Community Pharmacy Staff’s Knowledge, Educational Needs, and Barriers Related to Counseling Cancer Patients and Cancer Survivors in Denmark
Abstract
:1. Introduction
Objective of the Study
2. Materials and Methods
2.1. Questionnaire Development
2.2. Sampling
2.3. Analysis
2.4. Ethical Considerations
3. Results
3.1. Characteristics of Respondents
3.2. Knowledge and Education Needs
3.3. Differences between Pharmacists and Pharmaconomists
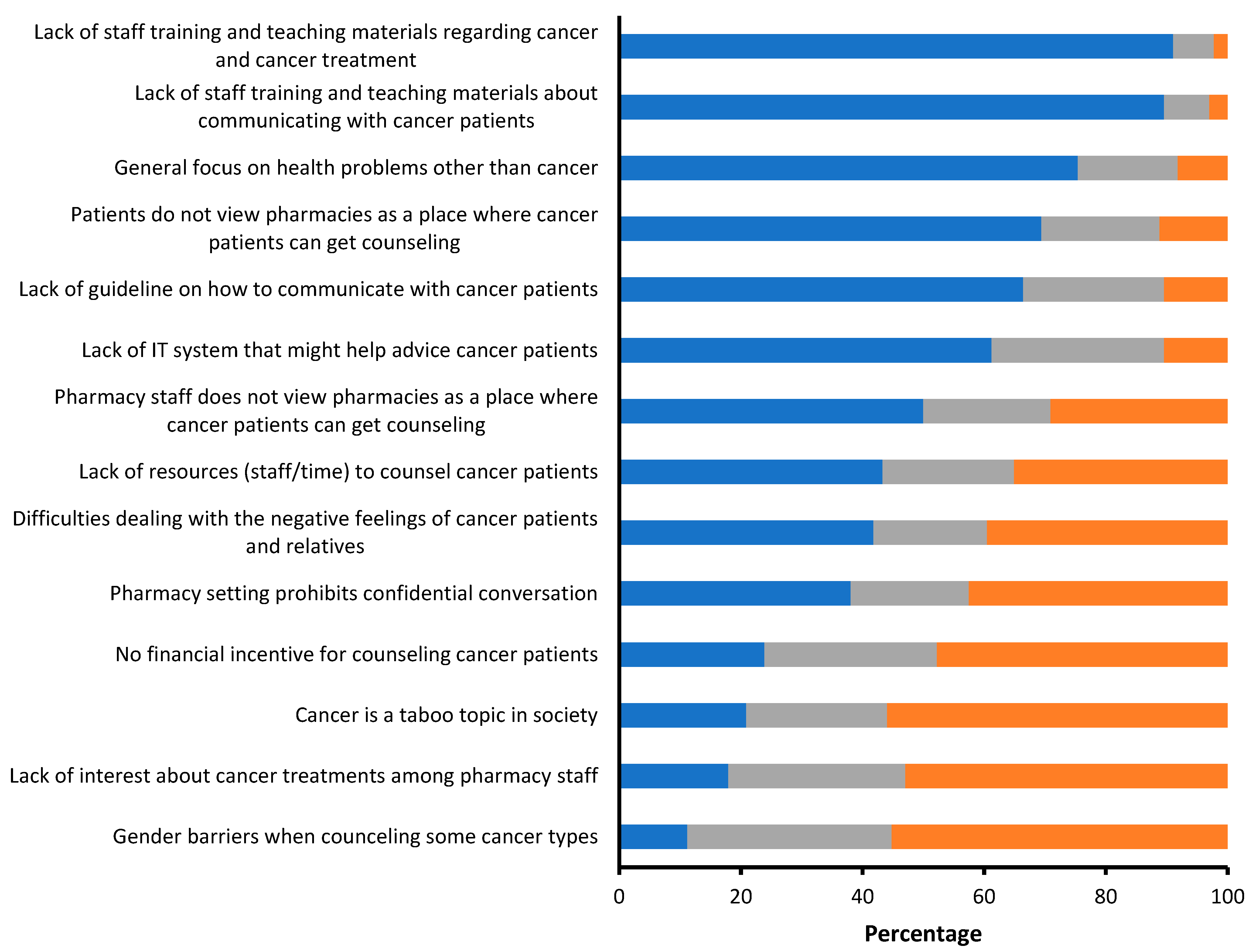
3.4. Barriers
3.5. Interest in Education
4. Discussion
Methodological Considerations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A


References
- WHO. World Health Organization. Cancer. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 24 November 2022).
- Cancer. Copenhagen (DK): Kræftens Bekæmpelse; 2022 Aug. Kræft i Danmark. 2022. Available online: https://www.cancer.dk/dyn/resources/File/file/9/9699/1665127828/kraeft-i-danmark-2022-bog-singlepages-3udg.pdf (accessed on 24 November 2022).
- PGEU. Brussels (BE): Pharmaceutical Group of European Union; PGEU Position Paper on Cancer. 2020. Available online: https://www.pgeu.eu/?s=&cats%5B%5D=539&date=all (accessed on 14 February 2022).
- Wiedenmayer, K.; Summers, R.S.; Mackie, C.A.; Gous, A.G.S.; Everard, M.; Tromp, D. World Health Organization. Developing Pharmacy Practice: A Focus on Patient Care; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Druedahl, L.C.; Hansen, J.M.; Freese, E.L.; Almarsdóttir, A.B.; Traulsen, J.M. Mandatory medication content in the curricula of six healthcare personnel types with patient contact in Denmark. Basic Clin. Pharmacol. Toxicol. 2019, 124, 431–438. [Google Scholar] [CrossRef]
- Herborg, H.; Sørensen, E.W.; Frøkjaer, B. Pharmaceutical care in community pharmacies: Practice and research in Denmark. Ann. Pharmacother. 2007, 41, 681–689. [Google Scholar] [CrossRef]
- Hassali, M.; Palaian, S.; Shafie, A.; Ibrahim, M. Perceptions and barriers towards provision of health promotion activities among community pharmacists in the State of Penang, Malaysia. J. Clin. Diagn. Res. 2009, 3, 1562–1568. [Google Scholar]
- Albanese, N.P.; Rouse, M.J.; Schlaifer, M. Scope of contemporary pharmacy practice: Roles, responsibilities, and functions of pharmacists and pharmacy technicians. J. Am. Pharm. Assoc. 2010, 50, e35–e69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koehler, T.; Brown, A. A global picture of pharmacy technician and other pharmacy support workforce cadres. Res. Soc. Adm. Pharm. 2017, 13, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsen, B.; Burghle, A.H.; Rossing, C. Pharmaceutical care services available in Danish community pharmacies. Int. J. Clin. Pharm. 2020, 42, 315–320. [Google Scholar] [CrossRef]
- Agergaard, M.; Rossing, C.; Herborg, H. Evidens for Apotekets Rådgivning; Resumé og Hovedkonklusioner; Pharmakon: Hillerød, Denmark, 2009; p. 37. [Google Scholar]
- Tomsen, D.; Søndergaard, B.; Herborg, H.; Klinke, B.O. Forbedret Selvmedicinering og Egenomsorg en Kontrolleret Undersøgelse; Pharmakon: Hillerød, Denmark, 2004; p. 63. [Google Scholar]
- Mensah, K.B.; Mensah, A.B.B.; Yamoah, P.; Attakorah, J.; Bangalee, V.; Oosthuizen, F. Knowledge assessment and barriers to cancer screening among Ghanaian community pharmacists. J. Oncol. Pharm. Pract. 2021, 28, 64–73. [Google Scholar] [CrossRef]
- Lindsey, L.; Husband, A.; Nazar, H.; Todd, A. Promoting the early detection of cancer: A systematic review of community pharmacy-based education and screening interventions. Cancer Epidemiol. 2015, 39, 673–681. [Google Scholar] [CrossRef] [Green Version]
- Alqudah, M.A.Y.; Al-Samman, R.M.; Mukattash, T.L.; Abu-Farha, R.K. Knowledge and attitudes of pharmacists towards colorectal cancer health education in Jordan: A cross-sectional study. Int. J. Clin. Pract. 2021, 75, e13986. [Google Scholar] [CrossRef]
- Abbott, R.; Edwards, S.; Whelan, M.; Edwards, J.; Dranitsaris, G. Are community pharmacists equipped to ensure the safe use of oral anticancer therapy in the community setting? Results of a cross-country survey of community pharmacists in Canada. J Oncol. Pharm. Pract. 2014, 20, 29–39. [Google Scholar] [CrossRef]
- Charpentier, M.M.; Orr, K.K.; Taveira, T.H. Improving pharmacist knowledge of oral chemotherapy in the community. Ann. Pharmacother. 2012, 46, 1205–1211. [Google Scholar] [CrossRef]
- Hussainy, S.Y.; Beattie, J.; Nation, R.L.; Dooley, M.J.; Fleming, J.; Wein, S.; Pisasale, M.; Scott, W.J.; Marriott, J.L. Palliative care for patients with cancer: What are the educational needs of community pharmacists? Support. Care Cancer 2006, 14, 177–184. [Google Scholar] [CrossRef]
- SST. Copenhagen (DK): Sundhedsstyrelsen. 2018. Forløbsprogram for rehabilitering og palliation i forbindelse med kræft. Available online: https://www.sst.dk/~/media/B0FD5078B1654B33A9E744CCBAE89022.ashx (accessed on 24 November 2022).
- SST. Copenhagen (DK): Sundhedsstyrelsen. 2018. Pakkeforløb og opfølgningsprogrammer. Available online: https://www.sst.dk/~/media/028409D2A0F94772B19868ABEF06B626.ashx (accessed on 24 November 2022).
- Shawahna, R.; Awawdeh, H. Pharmacists’ knowledge, attitudes, beliefs, and barriers toward breast cancer health promotion: A cross-sectional study in the Palestinian territories. BMC Health Serv. Res. 2021, 21, 429. [Google Scholar] [CrossRef]
- Butt, F.; Ream, E. Implementing oral chemotherapy services in community pharmacies: A qualitative study of chemotherapy nurses’ and pharmacists’ views. Int. J. Pharm. Pract. 2016, 24, 149–159. [Google Scholar] [CrossRef]
- Beshir, S.A.; Hanipah, M.A. Knowledge, perception, practice and barriers of breast cancer health promotion activities among community pharmacists in two Districts of Selangor state, Malaysia. Asian Pac. J. Cancer Prev. 2012, 13, 4427–4430. [Google Scholar] [CrossRef] [Green Version]
- Mensah, K.B.; Oosthuizen, F.; Bangalee, V. Cancer health promotion in Ghana: A survey of community pharmacists’ perception and barriers. J. Oncol. Pharm. Pract. 2020, 26, 1361–1368. [Google Scholar] [CrossRef] [PubMed]
- Kameda, S.; Kitamura, Y.; Masaoka, Y.; Fujimoto, M.; Ushio, S.; Sendo, T. Investigation of the difficulties experienced by pharmacists in Japan when communicating with cancer patients. J. Clin. Pharm. Ther. 2021, 46, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Willis, G.B.; Artino, A.R., Jr. What Do Our Respondents Think We’re Asking? Using Cognitive Interviewing to Improve Medical Education Surveys. J. Grad. Med. Educ. 2013, 5, 353–356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willis, G.B. Cognitive Interviewing. A “How To” Guide. 1999. Available online: https://www.hkr.se/contentassets/9ed7b1b3997e4bf4baa8d4eceed5cd87/gordonwillis.pdf (accessed on 25 October 2021).
- Beatty, P.C.; Willis, G.B. Research Synthesis: The Practice of Cognitive Interviewing. Public Opin. Q. 2007, 71, 287–311. [Google Scholar] [CrossRef] [Green Version]
- Tourangeau, R. Cognitive Sciences and survey methods. In Cognitive Aspects of Survey Methodology: Building a Bridge between Disciplines; Jabine, T., Straf, M., Tanur, J., Tourangeau, R., Eds.; National Academy Press: Washington, DC, USA, 1984; pp. 83–106. [Google Scholar]
- European Union. Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the Protection of Natural Persons with Regard to the Processing of Personal Data and on the Free Movement of Such Data, and Repealing Directive 95/46/Ec (General Data Protection Regulation). Off. J. Eur. Union 2016, 199, 1–88. [Google Scholar]
- European Commission. Ethics and Data Protection. Brussels (BE): European Commission. 5 July. 2021; 21p. Available online: https://ec.europa.eu/info/funding-tenders/opportunities/docs/2021-2027/horizon/guidance/ethics-and-data-protection_he_en.pdf (accessed on 7 December 2021).
- National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. The Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research; Department of Health, Education, and Welfare: Washington, DC, USA, 1979. [Google Scholar]
- CIOMS. International Ethical Guidelines for biomedical research involving human subjects. Bull. Med. Ethics 2002, 182, 17–23. [Google Scholar]
- Lægemiddelstyrelsen. Copenhagen (DK): Danish Medicines Agency. 2021. Undersøgelse Over Apotekernes Driftsforhold i 2019. Available online: https://laegemiddelstyrelsen.dk/da/udgivelser/2021/~/media/36C42086DA2949A091E713D757383EF9.ashx (accessed on 20 December 2021).
- Leinweber, C.E.; Campbell, H.S.; Trottier, D.L. Is a health promotion campaign successful in retail pharmacies? Can. J. Public Health 1995, 86, 380–383. [Google Scholar] [PubMed]
- Souvignier, S.T.; Mayer, J.A.; Eckhardt, L. Educating the public about skin cancer prevention: A role for pharmacists. J. Clin. Pharm Ther. 1996, 21, 399–406. [Google Scholar] [CrossRef]
- Armstrong, E.P.; Campbell, C.; Van Allen, A.; Vincent, E. Skin cancer knowledge and prevention counseling among Arizona pharmacists. J. Pharm. Pract. 2010, 23, 358–366. [Google Scholar] [CrossRef]
- Odedina, F.T.; Warrick, C.; Vilme, H.; Young, S. Pharmacists as health educators and risk communicators in the early detection of prostate cancer. Res. Social Adm. Pharm. 2008, 4, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Mensah, K.B.; Oosthuizen, F.; Bonsu, A.B. Cancer awareness among community pharmacist: A systematic review. BMC Cancer 2018, 18, 299. [Google Scholar] [CrossRef] [Green Version]
- Sendall, M.C.; Ostermann, L.; Brown, C.; McCosker, L. Health promotion of bowel cancer and breast cancer screening in community pharmacies: Pharmacists’ perceptions of their role, knowledge and confidence. Pharm. Pract. 2018, 16, 1275. [Google Scholar] [CrossRef] [Green Version]
- Ayoub, N.M.; Nuseir, K.Q.; Othman, A.K.; Abu Alkishik, S. Knowledge, attitudes and barriers towards breast cancer health education among community pharmacists. J. Pharm. Health Serv. Res. 2016, 7, 189–198. [Google Scholar] [CrossRef]
- Vu, K.; Pardhan, A.; Lakhani, N.; Metcalfe, S.; Mozuraitis, M.; Krzyzanowska, M. Managing chemotherapy-related toxicities in the community setting: A survey of pharmacists in Ontario. J. Oncol. Pharm. Pract. 2020, 26, 1903–1911. [Google Scholar] [CrossRef]
- Apotekerforeningen. Copenhagen (DK): Danmarks Apotekerforening; Apotekets Sundhedsydelser. 2021. Available online: https://www.apotekerforeningen.dk/om-os/apoteket-i-sundhedssektoren/sundhedsydelser (accessed on 30 November 2021).
- Danmarks Apotekerforening. Standard for Skrankerådgivning, 2nd ed.; Danmarks Apotekerforening: Copenhagen, Denmark, 2008; 22p. [Google Scholar]
- Fosgerau, C.; Clemmensen, N.B.; Husted, G.R.; Kaae, S.; Rossing, C. Programme Description: A mentalising education programme for community pharmacy workforce. Pharm. Educ. 2022, 22, 77–87. [Google Scholar] [CrossRef]
- Zamanzadeh, V.; Rahmani, A.; Valizadeh, L.; Ferguson, C.; Hassankhani, H.; Nikanfar, A.R.; Howard, F. The taboo of cancer: The experiences of cancer disclosure by Iranian patients, their family members and physicians. Psychooncology 2013, 22, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Estapé, J.; Palombo, H.; Hernández, E.; Daniels, M.; Estapé, T.; Grau, J.J.; Vinolas, N.; Mane, J.M. Cancer diagnosis disclosure in a Spanish hospital. Ann. Oncol. 1992, 3, 451–454. [Google Scholar] [CrossRef] [PubMed]
- Perez, G.K.; Salsman, J.M.; Fladeboe, K.; Kirchhoff, A.C.; Park, E.R.; Rosenberg, A.R. Taboo Topics in Adolescent and Young Adult Oncology: Strategies for Managing Challenging but Important Conversations Central to Adolescent and Young Adult Cancer Survivorship. Am. Soc. Clin. Oncol. Educ. Book 2020, 40, e171–e185. [Google Scholar] [CrossRef] [PubMed]
- Galanti, G.A. An introduction to cultural differences. West. J. Med. 2000, 172, 335–336. [Google Scholar] [CrossRef] [Green Version]
- Israel, G.D.; Taylor, C.L. Can response order bias evaluations? Eval. Program Plan. 1990, 13, 365–371. [Google Scholar] [CrossRef]
| Cognitive Probe | Question |
|---|---|
| Think-aloud | What did you think when answering this question? Was it hard/easy to understand? And why? |
| Comprehension | How do you understand the question? |
| Retrieval of information | How did you get to this answer? On what did you base your answer? Is there a specific situation you think about? |
| Judgment | How sure are you in answering the question? |
| Selection of a response to the question | How was it to answer the question? Do you think you could answer sufficiently based on how the question was posed? |
| Characteristics | Frequency | Percentage | |
|---|---|---|---|
| Gender | |||
| Male | 22 | 16.4 | |
| Female | 112 | 83.6 | |
| Age group (years) | |||
| Under 25 | 8 | 6.0 | |
| 25–34 | 49 | 36.6 | |
| 35–44 | 31 | 23.1 | |
| 45–54 | 17 | 12.7 | |
| 55–64 | 25 | 18.7 | |
| Over 65 | 4 | 3.0 | |
| Education | |||
| Pharmacist | 79 | 59.0 | |
| Pharmaconomist | 51 | 38.1 | |
| Pharmacy student | 4 | 3.0 | |
| Job title | |||
| Pharmacy owner | 18 | 13.4 | |
| Pharmacy manager | 22 | 16.4 | |
| Information-, quality-, prescription pharmacist | 29 | 21.6 | |
| Practicing pharmacist | 19 | 14.2 | |
| Practicing pharmaconomist | 42 | 31.3 | |
| Pharmacy student under an internship | 4 | 3.0 | |
| Region | |||
| North Denmark region | 12 | 9.0 | |
| Central Denmark Region | 26 | 19.4 | |
| Region of Southern Denmark | 28 | 20.9 | |
| Region Zealand | 21 | 15.7 | |
| Capital Region of Denmark | 47 | 35.1 | |
| Years of Practice | |||
| Less than 1 year | 4 | 3.0 | |
| 1–3 years | 29 | 21.6 | |
| 4–10 years | 33 | 24.6 | |
| 11–20 years | 33 | 24.6 | |
| More than 20 years | 35 | 26.1 | |
| Knowledge of Cancer from | Pharmacists (n = 79) | Pharmaconomists (n = 51) | ||
|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | |
| No knowledge | 3 | 3.8 | 4 | 7.8 |
| Pharmacist-/pharmaconomist education | 50 | 63.3 | 25 | 49.0 |
| Continuous education (e.g., courses) | 14 | 17.7 | 3 | 5.9 |
| Work experience | 37 | 46.8 | 23 | 45.1 |
| Self-study | 29 | 36.7 | 18 | 35.3 |
| Cancer trajectories I have experienced or been close to (e.g., own or relatives’) | 42 | 53.2 | 33 | 64.7 |
| Other | 7 | 8.9 | 4 | 7.8 |
| Category a | Topic | Knowledge | Importance | ||||
|---|---|---|---|---|---|---|---|
| Mean b | CI (95%) | SD | Mean c | CI (95%) | SD | ||
| Treatment | Causes and risk factors for getting cancer | 3.4 | [3.24; 3.49] | ** | 3.4 | [3.28; 3.60] | |
| - | Stages of cancer | 2.7 | [2.55; 2.87] | ** | 3.1 | [2.89; 3.21] | |
| - | Incidence and prevalence of cancer | 2.1 | [1.97; 2.24] | * | 2.6 | [2.48; 2.79] | |
| - | Diagnosing of cancer | 2.7 | [2.53; 2.80] | ** | 3.2 | [2.74; 3.05] | |
| - | Surgical treatment of cancer | 2.6 | [2.42; 2.70] | 2.7 | [2.56; 2.90] | ||
| - | Radiation therapy for cancer | 2.5 | [2.38; 2.65] | 2.9 | [2.75; 3.09] | ||
| - | Medical treatment of cancer | 2.8 | [2.65; 2.96] | * | 3.8 | [3.59; 3.91] | |
| - | Side effects of medical treatment of cancer | 3.3 | [3.21; 3.48] | * | 4.3 | [4.13; 4.40] | |
| - | Complications after surgery and radiation therapy | 2.8 | [2.68; 2.98] | ** | 3.8 | [3.68; 3.99] | |
| - | Drug interactions during cancer treatment | 2.4 | [2.20; 2.51] | 4.4 | [4.28; 4.53] | ||
| - | Supplementary use of herbal remedies or supplements at the same time as medical cancer treatment | 2.2 | [2.08; 2.37] | 4.1 | [3.99; 4.28] | ||
| - | Rehabilitation of cancer patients | 2.2 | [2.03; 2.30] | 3.0 | [2.84; 3.16] | ||
| - | Late effects of cancer and/ or treatment | 2.6 | [2.44; 2.73] | 3.7 | [3.54; 3.83] | ||
| Organization | Overall about the national cancer plan | 2.3 | [2.15; 2.47] | ** | 3.0 | [2.88; 3.17] | |
| - | Screening for cancer | 3.0 | [2.89; 3.16] | 3.0 | [2.83; 3.14] | ||
| - | Diagnosis of cancer | 2.4 | [2.25; 2.55] | ** | 2.9 | [2.74; 3.05] | |
| - | Treatment of cancer | 2.5 | [2.38; 2.71] | ** | 3.2 | [3.04; 3.37] | |
| - | Rehabilitation services for cancer patients | 2.1 | [1.96; 2.25] | 3.2 | [2.99; 3.31] | ||
| - | Follow-up after cancer treatment | 2.2 | [2.06; 2.36] | 3.1 | [2.96; 3.28] | ||
| - | Management of side effects in cancer treatment | 2.6 | [2.44; 2.75] | 4.1 | [4.00; 4.27] | ||
| - | Management of late effects after cancer and/or cancer treatment | 2.3 | [2.14; 2.44] | 3.9 | [3.76; 4.03] | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buhl, C.; Olsen, N.L.; Nørgaard, L.S.; Thomsen, L.A.; Jacobsen, R. Community Pharmacy Staff’s Knowledge, Educational Needs, and Barriers Related to Counseling Cancer Patients and Cancer Survivors in Denmark. Int. J. Environ. Res. Public Health 2023, 20, 2287. https://doi.org/10.3390/ijerph20032287
Buhl C, Olsen NL, Nørgaard LS, Thomsen LA, Jacobsen R. Community Pharmacy Staff’s Knowledge, Educational Needs, and Barriers Related to Counseling Cancer Patients and Cancer Survivors in Denmark. International Journal of Environmental Research and Public Health. 2023; 20(3):2287. https://doi.org/10.3390/ijerph20032287
Chicago/Turabian StyleBuhl, Caroline, Nadia Lund Olsen, Lotte Stig Nørgaard, Linda Aagaard Thomsen, and Ramune Jacobsen. 2023. "Community Pharmacy Staff’s Knowledge, Educational Needs, and Barriers Related to Counseling Cancer Patients and Cancer Survivors in Denmark" International Journal of Environmental Research and Public Health 20, no. 3: 2287. https://doi.org/10.3390/ijerph20032287
APA StyleBuhl, C., Olsen, N. L., Nørgaard, L. S., Thomsen, L. A., & Jacobsen, R. (2023). Community Pharmacy Staff’s Knowledge, Educational Needs, and Barriers Related to Counseling Cancer Patients and Cancer Survivors in Denmark. International Journal of Environmental Research and Public Health, 20(3), 2287. https://doi.org/10.3390/ijerph20032287







