Fewer Children in Families Associated with Lower Odds of Early Childhood Caries: A Sample from Three Countries
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection
2.3. Data Analysis
3. Results
3.1. Family Demographic Characteristics
3.2. Oral Health Knowledge and Practices
3.3. Child Oral Health Status
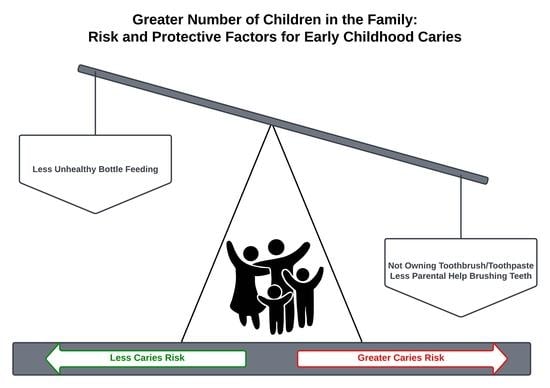
3.4. Association between Number of Children and Early Childhood Caries
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baker, P.; Machado, P.; Santos, T.; Sievert, K.; Backholer, K.; Hadjikakou, M.; Russell, C.; Huse, O.; Bell, C.; Scrinis, G.; et al. Ultra-processed Foods and the Nutrition Transition: Global, Regional and National Trends, Food Systems Transformations and Political Economy Drivers. Obes. Rev. 2020, 21, 13126. [Google Scholar] [CrossRef] [PubMed]
- Kaye, E.A.; Sohn, W.; Garcia, R.I. The Healthy Eating Index and Coronal Dental Caries in US Adults. J. Am. Dent. Assoc. 2020, 151, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Seiler, A.; Chen, M.A.; Brown, R.L.; Fagundes, C.P. Obesity, Dietary Factors, Nutrition, and Breast Cancer Risk. Curr. Breast Cancer Rep. 2018, 10, 14–27. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Sokal-Gutierrez, K.; Chung, K.; Lin, W.; Khanh, L.N.; Chung, R.; Hoang, H.T.; Ivey, S.L. Maternal and Child Nutrition and Oral Health in Urban Vietnam. Int. J. Environ. Res. Public Health 2019, 16, 2579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pham, T.A.V.; Nguyen, P.A. Factors Related to Dental Caries in 10-Year-Old Vietnamese Schoolchildren. Int. Dent. J. 2019, 69, 214–222. [Google Scholar] [CrossRef]
- Nseir, W. Soft Drinks Consumption and Nonalcoholic Fatty Liver Disease. WJG 2010, 16, 2579. [Google Scholar] [CrossRef] [PubMed]
- Panagiotakos, D.B.; Tzima, N.; Pitsavos, C.; Chrysohoou, C.; Papakonstantinou, E.; Zampelas, A.; Stefanadis, C. The Relationship between Dietary Habits, Blood Glucose and Insulin Levels among People without Cardiovascular Disease and Type 2 Diabetes; The ATTICA Study. Rev. Diabetic Stud. 2005, 2, 208. [Google Scholar] [CrossRef] [Green Version]
- Sami, W.; Ansari, T.; Butt, N.S.; Hamid, M.R.A. Effect of Diet on Type 2 Diabetes Mellitus: A Review. Int. J. Health Sci. 2017, 11, 65–71. [Google Scholar]
- Forouzanfar, M.H.; Alexander, L.; Anderson, H.R.; Bachman, V.F.; Biryukov, S.; Brauer, M.; Burnett, R.; Casey, D.; Coates, M.M.; Cohen, A.; et al. Global, Regional, and National Comparative Risk Assessment of 79 Behavioural, Environmental and Occupational, and Metabolic Risks or Clusters of Risks in 188 Countries, 1990–2013: A Systematic Analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar] [CrossRef] [Green Version]
- Pan, A.; Lin, X.; Hemler, E.; Hu, F.B. Diet and Cardiovascular Disease: Advances and Challenges in Population-Based Studies. Cell Metab. 2018, 27, 489–496. [Google Scholar] [CrossRef] [Green Version]
- Petersen, P.E.; Bourgeois, D.; Ogawa, H.; Estupinan-Day, S.; Ndiaye, C. The Global Burden of Oral Diseases and Risks to Oral Health. Bull. World Health Organ. 2005, 83, 661–669. [Google Scholar]
- Vasireddy, D.; Sathiyakumar, T.; Mondal, S.; Sur, S. Socioeconomic Factors Associated With the Risk and Prevalence of Dental Caries and Dental Treatment Trends in Children: A Cross-Sectional Analysis of National Survey of Children’s Health (NSCH) Data, 2016-2019. Cureus 2021, 13, 19184. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.L.; Marcenes, W. Global Burden of Untreated Caries: A Systematic Review and Metaregression. J. Dent. Res. 2015, 94, 650–658. [Google Scholar] [CrossRef] [PubMed]
- Karam, S.A.; Costa, F.D.S.; Peres, K.G.; Peres, M.A.; Barros, F.C.; Bertoldi, A.D.; Santos, I.S.; Tovo, L.; Matijasevich, A.B.; Menezes, A.M.; et al. Two Decades of Socioeconomic Inequalities in the Prevalence of Untreated Dental Caries in Early Childhood: Results from Three Birth Cohorts in Southern Brazil. Comm. Dent. Oral Epid. 2022, cdoe.12747. [Google Scholar] [CrossRef] [PubMed]
- Tinanoff, N.; Baez, R.J.; Diaz Guillory, C.; Donly, K.J.; Feldens, C.A.; McGrath, C.; Phantumvanit, P.; Pitts, N.B.; Seow, W.K.; Sharkov, N.; et al. Early Childhood Caries Epidemiology, Aetiology, Risk Assessment, Societal Burden, Management, Education, and Policy: Global Perspective. Int. J. Paediatr. Dent. 2019, 29, 238–248. [Google Scholar] [CrossRef] [PubMed]
- Phantumvanit, P.; Makino, Y.; Ogawa, H.; Rugg-Gunn, A.; Moynihan, P.; Petersen, P.E.; Evans, W.; Feldens, C.A.; Lo, E.; Khoshnevisan, M.H.; et al. WHO Global Consultation on Public Health Intervention against Early Childhood Caries. Community Dent. Oral Epidemiol. 2018, 46, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Psoter, W.J.; Reid, B.C.; Katz, R.V. Malnutrition and Dental Caries: A Review of the Literature. Caries Res. 2005, 39, 441–447. [Google Scholar] [CrossRef] [Green Version]
- Freire, M.D.C.M.; Corrêa-Faria, P.; Costa, L.R. Effect of Dental Pain and Caries on the Quality of Life of Brazilian Preschool Children. Rev. Saúd. Pública 2018, 52, 30. [Google Scholar] [CrossRef]
- Fisher-Owens, S.A.; Gansky, S.A.; Platt, L.J.; Weintraub, J.A.; Soobader, M.-J.; Bramlett, M.D.; Newacheck, P.W. Influences on Children’s Oral Health: A Conceptual Model. Pediatrics 2007, 120, e510–e520. [Google Scholar] [CrossRef] [Green Version]
- Dabawala, S.; Suprabha, B.S.; Shenoy, R.; Rao, A.; Shah, N. Parenting Style and Oral Health Practices in Early Childhood Caries: A Case-Control Study. Int. J. Paediatr. Dent. 2017, 27, 135–144. [Google Scholar] [CrossRef]
- Dülgergil, Ç.; Dalli, M.; Hamidi, M.; Çolak, H. Early Childhood Caries Update: A Review of Causes, Diagnoses, and Treatments. J. Nat. Sci. Biol. Med. 2013, 4, 29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization Ending Childhood Dental Caries: WHO Implementation Manual; World Health Organization: Geneva, Switzerland, 2020; ISBN 978-92-4-000005-6.
- Rathee, M.; Sapra, A. Dental Caries. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Moye, Z.D.; Zeng, L.; Burne, R.A. Fueling the Caries Process: Carbohydrate Metabolism and Gene Regulation by Streptococcus Mutans. J. Oral Microbiol. 2014, 6, 24878. [Google Scholar] [CrossRef]
- Essalat, M.; Morrison, D.; Kak, S.; Chang, E.J.; Penso, I.R.; Kulchar, R.J.; Padilla, O.H.M.; Shetty, V. A Naturalistic Study of Brushing Patterns Using Powered Toothbrushes. PLoS ONE 2022, 17, e0263638. [Google Scholar] [CrossRef] [PubMed]
- Julihn, A.; Soares, F.C.; Hjern, A.; Dahllöf, G. Socioeconomic Determinants, Maternal Health, and Caries in Young Children. JDR Clin. Transl. Res. 2018, 3, 395–404. [Google Scholar] [CrossRef] [Green Version]
- Arora, A.; Chew, L.; Kang, K.; Tang, L.; Estai, M.; Thepsourinthone, J.; Chandio, N.; Parmar, J.; Doyizode, A.M.; Jain, K.V.; et al. Diet, Nutrition, and Oral Health: What Influences Mother’s Decisions on What to Feed Their Young Children? Int. J. Environ. Res. Public Health 2021, 18, 8159. [Google Scholar] [CrossRef] [PubMed]
- Pierce, A.; Singh, S.; Lee, J.; Grant, C.; Cruz de Jesus, V.; Schroth, R.J. The Burden of Early Childhood Caries in Canadian Children and Associated Risk Factors. Front. Public Health 2019, 7, 328. [Google Scholar] [CrossRef] [Green Version]
- Elwell, K.; Camplain, C.; Kirby, C.; Sanderson, K.; Grover, G.; Morrison, G.; Gelatt, A.; Baldwin, J.A. A Formative Assessment of Social Determinants of Health Related to Early Childhood Caries in Two American Indian Communities. Int. J. Environ. Res. Public Health 2021, 18, 9838. [Google Scholar] [CrossRef]
- Berger, L.M. Income, Family Structure, and Child Maltreatment Risk. Child. Youth Serv. Rev. 2004, 26, 725–748. [Google Scholar] [CrossRef]
- Chen, A.Y.; Escarce, J.J. Family Structure and Childhood Obesity: An Analysis Through 8th Grade. Matern. Child Health J. 2014, 18, 1772–1777. [Google Scholar] [CrossRef]
- Ochiai, H.; Shirasawa, T.; Ohtsu, T.; Nishimura, R.; Morimoto, A.; Obuchi, R.; Hoshino, H.; Tajima, N.; Kokaze, A. Number of Siblings, Birth Order, and Childhood Overweight: A Population-Based Cross-Sectional Study in Japan. BMC Public Health 2012, 12, 766. [Google Scholar] [CrossRef] [Green Version]
- Balderama-guzman, V. Child Health, Nutrition and Family Size: A Comparative Study of Rural and Urban Children. Popul. Data Inf. Serv. 1978, 32–33. [Google Scholar]
- Omariba, D.W.R.; Boyle, M.H. Family Structure and Child Mortality in Sub-Saharan Africa: Cross-National Effects of Polygyny. J. Marriage Fam. 2007, 69, 528–543. [Google Scholar] [CrossRef]
- Hooley, M.; Skouteris, H.; Boganin, C.; Satur, J.; Kilpatrick, N. Parental Influence and the Development of Dental Caries in Children Aged 0–6 Years: A Systematic Review of the Literature. J. Dent. 2012, 40, 873–885. [Google Scholar] [CrossRef]
- Lam, P.P.Y.; Chua, H.; Ekambaram, M.; Lo, E.C.M.; Yiu, C.K.Y. Risk Predictors of Early Childhood Caries Increment--A Systematic Review and Meta-Analysis. J. Evid.-Based Dent. Pract. 2022, 22, 101732. [Google Scholar] [CrossRef]
- Lundborg, P.; Ralsmark, H.; Rooth, D.-O. When a Little Dirt Doesn’t Hurt—The Effect of Family Size on Child Health Outcomes; Linneuniversitetet: Växjö, Sweden, 2013. [Google Scholar]
- Downey, D.B. Number of Siblings and Intellectual Development: The Resource Dilution Explanation. Am. Psychol. 2001, 56, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Sokal-Gutierrez, K.; Turton, B.; Husby, H.; Paz, C.L. Early Childhood Caries and Malnutrition: Baseline and Two-Year Follow-up Results of a Community-Based Prevention Intervention in Rural Ecuador. BMC Nutr. 2016, 2, 73. [Google Scholar] [CrossRef] [Green Version]
- Tsang, C.; Sokal-Gutierrez, K.; Patel, P.; Lewis, B.; Huang, D.; Ronsin, K.; Baral, A.; Bhatta, A.; Khadka, N.; Barkan, H.; et al. Early Childhood Oral Health and Nutrition in Urban and Rural Nepal. Int. J. Environ. Res. Public Health 2019, 16, 2456. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Oral Health Surveys: Basic Methods, 4th ed.; World Health Organization: Geneva, Switzerland, 1997; Available online: https://apps.who.int/iris/handle/10665/41905 (accessed on 21 July 2022).
- He, H.; Zhang, H.; Ye, P.; Tang, W. A Test of Inflated Zeros for Poisson Regression Models. Stat. Methods Med. Res. 2019, 28, 1157–1169. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Patel, A.B.; Bann, C.M.; Garces, A.L.; Krebs, N.F.; Lokangaka, A.; Tshefu, A.; Bose, C.L.; Saleem, S.; Goldenberg, R.L.; Goudar, S.S.; et al. Development of the Global Network for Women’s and Children’s Health Research’s Socioeconomic Status Index for Use in the Network’s Sites in Low and Lower Middle-Income Countries. Reprod. Health 2020, 17, 193. [Google Scholar] [CrossRef]
- Filmer, D.; Pritchett, L.H. Estimating Wealth Effects without Expenditure Data—Or Tears: An Application to Educational Enrollments in States of India. Demography 2001, 38, 115–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sampaio, F.C.; Bönecker, M.; Paiva, S.M.; Martignon, S.; Ricomini Filho, A.P.; Pozos-Guillen, A.; Oliveira, B.H.; Bullen, M.; Naidu, R.; Guarnizo-Herreño, C.; et al. Dental Caries Prevalence, Prospects, and Challenges for Latin America and Caribbean Countries: A Summary and Final Recommendations from a Regional Consensus. Braz. Oral Res. 2021, 35, e056. [Google Scholar] [CrossRef] [PubMed]
- Duangthip, D.; Gao, S.S.; Lo, E.C.M.; Chu, C.H. Early childhood caries among 5- to 6-year-old children in Southeast Asia. Int. Dent. J. 2017, 67, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Northridge, M.E.; Kumar, A.; Kaur, R. Disparities in Access to Oral Health Care. Annu. Rev. Public Health 2020, 41, 513–535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pentapati, K.C.; Yeturu, S.K.; Siddiq, H. Global and Regional Estimates of Dental Pain among Children and Adolescents—Systematic Review and Meta-Analysis. Eur. Arch. Paediatr. Dent 2021, 22, 1–12. [Google Scholar] [CrossRef] [PubMed]
- So, M.; Ellenikiotis, Y.; Husby, H.; Paz, C.; Seymour, B.; Sokal-Gutierrez, K. Early Childhood Dental Caries, Mouth Pain, and Malnutrition in the Ecuadorian Amazon Region. Int. J. Environ. Res. Public Health 2017, 14, 550. [Google Scholar] [CrossRef] [Green Version]
- Sujlana, A.; Pannu, P. Family Related Factors Associated with Caries Prevalence in the Primary Dentition of Five-Year-Old Children. J. Indian Soc. Pedod. Prev. Dent. 2015, 33, 83. [Google Scholar] [CrossRef]
- Folayan, M.; Kolawole, K.; Oziegbe, E.; Oyedele, T.; Agbaje, H.; Onjejaka, N.; Oshomoji, V. Association between Family Structure and Oral Health of Children with Mixed Dentition in Suburban Nigeria. J. Indian Soc. Pedod. Prev. Dent. 2017, 35, 134. [Google Scholar] [CrossRef]
- Oyedele, T.A.; Fadeju, A.D.; Adeyemo, Y.I.; Nzomiwu, C.L.; Ladeji, A.M. Impact of Oral Hygiene and Socio-Demographic Factors on Dental Caries in a Suburban Population in Nigeria. Eur. Arch. Paediatr. Dent. 2018, 19, 155–161. [Google Scholar] [CrossRef]
- Chen, K.J.; Gao, S.S.; Duangthip, D.; Li, S.K.Y.; Lo, E.C.M.; Chu, C.H. Dental Caries Status and Its Associated Factors among 5-Year-Old Hong Kong Children: A Cross-Sectional Study. BMC Oral Health 2017, 17, 121. [Google Scholar] [CrossRef] [Green Version]
- Joshi, D.S.; Lebrun-Harris, L.A. Child Health Status and Health Care Use in Grandparent- Versus Parent-Led Households. Pediatrics 2022, 150, e2021055291. [Google Scholar] [CrossRef] [PubMed]
- Burgette, J.M.; Trivedi, A.V.; Dahl, Z.T.; Weyant, R.J.; McNeil, D.W.; Foxman, B.; Marazita, M.L. Mother’s Experience of Conflict Within Their Family Social Network When Advocating for Children’s Oral Health. Matern. Child Health J. 2023, 27, 151–157. [Google Scholar] [CrossRef]
- World Health Organization. Guideline: Sugars Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Huffman, S.L.; Piwoz, E.G.; Vosti, S.A.; Dewey, K.G. Babies, Soft Drinks and Snacks: A Concern in Low- and Middle-income Countries? Matern. Child Nutr. 2014, 10, 562–574. [Google Scholar] [CrossRef] [PubMed]
- Yousaf, M.; Aslam, T.; Saeed, S.; Sarfraz, A.; Sarfraz, Z.; Cherrez-Ojeda, I. Individual, Family, and Socioeconomic Contributors to Dental Caries in Children from Low- and Middle-Income Countries. Int. J. Environ. Res. Public Health 2022, 19, 7114. [Google Scholar] [CrossRef] [PubMed]
- Karobari, M.I.; Siddharthan, S.; Adil, A.H.; Khan, M.M.; Venugopal, A.; Rokaya, D.; Heboyan, A.; Marya, C.M.; Marya, A. Modifiable and Non-modifiable Risk Factors Affecting Oral and Periodontal Health and Quality of Life in South Asia. Open Dent. J. 2022, 16, e187421062209270. [Google Scholar] [CrossRef]
- Roundtable on Health Literacy; Board on Population Health and Public Health Practice; Institute of Medicine. Oral Health Literacy; Oral Health Literacy Programs; National Academies Press (US): Washington, DC, USA, 2013. Available online: https://www.ncbi.nlm.nih.gov/books/NBK207117/ (accessed on 15 January 2023).
- Susarla, S.M.; Trimble, M.; Sokal-Gutierrez, K. Cross-Sectional Analysis of Oral Healthcare vs. General Healthcare Utilization in Five Low- and Middle-Income Countries. Front. Oral. Health 2022, 3, 911110. [Google Scholar] [CrossRef]
- Kim Seow, W. Environmental, Maternal, and Child Factors Which Contribute to Early Childhood Caries: A Unifying Conceptual Model for Early Childhood Caries. Int. J. Paediatr. Dent. 2012, 22, 157–168. [Google Scholar] [CrossRef]
- Burgette, J.M. Family Resilience and Connection Is Associated with Dental Caries in US Children. JDR Clin. Transl. Res. 2022, 7, 61–70. [Google Scholar] [CrossRef]
- Burgette, J.M.; Polk, D.E.; Shah, N.; Malik, A.; Crout, R.J.; Mcneil, D.W.; Foxman, B.; Weyant, R.J.; Marazita, M.L. Mother’s Perceived Social Support and Children’s Dental Caries in Northern Appalachia. Pediatr. Dent. 2019, 41, 200–205. [Google Scholar]
- Peres, M.A.; Macpherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral Diseases: A Global Public Health Challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- WHO Expert Consultation on Public Health Intervention against Early Childhood Caries: Report of a Meeting, Bangkok, Thailand, 26–28 January 2016. Available online: https://apps.who.int/iris/handle/10665/255627 (accessed on 26 December 2022).
- Follow-Up to the Political Declaration of the Third High-Level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Disease. Available online: https://apps.who.int/gb/ebwha/pdf_files/wha75/A75_10Add1-En.Pdf (accessed on 26 December 2022).
- Delivering Optimal Oral Health for All. Available online: https://www.fdiworlddental.org/sites/default/files/2021-02/Vision-2030-Delivering%20Optimal-Oral-Health-for-All_0.Pdf (accessed on 26 December 2022).

| Characteristics | Total N = 1352 Children/ Mothers a | Ecuador N = 290 Children/ Mothers a | Nepal N = 469 Children/ Mothers a | Vietnam N = 593 Children/ Mothers a | One Child N = 496 Children/ Mothers a | Multiple Children N = 851 Children/ Mothers a | Difference between One Child and Multiple Children (p-Value) b |
|---|---|---|---|---|---|---|---|
| Site Type | Urban: 51.7% Rural: 48.3% | Rural: 100% | Urban: 69.7% Rural: 30.3% | Urban: 100% | Urban: 83.1% Rural: 16.9% | Urban: 57.9% Rural: 43.0% | <0.001 |
| Children | |||||||
| Age (years) | 3.7 ± 1.5 | 3.8 ± 1.8 | 3.7 ± 1.7 | 3.6 ± 1.0 | 3.2 ± 1.4 | 4.0 ± 1.4 | <0.001 |
| Sex (Male/Female) | 52.7%/47.3% | 54.8%/45.2% | 53.2%/46.8% | 51.2%/48.8% | 55.9%/44.1% | 50.2%/49.8% | 0.076 |
| Mothers and Households | |||||||
| Age (years) | 30.9 ± 6.4 | 30.4 ± 8.4 | 28.6 ± 5.4 | 33.0 ± 5.1 | 28.7 ± 5.7 | 32.2 ± 6.4 | <0.001 |
| Education (years) | 8.7 ± 5.5 | 7.1 ± 4.8 | 5.1 ± 4.4 | 12.8 ± 3.7 | 10.9 ± 4.8 | 7.4 ± 5.5 | <0.001 |
| Number of Children | 2.2 ± 1.6 | 3.7 ± 2.4 | 2.2 ± 1.1 | 1.6 ± 0.7 | 1.0 ± 0.0 | 2.9 ± 1.6 | <0.001 |
| Range of Number of Children | 1–12 | 1–12 | 1–7 | 1–5 | 1 | 2–12 | |
| Number in Household | 5.3 ± 2.3 | 7.0 ± 2.9 | 5.1 ± 2.0 | 4.5 ± 1.7 | 4.6 ± 2.2 | 5.7 ± 2.3 | <0.001 |
| Potable Water at Home | 79.3% | 32.1% | 85.5% | 98.6% | 89.1% | 73.6% | <0.001 |
| Electricity | 98.0% | 87.6% | 98.5% | 99.5% | 98.6% | 95.4% | <0.001 |
| Cooking Fuel Other Than Wood (Gas or Electric) | 84.1% | 86.9% | 63.7% | 98.8% | 92.5% | 79.0% | 0.019 |
| Time to walk from home to a store that sells junk food: | |||||||
| Less than 5 min | 84.7% | 64.4% | 78.9% | 82.3% | 85.1% | 73.3% | <0.001 |
| 6–20 min | 16.4% | 23.4% | 13.9% | 15.5% | 12.8% | 23.5% | <0.001 |
| Over 20 min | 5.9% | 12.1% | 8.1% | 2.2% | 2.1% | 3.2% | 0.221 |
| Characteristics | Total N = 1352 Children/ Mothers a | Ecuador N = 290 Children/ Mothers a | Nepal N = 469 Children/ Mothers a | Vietnam N = 593 Children/ Mothers a | One Child N = 496 Children/ Mothers a | Multiple Children N = 851 Children/ Mothers a | Difference between One Child and Multiple Children (p-Value) b |
|---|---|---|---|---|---|---|---|
| Mother’s knowledge of the causes of childhood caries c | |||||||
| Don’t know | 15.1% | 14.8% | 10.9% | 20.0% | 14.7% | 15.4% | <0.001 |
| Eating sweets | 73.6% | 66.2% | 85.3% | 66.8% | 73.8% | 73.5% | 0.891 |
| Not brushing teeth | 26.4% | 44.8% | 27.7% | 16.4% | 24.4% | 27.6% | 0.196 |
| Drinking soda/juice | 3.8% | 6.6% | 5.3% | 1.2% | 3.6% | 3.9% | 0.768 |
| Using the baby bottle | 0.9% | 3.8% | 0.2% | 0.0% | 0.2% | 1.3% | 0.040 |
| Mother’s knowledge of the complications of childhood caries c | |||||||
| Don’t know | 5.5% | 11.4% | 7.2% | 0.2% | 3.8% | 6.5% | 0.046 |
| Pain | 56.0% | 62.8% | 76.8% | 31.1% | 49.3% | 59.9% | <0.001 |
| Difficulty eating | 40.9% | 27.9% | 45.0% | 44.9% | 41.9% | 40.4% | 0.591 |
| Difficulty sleeping | 14.6% | 19.3% | 17.5% | 8.9% | 15.2% | 16.1% | 0.056 |
| Harm their health | 22.3% | 13.1% | 8.7% | 41.3% | 26.7% | 19.7% | 0.004 |
| Child Nutrition Practices | |||||||
| Child breastfed | 97.3% | 97.5% | 98.7% | 96.0% | 96.1% | 98.1% | 0.020 |
| Mean duration of breastfeeding (months) | 18.3 ± 12.2 | 17.7 ± 8.2 | 22.5 ± 16.0 | 14.9 ± 8.4 | 19.0 ± 12.1 | 22.5 ± 13.5 | <0.001 |
| Child bottle fed (mixed breast- and bottle feeding) | 52.8% | 40.1% | 19.0% | 86.1% | 64.2% | 46.0% | <0.001 |
| Mean duration of bottle feeding (months) | 27.5 ± 15.2 | 21.2 ± 15.2 | 20.3 ± 14.4 | 30.1 ± 14.5 | 29.4 ± 15.1 | 27.6 ± 15.0 | 0.014 |
| Unhealthy bottle feeding practices | 44.6% | 35.6% | 13.2% | 74.3% | 54.6% | 38.6% | <0.001 |
| Bottle fed with sugary liquid | 29.4% | 31.7% | 1.9% | 62.3% | 35.8% | 25.8% | <0.001 |
| Bottle fed while sleeping | 14.6% | 12.0% | 7.1% | 22.1% | 16.2% | 13.5% | 0.184 |
| Bottle fed past 24 months of age | 34.3% | 18.7% | 8.3% | 62.8% | 43.6% | 28.7% | <0.001 |
| Daily consumption of milk | 67.2% | 20.8% | 69.9% | 91.0% | 79.7% | 60.1% | <0.001 |
| Daily consumption of soda | 6.1% | 7.8% | 5.0% | 5.9% | 6.3% | 6.0% | 0.847 |
| Daily consumption of candy/sweets | 29.9% | 21.8% | 53.4% | 12.9% | 26.0% | 32.2% | 0.024 |
| Daily consumption of chips/biscuits | 17.6% | 15.9% | 25.6% | 11.6% | 17.6% | 17.7% | 0.954 |
| Daily consumption of any junk food or sugary drink | 34.6% | 28.9% | 56.0% | 18.2% | 36.5% | 40.4% | 0.048 |
| Mother calms fussy child with sweets | 13.8% | 9.7% | 27.5% | 1.8% | 11.3% | 15.2% | 0.058 |
| Mother restricts candy | 6.9% | 7.9% | 13.6% | 1.0% | 6.0% | 7.4% | 0.333 |
| Child Oral Health Practices | |||||||
| Child has own toothbrush | 88.2% | 90.8% | 75.7% | 97.0% | 88.4% | 88.0% | 0.810 |
| Child has toothpaste | 90.4% | 84.4% | 89.6% | 94.1% | 91.9% | 89.6% | 0.169 |
| Mother helps with brushing frequently/almost always | 54.6% | 54.0% | 24.5% | 80.0% | 64.2% | 48.9% | <0.001 |
| Mother never/occasionally helps with brushing | 45.4% | 46.0% | 75.5% | 20.0% | 35.8% | 51.1% | <0.001 |
| Mother does nothing to care for child’s teeth | 6.4% | 7.6% | 12.6% | 0.2% | 5.3% | 7.1% | 0.223 |
| Child has visited the dentist | 38.1% | 74.0% | 9.7% | 44.5% | 30.9% | 42.0% | <0.001 |
| Characteristics | Total N = 1352 Children/ Mothers a | Ecuador N = 290 Children/ Mothers a | Nepal N = 469 Children/ Mothers a | Vietnam N = 593 Children/ Mothers a | One Child N = 496 Children/ Mothers a | Multiple Children N = 851 Children/ Mothers a | Difference between One Child and Multiple Children (p-Value) b |
|---|---|---|---|---|---|---|---|
| Child Tooth Decay | |||||||
| Child has any decayed, missing or filled teeth (dmft) | 72.3% | 86.9% | 59.9% | 75.0% | 64.1% | 77.2% | <0.001 |
| Range in number of dmft | 0–24 | 0–24 | 0–17 | 0–23 | 0–20 | 0–24 | |
| Mean dmft | 5.4 ± 5.3 | 8.3 ± 5.4 | 3.1 ± 3.8 | 5.9 ± 5.4 | 4.4 ± 4.9 | 6.0 ± 5.4 | <0.001 |
| Mean # dmft for children with caries | 7.5 ± 4.8 | 9.6 ± 4.6 | 5.2 ± 3.6 | 7.8 ± 4.9 | 6.9 ± 4.5 | 7.8 ± 4.9 | 0.003 |
| Prevalence of deep decay, in or near pulp | 28.5% | 39.7% | 20.7% | 31.2% | 16.9% | 28.0% | <0.001 |
| Child Mouth Pain | |||||||
| Any mouth pain (occasionally/frequently/always) | 51.2% | 47.2% | 27.5% | 71.8% | 52.4% | 50.4% | 0.023 |
| Mouth pain (frequently/always) | 22.9% | 18.1% | 5.5% | 39.0% | 26.9% | 20.4% | 0.617 |
| Mother’s Overall Assessment of Child’s Health | |||||||
| Mother’s assessment of child’s oral health as “bad” | 17.4% | 13.8% | 21.9% | 15.5% | 15.1% | 18.8% | 0.089 |
| Mother’s assessment of child’s overall health as “bad” | 2.9% | 3.9% | 3.2% | 2.1% | 2.3% | 3.1% | 0.365 |
| Logistic Regression Analysis | ||||
|---|---|---|---|---|
| Oral Health Practices | Unadjusted Odds Ratio (OR) (95% Confidence Interval) | Adjusted Odds Ratio (aOR) a (95% Confidence Interval) | Significance of aOR p-Value | |
| Nutrition practices | ||||
| Unhealthy baby bottle feeding | 0.75 (0.69–0.82) | 0.85 (0.77–0.93) | 0.0009 | |
| Daily consumption of junk food | 0.97 (0.90–1.04) | 1.00 (0.92–1.09) | 0.96 | |
| Calms child with sweets | 1.04 (0.94–1.13) | 0.99 (0.88–1.11) | 0.93 | |
| Mother restricts candy | 1.08 (0.96–1.21) | 1.03 (0.89–1.18) | 0.65 | |
| Oral Hygiene Practices | ||||
| Child has own toothbrush | 0.90 (0.82–0.99) | 0.89 (0.80–0.99) | 0.031 | |
| Child has toothpaste | 0.80 (0.74–0.88) | 0.83 (0.75–0.93) | 0.0007 | |
| Mother helps child brush | 0.78 (0.72–0.85) | 0.86 (0.79–0.94) | 0.001 | |
| Child has been to the dentist | 1.33 (1.23–1.45) | 1.19 (1.09–1.30) | 0.0001 | |
| Child Caries Experience | ||||
| Child has any decayed, missing or filled teeth (dmft) | 1.36 (1.22–1.52) | 1.18 (1.06–1.32) | 0.005 | |
| Zero-Inflated Poisson (ZIP) Regression Analysis | ||||
| Oral Health Outcome | Count Model Estimate b,d (95% CI) | Count Model p-value | Inflation Model Estimate c,d (95% CI) | Inflation Model p-value |
| Number of decayed, missing and filled teeth (dmft) | 1.04 (1.01–1.06) | <0.0001 | 0.85 (0.76–0.94) | 0.005 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, A.H.; Kulchar, R.J.; Susarla, S.M.; Turton, B.; Sokal-Gutierrez, K. Fewer Children in Families Associated with Lower Odds of Early Childhood Caries: A Sample from Three Countries. Int. J. Environ. Res. Public Health 2023, 20, 2195. https://doi.org/10.3390/ijerph20032195
Park AH, Kulchar RJ, Susarla SM, Turton B, Sokal-Gutierrez K. Fewer Children in Families Associated with Lower Odds of Early Childhood Caries: A Sample from Three Countries. International Journal of Environmental Research and Public Health. 2023; 20(3):2195. https://doi.org/10.3390/ijerph20032195
Chicago/Turabian StylePark, Amy H., Rachel J. Kulchar, Sita Manasa Susarla, Bathsheba Turton, and Karen Sokal-Gutierrez. 2023. "Fewer Children in Families Associated with Lower Odds of Early Childhood Caries: A Sample from Three Countries" International Journal of Environmental Research and Public Health 20, no. 3: 2195. https://doi.org/10.3390/ijerph20032195