Relationship between Strength and Professional Quality of Life of Nurses Working Hospital Emergency Departments
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Determinations
2.3. Statistics
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- García Sánchez, S. La qualitat de vida professional com a avantatge competitiu. Rev. Qual. 1993, 11, 4–9. [Google Scholar]
- Howie, J. Atttitudes to medical care, the organization of work and stress among general practitioners. Br. J. Gen. Pr. 1992, 42, 181–185. [Google Scholar]
- Villares, J.E.; Ruiz, A.; López, M.P.; Sáinz, R. La satisfacción profesional en el equipo de atención primaria: Oportunidades de mejora. Cuad. Gestión 2000, 6, 60–67. [Google Scholar]
- Cabezas Peña, C. La calidad de vida de los profesionales. FMC 2000, 7 (Suppl. 7), 53–68. [Google Scholar]
- Martín, J.; Gómez Gascón, T.; Martínez, C.; Del Cura, I.; Cabezas, M.C.; García, S. Measurement of the evaluative capacity of the QPL-35 (CVP–35) questionnaire for perceiving quality of professional life. Aten Primaria 2008, 40, 327–336. [Google Scholar] [CrossRef][Green Version]
- Sibbald, B.; Enzer, I.; Cooper, C.; Routh, U.; Sutherland, V. GP job satisfaction in 1987, 1990, and 1998: Lessons for the future? Fam. Pr. 2000, 17, 364–371. [Google Scholar] [CrossRef][Green Version]
- Warren, N.; Hodgson, H.; Craig, T.; Dyrenforth, S.; Perlin, J.; Murphy, F.; Veterans Health Administration. Employee working conditions and healthcare system performance: The veterans health administration experience. J. Occup. Environ. Med. 2007, 49, 417–429. [Google Scholar] [CrossRef] [PubMed]
- Alonso Fernández, M.; Iglesias Carbajo, A.I.; Franco Vidal, A. Percepción de la calidad de vida profesional en un área sanitaria de Asturias. Aten Primaria 2002, 30, 483–489. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fernández Araque, A.; Cuairán Sola, M.; Curbelo Rodríguez, R. Calidad de vida profesional de enfermería en urgencias de un hospital de referencia. Enferm. Glob. 2016, 42, 376–385. [Google Scholar] [CrossRef]
- Chóliz, M. Ansiedad y trastornos del sueño [Anxiety and sleep disorders]. In Emociones y Salud [Emotions and Health]; Fernández-Abascal, E.G., Palmero, F., Eds.; Ariel: Barcelona, Spain, 1999; pp. 159–182. [Google Scholar]
- Martın, J.; Cortes, J.A. Caracterısticas metricas del cuestionario de calidad de vida profesional (CVP-35). Gac Sanit 2004, 18, 129–136. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Cavero-Redondo, I.; Ramírez-Vélez, R.; Ruiz, J.R.; Ortega, F.B.; Lee, D.C.; Martínez-Vizcaíno, V. Muscular strength as a predictor of all-cause mortality in an apparently healthy population: A Systematic Review and Meta-Analysis of data from approximately 2 million men and women. Arch. Phys. Med. Rehabil. 2018, 99, 2100–2113. [Google Scholar] [CrossRef] [PubMed]
- Celis-Morales, C.A.; Welsh, P.; Lyall, D.M.; Steell, L.; Petermann, F.; Anderson, J.; Iliodromiti, S.; Sillars, A.; Graham, N.; Mackay, D.F.; et al. Associations of grip strength with cardiovascular, respiratory, and cancer outcomes and all-cause mortality: Prospective cohort study of half a million UK Biobank participants. BMJ 2018, 361, k1651. [Google Scholar] [CrossRef] [PubMed]
- Mateo Lázaro, M.L.; Penacho Lázaro, M.A.; Berisa Losantos, F.; Plaza Bayo, A. Nuevas tablas de fuerza de la mano para población adulta de Teruel. Nutr. Hosp. 2008, 23, 35–40. [Google Scholar] [PubMed]
- Córdova, A. Fisiología Deportiva; Sintesis: Madrid, Spain, 2013. [Google Scholar]
- Heyward, V. Evaluación de la aptitud muscular. In Evaluación de la Aptitud Física y Prescripción del Ejercicio, 5th ed.; Heyward, V., Ed.; Editorial Médica Panamericana: Madrid, Spain, 2008; pp. 117–139. [Google Scholar]
- Chau, N.; Bourgkard, E.; Pétry, D.; Huguenin, P.; Remy, E.; André, J. Comparison between estimates of hand volume and hand strengths with sex and age with and without anthropometric data in healthy working people. Eur. J. Epidemiol. 1997, 13, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Valdecantos, D.; Caballero-García, A.; Del Castillo-Sanz, T.; Bello, H.J.; Roche, E.; Córdova, A. Stress salivary biomarkers variation during the work day in Emergencies in healthcare professionals. Int. J. Environ. Res. Public Health 2021, 18, 3937. [Google Scholar] [CrossRef]
- Weibel, L.; Gabrion, I.; Aussedat, M.; Kreutz, G. Work-related stress in an emergency medical dispatch center. Ann. Emerg. Med. 2003, 41, 500–506. [Google Scholar] [CrossRef]
- Karasek, R. The political implications of psychosocial work redesign: A model of the psychosocial class structure. Int. J. Health Serv. 1989, 19, 481–508. [Google Scholar] [CrossRef]
- Pérez-Valdecantos, D.; Caballero-García, A.; Bello-Gutiérrez, H.; Noriega-González, D.; Palomar-Ciria, N.; Roche, A.; Roche, E.; Córdova-Martínez, A. Health and Quality of Life of healthcare professionals working in Hospital Emergency Departments. Behav. Sci. 2022, 12, 188. [Google Scholar] [CrossRef]
- Adriaenssens, J.; De Gucht, V.; Van Der Doef, M.; Maes, S. Exploring the burden of emergency care: Predictors of stress-health outcomes in emergency nurses. J. Adv. Nurs. 2011, 67, 1317–1328. [Google Scholar] [CrossRef]
- Bohannon, R.W. Muscle strength: Clinical and prognostic value of hand-grip dynamometry. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 465–470. [Google Scholar] [CrossRef]
- Torres, M.; González del Pino, J.; Yáñez, J.; del Valle, E.B. Estudio dinamométrico de la mano y el pulgar. [Dynamometric study of the hand and thumb]. Rev. Esp. Cir. Ortop. Traumatol. 1999, 43, 321–326. [Google Scholar]
- Roberts, H.C.; Denison, H.J.; Martin, H.J.; Patel, H.P.; Syddall, H.; Cooper, C.; Sayer, A.A. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardised approach. Age Ageing 2021, 40, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W. Hand-grip dynamometry predicts future outcomes in aging adults. J. Geriatr. Phys. 2008, 31, 3–10. [Google Scholar] [CrossRef]
- Silventoinen, K.; Magnusson, P.K.; Tynelius, P.; Batty, G.D.; Rasmussen, F. Association of body size and muscle strength with incidence of coronary heart disease and cerebrovascular diseases: A population-based cohort study of one million Swedish men. Int. J. Epidemiol. 2009, 38, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Fraser, B.J.; Huynh, Q.L.; Schmidt, M.D.; Dwyer, T.; Venn, A.J.; Magnussen, C.G. Childhood muscular fitness phenotypes and adult metabolic syndrome. Med. Sci. Sport. Exerc. 2016, 48, 1715–1722. [Google Scholar] [CrossRef]
- Sayer, A.A.; Syddall, H.E.; Martin, H.J.; Dennison, E.M.; Roberts, H.C.; Cooper, C. Is grip strength associated with health-related quality of life? Findings from the Hertfordshire Cohort Study. Age Ageing 2006, 35, 409–415. [Google Scholar] [CrossRef]
- Stessman, J.; Rottenberg, Y.; Fischer, M.; Hammerman-Rozenberg, A.; Jacobs, J.M. Handgrip Strength in Old and Very Old Adults: Mood, Cognition, Function, and Mortality. J. Am. Geriatr. Soc. 2017, 65, 526–532. [Google Scholar] [CrossRef]
- Weyerer, S.; Schäufele, M. The assessment of quality of life in dementia. Int. Psychogeriatr. 2003, 15, 213–218. [Google Scholar] [CrossRef]
- Clúa, J.L.; Aguilar, C. La calidad de vida profesional y el orgullo de trabajar en la sanidad pública. Resultados de una encuesta. Aten Primaria 1998, 22, 308–313. [Google Scholar]
- Casas, J.; Repullo, J.R.; Lorenzo, S.; Cañas, J.J. Dimensiones y medición de la calidad de vida laboral en profesionales sanitarios. Rev. Adm. Sanit. 2002, VI, 527–544. [Google Scholar]
- Pérez-Valdecantos, D.; Caballero-García, A.; Del Castillo-Sanz, T.; Bello, H.J.; Roche, E.; Roche, A.; Córdova, A. Variations in salivary stress biomarkers and their relationship with Anxiety, Self-Efficacy and Sleeping Quality in Emergency Health Care Professionals. Int. J. Environ. Res. Public Health 2021, 18, 9277. [Google Scholar] [CrossRef] [PubMed]
- Keller, S.M. Effects of extended work shifts and shift work on patient safety, productivity, and employee health. AAOHN J. 2009, 57, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Lockley, S.W.; Barger, L.K.; Ayas, N.T.; Rothschild, J.M.; Czeisler, C.A.; Landrigan, C.P. Effects of health care provider work hours and sleep deprivation on safety and performance. Jt. Comm. J. Qual. Patient Saf. 2007, 33, 7–18. [Google Scholar] [CrossRef] [PubMed]
- Folkard, S.; Tucker, P. Shift work, safety and productivity. Occup. Med. 2003, 53, 95–101. [Google Scholar] [CrossRef]
| HOSPITALS | n | Gender |
|---|---|---|
| Total | 59 | 49 Women/10 Men |
| HCUV | 28 | 23 Women/5 Men |
| HSBS | 31 | 26 Women/5 Men |
| AGE (years) | ||
| HCUV | ||
| Nurses (Women) | 35.6 ± 10.6 | |
| Nurses (Men) | 34.6 ± 7.0 | |
| HSBS | ||
| Nurses (Women) | 42.6 ± 13.1 | |
| Nurses (Men) | 45.2 ± 15.7 | |
| HSBS | WOMEN | MEN |
|---|---|---|
| Dynamometry T1 (Kg) | 29.0 ± 1.0 | 43.0 ± 9.0 * |
| Dynamometry T2 (Kg) | 27.5 ± 1.5 | 44.0 ± 8.0 * |
| Δ% Change | −5.17 | 2.33 |
| Lactate T1 (mmol/L) | 2.2 ± 0.5 | 2.6 ± 1.4 |
| Lactate T2 (mmol/L) | 3.2 ± 0.8 # | 5.5 ± 2.3 *,# |
| Δ% Change | 51.2 | 115.7 |
| HCUV | WOMEN | MEN |
| Dynamometry T1 (Kg) | 27.0 ± 3.0 | 44.0 ± 12.0 * |
| Dynamometry T2 (Kg) | 24.5 ± 3.5 | 41.0 ± 11.0 * |
| Δ% Change | −9.3 | −6.8 |
| Lactate T1 (mmol/L) | 2.0 ± 0.2 | 2.1 ± 0.5 |
| Lactate T2 (mmol/L) | 2.9 ± 0.4 # | 2.5 ± 1.1# |
| Δ% Change | 45.0 | 19.5 |
| HSBS | WOMEN | MEN |
|---|---|---|
| Cortisol T1 (µg/dL) | 10.1 ± 3.5 | 14.7 ± 10.1 |
| Cortisol T2 (µg/dL) | 1.3 ± 0.3 # | 1.5 ± 0.8 # |
| Δ% Change | −87.0 | −90.0 |
| HCUV | WOMEN | MEN |
| Cortisol T1 (µg/dL) | 7.4 ± 1.9 | 23.4 ± 14.4 * |
| Cortisol T2 (µg/dL) | 1.2 ± 0.3 # | 3.0 ± 2.4 # |
| Δ% Change | −84.0 | −87.1 |
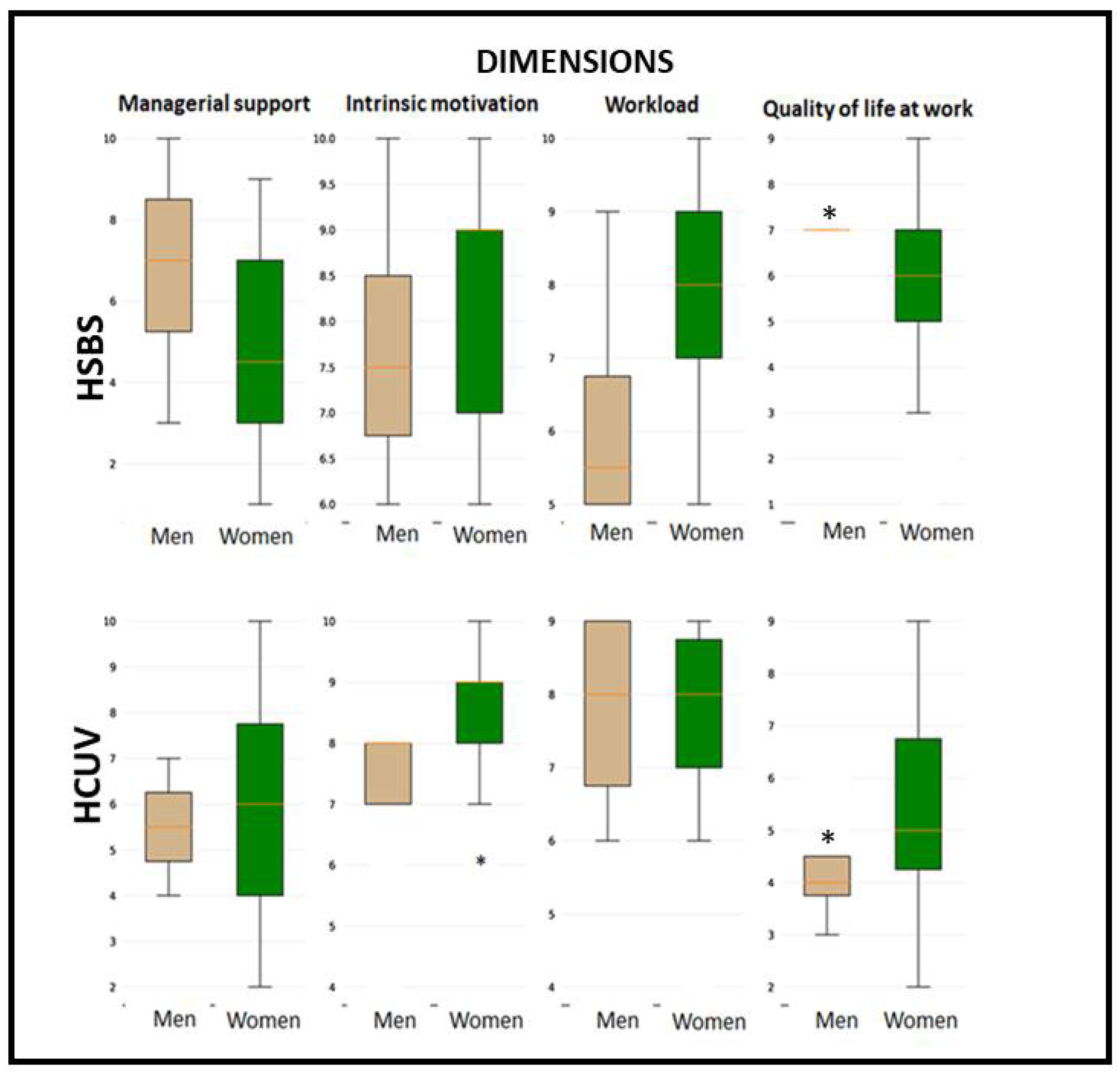
| Factors | 95% Median CI | |
|---|---|---|
| HSBS | HCUV | |
| Managerial support factor (dimension 1) | 7.3 ± 1.3 | 7.2 ± 1.3 |
| Workload factor (dimension 2) | 6.0 ± 1.1 | 6.2 ± 1.0 |
| Intrinsic motivation factor (dimension 3) | 8.3 ± 0.8 | 8.2 ± 0.7 |
| Quality of life at work | 6.1 ± 1.0 | 6.0 ± 1.2 |
| Dynamometry (Kg) | Dynamometry (Kg) | Lactate (mmol/L) | Lactate (mmol/L) | Cortisol (μg/dL) | Cortisol (μg/dL) | ||
|---|---|---|---|---|---|---|---|
| T1 | T2 | T1 | T2 | T1 | T2 | ||
| Dynamometry (Kg) | T1 | 1 | 0.84 | −0.061 | −0.005 | 0.014 | 0.028 |
| Dynamometry (Kg) | T2 | 0.84 | 1 | 0.03 | 0.067 | −0.037 | −0.025 |
| Lactate (mmol/L) | T1 | −0.061 | 0.03 | 1 | 0.26 | −0.0072 | −0.0087 |
| Lactate (mmol/L) | T2 | −0.005 | 0.067 | 0.26 | 1 | 0.14 | 0.022 |
| Cortisol (μg/dL) | T1 | 0.014 | −0.037 | −0.0072 | 0.14 | 1 | 0.11 |
| Cortisol (μg/dL) | T2 | 0.028 | −0.025 | −0.0087 | 0.022 | 0.11 | 1 |
| Dynamometry (Kg) | Dynamometry (Kg) | Lactate (mmol/L) | Lactate (mmol/L) | Cortisol (μg/dL) | Cortisol (μg/dL) | ||
|---|---|---|---|---|---|---|---|
| T1 | T2 | T1 | T2 | T1 | T2 | ||
| Dynamometry (Kg) | T1 | 1 | 0.94 | −0.11 | 0.14 | 0.32 | 0.29 |
| Dynamometry (Kg) | T2 | 0.94 | 1 | 0.21 | −0.061 | 0.38 | 0.2 |
| Lactate (mmol/L) | T1 | −0.11 | 0.21 | 1 | 0.48 | 0.28 | −0.34 |
| Lactate (mmol/L) | T2 | −0.14 | −0.061 | 0.48 | 1 | 0.19 | −0.34 |
| Cortisol (μg/dL) | T1 | 0.32 | 0.38 | 0.28 | 0.19 | 1 | 0.68 |
| Cortisol (μg/dL) | T2 | 0.29 | 0.2 | −0.34 | −0.34 | 0.68 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Córdova-Martínez, A.; Pérez-Valdecantos, D.; Caballero-García, A.; Bello, H.J.; Roche, E.; Noriega-González, D. Relationship between Strength and Professional Quality of Life of Nurses Working Hospital Emergency Departments. Int. J. Environ. Res. Public Health 2023, 20, 2052. https://doi.org/10.3390/ijerph20032052
Córdova-Martínez A, Pérez-Valdecantos D, Caballero-García A, Bello HJ, Roche E, Noriega-González D. Relationship between Strength and Professional Quality of Life of Nurses Working Hospital Emergency Departments. International Journal of Environmental Research and Public Health. 2023; 20(3):2052. https://doi.org/10.3390/ijerph20032052
Chicago/Turabian StyleCórdova-Martínez, Alfredo, Daniel Pérez-Valdecantos, Alberto Caballero-García, Hugo J. Bello, Enrique Roche, and David Noriega-González. 2023. "Relationship between Strength and Professional Quality of Life of Nurses Working Hospital Emergency Departments" International Journal of Environmental Research and Public Health 20, no. 3: 2052. https://doi.org/10.3390/ijerph20032052
APA StyleCórdova-Martínez, A., Pérez-Valdecantos, D., Caballero-García, A., Bello, H. J., Roche, E., & Noriega-González, D. (2023). Relationship between Strength and Professional Quality of Life of Nurses Working Hospital Emergency Departments. International Journal of Environmental Research and Public Health, 20(3), 2052. https://doi.org/10.3390/ijerph20032052











