Impact of the COVID-19 Pandemic on Psychosocial Well-being and Adaptation in Children and Adolescents with Asperger’s Syndrome
Abstract
1. Introduction
Research Questions
2. Materials and Methods
2.1. Procedures
2.2. Participants
2.3. Instruments
2.3.1. Perceived Risk Questionnaire
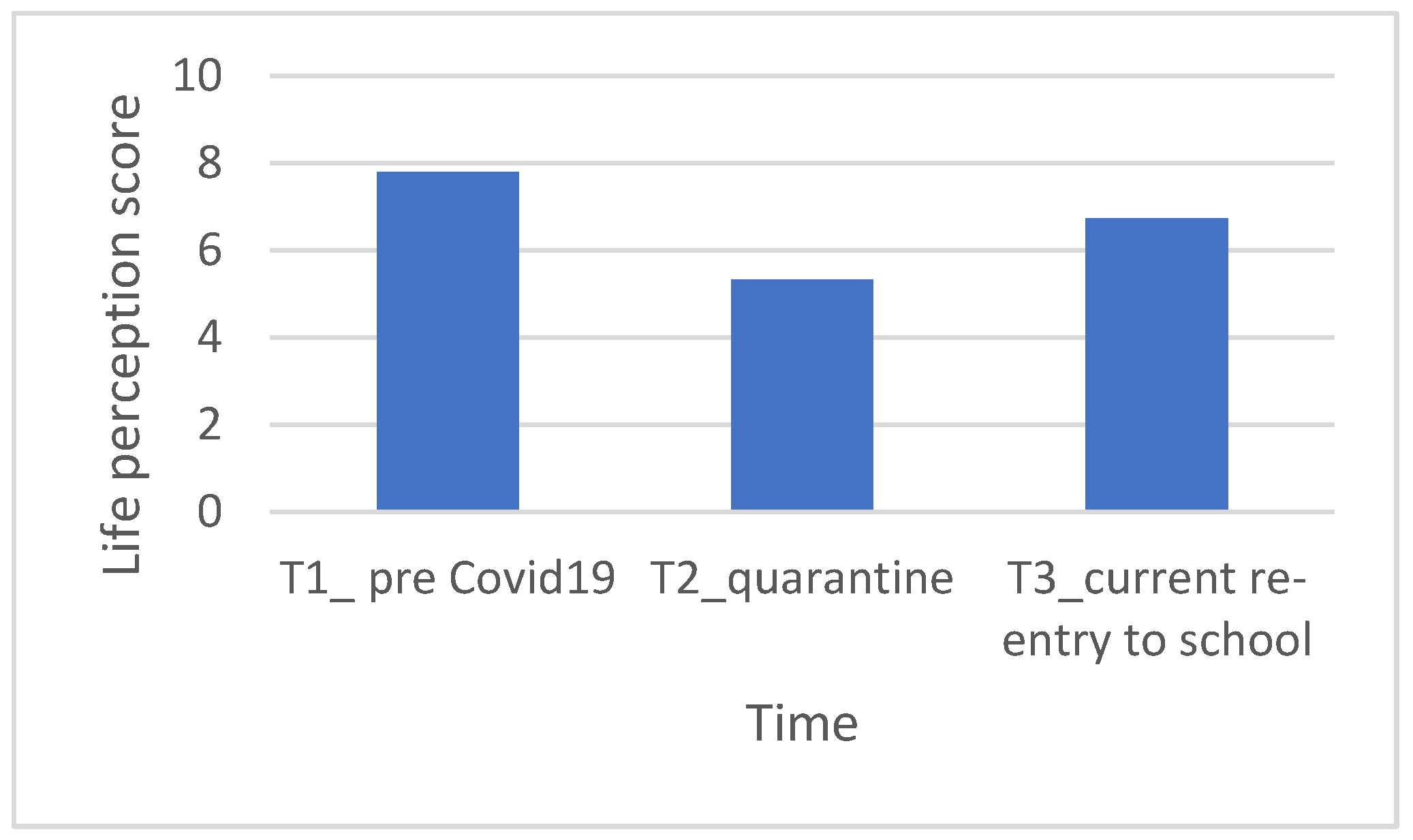
2.3.2. Cantrill’s Self-Anchoring Ladder of Life Satisfaction
- What level would you have been at about a year ago when you started school in September 2019.
- At what level would you have placed yourself during quarantine.
- At what level do you position yourself at the moment.
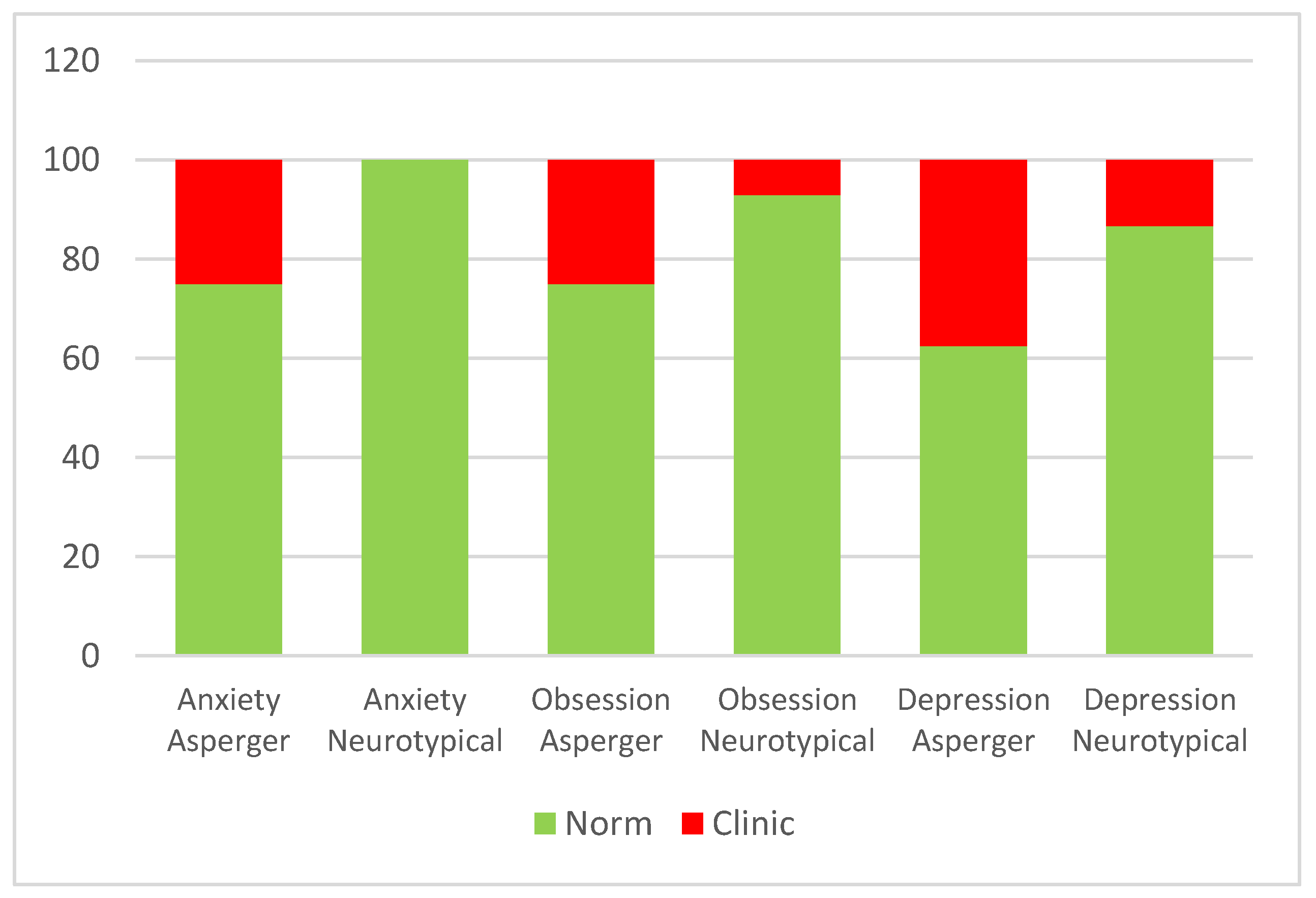
2.3.3. The SAFA Battery
2.3.4. The Adaptive Behavior Assessment System II (ABAS-II)
2.3.5. Center for Epidemiological Studies-Depression (CES-D)
2.3.6. General Anxiety Disorder-7 (GAD-7)
2.3.7. General Health Questionnaire (GH12)
2.4. Statistical Analysis Plan
3. Results
3.1. Knolewdge about Coronavirus and Anti-COVID Rules in Asperger and Typically Adolescents
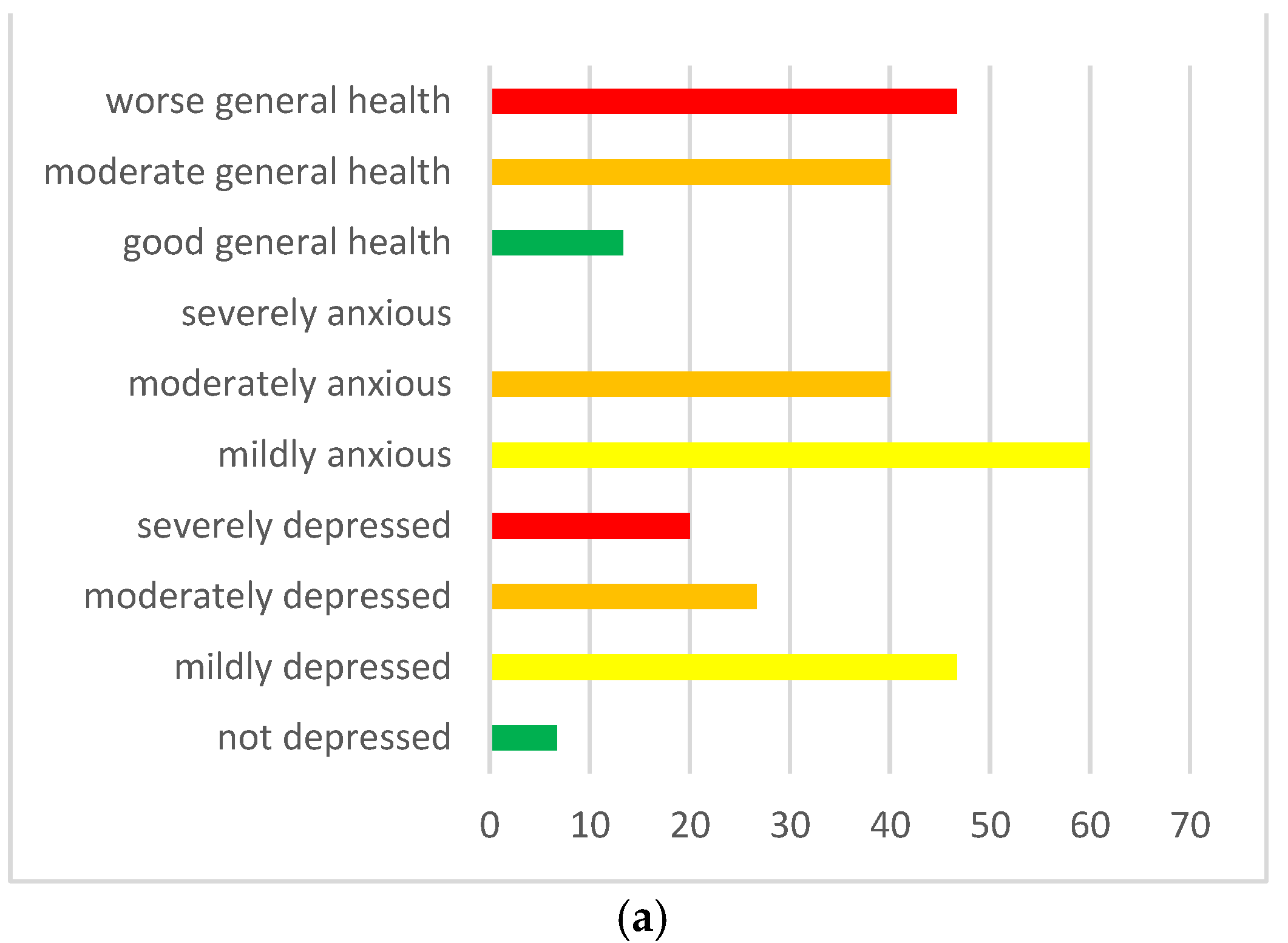
3.2. Possible Psychological Consequences in Children with Asperger’s and in Their Parents during Quarantine
3.3. Main Psychological Difficulties for Children and Young People with Asperger Syndrome with Returning to School and Resuming Social Life since September 2020
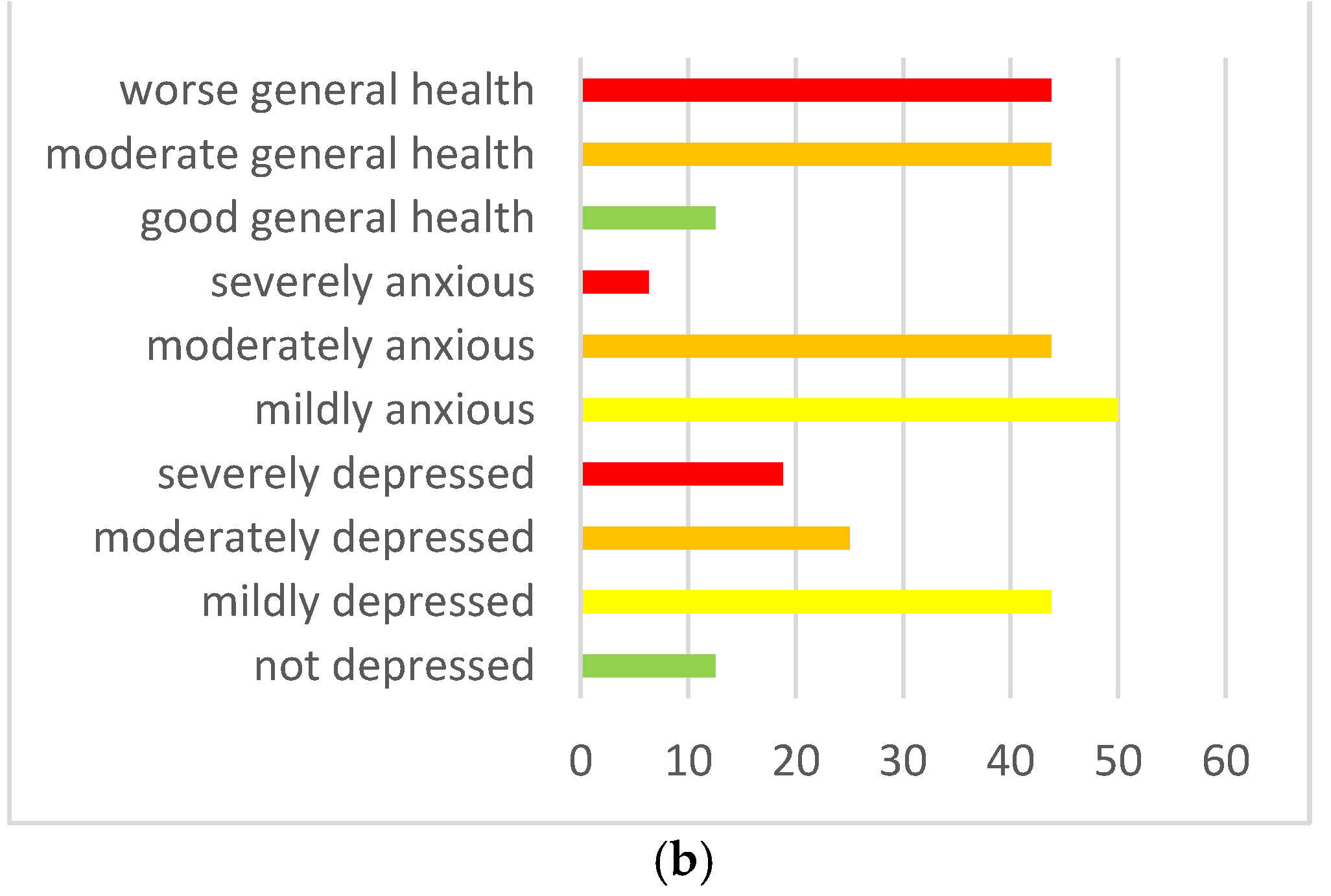
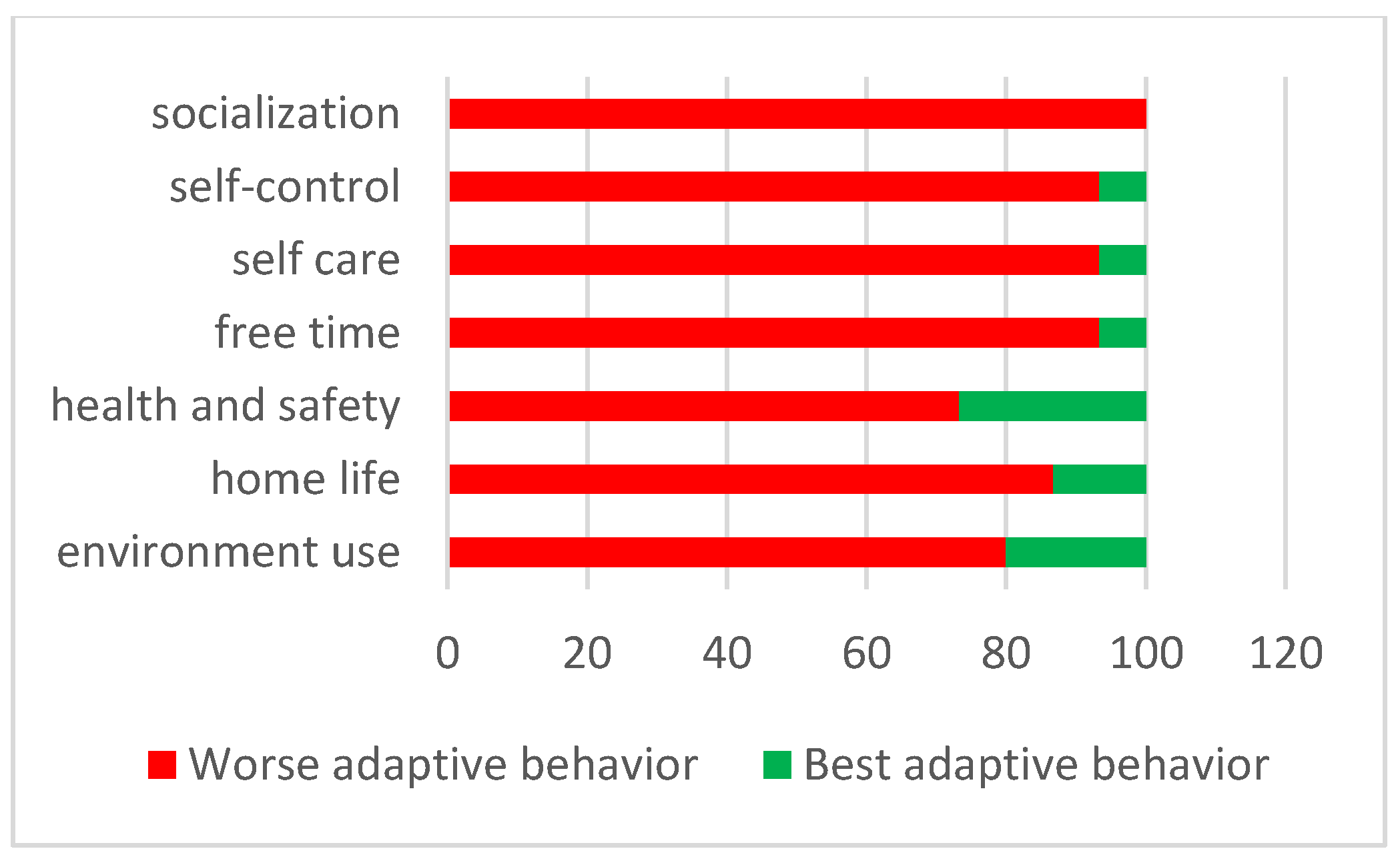
3.4. The High Parental Stress Experienced during the Lockdown Influenced the Emotional and Behavioral Difficulties when Children Experienced the Return to School and to Everyday Life since September 2020
4. Discussion
Strengths and Limits
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5); American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Attwood, T. Guida Completa alla Sindrome di Asperger; Edra: Perignano, Italy, 2019. [Google Scholar]
- Baio, J.; Wiggins, L.; Christensen, D.L.; Maenner, M.J.; Daniels, J.; Warren, Z.; Vehorn, A.; Esler, A.; Salinas, A.; Durkin, M.S.; et al. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR Surveill. Summ. 2018, 67, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Baumer, N.; Spence, S. Evaluation and management of the child with autism spectrum disorder. Continuum 2018, 24, 248–275. [Google Scholar] [CrossRef]
- Di Giorgio, E.; Polli, R.; Lunghi, M.; Murgia, A. Impact of the COVID-19 Italian Lockdown on the Physiological and Psychological Well-Being of Children with Fragile X Syndrome and Their Families. Int. J. Environ. Res. Public Health 2021, 18, 5752. [Google Scholar] [CrossRef] [PubMed]
- Vasa, R.A.; Singh, V.; Holingue, C.; Kalb, L.G.; Jang, Y.; Keefer, A. Psychiatric problems during the COVID-19 pandemic in children with autism spectrum disorder. Autism Res. 2021, 14, 2113–2119. [Google Scholar] [CrossRef]
- Amorim, R.; Catarino, S.; Miragaia, P.; Ferreras, C.; Viana, V.; Guardiano, M. The impact of COVID-19 on children with autism spectrum disorder. Rev. Neurol. 2020, 71, 285–291. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, H.; Shang, C.; Liang, H.; Liu, W.; Han, B.; Xia, W.; Zou, M.; Sun, C. Mental health issues in parents of children with autism spectrum disorder: A multi-time-point study related to COVID-19 pandemic. Autism Res. 2022, 15, 2346–2358. [Google Scholar] [CrossRef]
- Liu, J.J.; Bao, Y.; Huang, X.; Shi, J.; Lu, L. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc. Health 2020, 4, 347–349. [Google Scholar] [CrossRef]
- Marjanovic, Z.; Greenglass, E.R.; Coffey, S. The relevance of psychosocial variables and working conditions in predicting nurses coping strategies during the SARS crisis: An online questionnaire survey. Int. J. Nurs. Stud. 2007, 44, 991–998. [Google Scholar] [CrossRef]
- Reynolds, D.L.; Garay, J.R.; Deamond, S.L.; Moran, M.K.; Gold, W.; Styra, R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol. Infect. 2008, 136, 997–1007. [Google Scholar] [CrossRef]
- Bai, Y.; Lin, C.C.; Lin, C.Y.; Chen, J.Y.; Chue, C.M.; Chou, P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr. Serv. 2004, 55, 1055–1057. [Google Scholar] [CrossRef] [PubMed]
- Cava, M.A.; Fay, K.E.; Beanlands, H.J.; McCay, E.A.; Wignall, R. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nurs. 2005, 22, 398–406. [Google Scholar] [CrossRef] [PubMed]
- Robertson, E.; Hershenfield, K.; Grace, S.L.; Stewart, D.E. The psychosocial effects of being quarantined following exposure to SARS: A qualitative study of Toronto health care workers. Can. J. Psychiatry 2004, 49, 403–407. [Google Scholar] [CrossRef]
- Blendon, R.J.; Benson, J.M.; DesRoches, C.M.; Raleig, E.; Taylor-Clark, K. The public’s response to severe acute respiratory syndrome in Toronto and the United States. Clin. Infect. Dieasess 2004, 38, 925–931. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.; Yim, H.W.; Song, Y.J.; Ki, M.; Min, J.A.; Cho, J.; Chae, J.H. Mental health status of people isolated due to Middle East respiratory syndrome. Epidemiol. Health 2016, 38, e2016048. [Google Scholar] [CrossRef]
- Di Giovanni, C.; Conley, J.; Chiu, D.; Zaborski, J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur. Bioterror 2004, 2, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Xiang, M.; Zhang, Z.; Kuwahara, K. Impact of COVID-19 Pandemic on children and adolescents’ lifestyle behavior larger than expected. Prog. Cardiovasc. Dis. 2020, 63, 531–532. [Google Scholar] [CrossRef]
- Zhou, S.-J.; Wang, L.-L.; Yang, R.; Yang, X.-J.; Zhang, L.-G.; Guo, Z.-C.; Chen, J.-C.; Wang, J.-Q.; Chen, J.-X. Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med. 2020, 74, 39–47. [Google Scholar] [CrossRef]
- Uccella, S.; De Grandis, E.; De Carli, F.; D’Apruzzo, M.; Siri, L.; Preiti, D.; Di Profio, S.; Rebora, S.; Cimellaro, P.; Biolcati Rinaldi, A.; et al. Impact of the COVID-19 Outbreak on the Behavior of Families in Italy: A Focus on Children and Adolescents. Public Health 2021, 9, 32–43. [Google Scholar] [CrossRef]
- Zhou, S.-J.; Wang, L.-L.; Qi, M.; Yang, X.-J.; Gao, L.; Zhang, S.-Y.; Zhang, L.-G.; Yang, R.; Chen, J.-X. Depression, Anxiety, and Suicidal Ideation in Chinese University Students During the COVID-19 Pandemic. Front. Psychol. 2021, 12, 669833. [Google Scholar] [CrossRef]
- Magson, N.R.; Freeman, J.Y.A.; Rapee, R.M.; Richardson, C.E.; Oarl, E.L.; Fardouly, J. Risk and Protective Factors for Prospective Changes in Adolescent Mental Health during the COVID-19 Pandemic. J. Youth Adolesc. 2020, 50, 44–57. [Google Scholar] [CrossRef] [PubMed]
- Nearchou, F.; Flinn, C.; Niland, R.; Subramaniam, S.S.; Hennessy, E. Exploring the Impact of COVID-19 on Mental Health Outcomes in Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 8479. [Google Scholar] [CrossRef] [PubMed]
- Orgilés, M.; Morales, A.; Delvecchio, E.; Mazzeschi, C.; Espada, J.P. Immediate Psychological Effects of the COVID-19 Quarantine in Youth From Italy and Spain. Front. Psychol. 2020, 11, 579038. [Google Scholar] [CrossRef]
- Racine, N.; Cooke, J.E.; Eirich, R.; Korczak, D.J.; McArthur, B.; Madigan, S. Child and adolescent mental illness during COVID-19: A rapid review. Psychiatry Res. 2020, 292, 113307. [Google Scholar] [CrossRef] [PubMed]
- Spinelli, M.; Lionetti, F.; Pastore, M.; Fasolo, M. Parents’ Stress and Children’s Psychological Problems in Families Facing the COVID-19 Outbreak in Italy. Front. Psychol. 2020, 11, 1713. [Google Scholar] [CrossRef]
- Cantril, H. The Pattern of Human Concerns; Rutgers University Press: New Brunswick, NJ, USA, 1965; p. 22. [Google Scholar]
- Cianchetti, C.; Sannio Fancello, G. SAFA: Scale Psichiatriche Di Autosomministrazione Per Fanciulli E Adolescenti; Organizzazioni Speciali: Florence, Italy, 2001. [Google Scholar]
- Harrison, P.L.; Oakland, T. Adaptive Behavior Assessment System—Second Edition; Pearson Education: Los Angeles, CA, USA, 2003. [Google Scholar]
- Radloff, L.S. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl. Psychol. Meas. Psicol. Appl. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Gater, R.; Sartorius, N.; Ustun, T.B.; Piccinelli, M.; Gureje, O.; Rutter, C. The Validity of two Versions of the GHQ in the WHO Study of Mental Illness in General Health Care. Psychol. Med. 1997, 27, 191–197. [Google Scholar] [CrossRef]
- Goldberg, D.P. General Health Questionnaire (GHQ-12); NFER-Nelson: Windsor, UK, 1992. [Google Scholar]
- Politi, P.L.; Piccinelli, M.; Wilkinson, G. Reliability, validity and factor structure of the 12-item General Health Questionnaire among young males in Italy. Acta Psychiatr. Scand. 1994, 90, 432–437. [Google Scholar] [CrossRef]
- Piccinelli, M.; Bisoffi, G.; Bon, M.G.; Cunico, L.; Tansella, M. Validity and test-retest reliability of the Italian version of the 12-item General Health Questionnaire in general practice: A comparison between three scoring methods. Compreh. Psychiat. 1993, 34, 198–205. [Google Scholar] [CrossRef]
- Bonichini, S.; Tremolada, M. Quality of Life and Symptoms of PTSD during the COVID-19. Lockdown in Italy. Int. J. Environ. Res. Public Health 2021, 18, 4385. [Google Scholar] [CrossRef] [PubMed]
- Conti, E.; Sgandurra, G.; De Nicola, G.; Biagioni, T.; Boldrini, S.; Bonaventura, E.; Buchignani, B.; Della Vecchia, S.; Falcone, F.; Fedi, C.; et al. Behavioural and Emotional Changes during COVID-19 Lockdown in an Italian Paediatric Population with Neurologic and Psychiatric Disorders. Brain Sci. 2020, 10, 918. [Google Scholar] [CrossRef] [PubMed]
- Bates, L.C.; Zieff, G.; Stanford, K.; Moore, J.B.; Kerr, Z.Y.; Hanson, E.D.; Barone Gibbs, B.; Kline, C.E.; Stoner, L. COVID-19 Impact on Behaviors across the 24-Hour Day in Children and Adolescents: Physical Activity, Sedentary Behavior, and Sleep. Children 2020, 7, 138. [Google Scholar] [CrossRef] [PubMed]
- Masten, A.S.; Motti-Stefanidi, F. Multisystem Resilience for Children and Youth in Disaster: Reflections in the Context of COVID-19. Advers. Resil. Sci. 2020, 1, 95–106. [Google Scholar] [CrossRef] [PubMed]
- Prime, H.; Wade, M.; Browne, D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020, 75, 631–643. [Google Scholar] [CrossRef]
- Montirosso, R.; Mascheroni, E.; Guida, E.; Piazza, C.; Sali, M.E.; Molteni, M.; Reni, G. Stress symptoms and resilience factors in children with neurodevelopmental disabilities and their parents during the COVID-19 pandemic. Health Psychol. 2021, 40, 428–438. [Google Scholar] [CrossRef]
| Asperger | Neuro Typical | ||||||
|---|---|---|---|---|---|---|---|
| Adolescents | Frequency | Mean | SD | Frequency | Mean | SD | |
| Gender | Male | 16 | 16 | ||||
| Age | 14 | 3.62 | 14.07 | 3.31 | |||
| Age groups | 10–14 yrs old | 10 | 9 | ||||
| 15–20 yrs old | 6 | 6 | |||||
| School | Primary | 3 | 3 | ||||
| Secondary first grade | 6 | 5 | |||||
| Secondary second grade | 7 | 7 | |||||
| Support school | Yes | 12 | 0 | ||||
| No | 4 | 15 | |||||
| Parents | Frequency | Mean | SD | Frequency | Mean | SD | |
| Role | Father | 4 | 4 | ||||
| Mother | 11 | 12 | |||||
| Education | Primary/secondary school first grade | 0 | 0 | ||||
| Secondary second grade | 6 | 9 | |||||
| Yunior degree | 2 | 1 | |||||
| Degree | 7 | 5 | |||||
| Master/Ph.D. | 3 | 1 | |||||
| Number of children | 1 | 4 | 4 | ||||
| 2 | 8 | 9 | |||||
| 3 | 2 | 2 | |||||
| 4 | 0 | 1 | |||||
| 5 | 1 | 0 | |||||
| Child with other disabilities | Yes | 2 | 0 | ||||
| No | 13 | 15 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tremolada, M.; Rosa, M.; Incardona, R.M.; Taverna, L.; Guidi, M. Impact of the COVID-19 Pandemic on Psychosocial Well-being and Adaptation in Children and Adolescents with Asperger’s Syndrome. Int. J. Environ. Res. Public Health 2023, 20, 2132. https://doi.org/10.3390/ijerph20032132
Tremolada M, Rosa M, Incardona RM, Taverna L, Guidi M. Impact of the COVID-19 Pandemic on Psychosocial Well-being and Adaptation in Children and Adolescents with Asperger’s Syndrome. International Journal of Environmental Research and Public Health. 2023; 20(3):2132. https://doi.org/10.3390/ijerph20032132
Chicago/Turabian StyleTremolada, Marta, Mariangela Rosa, Roberta Maria Incardona, Livia Taverna, and Michele Guidi. 2023. "Impact of the COVID-19 Pandemic on Psychosocial Well-being and Adaptation in Children and Adolescents with Asperger’s Syndrome" International Journal of Environmental Research and Public Health 20, no. 3: 2132. https://doi.org/10.3390/ijerph20032132
APA StyleTremolada, M., Rosa, M., Incardona, R. M., Taverna, L., & Guidi, M. (2023). Impact of the COVID-19 Pandemic on Psychosocial Well-being and Adaptation in Children and Adolescents with Asperger’s Syndrome. International Journal of Environmental Research and Public Health, 20(3), 2132. https://doi.org/10.3390/ijerph20032132









