COVID-19 Pandemic Impact on the Maternal Mortality in Kazakhstan and Comparison with the Countries in Central Asia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Maternal Mortality Registration Process in CA Countries
2.3. Data Analysis
3. Results
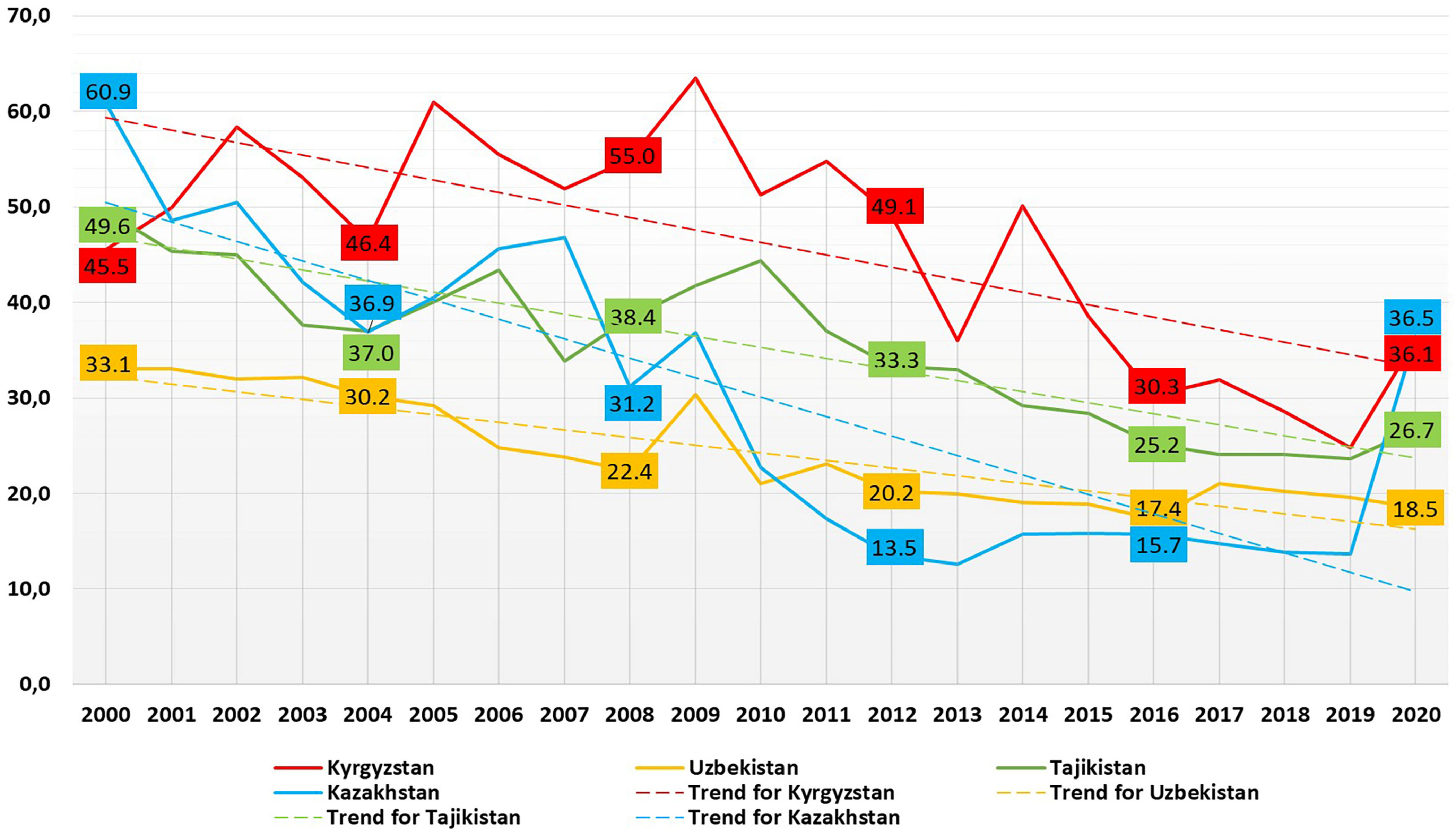
3.1. MM Situation in CA Countries and Its Trends from 2000 to 2020
3.2. The Comparison of the MM Causes before and during the Pandemic in Kazakhstan
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Years | Mean MMR | 95.0% Lower CI for Mean MMR | 95.0% Upper CI for Mean MMR |
|---|---|---|---|
| 2000 | 47.2 | 29.0 | 65.5 |
| 2001 | 44.2 | 32.0 | 56.4 |
| 2002 | 46.4 | 28.8 | 64.1 |
| 2003 | 41.2 | 27.1 | 55.3 |
| 2004 | 37.6 | 27.0 | 48.2 |
| 2005 | 42.7 | 21.5 | 63.8 |
| 2006 | 42.3 | 21.9 | 62.7 |
| 2007 | 39.1 | 18.8 | 59.3 |
| 2008 | 36.7 | 14.7 | 58.7 |
| 2009 | 43.1 | 20.2 | 65.9 |
| 2010 | 34.8 | 10.5 | 59.1 |
| 2011 | 33.0 | 6.5 | 59.5 |
| 2012 | 29.0 | 4.0 | 54.0 |
| 2013 | 25.4 | 7.8 | 42.9 |
| 2014 | 28.5 | 3.8 | 53.1 |
| 2015 | 25.4 | 9.0 | 41.7 |
| 2016 | 22.1 | 11.2 | 33.0 |
| 2017 | 22.9 | 11.6 | 34.2 |
| 2018 | 21.7 | 11.7 | 31.6 |
| 2019 | 20.4 | 12.4 | 28.3 |
| 2020 | 29.4 | 15.7 | 43.1 |
| Year | Tajikistan | Kazakhstan | Kyrgyzstan | Uzbekistan | ||||
|---|---|---|---|---|---|---|---|---|
| MM Cases | TFR | MM Cases | TFR | MM Cases | TFR | MM Cases | TFR | |
| 2000 | 100 | 4.0 | 134 | 1.8 | 44 | 2.4 | 230 | 2.6 |
| 2001 | 100 | 3.9 | 108 | 1.9 | 79 | 2.4 | 230 | 2.5 |
| 2002 | 83 | 3.8 | 118 | 2.0 | 86 | 2.4 | 230 | 2.5 |
| 2003 | 68 | 3.6 | 104 | 2.0 | 85 | 2.5 | 220 | 2.4 |
| 2004 | 64 | 3.5 | 100 | 2.2 | 85 | 2.6 | 210 | 2.5 |
| 2005 | 64 | 3.4 | 114 | 2.2 | 66 | 2.5 | 220 | 2.4 |
| 2006 | 61 | 3.4 | 138 | 2.4 | 67 | 2.7 | 210 | 2.4 |
| 2007 | 59 | 3.4 | 153 | 2.5 | 64 | 2.7 | 210 | 2.6 |
| 2008 | 57 | 3.4 | 204 | 2.7 | 70 | 2.8 | 210 | 2.6 |
| 2009 | 60 | 3.4 | 134 | 2.5 | 86 | 2.9 | 210 | 2.5 |
| 2010 | 55 | 3.5 | 84 | 2.6 | 75 | 3.1 | 133 | 2.4 |
| 2011 | 54 | 3.5 | 66 | 2.6 | 82 | 3.1 | 144 | 2.3 |
| 2012 | 52 | 3.4 | 52 | 2.6 | 76 | 3.2 | 126 | 2.2 |
| 2013 | 51 | 3.4 | 49 | 2.6 | 56 | 3.1 | 136 | 2.4 |
| 2014 | 50 | 3.5 | 47 | 2.7 | 81 | 3.2 | 137 | 2.5 |
| 2015 | 49 | 3.5 | 51 | 2.7 | 63 | 3.2 | 139 | 2.5 |
| 2016 | 47 | 3.4 | 52 | 2.8 | 48 | 3.1 | 126 | 2.5 |
| 2017 | 46 | 3.3 | 49 | 2.8 | 49 | 3 | 150 | 2.4 |
| 2018 | * | 3.3 | 56 | 2.8 | 49 | 3.3 | 155 | 2.6 |
| 2019 | * | 3.3 | 55 | 2.9 | 43 | 3.3 | 160 | 2.8 |
| 2020 | * | 3.2 | 156 | 3.1 | 61 | 3 | 156 | 2.9 |
| Year | MMR | Beds * | Obstetricians * | Women Accessing Prenatal Care, % | Women Accessing Postnatal Care, % | Share of Pregnancy Complications | Pregnancy, Postnatal Complications *** | ||
|---|---|---|---|---|---|---|---|---|---|
| Pregnancy Hypertensive Disorders, % | CVD **, % | Anemia, % | |||||||
| 2000 | 60.90 | 39.5 | 13.9 | 66.5 | 96.6 | 16.6 | 3.9 | 60.3 | 3320.2 |
| 2001 | 48.60 | 39.4 | 13.8 | 67 | 96.7 | 19.1 | 4 | 63.5 | 4263.9 |
| 2002 | 50.50 | 38.7 | 13.5 | 68.8 | 92.9 | 26.7 | 3.8 | 61.1 | 4921.5 |
| 2003 | 42.10 | 37 | 13.1 | 69.2 | 96.3 | 21.9 | 4 | 63.4 | 4547.3 |
| 2004 | 36.90 | 34.5 | 12.4 | 70.1 | 96 | 18.2 | 3.6 | 58.8 | 6368.5 |
| 2005 | 40.50 | 34.2 | 12.1 | 71.7 | 97.3 | 16.8 | 3.6 | 55.8 | 6787.4 |
| 2006 | 45.60 | 32.3 | 13.9 | 72.3 | 96.1 | 14 | 3.3 | 54.8 | 7817.4 |
| 2007 | 46.80 | 31.5 | 11 | 71.4 | 98 | 13.9 | 3.1 | 49.7 | 8012.7 |
| 2008 | 31.20 | 28.2 | 10.2 | 71.2 | 94.7 | 10.8 | 2.6 | 43.2 | 8075.1 |
| 2009 | 36.80 | 28.5 | 10.2 | 73 | 91.2 | 10.5 | 2.8 | 44.9 | 8367.3 |
| 2010 | 22.70 | 26.8 | 10.5 | 64.8 | 90.5 | 9.7 | 2.5 | 49.4 | 8517.7 |
| 2011 | 17.40 | 26.3 | 10.3 | 67.3 | 89.5 | 7.2 | 2 | 47.4 | 7598.3 |
| 2012 | 13.50 | 25 | 10.3 | 72.9 | 91.2 | 5.4 | 3.5 | 35.5 | 7091.1 |
| 2013 | 12.60 | 24.1 | 10.4 | 75.1 | 94 | 4.4 | 3.4 | 30.3 | 6495.3 |
| 2014 | 11.70 | 22.6 | 10.1 | 75.4 | 94.7 | 4 | 3.5 | 29.1 | 6223.4 |
| 2015 | 12.50 | 22 | 10.3 | 79.2 | 98.5 | 4.4 | 6.5 | 38.3 | 4617.6 |
| 2016 | 12.70 | 21.2 | 9.5 | 81.6 | 99.1 | 4.5 | 5.6 | 34.4 | 4591.5 |
| 2017 | 12.50 | 21.2 | 9.7 | 82.7 | 99.3 | 4.2 | 6 | 31.8 | 7128.2 |
| 2018 | 13.90 | 20.7 | 9.4 | 84.9 | 98.9 | 3.9 | 5.7 | 30.7 | 7448.3 |
| 2019 | 13.70 | 20.2 | 7.6 | 87.4 | 98.1 | 3.7 | 5.3 | 28.2 | 6239.7 |
| 2020 | 36.50 | 19.5 | 7.3 | 83.9 | 98 | 3.2 | 5.8 | 27 | 6071.4 |
References
- Moynihan, R.; Sanders, S.; Michaleff, Z.A.; Scott, A.M.; Clark, J.; To, E.J.; Jones, M.; Kitchener, E.; Fox, M.; Johansson, M.; et al. Impact of COVID-19 pandemic on utilization of healthcare services: A systematic review. BMJ Open 2021, 11, e045343. [Google Scholar] [CrossRef]
- Chmielewska, B.; Barratt, I.; Townsend, R.; Kalafat, E.; van der Meulen, J.; Gurol-Urganci, I.; O’Brien, P.; Morris, E.; Draycott, T.; Thangaratinam, S.; et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: A systematic review and meta-analysis. Lancet Glob. Health 2021, 9, e759–e772. [Google Scholar] [CrossRef] [PubMed]
- Aziz, N.; He, J.; Sarker, T.; Sui, H. Exploring the Role of Health Expenditure and Maternal Mortality in South Asian Countries: An Approach towards Shaping Better Health Policy. Int. J. Environ. Res. Public Health 2021, 18, 11514. [Google Scholar] [CrossRef]
- Dahab, R.; Sakellariou, D. Barriers to Accessing Maternal Care in Low Income Countries in Africa: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 4292. [Google Scholar] [CrossRef]
- Duarte, P. Central Asia: The Bends of History and Geography. Rev. Relac. Int. Estrateg. Segur. 2014, 9, 21–35. [Google Scholar] [CrossRef] [Green Version]
- World Bank Group. International Development, Poverty, & Sustainability. Available online: https://www.worldbank.org/en/home (accessed on 20 September 2022).
- Organisation for Economic Co-operation and Development. COVID-19 crisis response in Central Asia. 2020. Available online: https://www.oecd.org/coronavirus/policy-responses/covid-19-crisis-response-in-central-asia-5305f172/ (accessed on 23 September 2022).
- Balakrishnan, V.S. COVID-19 response in central Asia. Lancet Microbe 2020, 1, e281. [Google Scholar] [CrossRef] [PubMed]
- Health Spending as Percent of GDP—Country Rankings. Available online: https://www.theglobaleconomy.com/rankings/health_spending_as_percent_of_gdp/WB-high/ (accessed on 3 December 2022).
- Weaver, M.R.; Nandakumar, V.; Joffe, J.; Barber, R.M.; Fullman, N.; Singh, A.; Sparks, G.W.; Yearwood, J.; Lozano, R.; Murray, C.J.L.; et al. Variation in Health Care Access and Quality Among US States and High-Income Countries with Universal Health Insurance Coverage. JAMA Netw Open 2021, 4, e2114730. [Google Scholar] [CrossRef]
- World Health Organization. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. 2019. Available online: https://www.unfpa.org/sites/default/files/pub-pdf/Maternal_mortality_report.pdf (accessed on 4 October 2022).
- World Health Organization. Maternal Mortality. Evidence Brief Progress towards Achieving the Sustainable Development Goals. Available online: https://apps.who.int/iris/bitstream/handle/10665/329886/WHO-RHR-19.20-eng.pdf (accessed on 22 September 2022).
- GBD 2015 Maternal Mortality Collaborators. Global, regional, and national levels of maternal mortality, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1775–1812. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Say, L.; Chou, D.; Gemmill, A.; Tunçalp, Ö.; Moller, A.B.; Daniels, J.; Gülmezoglu, A.M.; Temmerman, M.; Alkema, L. Global causes of maternal death: A WHO systematic analysis. Lancet Glob. Health 2014, 2, e323–e333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skhvitaridze, N.; Anda, E.E.; Brenn, T.; Kintraia, N.; Gamkrelidze, A. Scoping maternal care through the lens of maternal deaths: A retrospective analysis of maternal mortality in Georgia. Sex Reprod. Healthc. 2020, 26, 100560. [Google Scholar] [CrossRef]
- Statistical Agency under the President of the Republic of Tajikistan; Ministry of Health and Social Protection of Population of the Republic of Tajikistan; ICF. Tajikistan Demographic and Health Survey 2017; Statistical Agency: Dushanbe, Tajikistan; ICF: Rockville, AR, USA, 2018; Available online: http://dhsprogram.com/pubs/pdf/FR341/FR341.pdf (accessed on 22 September 2022).
- WHO. SDG Target 3.1 Maternal Mortality. Available online: https://www.who.int/data/gho/data/themes/topics/sdg-target-3-1-maternal-mortality (accessed on 22 September 2022).
- Berhan, Y.; Berhan, A. Skilled Health Personnel Attended Delivery as a Proxy Indicator for Maternal and Perinatal Mortality: A Systematic Review. Ethiop. J. Health Sci. 2014, 24, 69–80. [Google Scholar] [CrossRef] [Green Version]
- Chen, L.; Feng, P.; Shaver, L.; Wang, Z. Maternal mortality ratio in China from 1990 to 2019: Trends, causes and correlations. BMC Public Health 2021, 21, 1536. [Google Scholar] [CrossRef] [PubMed]
- Owusu, P.A.; Sarkodie, S.A.; Pedersen, P.A. Relationship between mortality and health care expenditure: Sustainable assessment of health care system. PLoS ONE 2021, 16, e0247413. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, J.; Lawson, H.; Allotey, J.; Yap, M.; Balaji, R.; Kew, T.; Stallings, E.; Coomar, D.; Gaetano-Gil, A.; Zamora, J.; et al. Global variations in the burden of SARS-CoV-2 infection and its outcomes in pregnant women by geographical region and country’s income status: A meta-analysis. BMJ Glob. Health 2022, 7, e010060. [Google Scholar] [CrossRef]
- Meh, C.; Sharma, A.; Ram, U.; Fadel, S.; Correa, N.; Snelgrove, J.W.; Shah, P.; Begum, R.; Shah, M.; Hana, T.; et al. Trends in maternal mortality in India over two decades in nationally representative surveys. BJOG 2022, 129, 550–561. [Google Scholar] [CrossRef]
- Di Toro, F.; Gjoka, M.; Di Lorenzo, G.; De Santo, D.; De Seta, F.; Maso, G.; Risso, F.M.; Romano, F.; Wiesenfeld, U.; Levi-D’Ancona, R.; et al. Impact of COVID-19 on maternal and neonatal outcomes: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2021, 27, 36–46. [Google Scholar] [CrossRef]
- Sunder, A.; Varghese, B.; Darwish, B.; Shaikho, N.; Rashid, M. Impacts and effects of COVID-19 infection in pregnancy. Saudi Med. J. 2022, 43, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Januszewski, M.; Ziuzia-Januszewska, L.; Jakimiuk, A.A.; Wierzba, W.; Gluszko, A.; Zytynska-Daniluk, J.; Jakimiuk, A.J. Is the Course of COVID-19 Different during Pregnancy? A Retrospective Comparative Study. Int. J. Environ. Res. Public Health 2021, 18, 12011. [Google Scholar] [CrossRef]
- Naqvi, S.; Naqvi, F.; Saleem, S.; Thorsten, V.R.; Figueroa, L.; Mazariegos, M.; Garces, A.; Patel, A.; Das, P.; Kavi, A.; et al. Health care in pregnancy during the COVID -19 pandemic and pregnancy outcomes in six low-and-middle-income countries: Evidence from a prospective, observational registry of the Global Network for Women’s and Children’s Health. BJOG Int. J. Obstet. Gynaecol. 2022, 129, 1298–1307. [Google Scholar] [CrossRef]
- Al-Hajjar, S.; Ibrahim, L.; Kurdi, W.; Tulbah, M.; Alnemer, M.; Bin Jabr, M.; Elsaidawi, W.; Binmanee, A.; Ali, M.; Bukhari, H.; et al. Observational cohort study of perinatal outcomes of women with COVID-19. J. Infect. Public Health 2022, 15, 1503–1507. [Google Scholar] [CrossRef]
- Kotlar, B.; Gerson, E.; Petrillo, S.; Langer, A.; Tiemeier, H. The impact of the COVID-19 pandemic on maternal and perinatal health: A scoping review. Reprod. Health 2021, 18, 10. [Google Scholar] [CrossRef] [PubMed]
- Villar, J.; Ariff, S.; Gunier, R.B.; Thiruvengadam, R.; Rauch, S.; Kholin, A.; Roggero, P.; Prefumo, F.; Vale, M.S.D.; Cardona-Perez, J.A.; et al. Maternal and Neonatal Morbidity and Mortality Among Pregnant Women with and Without COVID-19 Infection. JAMA Pediatr. 2021, 175, 817–826. [Google Scholar] [CrossRef] [PubMed]
- Lokken, E.M.; Huebner, E.M.; Taylor, G.G.; Hendrickson, S.; Vanderhoeven, J.; Kachikis, A.; Coler, B.; Walker, C.L.; Sheng, J.S.; Al-Haddad, B.J.; et al. Disease severity, pregnancy outcomes, and maternal deaths among pregnant patients with severe acute respiratory syndrome coronavirus 2 infection in Washington State. Am. J. Obstet. Gynecol. 2021, 225, 77.e1–77.e14. [Google Scholar] [CrossRef]
- Metz, T.D.; Clifton, R.G.; Hughes, B.L.; Sandoval, G.J.; Grobman, W.A.; Saade, G.R.; Manuck, T.A.; Longo, M.; Sowles, A.; Clark, K.; et al. Association of SARS-CoV-2 Infection with Serious Maternal Morbidity and Mortality from Obstetric Complications. JAMA 2022, 327, 748–759. [Google Scholar] [CrossRef]
- Tekin, A.B.; Yassa, M.; Ilter, P.B.; Yavuz, E.; Önden, B.; Usta, C.; Budak, D.; Günkaya, O.S.; Çavuşoğlu, G.; Taymur, B.D.; et al. COVID-19 related maternal mortality cases in associated with Delta and Omicron waves and the role of lung ultrasound. J. Turk. Soc. Obstet. Gynecol. 2022, 19, 88–97. [Google Scholar] [CrossRef]
- Stock, S.J.; Moore, E.; Calvert, C.; Carruthers, J.; Denny, C.; Donaghy, J.; Hillman, S.; Hopcroft, L.E.M.; Hopkins, L.; Goulding, A.; et al. Pregnancy outcomes after SARS-CoV-2 infection in periods dominated by delta and omicron variants in Scotland: A population-based cohort study. Lancet Respir. Med. 2022, 10, 1129–1136. [Google Scholar] [CrossRef] [PubMed]
- Karimi, L.; Makvandi, S.; Vahedian-Azimi, A.; Sathyapalan, T.; Sahebkar, A. Effect of COVID-19 on Mortality of Pregnant and Postpartum Women: A Systematic Review and Meta-Analysis. J. Pregnancy 2021, 2021, 1–33. [Google Scholar] [CrossRef]
- Bisht, R.; Kandalgaonkar, V.P.; Shinde, K.K. Cesarean Section Rate among COVID-19 Mothers and Its Classification through Robson’s Criteria. J. South Asian Fed. Obstet. Gynaecol. 2021, 13, 342–346. [Google Scholar] [CrossRef]
- Michels, B.D.; Marin, D.F.D.; Iser, B.P.M. Increment of Maternal Mortality Among Admissions for Childbirth in Low-risk Pregnant Women in Brazil: Effect of COVID-19 Pandemic? Rev. Bras. Ginecol. Obstet. 2022, 44, 740–745. [Google Scholar] [CrossRef] [PubMed]
- Takemoto, M.L.; Menezes, M.O.; Andreucci, C.B.; Knobel, R.; Sousa, L.A.; Katz, L.; Fonseca, E.B.; Nakamura-Pereira, M.; Magalhães, C.G.; Diniz, C.S.; et al. Clinical characteristics and risk factors for mortality in obstetric patients with severe COVID-19 in Brazil: A surveillance database analysis. BJOG: Int. J. Obstet. Gynaecol. 2020, 127, 1618–1626. [Google Scholar] [CrossRef] [PubMed]
- Hessami, K.; Homayoon, N.; Hashemi, A.; Vafaei, H.; Kasraeian, M.; Asadi, N. COVID-19 and maternal, fetal and neonatal mortality: A systematic review. J. Matern. Neonatal Med. 2020, 35, 2936–2941. [Google Scholar] [CrossRef]
- La Verde, M.; Riemma, G.; Torella, M.; Cianci, S.; Savoia, F.; Licciardi, F.; Scida, S.; Morlando, M.; Colacurci, N.; De Franciscis, P. Maternal death related to COVID-19: A systematic review and meta-analysis focused on maternal co-morbidities and clinical characteristics. Int. J. Gynecol. Obstet. 2021, 154, 212–219. [Google Scholar] [CrossRef]
- Diniz, D.; Brito, L.; Rondon, G. Maternal mortality and the lack of women-centered care in Brazil during COVID-19: Preliminary findings of a qualitative study. Lancet Reg. Health Am. 2022, 10, 100239. [Google Scholar] [CrossRef] [PubMed]
- Lumbreras-Marquez, M.I.M.; Campos-Zamora, M.M.; Seifert, S.M.; Kim, J.M.; Lumbreras-Marquez, J.M.; Vazquez-Alaniz, F.; Fields, K.G.M.; Farber, M.K.M. Excess Maternal Deaths Associated with Coronavirus Disease 2019 (COVID-19) in Mexico. Obstet. Gynecol. 2020, 136, 1114–1116. [Google Scholar] [CrossRef] [PubMed]
- WHO. Maternal Mortality Ratio per 100,000 Live Births. Available online: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/26 (accessed on 22 September 2022).
- Ministry of Healthcare of the Republic of Kazakhstan. Kazakhstan Ministry of Health. Statistical Industry Data. Available online: https://www.gov.kz/memleket/entities/dsm/activities/directions?lang=en (accessed on 22 October 2022).
- Center of eHealth of Ministry of Health Republic of Kyrgyzstan. eHealth. Available online: http://cez.med.kg (accessed on 22 October 2022).
- Agency of Statistics under President of the Republic of Tajikistan. Demographic Yearbook of the Republic of Tajikistan. Available online: https://www.stat.tj/en/news/publications/demographic-yearbook-of-the-republic-of-tajikistan (accessed on 28 October 2022).
- United Nations Population Fund. Uzbekistan. Available online: https://uzbekistan.unfpa.org/en (accessed on 28 October 2022).
- World Health Organization. Maternal Mortality Measurement: Guidance to Improve National Reporting. 2022. Available online: https://apps.who.int/iris/handle/10665/360576 (accessed on 28 October 2022).
- WHO. Global Health Expenditure Database. Available online: https://apps.who.int/nha/database (accessed on 26 September 2022).
- Ministry of Justice of the Republic of Kazakhstan. Rules for the Provision of Maternal Mortality Information. Available online: https://adilet.zan.kz/kaz/docs/V2000021181 (accessed on 6 January 2022).
- Minister of Health of the Republic of Kazakhstan. Standard of Pathological and Anatomical Diagnostics in the Republic of Kazakhstan. 2020. Available online: https://adilet.zan.kz/kaz/docs/V2000021790 (accessed on 6 January 2022).
- Ministry of Health of the Kyrgyz Republic. On Improving the Completeness of Registration, Timely Reporting of Maternal Deaths to the Appropriate Authorities and the Reliability of the Maternal Mortality Indicator. 2011. Available online: https://online.zakon.kz/Document/?doc_id=31028500 (accessed on 6 January 2022).
- Rechel, B.; Ahmedov, M.; Akkazieva, B.; Katsaga, A.; Khodjamurodov, G.; McKee, M. Lessons from two decades of health reform in Central Asia. Health Policy Plan. 2011, 27, 281–287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dominis, S.; Yazbeck, A.S.; Hartel, L.A. Keys to Health System Strengthening Success: Lessons from 25 Years of Health System Reforms and External Technical Support in Central Asia. Health Syst. Reform 2018, 4, 160–169. [Google Scholar] [CrossRef]
- Thoma, M.E.; Declercq, E.R. All-Cause Maternal Mortality in the US Before vs During the COVID-19 Pandemic. JAMA Netw. Open 2022, 5, e2219133. [Google Scholar] [CrossRef] [PubMed]
- Amorim, M.M.R.; Takemoto, M.L.S.; da Fonseca, E.B. Maternal deaths with coronavirus disease 2019: A different outcome from low- to middle-resource countries? Am. J. Obstet. Gynecol. 2020, 223, 298–299. [Google Scholar] [CrossRef] [PubMed]
- World Bank Group. Fertility Rate, Total (Births per Woman). Available online: https://data.worldbank.org/indicator/SP.DYN.TFRT.IN?locations=KZ-TJ-KG-UZ (accessed on 7 January 2022).
- Laatikainen, T.; Inglin, L.; Chonmurunov, I.; Stambekov, B.; Altymycheva, A.; Farrington, J.L. National electronic primary health care database in monitoring performance of primary care in Kyrgyzstan. Prim. Health Care Res. Dev. 2022, 23. [Google Scholar] [CrossRef]
- Obermann, K.; Chanturidze, T.; Richardson, E.; Tanirbergenov, S.; Shoranov, M.; Nurgozhaev, A. Data for development in health: A case study and monitoring framework from Kazakhstan. BMJ Glob. Health 2016, 1, e000003. [Google Scholar] [CrossRef]
- World Health Organization. Quality of Care Review in Kyrgyzstan, Working Document. 2018. Available online: https://www.euro.who.int/__data/assets/pdf_file/0004/383890/kgz-qoc-eng.pdf (accessed on 9 January 2023).
- United Nations Economic Commission for Europe (UNECE), Eurostat (the Statistical Office of the European Union) and the Statistical Office of the European Free Trade Association (EFTA). Global Assessment of the National Statistical System of Kyrgyzstan. Available online: https://www.efta.int/sites/default/files/images/publications/GA%20Kyrgyzstan%20Final%20EN.pdf (accessed on 9 January 2023).
- United Nations Economic Commission for Europe (UNECE), the European Free Trade Association (EFTA) and the European Commission (Eurostat). Global Assessment of the National Statistical System of Tajikistan. Available online: https://unece.org/DAM/stats/documents/technical_coop/GA_Tajikistan_ENG.pdf (accessed on 9 January 2023).
- Rana, R.H.; Alam, K.; Gow, J. Health expenditure, child and maternal mortality nexus: A comparative global analysis. BMC Int. Health Hum. Rights 2018, 18, 29. [Google Scholar] [CrossRef] [PubMed]


| Year | Kazakhstan (Tenge) | Kyrgyzstan (Som) | Uzbekistan (Sum) | Tajikistan (Somoni) |
|---|---|---|---|---|
| 2000 | 108.164 | 2.885 | 209.474 | 77 |
| 2001 | 112.827 | 3.160 | 323.361 | 115 |
| 2002 | 136.505 | 3.461 | 480.187 | 148 |
| 2003 | 171.720 | 4.885 | 639.818 | 224 |
| 2004 | 233.812 | 5.852 | 744.062 | 296 |
| 2005 | 296.164 | 7.517 | 954.605 | 375 |
| 2006 | 347.088 | 9.459 | 1236.557 | 467 |
| 2007 | 347.349 | 9.837 | 1605.195 | 708 |
| 2008 | 489.538 | 12.267 | 2226.225 | 1041 |
| 2009 | 595.121 | 13.882 | 2949.005 | 1208 |
| 2010 | 596.963 | 15.316 | 3866.230 | 1417 |
| 2011 | 734.988 | 20.326 | 4986.864 | 1762 |
| 2012 | 942.012 | 26.420 | 6561.890 | 2163 |
| 2013 | 958.606 | 29.090 | 8183.944 | 2647 |
| 2014 | 1180.231 | 29.482 | 8278.274 | 3040 |
| 2015 | 1243.087 | 30.777 | 10,483.103 | 3343 |
| 2016 | 1607.520 | 30.545 | 12,043.255 | 3815 |
| 2017 | 1659.885 | 32.815 | 15,359.188 | 4416 |
| 2018 | 1741.988 | 28.528 | 21,563.590 | 4984 |
| 2019 | 1938.192 | 27.826 | 28,753.029 | 5496 |
| r | −0.86 | −0.70 | −0.66 | −0.89 |
| p | <0.001 | <0.001 | <0.01 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhamantayev, O.; Kayupova, G.; Nukeshtayeva, K.; Yerdessov, N.; Bolatova, Z.; Turmukhambetova, A. COVID-19 Pandemic Impact on the Maternal Mortality in Kazakhstan and Comparison with the Countries in Central Asia. Int. J. Environ. Res. Public Health 2023, 20, 2184. https://doi.org/10.3390/ijerph20032184
Zhamantayev O, Kayupova G, Nukeshtayeva K, Yerdessov N, Bolatova Z, Turmukhambetova A. COVID-19 Pandemic Impact on the Maternal Mortality in Kazakhstan and Comparison with the Countries in Central Asia. International Journal of Environmental Research and Public Health. 2023; 20(3):2184. https://doi.org/10.3390/ijerph20032184
Chicago/Turabian StyleZhamantayev, Olzhas, Gaukhar Kayupova, Karina Nukeshtayeva, Nurbek Yerdessov, Zhanerke Bolatova, and Anar Turmukhambetova. 2023. "COVID-19 Pandemic Impact on the Maternal Mortality in Kazakhstan and Comparison with the Countries in Central Asia" International Journal of Environmental Research and Public Health 20, no. 3: 2184. https://doi.org/10.3390/ijerph20032184
APA StyleZhamantayev, O., Kayupova, G., Nukeshtayeva, K., Yerdessov, N., Bolatova, Z., & Turmukhambetova, A. (2023). COVID-19 Pandemic Impact on the Maternal Mortality in Kazakhstan and Comparison with the Countries in Central Asia. International Journal of Environmental Research and Public Health, 20(3), 2184. https://doi.org/10.3390/ijerph20032184






