Comparison of Functional Outcomes between Supervised Rehabilitation and Telerehabilitation in Female Patients with Patellofemoral Pain Syndrome during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Isokinetic Knee Muscle Strength and Muscle Activation Time
2.3. Isometric Hip Muscle Strength
2.4. Patient-Reported Outcomes
2.5. Conservative Rehabilitation Protocol and Interventions
2.6. Statistical Analysis
3. Results
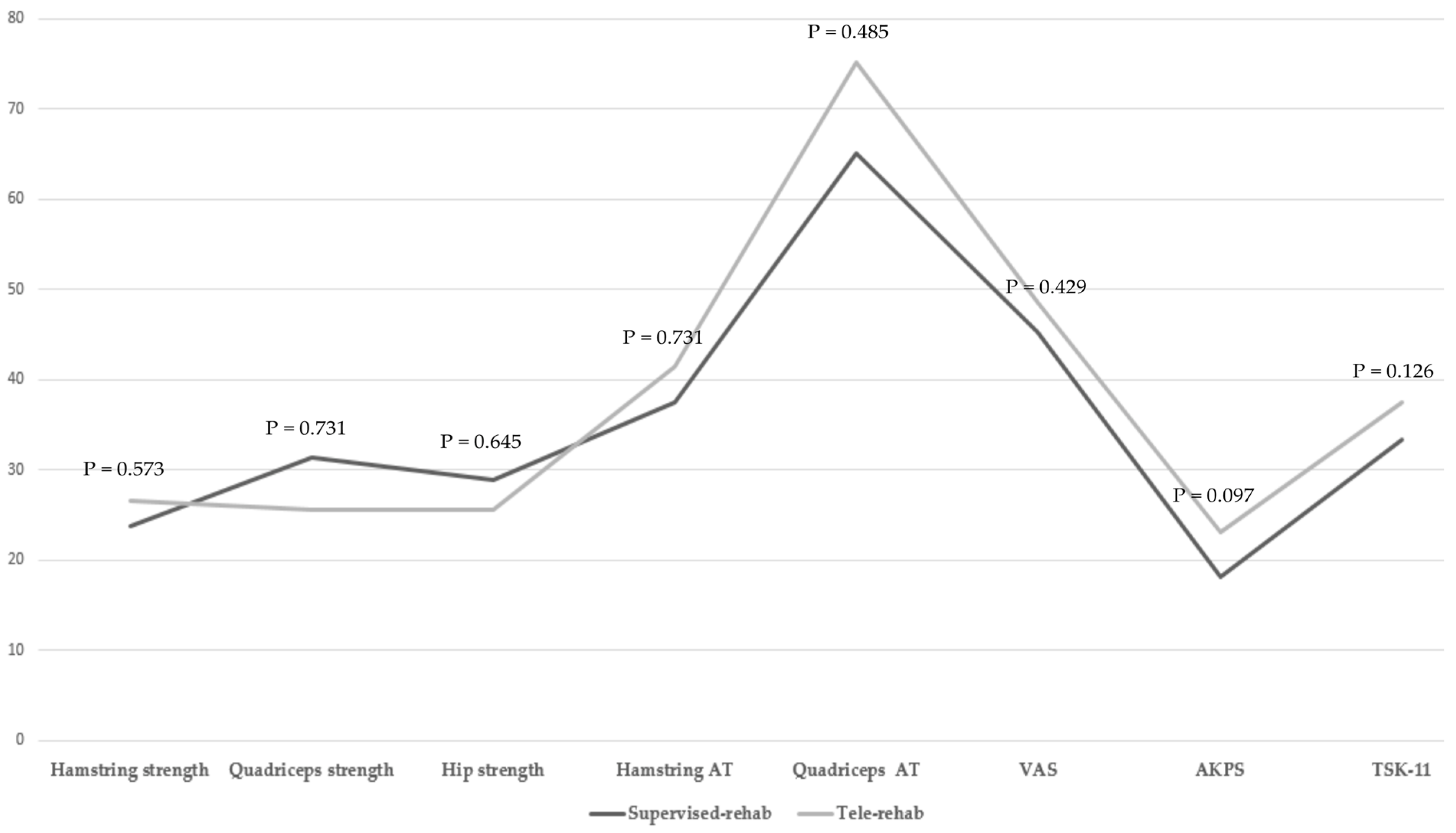
3.1. Comparison of Muscle Strength and Muscle Activation Time between the Two Groups
3.2. Comparison of Patient-Reported Outcomes between the Two Groups
3.3. Comparison of Muscle Strength, Muscle Activation Time, and Patient-Reported Outcomes in Each Group
3.4. Correlations between Adherence Rate and Rate of Change in Muscle Strength, Muscle Activation Time, and Patient-Reported Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Witvrouw, E.; Werner, S.; Mikkelsen, C.; Van Tiggelen, D.; Vanden Berghe, L.; Cerulli, G. Clinical classification of patellofemoral pain syndrome: Guidelines for non-operative treatment. Knee Surg. Sport. Traumatol. Arthrosc. 2005, 13, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Neal, B.S.; Lack, S.D.; Lankhorst, N.E.; Raye, A.; Morrissey, D.; van Middelkoop, M. Risk factors for patellofemoral pain: A systematic review and meta-analysis. Br. J. Sport. Med. 2019, 53, 270–281. [Google Scholar] [CrossRef] [Green Version]
- Aminaka, N.; Pietrosimone, B.G.; Armstrong, C.W.; Meszaros, A.; Gribble, P.A. Patellofemoral pain syndrome alters neuromuscular control and kinetics during stair ambulation. J. Electromyogr. Kinesiol. 2011, 21, 645–651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Richmond, S.A.; Kang, J.; Doyle-Baker, P.K.; Nettel-Aguirre, A.; Emery, C.A. A school-based injury prevention program to reduce sport injury risk and improve healthy outcomes in youth: A pilot cluster-randomized controlled trial. Clin. J. Sport Med. 2016, 26, 291–298. [Google Scholar] [CrossRef] [PubMed]
- van der Heijden, R.A.; Lankhorst, N.E.; van Linschoten, R.; Bierma-Zeinstra, S.M.; van Middelkoop, M. Exercise for treating patellofemoral pain syndrome. Cochrane Database Syst. Rev. 2015, 1, Cd010387. [Google Scholar] [CrossRef]
- Young, J.L.; Snodgrass, S.J.; Cleland, J.A.; Rhon, D.I. Usual medical care for patellofemoral pain does not usually involve much care: 2-year follow-up in the military health system. J. Orthop. Sport. Phys. Ther. 2021, 51, 305–313. [Google Scholar] [CrossRef]
- Holden, M.K.; Dyar, T.A.; Schwamm, L.; Bizzi, E.J.P.T. Virtual-environment-based telerehabilitation in patients with stroke. Presence Teleoperat. Virtual Environ. 2005, 14, 214–233. [Google Scholar] [CrossRef]
- Reinkensmeyer, D.J.; Pang, C.T.; Nessler, J.A.; Painter, C.C. Web-based telerehabilitation for the upper extremity after stroke. IEEE Trans. Neural Syst. Rehabil. Eng. 2002, 10, 102–108. [Google Scholar] [CrossRef]
- Nelson, M.; Bourke, M.; Crossley, K.; Russell, T. Telerehabilitation versus traditional care following total hip replacement: A randomized controlled trial protocol. JMIR Res. Protoc. 2017, 6, e34. [Google Scholar] [CrossRef]
- Castro-Sanchez, A.M.; Matarán-Peñarrocha, G.A.; Gómez-García, S.; García-López, H.; Andronis, L.; Albornoz-Cabello, M.; Palomo, I.C.L. Study protocol randomised controlled trial comparison of cost-utility and cost-effectiveness of a face-to-face rehabilitation programme versus a telemedicine programme in the treatment of patients with chronic low back pain. BMJ Open 2020, 10, e040633. [Google Scholar] [CrossRef]
- Albornoz-Cabello, M.; Barrios-Quinta, C.J.; Barrios-Quinta, A.M.; Escobio-Prieto, I.; Cardero-Durán, M.L.A.; Espejo-Antunez, L. Effectiveness of tele-prescription of therapeutic physical exercise in patellofemoral pain syndrome during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 1048. [Google Scholar] [CrossRef]
- Azma, K.; RezaSoltani, Z.; Rezaeimoghaddam, F.; Dadarkhah, A.; Mohsenolhosseini, S. Efficacy of tele-rehabilitation compared with office-based physical therapy in patients with knee osteoarthritis: A randomized clinical trial. J. Telemed. Telecare 2018, 24, 560–565. [Google Scholar] [CrossRef]
- Kampshoff, C.S.; van Mechelen, W.; Schep, G.; Nijziel, M.R.; Witlox, L.; Bosman, L.; Chinapaw, M.J.; Brug, J.; Buffart, L.M. Participation in and adherence to physical exercise after completion of primary cancer treatment. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 100. [Google Scholar] [CrossRef] [Green Version]
- Hawley-Hague, H.; Horne, M.; Skelton, D.A.; Todd, C. Review of how we should define (and measure) adherence in studies examining older adults’ participation in exercise classes. BMJ Open 2016, 6, e011560. [Google Scholar] [CrossRef] [Green Version]
- Lund, L.W.; Ammitzbøll, G.; Hansen, D.G.; Andersen, E.A.W.; Dalton, S.O. Adherence to a long-term progressive resistance training program, combining supervised and home-based exercise for breast cancer patients during adjuvant treatment. Acta Oncol. 2019, 58, 650–657. [Google Scholar] [CrossRef]
- Emamvirdi, M.; Letafatkar, A.; Khaleghi Tazji, M. The effect of valgus control instruction exercises on pain, strength, and functionality in active females with patellofemoral pain syndrome. Sport. Health 2019, 11, 223–237. [Google Scholar] [CrossRef]
- Foroughi, F.; Sobhani, S.; Yoosefinejad, A.K.; Motealleh, A. Added value of isolated core postural control training on knee pain and function in women with patellofemoral pain syndrome: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2019, 100, 220–229. [Google Scholar] [CrossRef]
- Lee, J.H.; Jang, K.M.; Kim, E.; Rhim, H.C.; Kim, H.D. Static and dynamic quadriceps stretching exercises in patients with patellofemoral pain: A randomized controlled trial. Sport. Health 2021, 13, 482–489. [Google Scholar] [CrossRef]
- Lee, J.H.; Jang, K.M.; Kim, E.; Rhim, H.C.; Kim, H.D. Effects of static and dynamic stretching with strengthening exercises in patients with patellofemoral pain who have inflexible hamstrings: A randomized controlled trial. Sport. Health 2021, 13, 49–56. [Google Scholar] [CrossRef]
- van Cingel, R.E.; Kleinrensink, G.; Uitterlinden, E.J.; Rooijens, P.P.; Mulder, P.G.; Aufdemkampe, G.; Stoeckart, R. Repeated ankle sprains and delayed neuromuscular response: Acceleration time parameters. J. Orthop. Sport. Phys. Ther. 2006, 36, 72–79. [Google Scholar] [CrossRef]
- Heilman, A.E.; Braly, W.G.; Bishop, J.O.; Noble, P.C.; Tullos, H.S. An anatomic study of subtalar instability. Foot Ankle 1990, 10, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Riemann, B.L.; Lephart, S.M. The sensorimotor system, part i: The physiologic basis of functional joint stability. J. Athl. Train. 2002, 37, 71–79. [Google Scholar] [PubMed]
- Almeida, G.P.L.; das Neves Rodrigues, H.L.; de Freitas, B.W.; de Paula Lima, P.O. Reliability and validity of the hip stability isometric test (hipsit): A new method to assess hip posterolateral muscle strength. J. Orthop. Sport. Phys. Ther. 2017, 47, 906–913. [Google Scholar] [CrossRef] [PubMed]
- Rathleff, M.S.; Rathleff, C.R.; Crossley, K.M.; Barton, C.J. Is hip strength a risk factor for patellofemoral pain? A systematic review and meta-analysis. Br. J. Sport. Med. 2014, 48, 1088. [Google Scholar] [CrossRef]
- Mentiplay, B.F.; Perraton, L.G.; Bower, K.J.; Adair, B.; Pua, Y.H.; Williams, G.P.; McGaw, R.; Clark, R.A. Assessment of lower limb muscle strength and power using hand-held and fixed dynamometry: A reliability and validity study. PLoS ONE 2015, 10, e0140822. [Google Scholar] [CrossRef] [Green Version]
- Crossley, K.M.; Bennell, K.L.; Cowan, S.M.; Green, S. Analysis of outcome measures for persons with patellofemoral pain: Which are reliable and valid? Arch. Phys. Med. Rehabil. 2004, 85, 815–822. [Google Scholar] [CrossRef]
- Crombez, G.; Vlaeyen, J.W.; Heuts, P.H.; Lysens, R. Pain-related fear is more disabling than pain itself: Evidence on the role of pain-related fear in chronic back pain disability. Pain 1999, 80, 329–339. [Google Scholar] [CrossRef]
- Woby, S.R.; Roach, N.K.; Urmston, M.; Watson, P.J. Psychometric properties of the tsk-11: A shortened version of the tampa scale for kinesiophobia. Pain 2005, 117, 137–144. [Google Scholar] [CrossRef]
- Larsson, C.; Hansson, E.E.; Sundquist, K.; Jakobsson, U. Psychometric properties of the tampa scale of kinesiophobia (tsk-11) among older people with chronic pain. Physiother. Theory Pract. 2014, 30, 421–428. [Google Scholar] [CrossRef]
- Ferber, R.; Bolgla, L.; Earl-Boehm, J.E.; Emery, C.; Hamstra-Wright, K. Strengthening of the hip and core versus knee muscles for the treatment of patellofemoral pain: A multicenter randomized controlled trial. J. Athl. Train. 2015, 50, 366–377. [Google Scholar] [CrossRef] [Green Version]
- Hanson, E.D.; Carver, J.L.; Lucas, A.; Bass, M.; Alzer, M.; Whang, Y.; Harrison, M.; Milowsky, M.I.; Bitting, R.L.; Battaglini, C.L.J.M.; et al. High adherence to home-based exercise improves muscle strength and cardiorespiratory fitness with advanced prostate cancer: 74 board# 5 may 29 9:30 am-11:30 am. Med. Sci. Sport. Exerc. 2019, 51, 6–7. [Google Scholar]
- Lowe, D.A.; Alway, S.E. Animal models for inducing muscle hypertrophy: Are they relevant for clinical applications in humans? J. Orthop. Sport. Phys. Ther. 2002, 32, 36–43. [Google Scholar] [CrossRef]
- Mithal, A.; Bonjour, J.P.; Boonen, S.; Burckhardt, P.; Degens, H.; El Hajj Fuleihan, G.; Josse, R.; Lips, P.; Morales Torres, J.; Rizzoli, R.; et al. Impact of nutrition on muscle mass, strength, and performance in older adults. Osteoporos. Int. 2013, 24, 1555–1566. [Google Scholar] [CrossRef]
- Sacomori, C.; Berghmans, B.; Mesters, I.; de Bie, R.; Cardoso, F.L. Strategies to enhance self-efficacy and adherence to home-based pelvic floor muscle exercises did not improve adherence in women with urinary incontinence: A randomised trial. J. Physiother. 2015, 61, 190–198. [Google Scholar] [CrossRef] [Green Version]
- Suchomel, T.J.; Nimphius, S.; Bellon, C.R.; Stone, M.H. The importance of muscular strength: Training considerations. Sport. Med. 2018, 48, 765–785. [Google Scholar] [CrossRef]
- De Geest, S.; Sabaté, E. Adherence to long-term therapies: Evidence for action. Eur. J. Cardiovasc. Nurs. 2003, 2, 323. [Google Scholar] [CrossRef]
- Witlox, L.; Velthuis, M.J.; Boer, J.H.; Steins Bisschop, C.N.; Wall, E.V.; Meulen, W.; Schröder, C.D.; Peeters, P.H.M.; May, A.M. Attendance and compliance with an exercise program during localized breast cancer treatment in a randomized controlled trial: The pact study. PLoS ONE 2019, 14, e0215517. [Google Scholar] [CrossRef]
- Herda, T.J.; Cramer, J.T.; Ryan, E.D.; McHugh, M.P.; Stout, J.R. Acute effects of static versus dynamic stretching on isometric peak torque, electromyography, and mechanomyography of the biceps femoris muscle. J. Strength Cond. Res. 2008, 22, 809–817. [Google Scholar] [CrossRef]
- Hedayatpour, N.; Falla, D. Physiological and neural adaptations to eccentric exercise: Mechanisms and considerations for training. Biomed. Res. Int. 2015, 2015, 193741. [Google Scholar] [CrossRef] [Green Version]
- McHugh, M.P.; Tyler, T.F.; Greenberg, S.C.; Gleim, G.W. Differences in activation patterns between eccentric and concentric quadriceps contractions. J. Sport. Sci. 2002, 20, 83–91. [Google Scholar] [CrossRef]
- Lepley, L.K.; Lepley, A.S.; Onate, J.A.; Grooms, D.R. Eccentric exercise to enhance neuromuscular control. Sport. Health 2017, 9, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Riemann, B.L.; Lephart, S.M. The sensorimotor system, part ii: The role of proprioception in motor control and functional joint stability. J. Athl. Train. 2002, 37, 80–84. [Google Scholar] [PubMed]
- Semmler, J.G. Motor unit synchronization and neuromuscular performance. Exerc. Sport Sci. Rev. 2002, 30, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Rabelo, N.D.; Lima, B.; Reis, A.C.; Bley, A.S.; Yi, L.C.; Fukuda, T.Y.; Costa, L.O.; Lucareli, P.R. Neuromuscular training and muscle strengthening in patients with patellofemoral pain syndrome: A protocol of randomized controlled trial. BMC Musculoskelet. Disord. 2014, 15, 157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zech, A.; Hübscher, M.; Vogt, L.; Banzer, W.; Hänsel, F.; Pfeifer, K. Neuromuscular training for rehabilitation of sports injuries: A systematic review. Med. Sci. Sport. Exerc. 2009, 41, 1831–1841. [Google Scholar] [CrossRef] [Green Version]
- Nicolson, P.J.A.; Bennell, K.L.; Dobson, F.L.; Van Ginckel, A.; Holden, M.A.; Hinman, R.S. Interventions to increase adherence to therapeutic exercise in older adults with low back pain and/or hip/knee osteoarthritis: A systematic review and meta-analysis. Br. J. Sport. Med. 2017, 51, 791–799. [Google Scholar] [CrossRef]
- Heuts, P.H.; Vlaeyen, J.W.; Roelofs, J.; de Bie, R.A.; Aretz, K.; van Weel, C.; van Schayck, O.C. Pain-related fear and daily functioning in patients with osteoarthritis. Pain 2004, 110, 228–235. [Google Scholar] [CrossRef]
- Vlaeyen, J.W.S.; Linton, S.J. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain 2000, 85, 317–332. [Google Scholar] [CrossRef] [Green Version]
- Asmundson, G.J.; Taylor, S. Role of anxiety sensitivity in pain-related fear and avoidance. J. Behav. Med. 1996, 19, 577–586. [Google Scholar] [CrossRef]
- Bennie, J.A.; Teychenne, M.J.; De Cocker, K.; Biddle, S.J.H. Associations between aerobic and muscle-strengthening exercise with depressive symptom severity among 17,839 U.S. Adults. Prev. Med. 2019, 121, 121–127. [Google Scholar] [CrossRef]
- Rhim, H.C.; Lee, S.J.; Jeon, J.S.; Kim, G.; Lee, K.Y.; Lee, J.H.; Jang, K.M. Effectiveness of modeling videos on psychological responses of patients following anterior cruciate ligament reconstruction: A pilot randomized trial. Medicine 2020, 99, e23158. [Google Scholar] [CrossRef]
- Baldon Rde, M.; Serrão, F.V.; Scattone Silva, R.; Piva, S.R. Effects of functional stabilization training on pain, function, and lower extremity biomechanics in women with patellofemoral pain: A randomized clinical trial. J. Orthop. Sport. Phys. Ther. 2014, 44, 240–251. [Google Scholar] [CrossRef]

| Supervised-Rehab Group (n = 30) | Tele-Rehab Group (n = 31) | p-Value | |
|---|---|---|---|
| Sex (male/female) | 0/30 | 0/31 | |
| Age (years) | 27.0 ± 2.39 | 26.96 ± 5.99 | 0.753 |
| Height (cm) | 160.49 ± 4.83 | 159.88 ± 6.11 | 0.670 |
| Weight (kg) | 56.64 ± 7.67 | 56.51 ± 11.56 | 0.788 |
| Body mass index (BMI, kg/m2) | 21.92 ± 2.76 | 22.04 ± 3.62 | 0.448 |
| Pain duration (month) | 26.14 ± 15.94 | 27.45 ± 22.46 | 0.753 |
| Tegner activity scale | 4.32 ± 0.82 | 4.25 ± 1.40 | 0.484 |
| Adherence rate (%) | 98.8 ± 0.3 | 98.5 ± 0.3 | 0.689 |
| Injured side (right/left) | 15/15 | 16/15 | |
| Leg dominance | 27/3 | 27/4 |
| Supervised-Rehab Group | Tele-Rehab Group | MD (95% CI) | Effect Size | p-Value | ||
|---|---|---|---|---|---|---|
| Hamstring strength | Pre-intervention | 71.6 ± 18.8 | 75.3 ± 19.8 | −3.7 (−13.5 to 6.2) | −0.191 | 0.467 |
| Post-intervention | 87.3 ± 19.2 | 93.2 ± 20.4 | −5.9 (−16.1 to 4.2) | −0.297 | 0.251 | |
| MD (95% CI) | −15.6 (−18.6 to −12.7) | −17.9 (−22.3 to −13.6) | ||||
| Effect size | −0.826 | −0.890 | ||||
| p-value | 0.001 * | 0.001 * | ||||
| Quadriceps strength | Pre-intervention | 146.6 ± 42.9 | 139.6 ± 41.2 | 7.0 (−4.4 to 28.6) | 0.166 | 0.318 |
| Post-intervention | 189.5 ± 48.9 | 174.7 ± 40.2 | 14.8 (−8.0 to 37.7) | 0.330 | 0.200 | |
| MD (95% CI) | −42.8 (−51.4 to −34.2) | −45.1 (−63.31 to −26.9) | ||||
| Effect size | −0.932 | −0.862 | ||||
| p-value | 0.001 * | 0.001 * | ||||
| Hip strength | Pre-intervention | 0.5 ± 0.1 | 0.5 ± 0.1 | 0 (−0.1 to 0) | 0 | 0.471 |
| Post-intervention | 0.7 ± 0.1 | 0.7 ± 0.1 | 0 (−0.1 to 0) | 0 | 0.700 | |
| MD (95% CI) | −0.1 (−0.1 to 0) | −0.1 (−0.1 to 0) | ||||
| Effect size | −1.999 | −1.999 | ||||
| p-value | 0.001 * | 0.001 * | ||||
| Hamstring AT | Pre-intervention | 93.3 ± 21.3 | 88.3 ± 18.2 | 5.0 (−5.2 to 15.1) | 0.252 | 0.335 |
| Post-intervention | 72.6 ± 20.1 | 66.4 ± 19.9 | 6.2 (−4.0 to 16.4) | 0.309 | 0.231 | |
| MD (95% CI) | 20.6 (10.4 to 30.9) | 21.9 (15.5 to 28.3) | ||||
| Effect size | 0.999 | 1.148 | ||||
| p-value | 0.001 * | 0.001 * | ||||
| Quadriceps AT | Pre-intervention | 99.3 ± 25.7 | 92.9 ± 24.9 | 6.4 (−6.5 to 19.4) | 0.252 | 0.325 |
| Post-intervention | 64.0 ± 19.0 | 56.4 ± 18.5 | 7.6 (−2.0 to 17.1) | 0.405 | 0.122 | |
| MD (95% CI) | 35.3 (26.4 to 44.1) | 36.4 (28.0 to 44.8) | ||||
| Effect size | 1.561 | 1.664 | ||||
| p-value | 0.001 * | 0.001 * |
| Supervised-Rehab Group | Tele-Rehab Group | MD (95% CI) | Effect Size | p-Value | ||
|---|---|---|---|---|---|---|
| VAS score | Pre-intervention | 4.7 ± 0.7 | 4.8 ± 0.7 | −0.1 (−3.8 to 3.4) | −0.142 | 0.903 |
| Post-intervention | 2.5 ± 0.6 | 2.4 ± 0.9 | 1.1 (−2.9 to 5.4) | 0.130 | 0.547 | |
| MD (95% CI) | 21.5 (18.7 to 24.4) | 23.0 (19.5 to 26.5) | ||||
| Effect size | 3.374 | 2.976 | ||||
| p-value | 0.001 * | 0.001 * | ||||
| AKPS score | Pre-intervention | 65.7 ± 3.9 | 63.9 ± 7.9 | 1.8 (−1.4 to 5.0) | 0.288 | 0.262 |
| Post-intervention | 77.5 ± 4.3 | 78.9 ± 6.4 | −1.4 (−4.3 to 1.3) | −0.256 | 0.304 | |
| MD (95% CI) | −11.7 (−13.8 to −9.6) | −15.0 (−18.2 to −11.8) | ||||
| Effect size | 2.874 | −2.086 | ||||
| p-value | 0.001 * | 0.001 * | ||||
| TSK-11 score | Pre-intervention | 32.4 ± 7.2 | 33.3 ± 3.7 | −0.9 (−3.9 to 1.9) | −0.157 | 0.503 |
| Post-intervention | 21.1 ± 2.7 | 20.7 ± 3.6 | 0.4 (−1.2 to 2.0) | 0.125 | 0.638 | |
| MD (95% CI) | 11.3 (8.7 to 13.8) | 12.6 (11.0 to 14.2) | ||||
| Effect size | 2.078 | 3.451 | ||||
| p-value | 0.001 * | 0.001 * |
| Parameters | Supervised-Rehab Group | Tele-Rehab Group | |
|---|---|---|---|
| Adherence Rate | Adherence Rate | ||
| Hamstring strength | PCC (r) | −0.111 | 0.174 |
| p-value | 0.559 | 0.350 | |
| Quadriceps strength | PCC (r) | 0.516 | 0.637 |
| p-value | 0.002 * | 0.001 * | |
| Hip strength | PCC (r) | 0.494 | −0.086 |
| p-value | 0.006 * | 0.644 | |
| Hamstring AT | PCC (r) | −0.283 | −0.266 |
| p-value | 0.129 | 0.148 | |
| Quadriceps AT | PCC (r) | 0.432 | 0.371 |
| p-value | 0.021 * | 0.040 * | |
| VAS score | PCC (r) | 0.091 | 0.368 |
| p-value | 0.634 | 0.042 * | |
| AKPS score | PCC (r) | 0.650 | 0.456 |
| p-value | 0.001 * | 0.010 * | |
| TSK-11 score | PCC (r) | 0.444 | 0.509 |
| p-value | 0.014 * | 0.003 * | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.H.; Shin, K.H.; Lee, G.B.; Son, S.; Jang, K.-M. Comparison of Functional Outcomes between Supervised Rehabilitation and Telerehabilitation in Female Patients with Patellofemoral Pain Syndrome during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 2233. https://doi.org/10.3390/ijerph20032233
Lee JH, Shin KH, Lee GB, Son S, Jang K-M. Comparison of Functional Outcomes between Supervised Rehabilitation and Telerehabilitation in Female Patients with Patellofemoral Pain Syndrome during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2023; 20(3):2233. https://doi.org/10.3390/ijerph20032233
Chicago/Turabian StyleLee, Jin Hyuck, Ki Hun Shin, Gyu Bin Lee, Seiwook Son, and Ki-Mo Jang. 2023. "Comparison of Functional Outcomes between Supervised Rehabilitation and Telerehabilitation in Female Patients with Patellofemoral Pain Syndrome during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 20, no. 3: 2233. https://doi.org/10.3390/ijerph20032233







