible computational workflows. In Positioning and Power in Academic Publishing: Players, Agents and Agendas; IOS Press: Amsterdam, The Netherlands, 2016; pp. 87–90. [Google Scholar] [CrossRef]
- McKinney, W. Data structures for statistical computing in python. In Proceedings of the 9th Python in Science Conference, Austin, TX, USA, 28 June–3 July 2010; Volume 445, pp. 51–56. [Google Scholar]
- Yang, C.L.; Hicks, E.A.; Mitchell, P.; Reisman, J.; Podgers, D.; Hayward, K.M.; Waite, M.; Ramsey, C.D. 2021 Canadian Thoracic Society Guideline—A focused update on the management of very mild and mild asthma. Can. J. Respir. Crit. Care, Sleep Med. 2021, 5, 205–245. [Google Scholar] [CrossRef]
- Wikipedia. Timeline of the COVID-19 Pandemic in Alberta. 2022. Available online: https://en.wikipedia.org/wiki/Timeline_of_the_COVID-19_pandemic_in_Alberta (accessed on 1 December 2022).
- Larsen, K.; Zhu, J.; Feldman, L.Y.; Simatovic, J.; Dell, S.; Gershon, A.S.; To, T. The Annual September Peak in Asthma Exacerbation Rates. Still a Reality? Ann. Am. Thorac. Soc. 2016, 13, 231–239. [Google Scholar] [CrossRef]
- Bari, A.; Kindzierski, W.B. Characterization of air quality and sources of fine particulate matter (PM2.5) in the City of Calgary, Canada. Atmos. Pollut. Res. 2018, 9, 534–543. [Google Scholar] [CrossRef]
- Air Quality. Available online: https://www.calgary.ca/environment/air-quality.html (accessed on 28 November 2022).
- Bertazzon, S.; Calder-Bellamy, C.; Shahid, R.; Couloigner, I.; Wong, R. A Preliminary Spatial Analysis of the Association of Asthma and Traffic-Related Air Pollution in the Metropolitan Area of Calgary, Canada. Atmosphere 2020, 11, 1066. [Google Scholar] [CrossRef]
- Mahsin, M.D.; Cabaj, J.; Saini, V. Respiratory and cardiovascular condition-related physician visits associated with wildfire smoke exposure in Calgary, Canada, in 2015: A population-based study. Leuk. Res. 2021, 51, 166–178. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, W.J.; Patel, S.J.; Margolis, R.H.; Fox, E.R.; Shelef, D.Q.; Kachroo, N.; Pillai, D.; Teach, S.J. Pediatric asthma exacerbations during the COVID-19 pandemic: Absence of the typical fall seasonal spike in Washington, DC. J. Allergy Clin. Immunol. Pr. 2021, 9, 2073–2076. [Google Scholar] [CrossRef] [PubMed]
- Ford, A.; Little, C.; Bronconnier, C.; Courtney, K.; Olson, V.; Van De Wetering, S.; Noseworthy, M.; Dueck, B.; Humphries, T.; Desrosiers, D. The Community Pediatric Asthma Service-Together We’re Better: Asthma care in the Calgary zone. Can. J. Respir. Ther. 2018, 54, 77–82. [Google Scholar] [CrossRef]
| Air Quality Management Level | ||||
|---|---|---|---|---|
| Green | Yellow | Orange | Red | |
| PM2.5 (µg/m3) | ≤10 | 11–19 | 20–27 | >27 |
| Characteristic | Number |
|---|---|
| Cohort, n total | 57,375 |
| Sex | |
| Male, n (%) | 33,942 (59.2) |
| Female, n (%) | 23,433 (40.8) |
| Age (years) at asthma diagnosis, mean (95% CI) | 7.31 (7.27–7.36) |
| ED visits for asthma | |
| Total number of ED visits, n | 24,877 |
| Any—yes, n (%) | 14,120 (24.6) |
| Any—no, n (%) | 43,255 (75.4) |
| ED visits per patient, mean (95% CI) | 0.43 (0.42–0.44) |
| CTAS score per ED visit, mean (95% CI) | 2.67 (2.66–2.68) |
| Hospitalizations for asthma | |
| Total number of hospitalizations, n | 2624 |
| Any—yes, n (%) | 2106 (3.7) |
| Any—no, n (%) | 55,269 (96.3) |
| Number of hospitalizations for asthma per patient, mean (95% CI) | 0.05 (0.04–0.05) |
| PICU admissions | |
| Total number of PICU admissions, n | 566 |
| Any—yes, n (%) | 482 (0.8) |
| Any—no, n (%) | 56,893 (99.2) |
| Number of PICU admissions for asthma per patient, mean (95% CI) | 0.01 (0.01–0.01) |
| Medications in the first year after asthma diagnosis | |
| Short-acting beta-agonists, n (%) | 26,344 (45.9) |
| Inhaled corticosteroids *, n (%) | 18,632 (32.5) |
| Leukotriene receptor antagonists, n (%) | 2748 (4.8) |
| Oral corticosteroids, n (%) | 3687 (6.4) |
| Air Quality Exposure Category | Days in Period, n (%) | ED Visits, n | ED Visits per Day, n (95% CI) | IRR (95% CI) |
|---|---|---|---|---|
| Green zone PM2.5< 10 µg/m3 | 3178 (74.1) | 18,399 | 5.8 (5.6–5.9) | 1 (reference category) |
| Yellow zone PM2.5 10–19 µg/m3 | 938 (21.9) | 5438 | 5.8 (5.5–6.1) | 1.00 (0.97–1.03) |
| Orange zone PM2.5 20–27 µg/m3 | 85 (2.0) | 431 | 5.1 (4.2–5.9) | 0.88 (0.80–0.96) |
| Red zone PM2.5 >27 µg/m3 | 90 (2.1) | 501 | 5.6 (4.7–6.4) | 0.96 (0.88–1.05) |
| Wildfire smoke days | 60 (1.4) | 391 | 6.5 (5.6–7.5) | 1.13 (1.02–1.24) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moore, L.E.; Oliveira, A.; Zhang, R.; Behjat, L.; Hicks, A. Impacts of Wildfire Smoke and Air Pollution on a Pediatric Population with Asthma: A Population-Based Study. Int. J. Environ. Res. Public Health 2023, 20, 1937. https://doi.org/10.3390/ijerph20031937
Moore LE, Oliveira A, Zhang R, Behjat L, Hicks A. Impacts of Wildfire Smoke and Air Pollution on a Pediatric Population with Asthma: A Population-Based Study. International Journal of Environmental Research and Public Health. 2023; 20(3):1937. https://doi.org/10.3390/ijerph20031937
Chicago/Turabian StyleMoore, Linn E., Andre Oliveira, Raymond Zhang, Laleh Behjat, and Anne Hicks. 2023. "Impacts of Wildfire Smoke and Air Pollution on a Pediatric Population with Asthma: A Population-Based Study" International Journal of Environmental Research and Public Health 20, no. 3: 1937. https://doi.org/10.3390/ijerph20031937
APA StyleMoore, L. E., Oliveira, A., Zhang, R., Behjat, L., & Hicks, A. (2023). Impacts of Wildfire Smoke and Air Pollution on a Pediatric Population with Asthma: A Population-Based Study. International Journal of Environmental Research and Public Health, 20(3), 1937. https://doi.org/10.3390/ijerph20031937







