Loneliness and Psychosocial Resources among Indigenous and Afro-Descendant Older People in Rural Areas of Chile
Abstract
:1. Introduction
1.1. Loneliness among Older Adults
1.2. Risk Factors in Terms of Triggering Loneliness in Old Age
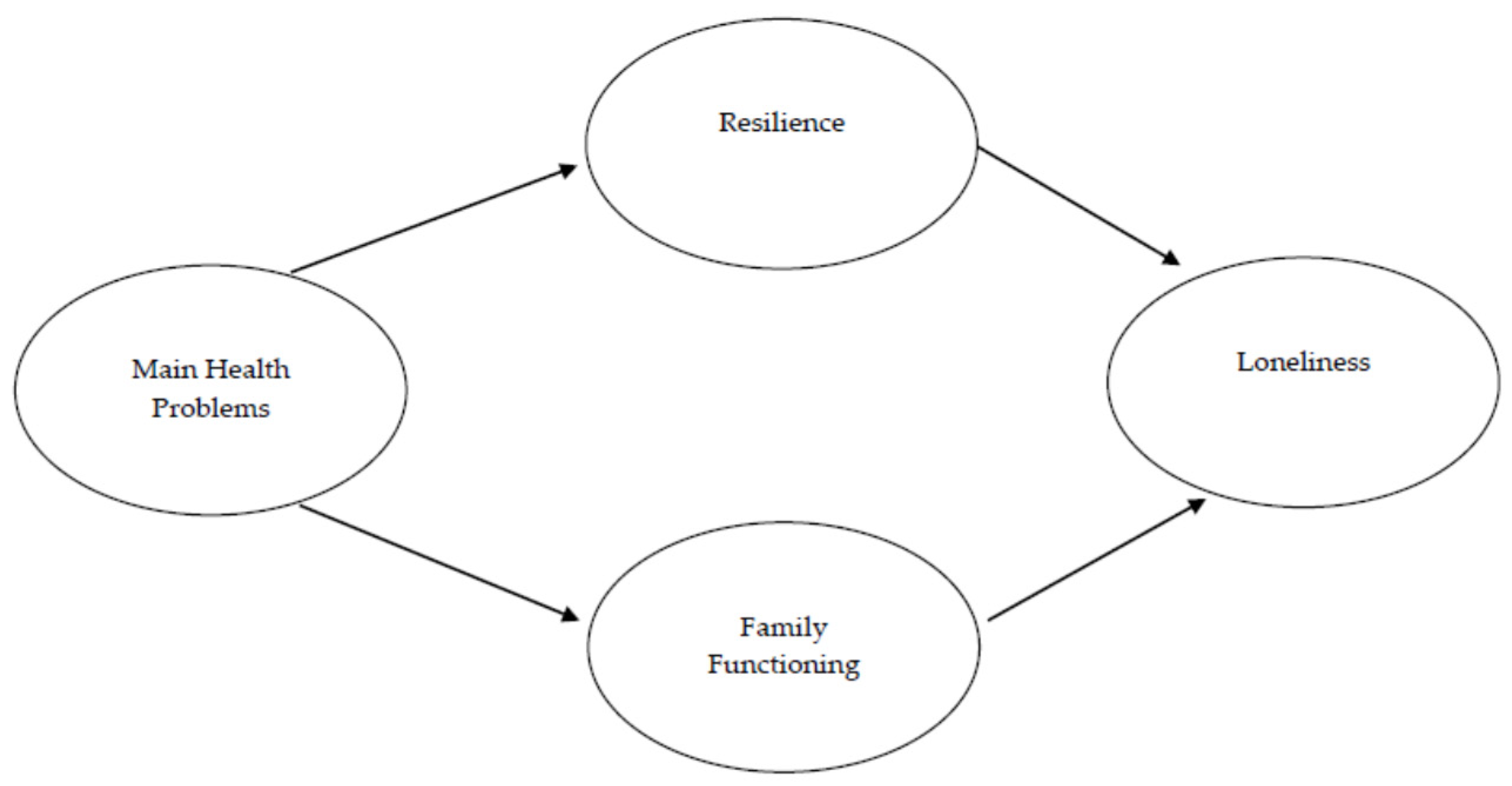
1.3. Present Piece of Research
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Ethical Issues
2.4. Measures
2.5. Analysis
3. Results
3.1. Descriptive and Correlation Analyses
3.2. Complete Structural Model
3.3. Structural Model of Mediated Relationships
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization (WHO). Advocacy Brief: Social Isolation and Loneliness among Older People; International Telecommunications Union, United Nations Department of Economic and Social Affairs, 2021. Available online: https://www.who.int/publications/i/item/9789240030749 (accessed on 17 October 2022).
- Surkalim, D.L.; Luo, M.; Eres, R.; Gebel, K.; van Buskirk, J.; Bauman, A.; Ding, D. The prevalence of loneliness across 113 countries: Systematic review and meta-analysis. BMJ 2022, 376, e067068. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, R.; Leavey, G.; Lawlor, B. We need a public health approach to loneliness. BMJ. 2022, 376, o280. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Cacioppo, S. The growing problem of loneliness. Lancet 2018, 391, 426. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peplau, L.A.; Perlman, D. Perspectives on loneliness. In Loneliness: A Source Book of Current Theory, Research and Therapy; Peplau, L.A., Perlman, D., Eds.; John Wiley & Sons: New York, NY, USA, 1982; pp. 1–18. [Google Scholar]
- de Jong Gierveld, J. A review of loneliness: Concept and definitions, determinants and consequences. Rev. Clin. Gerontol. 1998, 8, 73–80. [Google Scholar] [CrossRef] [Green Version]
- de Jong Gierveld, J.; Van Tilburg, T. A six-item scale for overall, emotional, and social loneliness: Confirmatory tests on survey data. Res. Aging 2006, 28, 582–598. [Google Scholar] [CrossRef] [Green Version]
- Newmyer, L.; Verdery, A.M.; Margolis, R.; Pessin, L. Measuring older adult loneliness across countries. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021, 76, 1408–1414. [Google Scholar] [CrossRef] [PubMed]
- Baumeister, R.F.; Leary, M.R. The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychol. Bull. 1995, 117, 497–529. [Google Scholar] [CrossRef] [PubMed]
- Weiss, R.S. Loneliness: The Experience of Emotional and Social Isolation; MIT Press: Cambridge, UK, 1973. [Google Scholar]
- Pinquart, M.; Sörensen, S. Influences on loneliness in older adults: A meta-analysis. Basic Appl. Soc. Psych. 2001, 23, 245–266. [Google Scholar] [CrossRef]
- Perlman, D.; Peplau, L.A. Loneliness. In Encyclopedia of Mental Health; Friedman, H., Ed.; Academic Press: San Diego, CA, USA, 1998; pp. 571–581. [Google Scholar]
- Lozano Benito, A.; Gallardo-Peralta, L.P. Soledad y bienestar emocional en mujeres mayores. Diversas experiencias durante el confinamiento en Bilbao. Alternativas 2022, 29, 208–235. [Google Scholar] [CrossRef]
- Ausín, B.; Muñoz, M.; Castellanos, M.A. Loneliness, Sociodemographic and Mental Health Variables in Spanish Adults over 65 Years Old. Span. J. Psychol. 2017, 20, 46. [Google Scholar] [CrossRef] [PubMed]
- Dykstra, P.A. Older adult loneliness: Myths and realities. Eur. J. Ageing 2009, 6, 91–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frenkel-Yosef, M.; Maytles, R.; Shrira, A. Loneliness and its concomitants among older adults during the covid-19 pandemic. Int. Psychogeriatr. 2020, 32, 1257–1259. [Google Scholar] [CrossRef] [PubMed]
- Gené-Badia, J.; Comice, P.; Belchín, A.; Erdozain, M.Á.; Cáliz, L.; Torres, S.; Rodríguez, R. Profiles of loneliness and social isolation in urban population. Aten. Primaria 2020, 52, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Kamiya, Y.; Doyle, M.; Henretta, J.C.; Timonen, V. Early-life circumstances and later-life loneliness in Ireland. Gerontologist 2014, 54, 773–783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Victor, C.R.; Scambler, S.J.; Bowling, A.; Bond, J. The prevalence of, and risk factors for, loneliness in later life: A survey of older people in Great Britain. Ageing Soc. 2005, 25, 357–375. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Social Development. The Social Report 2016: Te Purongo Oranga Tangata; Ministry of Social Development: Wellington, New Zealand, 2016. Available online: https://socialreport.msd.govt.nz/ (accessed on 18 October 2022).
- Cohen-Mansfield, J.; Hazan, H.; Lerman, Y.; Shalom, V. Correlates and predictors of loneliness in older-adults: A review of quantitative results informed by qualitative insights. Int. Psychogeriatr. 2016, 28, 557–576. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.H.; Islam, T.; Pillai, S.; Kalasapudi, L.; Mammen, S.; Inala, S.; Kalasapudi, V.; Islam, N.S.; Gunness, H. Loneliness and mental health outcomes among south asian older adult immigrants in the united states: A cross-sectional study. Int. J. Geriatr. Psychiatry 2021, 36, 1423–1435. [Google Scholar] [CrossRef] [PubMed]
- Lam, J. Neighbourhood characteristics, neighbourhood satisfaction and loneliness differences across ethnic-migrant groups in Australia. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021, 77, 2113–2125. [Google Scholar] [CrossRef] [PubMed]
- Cooper, E.J.; Sanguins, J.; Menec, V.; Chartrand, A.F.; Carter, S.; Driedger, S.M. Culturally Responsive Supports for Metis Elders and Metis Family Caregivers. Can. J. Aging 2020, 39, 206–219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marques, B.; Freeman, C.; Carter, L.; Pedersen Zari, M. Conceptualising therapeutic environments through culture, indigenous knowledge and landscape for health and well-being. Sustainability 2021, 13, 9125. [Google Scholar] [CrossRef]
- Pace, J. “Place-ing” dementia prevention and care in nunatukavut, labrador. Can. J. Aging 2020, 39, 247–262. [Google Scholar] [CrossRef] [PubMed]
- Quigley, R.; Russell, S.G.; Larkins, S.; Taylor, S.; Sagigi, B.; Strivens, E.; Redman-MacLaren, M. Aging Well for Indigenous Peoples: A Scoping Review. Front. Public Health 2022, 10, 780898. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Moreno, E.; Gallardo-Peralta, L.P.; Leyton, C. The social gradient in mental health and well-being for indigenous older adults living in rural areas: A cross-sectional comparison with rural non-indigenous population in Chile. J. Aging Health 2021, 33, 287–299. [Google Scholar] [CrossRef] [PubMed]
- Teh, J.K.; Tey, N.P.; Ng, S.T. Family support and loneliness among older persons in multiethnic Malaysia. Sci. World J. 2014, 2014, 654382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wright-St Clair, V.A.; Neville, S.; Forsyth, V.; White, L.; Napier, S. Integrative review of older adult loneliness and social isolation in Aotearoa/New Zealand. Australas. J. Ageing 2017, 36, 114–123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.; Shannon, K.; Napier, S.; Neville, S. Loneliness among older adults living in aged residential care in Aotearoa New Zealand and Australia: An integrative review. Nurs. Prax. N. Z. 2022, 38, 5–15. [Google Scholar] [CrossRef]
- Waters, W.F.; Gallegos, C.A. Aging, health, and identity in Ecuador’s indigenous communities. J. Cross-Cult. Gerontol. 2014, 29, 371–387. [Google Scholar] [CrossRef] [PubMed]
- Carrasco, M.; Fernández, M.; Alexander, E.; Herrera, M.S. Loneliness in Older Chilean People: Importance of Family Dysfunction and Depression. Int. J. Ment. Health Promot. 2021, 23, 99–109. [Google Scholar] [CrossRef]
- Ministry of Social Development. Corporación Nacional de Desarrollo Indígena (CONADI). Available online: https://www.bcn.cl/leychile/navegar?idNorma=1130641 (accessed on 15 December 2022).
- Herrera, M.S.; Elgueta, R.; Fernández, M.B.; Giacoman, C.; Leal, D.; Rubio, M.; Marshall, P.; Bustamante, F. Calidad de vida de las personas mayores chilenas durante la pandemia COVID-19. 2021. Available online: https://sociologia.uc.cl/wp-content/uploads/2021/07/libro_calidad-de-vida-pm-y-covid-19-.pdf (accessed on 15 December 2022).
- Rodríguez-Blázquez, C.; Ayala-García, A.; Forjaz, M.J.; Gallardo-Peralta, L.P. Validation of the De Jong Gierveld Loneliness Scale, 6-item version, in a multiethnic population of Chilean older adults. Australas. J. Ageing 2021, 40, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Economic Commission for Latin America and the Caribbean (ECLAC). El impacto del COVID-19 en los pueblos indígenas de América Latina-Abya Yala Entre la invisibilización y la resistencia colectiva. 2020. Available online: https://www.cepal.org/sites/default/files/publication/files/46543/S2000817_es.pdf (accessed on 18 October 2022).
- Sinclair, V.G.; Wallston, K.A. The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment 2004, 11, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Gallardo-Peralta, L.P.; Rodríguez-Blázquez, C.; Ayala-García, A.; Forjaz, M.J. Validación de la Escala Breve de Afrontamiento Resiliente (BRCS) en una muestra multiétnica de personas mayores chilenas. Interciencia 2020, 45, 524–531. [Google Scholar]
- Herrera, S.; Barros, C.; Fernández, B. Tercera Encuesta Nacional Calidad de Vida en la Vejez. 2013. Available online: http://www.senama.gob.cl/storage/docs/Resultados-Tercera-Encuesta-Nacional-Calidad-de-Vida-en-la-Vejez-2013.pdf (accessed on 25 October 2022).
- Smilkstein, G. The Family APGAR: A proposal for family function test and its use by physicians. J. Fam. Pract. 1978, 6, 1231–1239. [Google Scholar] [PubMed]
- Mayorga-Muñoz, C.; Gallardo-Peralta, L.; Galvez-Nieto, J.L. Propiedades psicométricas de la escala APGAR-familiar en personas mayores residentes en zonas rurales multiétnicas chilenas. Rev. méd. Chile. 2019, 147, 1283–1290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muthén, L.; Muthén, B. MPlus User’s Guide, 5th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2007. [Google Scholar]
- Schumacker, R.; Lomax, R.G. A Beginner’s Guide to Structural Equation Modelling; Lawrence Erlbaum Associates Inc.: Mahwah, NJ, USA, 1996. [Google Scholar]
- Browne, M.W.; Cudeck, R. Alternative ways of assessing model fit. In Testing Structural Equation Models; Bollen, K.A., Long, J.S., Eds.; Sage: Newbury Park, CA, USA, 1993; pp. 136–162. [Google Scholar]
- Gerino, E.; Rollè, L.; Sechi, C.; Brustia, P. Loneliness, Resilience, Mental Health, and Quality of Life in Old Age: A Structural Equation Model. Front. Psychol. 2017, 8, 2003. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Müller, F.; Röhr, S.; Reininghaus, U.; Riedel-Heller, S.G. Social Isolation and Loneliness during COVID-19 Lockdown: Associations with Depressive Symptoms in the German Old-Age Population. Int. J. Environ. Res. Public Health 2021, 18, 3615. [Google Scholar] [CrossRef] [PubMed]
- Pérez Peñaranda, A.; García Ortiz, L.; Rodríguez Sánchez, E.; Losada Baltar, A.; Porras Santos, N.; Gómez Marcos, M.A. Family function and the mental health of the career of the dependent relative. Aten. Primaria 2009, 41, 621–628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rocha-Vieira, C.; Oliveira, G.; Couto, L.; Santos, P. Impact of loneliness in the elderly in health care: A cross-sectional study in an urban region of Portugal. Fam. Med. Prim. Care Rev. 2019, 21, 138–143. [Google Scholar] [CrossRef]
- Dreser, A. Challenges and progress in the vaccination against COVID-19 in Latin America and the Caribbean. Rev. Univ. Ind. Santander. Salud. 2021, 53, e101. [Google Scholar]
- García Christian, L.L.; Gómez, M.I.; Martínez, C. Perspectiva ética de la priorización de vacunación contra el COVID-19 en Chile. Rev. méd. Chile. 2021, 149, 1795–1800. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Estrategia Gradual «Paso a Paso». 2020. Available online: https://cdn.digital.gob.cl/public_files/Campa%C3%B1as/Corona-Virus/documentos/paso-a-paso/Estrategia-Gradual-v2.pdf (accessed on 7 November 2022).
- Oppenheimer-Lewin, D.; Ortega-Palavecinos, M.; Núñez-Cortés, R. Resilience in older people during the first wave of the COVID-19 pandemic in Chile: Perspective from the social determinants of health. Rev. Esp. Geriatr. Gerontol. 2022, 57, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Franklin, A.; Tranter, B. Loneliness and the cultural, spatial, temporal and generational bases of belonging. Aust. J. Psychol. 2021, 73, 57–69. [Google Scholar] [CrossRef]
- Gallardo-Peralta, L.P.; Sanchez-Moreno, E.; Herrera, S. Aging and Family Relationships among Aymara, Mapuche and Non-Indigenous People: Exploring How Social Support, Family Functioning, and Self-Perceived Health Are Related to Quality of Life. Int. J. Environ. Res. Public Health 2022, 19, 9247. [Google Scholar] [CrossRef] [PubMed]
- Gallardo-Peralta, L.P.; Barrón López de Roda, A.; Molina-Martínez, M.A.; Schettini, R. Family and community support among older Chilean adults: The importance of heterogeneous social support sources for quality of life. J. Gerontol. Soc. Work 2018, 61, 584–604. [Google Scholar] [CrossRef] [PubMed]
- Gallardo-Peralta, L.P.; Raymond, É.; Gálvez-Nieto, J.L. Ageing in Context: An Ecological Model to Understand Social Participation Among Indigenous Adults in Chile. Res. Aging 2022, 52, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Carrasco, A.M.; González, H. Population mobility and processes of rural-urban linkages between the Aymara of northern Chile. Si Somos Am. 2014, 14, 217–231. [Google Scholar]
- Bolton, K.W.; Praetorius, R.T.; Smith-Osborne, A. Resilience protective factors in an older adult population: A qualitative interpretive meta-synthesis. Soc. Work Res. 2016, 40, 171–182. [Google Scholar] [CrossRef]
- Cosco, T.D.; Howse, K.; Brayne, C. Healthy ageing, resilience and wellbeing. Epidemiol. Psych. Sci. 2017, 26, 579–583. [Google Scholar] [CrossRef] [PubMed]
- Love, P.; Moore, M.; Warburton, J. Nurturing spiritual well-being among older people in australia: Drawing on indigenous and non-indigenous way of knowing. Australas. J. Ageing. 2017, 36, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Luthar, S.S.; Crossman, E.J.; Small, P.J. Resilience and adversity. In Handbook of Child Psychology and Developmental Science; Lerner, R., Ed.; Wiley: New York, NY, USA, 2015; pp. 247–386. [Google Scholar]
- Lavretsky, H. Cultural and ethnic factors in understanding and building resilience. In Resilience and Aging: Research and Practice; Lavretsky, H., Ed.; Johns Hopkins University Press: Baltimore, MD, USA, 2014; pp. 145–159. [Google Scholar]
- Olivi, A. Territorios de significado: La construcción del proyecto de vida de los mapuches en Chile. In Etnicidad y Desarrollo en los Andes; Palenzuela, P., Olivi, A., Eds.; Universidad de Sevilla: Sevilla, Spain, 2011; pp. 223–254. [Google Scholar]
- Rius-Ottenheim, N.; Kromhout, D.; van der Mast, R.C.; Zitman, F.G.; Geleijnse, J.M.; Giltay, E.J. Dispositional optimism and loneliness in older men. Int. J. Geriatr. Psychiatry 2012, 27, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, B.; Hülür, G. Well-Being and Loneliness in Swiss Older Adults During the COVID-19 Pandemic: The Role of Social Relationships. Gerontologist 2021, 61, 240–250. [Google Scholar] [CrossRef] [PubMed]
- Gallardo-Peralta, L.P.; Angulo, J.T.; Soto-Higuera, A.; Sánchez-Moreno, E. Cultural practices in indigenous Chilean communities: New findings for social work practice. In The Routledge Handbook of Social Work Field Education in the Global South; Taylor and Francis: London, UK, 2022; pp. 223–238. [Google Scholar]


| Quechua (n = 203) | Atacameño (n = 214) | Colla (n = 215) | Chango (n = 100) | Diaguita (n = 255) | Rapa Nui (n = 130) | Huilliche (n = 116) | Kawésqar (n = 10) | Afro-Descendants (n = 105) | Total (1.348) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | Women | 123 (61) | 152 (71) | 96 (45) | 53 (53) | 145 (57) | 71 (55) | 67 (58) | 8 (80) | 59 (56) | 774 (57) |
| Men | 80 (39) | 62 (29) | 119 (55) | 47 (47) | 110 (43) | 59 (45) | 49 (42) | 2(20) | 46 (44) | 574 (43) | |
| Age | 60–69 years | 105 (52) | 109 (51) | 85 (40) | 48 (48) | 104 (41) | 91 (70) | 43 (37) | 6 (60) | 67 (64) | 658 (49) |
| 70–79 years | 75 (37) | 80 (37) | 98 (46) | 35 (35) | 95 (37) | 31 (24) | 56 (48) | 4 (40) | 28 (27) | 502 (37) | |
| 80+ years | 23 (11) | 25 12) | 32 (14) | 17 (17) | 56 (22) | 8 (6) | 17 (15) | 0 | 10 (9) | 188 (14) | |
| Living situation | Alone | 84(41) | 52 (24) | 52(24) | 18(18) | 79 (31) | 25 (19) | 32 (28) | 1 (10) | 11 (10) | 69 (20) |
| With someone | 119 (59) | 162 (76) | 163 (76) | 82 (82) | 176 (69) | 105 (81) | 84 (72) | 9 (90) | 94 (90) | 275 (80) | |
| Marital status | Married/cohabiting | 108 (53) | 106 (50) | 123 (57) | 50 (50) | 110 (43) | 78 (60) | 61 (61) | 5 (50) | 72 (69) | 713 (53) |
| Single | 9 (4) | 33 (15) | 39 (18) | 23 (23) | 56 (22) | 25 (19) | 19 (16) | 0 | 11 (10) | 215 (16) | |
| Widow | 67 (33) | 53 (25) | 39 (18) | 13 (13) | 78 (31) | 27 (15) | 21 (18) | 5 (50) | 15 (14) | 318 (24) | |
| Divorced or similar | 19 (10) | 22 (10) | 14 (7) | 14 (14) | 11 (4) | 0 | 15 (13) | 0 | 7 (7) | 102 (7) | |
| Education | Primary school incomplete | 53 (26) | 24 (11) | 46 (21) | 10 (10) | 23 (9) | 8 (6) | 80 (69) | 4 (40) | 5 (5) | 253 (19) |
| Primary school | 72 (35) | 83 (39) | 83 (39) | 31 (31) | 45 (18) | 17 (13) | 21 (18) | 2 (20) | 12 (11) | 366 (27) | |
| High school or vocational education | 76 (38) | 100 (47) | 74 (34) | 53 (53) | 169 (66) | 88 (68) | 15 (13) | 4 (40) | 71 (68) | 650 (48) | |
| Higher education | 2 (1) | 7 (3) | 12 (6) | 6 (6) | 18 (7) | 17 (13) | 0 | 0 | 17 (16) | 79 (6) | |
| Afro-Descendants (n = 105) | Quechua (n = 203) | Atacameño (n = 214) | Colla (n = 215) | Chango (n = 100) | Diaguita (n = 255) | Rapa Nui (n = 130) | Huilliche (n = 116) | Kawésqar (n = 10) | Total (n = 1.348) | |
|---|---|---|---|---|---|---|---|---|---|---|
| n(%) | ||||||||||
| No loneliness (0–1 points) | s(45) | 61(30) | 54(25) | 50(23) | 38(38) | 219(86) | 118(91) | 3(2) | 2(20) | 592(44) |
| Loneliness (≥2 points) | 58(55) | 142(70) | 160(75) | 165(77) | 62(62) | 36(14) | 12(9) | 113(98) | 8(80) | 756(56) |
| Loneliness | Resilience | Health Problems | Family Functioning | |
|---|---|---|---|---|
| Median | −0.260 | 0.286 | −0.284 | 0.596 |
| Minimum | −1.396 | −4.043 | −1.118 | −3.205 |
| Maximum | 2.012 | 0.905 | 4.716 | 0.596 |
| K-S Test | 0.235 ** | 0.263 ** | 0.264 ** | 0.380 ** |
| Loneliness | Resilience | Health Problems | Family Functioning | |
|---|---|---|---|---|
| Loneliness | 1 | |||
| Resilience | −0.421 ** | 1 | ||
| Health problems | 0.138 ** | −0.172 ** | 1 | |
| Family functioning | −0.508 ** | 0.345 ** | −0.065 ** | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gallardo-Peralta, L.P.; Gálvez-Nieto, J.L.; Fernández-Dávila, P.; Veloso-Besio, C. Loneliness and Psychosocial Resources among Indigenous and Afro-Descendant Older People in Rural Areas of Chile. Int. J. Environ. Res. Public Health 2023, 20, 2138. https://doi.org/10.3390/ijerph20032138
Gallardo-Peralta LP, Gálvez-Nieto JL, Fernández-Dávila P, Veloso-Besio C. Loneliness and Psychosocial Resources among Indigenous and Afro-Descendant Older People in Rural Areas of Chile. International Journal of Environmental Research and Public Health. 2023; 20(3):2138. https://doi.org/10.3390/ijerph20032138
Chicago/Turabian StyleGallardo-Peralta, Lorena P., José Luis Gálvez-Nieto, Paula Fernández-Dávila, and Constanza Veloso-Besio. 2023. "Loneliness and Psychosocial Resources among Indigenous and Afro-Descendant Older People in Rural Areas of Chile" International Journal of Environmental Research and Public Health 20, no. 3: 2138. https://doi.org/10.3390/ijerph20032138





