Implementation of Health Impact Assessment in the Healthcare System of the Republic of Kazakhstan
Abstract
:1. Introduction
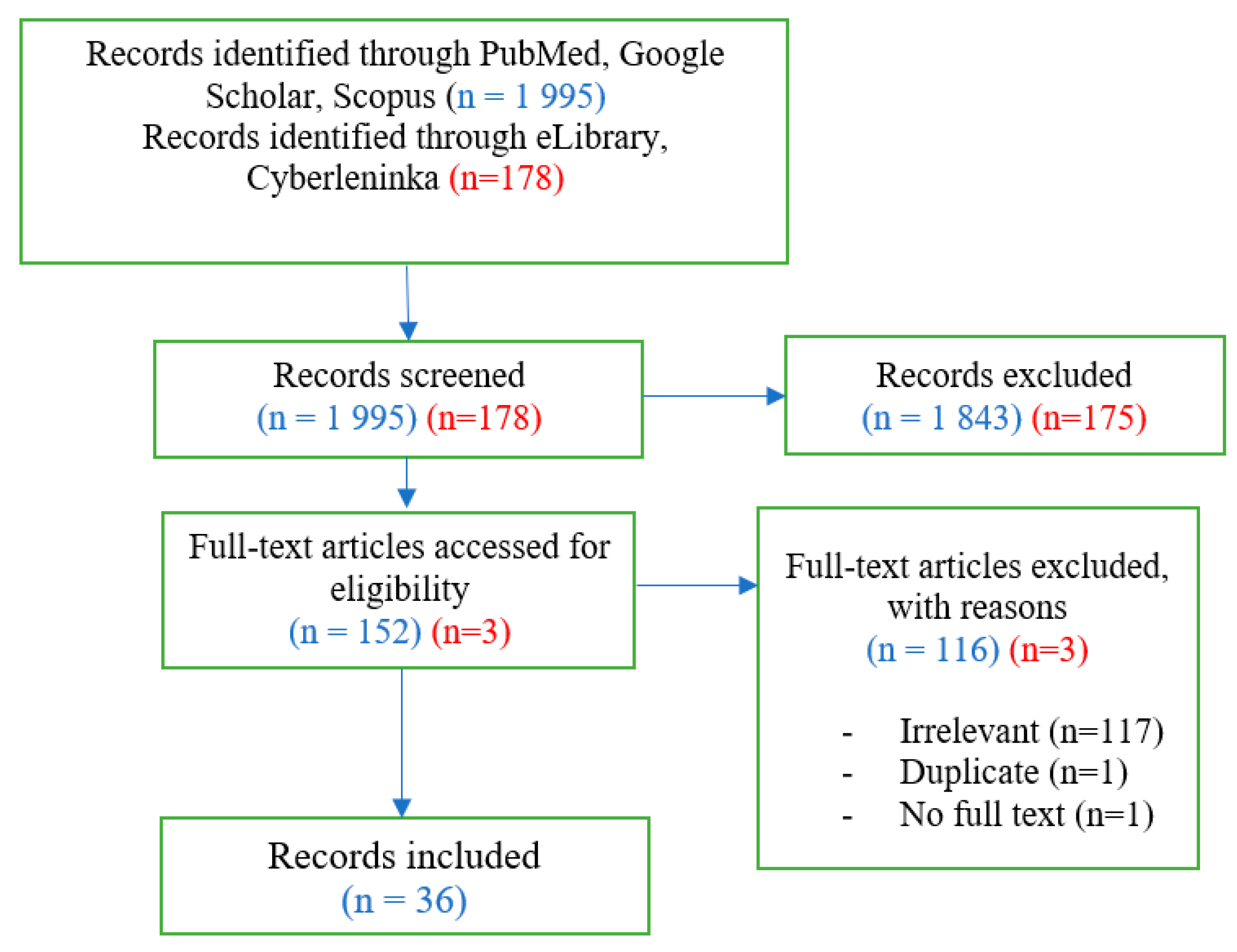
2. Materials and Methods
- Considers the model of implementation of HIA into existing systems;
- Demonstrates how HIA is currently established and functions in the country;
- Has full text available for free;
- Not older than 2003.
3. Results
3.1. Implementation of HIA on International Level
| Adapted HIA | Standalone HIA | Part of / In Conjunction with Another Assessment | Regulation | |
|---|---|---|---|---|
| Countries with HIA | Thailand—CHIA [48] | Wales [33]; Spain [50] | Mongolia—EIA [40]; Czech—EIA [41]; Lesotho—EIA [42]; Republic of South Africa—EIA [43]; Australia—EFHIA [44] | Nationally |
| France [29]; Denmark [38] | Locally | |||
| Quebec [10]; Sweden [24] | Mixed | |||
| Being implemented | Iran [49] | Myanmar, Cambodia, and Cameroon—EIA [37] |
3.2. HIA and Decision-Making in RK
3.3. Model of Implementation in RK
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Buse, K. Tedros Calls for a Paradigm Shift—What next on This Political Agenda? BMJ 2022, 379, 2529. [Google Scholar] [CrossRef]
- Kemm, J.; Parry, J.; Palmer, S. (Eds.) Health Impact Assessment; Oxford University Press: Oxford, UK, 2004. [Google Scholar]
- WHO. Jakarta Declaration on Leading Health Promotion into the 21st Century. Available online: https://www.who.int/teams/health-promotion/enhanced-wellbeing/fourth-conference/jakarta-declaration (accessed on 23 January 2023).
- Mittelmark, M. Promoting Social Responsibility for Health: Health Impact Assessment and Healthy Public Policy at the Community Level. Health Promot. Int. 2001, 16, 74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pennington, A.; Dreaves, H.; Scott-Samuel, A.; Haigh, F.; Harrison, A.; Verma, A.; Pope, D. Development of an Urban Health Impact Assessment Methodology: Indicating the Health Equity Impacts of Urban Policiesle. Eur. J. Public Health 2017, 27, 56–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kligerman, D.; Cardoso, T.; Cohen, S.; Azevedo, D.; Toledo, G.; Azevedo, A.P.C.B.; Charlesworth, S. Methodology for a Comprehensive Health Impact Assessment in Water Supply and Sanitation Programmes for Brazil. Int. J. Env. Res. Public Health 2022, 19, 12776. [Google Scholar] [CrossRef]
- Hoyer, D.; Dee, E.; O’Leary, M.; Heffernan, M.; Gelfand, K.; Kappel, R.; Fromknecht, C. How Do We Define and Measure Health Equity? The State of Current Practice and Tools to Advance Health Equity. J. Public Health Manag. Pract. 2022, 28, 570–577. [Google Scholar] [CrossRef] [PubMed]
- Dannenberg, A. Effectiveness of Health Impact Assessments: A Synthesis of Data from Five Impact Evaluation Reports. Prev. Chronic Dis. 2016, 13, E84. [Google Scholar] [CrossRef] [Green Version]
- Birley, M.; Bos, R. Health Impact Assessment: A Tool for Intersectoral Collaboration. Ecol. Control Vector Borne Dis. 2021, 6, 181–197. [Google Scholar]
- Gamache, S.; Diallo, T.T.A.; Shankardass, K.; Lebel, A. The Elaboration of an Intersectoral Partnership to Perform Health Impact Assessment in Urban Planning: The Experience of Quebec City (Canada). Int. J. Environ. Res. Public Health 2020, 17, 7556. [Google Scholar] [CrossRef]
- Haigh, F.; Baum, F.; Dannenberg, A.L.; Harris, M.F.; Harris-Roxas, B.; Keleher, H.; Kemp, L.; Morgan, R.; Chok, H.N.; Spickett, J.; et al. The Effectiveness of Health Impact Assessment in Influencing Decision-Making in Australia and New Zealand 2005–2009. BMC Public Health 2013, 13, 1188. [Google Scholar] [CrossRef] [Green Version]
- Kang, E.; Park, H.; Kim, J. Health Impact Assessment as a Strategy for Intersectoral Collaboration. J. Prev. Med. Public Health 2011, 44, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Wismar, H.; Blau, J.; Ernst, K. (Eds.) Is HIA Effective? A Synthesis of Concepts, Methodologies and Results. In The Effectiveness of Health Impact Assessment: Scope and Limitations of Supporting Decision Making in Europe; The European Observatory on Health Systems and Policies: Brussels, Belgium, 2007; pp. 15–36. [Google Scholar]
- Ramirez-Rubio, O.; Daher, C.; Fanjul, G.; Gascon, M.; Mueller, N.; Pajín, L.; Plasencia, A.; Rojas-Rueda, D.; Thondoo, M.; Nieuwenhuijsen, M.J. Urban Health: An Example of a “Health in All Policies” Approach in the Context of SDGs Implementation. Glob. Health 2019, 15, 87. [Google Scholar] [CrossRef]
- Government of the Republic of Kazakhstan. National Project “Quality and Affordable Healthcare for Every Citizen “Healthy Nation””; No. 725, Decree of the Government of the Republic of Kazakhstan dated 12 October 2021; Government of the Republic of Kazakhstan: Astana, Kazakhstan, 2021.
- Kögel, C.; Rodríguez Peña, T.; Sánchez, I.; Tobella, M.; López, J.; Espot, F.; Claramunt, F.; Rabal, G.; González Viana, A. Health Impact Assessment (HIA) of a Fluvial Environment Recovery Project in a Medium-Sized Spanish Town. Int. J. Environ. Res. Public Health 2020, 17, 1484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rogerson, B.; Lindberg, R.; Baum, F.; Dora, C.; Haigh, F.; Simoncelli, A.M.; Parry Williams, L.; Peralta, G.; Pollack Porter, K.M.; Solar, O. Recent Advances in Health Impact Assessment and Health in All Policies Implementation: Lessons from an International Convening in Barcelona. Int. J. Environ. Res. Public Health 2020, 17, 7714. [Google Scholar] [CrossRef] [PubMed]
- Such, E.; Smith, K.; Woods, H.B.; Meier, P. Governance of Intersectoral Collaborations for Population Health and to Reduce Health Inequalities in High-Income Countries: A Complexity-Informed Systematic Review. Int. J. Health Policy Manag. 2022, 11, 2780–2792. [Google Scholar] [CrossRef] [PubMed]
- Negev, M.; Zea-Reyes, L.; Caputo, L.; Weinmayr, G.; Potter, C.; de Nazelle, A. Barriers and Enablers for Integrating Public Health Cobenefits in Urban Climate Policy. Annu. Rev. Public Health 2022, 43, 255–270. [Google Scholar] [CrossRef]
- Caussy, D.; Kumar, P.; Than Sein, U. Health Impact Assessment Needs in South-East Asian Countries. Bull. World Health Organ. 2003, 81, 439–443. [Google Scholar]
- Sharma, M.; Netherton, A.; McLarty, K.; Petrokofsky, C.; Chang, M. Professional Workforce Training Needs for Health Impact Assessment in Spatial Planning: A Cross Sectional Survey, Public Health in Practice. Public Health Pract. 2022, 3, 100268. [Google Scholar] [CrossRef]
- Maidin, A.J.; Ahamed, N.F.S. Mandatory Health Impact Assessment in Malaysian Land Planning and Development Control System. Procedia Soc. Behav. Sci. 2012, 68, 164–172. [Google Scholar] [CrossRef] [Green Version]
- Thondoo, M.; Rojas-Rueda, D.; Gupta, J.; de Vries, D.; Nieuwenhuijsen, M. Systematic Literature Review of Health Impact Assessments in Low and Middle-Income Countries. Int. J. Environ. Res. Public Health 2019, 16, 2018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knuttson, I.; Linell, A. Health Impact Assessment Developments in Sweden. Scand. J. Public Health 2010, 38, 115–120. [Google Scholar] [CrossRef]
- Fedorowicz, M.; Aron, L.Y. Improving Evidence-Based Policymaking: A Review; Urban Institute: Washington, DC, USA, 2021. [Google Scholar]
- Mathias, K.R.; Harris-Roxas, B. Process and Impact Evaluation of the Greater Christchurch Urban Development Strategy Health Impact Assessment. BMC Public Health 2009, 9, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fakhri, A.; Maleki, M.; Gohari, M.; Harris, P. Investigating Underlying Principles to Guide Health Impact Assessment. Int. J. Health Policy Manag. 2014, 3, 17–22. [Google Scholar] [CrossRef]
- Green, L.; Ashton, K.; Parry-Williams, L.; Dyakova, M.; Clemens, T.; Bellis, M. Facilitators, Barriers and Views on the Role of Public Health Institutes in Promoting and Using Health Impact Assessment-An International Virtual Scoping Survey and Expert Interviews. Int. J. Environ. Res. Public Health 2022, 19, 13367. [Google Scholar] [CrossRef]
- Jabot, F.; Tremblay, E.; Rivadeneyra, A.; Diallo, T.A.; Lapointe, G. A Comparative Analysis of Health Impact Assessment Implementation Models in the Regions of Montérégie (Québec, Canada) and Nouvelle-Aquitaine (France). Int. J. Environ. Res. Public Health 2020, 17, 6558. [Google Scholar] [CrossRef]
- Thondoo, M.; De Vries, D.; Rojas-Rueda, D.; Ramkalam, Y.D.; Verlinghieri, E.; Gupta, J.; Nieuwenhuijsen, M. Framework for Participatory Quantitative Health Impact Assessment in Low- and Middle-Income Countries. Int. J. Environ. Res. Public Health 2020, 17, 7688. [Google Scholar] [CrossRef] [PubMed]
- Davenport, C.; Mathers, J.; Parry, J. Use of Health Impact Assessment in Incorporating Health Considerations in Decision Making. J. Epidemiol. Community Health 2006, 60, 196–201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoehner, M.C.; Rios, J.; Garmendia, C.; Baldwin, S.; Kelly, C.M.; Knights, D.-M.; Lesorogol, C.; Gunn McClendon, G.; Tranel, M. Page Avenue Health Impact Assessment: Building on Diverse Partnerships and Evidence to Promote a Healthy Community. Health Place 2012, 18, 85–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delany, T.; Harris, P.; Williams, C.; Harris, E.; Baum, F.; Lawless, A.; Wildgoose, D.; Haigh, F.; MacDougall, C.; Broderick, D.; et al. Health Impact Assessment in New South Wales & Health in All Policies in South Australia: Differences, Similarities and Connections. BMC Public Health 2014, 14, 699. [Google Scholar]
- Ison, E. Health Impact Assessment in a Network of European Cities. J. Urban Health 2013, 90, 105–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mwatsama, M.; Wong, S.; Ettehad, D.; Watt, N. Global Health Impacts of Policies: Lessons from the UK. Glob. Health 2014, 10, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dua, B.; Acharya, A. Health Impact Assessment: Need and Future Scope in India. Indian J. Community Med. 2014, 39, 76–81. [Google Scholar] [PubMed]
- ADB. A Health Impact Assessment Framework for Special Economic Zones in the Greater Mekong Subregion; ADB: Mandaluyong, Philippines, 2018. [Google Scholar]
- Kraemer, S.; Nikolajsen, L.; Gulis, G. Implementation of Health Impact Assessment in Danish Municipal Context. Cent. Eur. J. Public Health 2014, 22, 211–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Green, L.; Ashton, K.; Azam, S.; Dyakova, M.; Clemens, T.; Bellis, M. Using Health Impact Assessment (HIA) to Understand the Wider Health and Well-Being Implications of Policy Decisions: The COVID-19 “staying at Home and Social Distancing Policy” in Wales. BMC Public Health 2021, 21, 1456. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, M.; Vanya, D.; Davison, C.; Lkhagvasuren, O.; Johnston, L.; Janes, C. Harnessing Opportunities for Good Governance of Health Impacts of Mining Projects in Mongolia: Results of a Global Partnership. Glob. Health 2017, 13, 39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mařincová, L.; Loosová, J.; Valenta, V. Experiences and Needs of Licensed Health Risk Assessors Conducting Health Impact Assessment in the Czech Republic. Cent. Eur. J. Public Health 2020, 28, 108–113. [Google Scholar] [CrossRef]
- Gwimbi, P.; Lebese, P.; Kanono, K. Mainstreaming Health Impact Assessments in Environmental Impact Statements into Planning Obligations in Post Dam Construction in Metolong, Lesotho: A Qualitative Investigation. Heliyon 2020, 2, 7. [Google Scholar] [CrossRef]
- Leuenberger, A.; Winkler, M.; Cambaco, O.; Cossa, H.; Kihwele, F.; Lyatuu, I.; Zabré, H.R.; Farnham, A.; Macete, E.; Munguambe, K. Health Impacts of Industrial Mining on Surrounding Communities: Local Perspectives from Three Sub-Saharan African Countries. PLoS ONE 2021, 16, e0252433. [Google Scholar] [CrossRef]
- Harris-Roxas, B.; Haigh, F.; Travaglia, J.; Kemp, L. Evaluating the Impact of Equity Focused Health Impact Assessment on Health Service Planning: Three Case Studies. BMC Health Serv. Res. 2014, 14, 371. [Google Scholar] [CrossRef] [Green Version]
- Gulis, G.; Mochungong, P.I. Health Impact Assessment and Evaluation of a Clinical Waste Management Policy for Cameroon. J. Public Health Afr. 2013, 4, e7. [Google Scholar] [CrossRef] [Green Version]
- Kichigin, N.V. Legal Regulation of Environmental Impact Assessment in Russia and Abroad. J. Foreign Legis. Comp. Law 2016, 5, 117–123. [Google Scholar]
- Nikitina, V.N.; Kalinina, N.I.; Ljashko, G.G.; Dubrovskaja, E.N.; Plehanov, V.P. Features of architecture of 5g networks. Probabilistic prediction of the impact of electromagnetic fields of radio frequencies on the population (Review of literature). Hyg. Sanit. 2021, 100, 792–796. [Google Scholar] [CrossRef]
- Chanchang, C.; Sithisarankul, P.; Supanitayanon, T. Environmental and Health Impact Assessment for Ports in Thailand. Int Marit. Health 2016, 67, 112–116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Damari, B.; Vosoogh-Moghaddam, A.; Riazi-Isfahani, S. Implementing Health Impact Assessment at National Level: An Experience in Iran. Iran. J. Public Health 2018, 47, 246–255. [Google Scholar] [PubMed]
- Sanz, E.; Esnaola, S.; Aldasoro, E.; Bacigalupe, A.; Zuazagoitia, J. Steps towards the Institutionalization of Health Impact Assessment in Spain: Perception of Public Health Professionals. An. Sist. Sanit. Navar. 2012, 35, 403–412. [Google Scholar] [CrossRef] [PubMed]
- Government of the Republic of Kazakhstan. On the President of the Republic of Kazakhstan; No. 2733, Constitutional Law of the Republic of Kazakhstan dated 26 December 1995; Government of the Republic of Kazakhstan: Astana, Kazakhstan, 1995.
- Government of the Republic of Kazakhstan. On the Parliament of the Republic of Kazakhstan and the Status of Its Deputies; No. 2529, Constitutional Law of the Republic of Kazakhstan dated 16 October 1995; Government of the Republic of Kazakhstan: Astana, Kazakhstan, 1995.
- Government of the Republic of Kazakhstan. On the Government of the Republic of Kazakhstan; No. 2688, Constitutional Law of the Republic of Kazakhstan dated 18 December 1995; Government of the Republic of Kazakhstan: Astana, Kazakhstan, 1995.
- Government of the Republic of Kazakhstan. On Some Issues of the Ministries of Health and National Economy of the Republic of Kazakhstan; No. 412, Regulation of the Government of the Republic of Kazakhstan in accordance with the Decree of the President of the Republic of Kazakhstan “On further improvement of the public administration” dated 25 January 2017; Government of the Republic of Kazakhstan: Astana, Kazakhstan, 2017.
- Government of the Republic of Kazakhstan. On Some Issues of the Public Council of the Ministry of Health of the Republic of Kazakhstan; Order of the Ministry of Health of the Republic of Kazakhstan dated 12 April 2017; Government of the Republic of Kazakhstan: Astana, Kazakhstan, 2017.
- Government of the Republic of Kazakhstan. On Approval of the Rules for State Accounting of Scientific, Scientific and Technical Projects and Programs Financed from the State Budget, and Reports on Their Implementation; No. 149, Order of the Minister of Education and Science of the Republic of Kazakhstan dated 31 March 2015; Government of the Republic of Kazakhstan: Astana, Kazakhstan, 2015.
- Government of the Republic of Kazakhstan. On Program-Targeted Financing of Non-Competitive Procedures for 2020—2022; Regulation of the Government of the Republic of Kazakhstan in accordance with Article 27 of the Law of the Republic of Kazakhstan “On Science” dated 18 February 2011; Government of the Republic of Kazakhstan: Astana, Kazakhstan, 2011.
- Government of the Republic of Kazakhstan. Rules for the Organization and Conduct of State Scientific and Technical Expertise; Decree of the Government of the Republic of Kazakhstan dated 1 August 2011; Government of the Republic of Kazakhstan: Astana, Kazakhstan, 2011.
- Government of the Republic of Kazakhstan. On approval of the Rules for basic, grant, program-targeted financing of scientific and (or) scientific and technical activities; No. 758, Decree of the Government of the Republic of Kazakhstan dated October 22 2021; Government of the Republic of Kazakhstan: Astana, Kazakhstan, 2021.
- Government of the Republic of Kazakhstan. On National Scientific Councils; No. 519, Decree of the Government of the Republic of Kazakhstan dated 16 May 2011; Government of the Republic of Kazakhstan: Astana, Kazakhstan, 2011.
- Government of the Republic of Kazakhstan. Environmental Code of the Republic of Kazakhstan; No. 400-VI ZRK, Code of the Republic of Kazakhstan dated 2 January 2021; Government of the Republic of Kazakhstan: Astana, Kazakhstan, 2021.


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kalel, Z.S.; Gulis, G.; Aringazina, A.M. Implementation of Health Impact Assessment in the Healthcare System of the Republic of Kazakhstan. Int. J. Environ. Res. Public Health 2023, 20, 2335. https://doi.org/10.3390/ijerph20032335
Kalel ZS, Gulis G, Aringazina AM. Implementation of Health Impact Assessment in the Healthcare System of the Republic of Kazakhstan. International Journal of Environmental Research and Public Health. 2023; 20(3):2335. https://doi.org/10.3390/ijerph20032335
Chicago/Turabian StyleKalel, Zhan S., Gabriel Gulis, and Altyn M. Aringazina. 2023. "Implementation of Health Impact Assessment in the Healthcare System of the Republic of Kazakhstan" International Journal of Environmental Research and Public Health 20, no. 3: 2335. https://doi.org/10.3390/ijerph20032335






