Awake and Sleep Bruxism Prevalence and Their Associated Psychological Factors in First-Year University Students: A Pre-Mid-Post COVID-19 Pandemic Comparison
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Materials
2.3.1. Self-Reported Bruxism Questionnaire
2.3.2. Psychological Questionnaires
2.4. Procedure
2.5. Statistical Analysis
3. Results
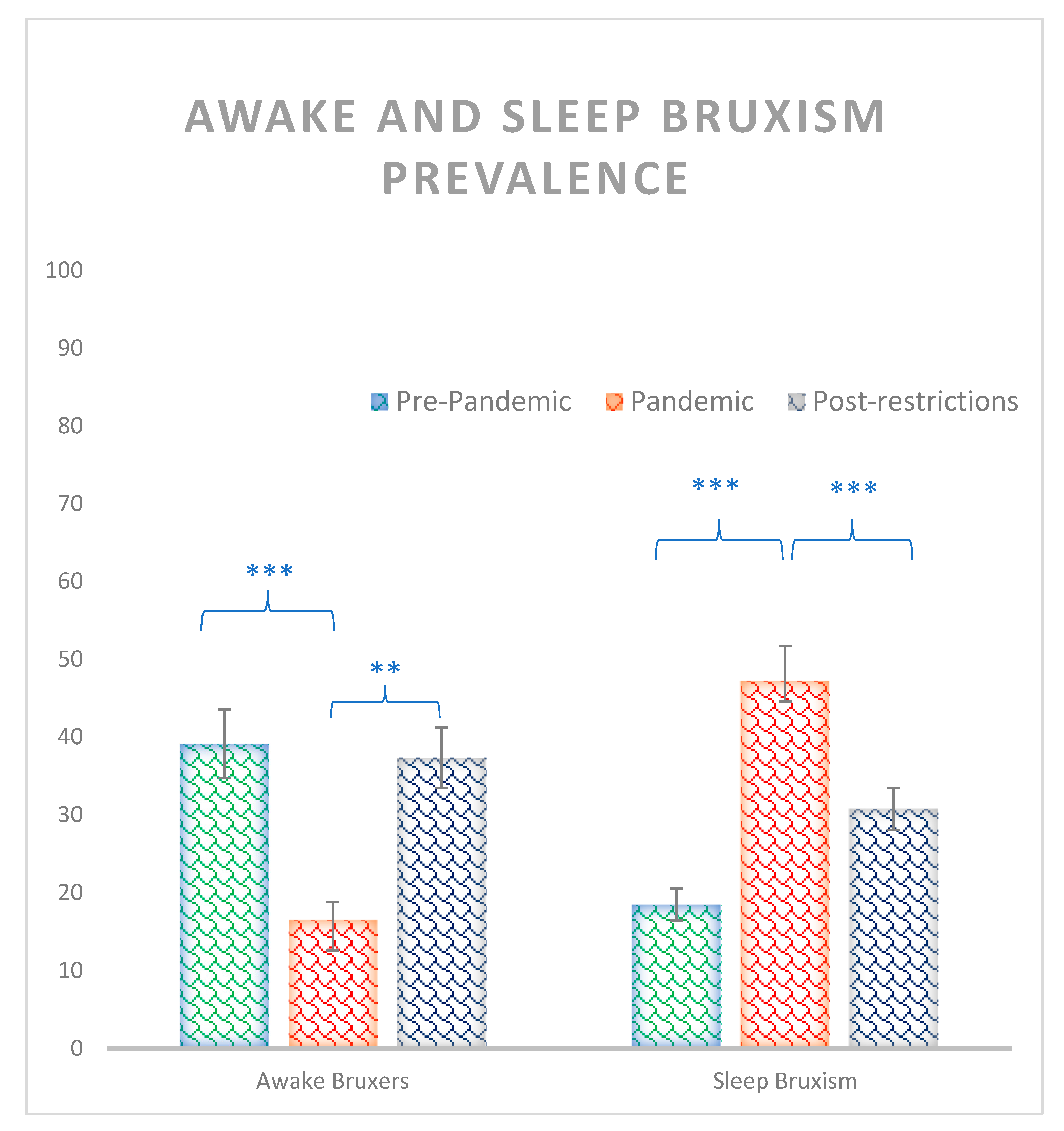
3.1. Awake and Sleep Bruxism Prevalence
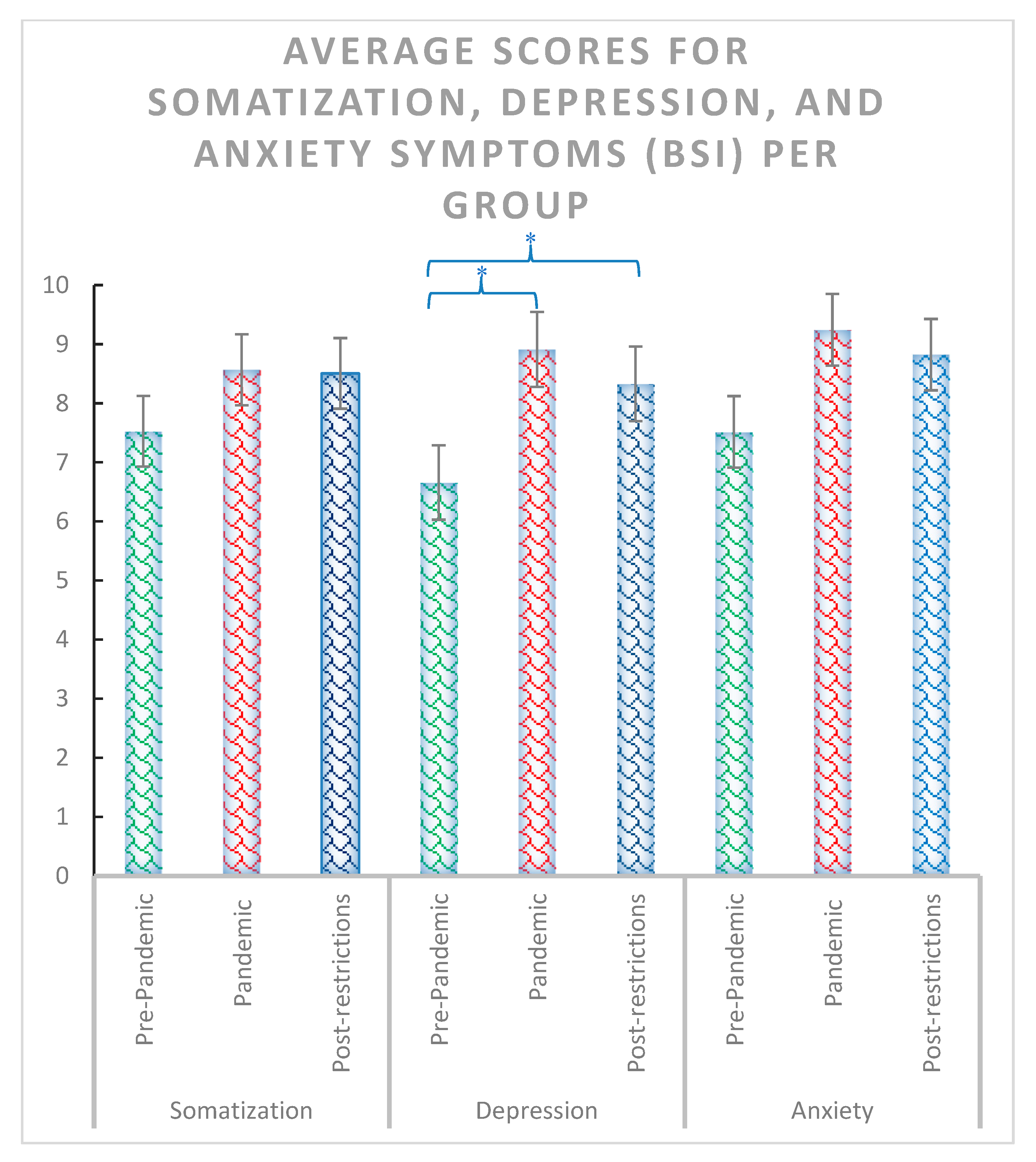
3.2. Questionnaires
4. Discussion
Limitations, Strengths and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lobbezoo, F.; Ahlberg, J.; Raphael, K.G.; Wetselaar, P.; Glaros, A.G.; Kato, T.; Santiago, V.; Winocur, E.; De Laat, A.; De Leeuw, R.; et al. International consensus on the assessment of bruxism: Report of a work in progress. J. Oral Rehabil. 2018, 45, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Klasser, G.D.; Rei, N.; Lavigne, G.J. Sleep bruxism etiology: The evolution of a changing paradigm. J. Can. Dent. Assoc. 2015, 81, f2. [Google Scholar] [PubMed]
- Sateia, M.J. International Classification of Sleep Disorders-Third Edition. Chest 2014, 146, 1387–1394. [Google Scholar] [CrossRef]
- Manfredini, D.; Ahlberg, J.; Wetselaar, P.; Svensson, P.; Lobbezoo, F. The bruxism construct: From cut-off points to a continuum spectrum. J. Oral Rehabil. 2019, 46, 991–997. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Fierro, N.; Martínez-Fierro, M.; Cerda-Flores, R.; Gómez-Govea, M.; Delgado-Enciso, I.; Martínez-De-Villarreal, L.; González-Ramírez, M.; Rodríguez-Sánchez, I. The phenotype, psychotype and genotype of bruxism. Biomed. Rep. 2018, 8, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Ahlberg, J.; Aarab, G.; Bracci, A.; Durham, J.; Ettlin, D.; Gallo, L.M.; Koutris, M.; Wetselaar, P.; Svensson, P.; et al. Towards a Standardized Tool for the Assessment of Bruxism (STAB)—Overview and general remarks of a multidimensional bruxism evaluation system. J. Oral Rehabil. 2020, 47, 549–556. [Google Scholar] [CrossRef]
- Cruz Fierro, N.; González Ramírez, M.T.; Juno Vanegas Farfano, M.T. Cuestionario de bruxismo autoinformado. Estudio piloto en el noreste de México. Interdiscip. Rev. Psicol. Cienc. Afines 2019, 36, 217–232. [Google Scholar] [CrossRef]
- Cruz-Fierro, N.; Vanegas-Farfano, M.T.J.; González-Ramírez, M.T.; Landero-Hernández, R. Síntomas de ansiedad, el manejo inadecuado de las emociones negativas y su asociación con bruxismo autoinformado. Ansiedad Estrés 2016, 22, 62–67. [Google Scholar] [CrossRef]
- Tavares, L.M.F.; da Silva Parente Macedo, L.C.; Duarte, C.M.R.; de Goffredo Filho, G.S.; de Souza Tesch, R. Cross-sectional study of anxiety symptoms and self-report of awake and sleep bruxism in female TMD patients. Cranio 2016, 34, 378–381. [Google Scholar] [CrossRef]
- Polmann, H.; Domingos, F.L.; Melo, G.; Stuginski-Barbosa, J.; da Silva Guerra, E.N.; Porporatti, A.L.; Dick, B.D.; Flores-Mir, C.; De Luca Canto, G. Association between sleep bruxism and anxiety symptoms in adults: A systematic review. J. Oral Rehabil. 2019, 46, 482–491. [Google Scholar] [CrossRef]
- Soto-Goñi, X.A.; Alen, F.; Buiza-González, L.; Marcolino-Cruz, D.; Sánchez-Sánchez, T.; Ardizone-García, I.; Aneiros-López, F.; Jiménez-Ortega, L. Adaptive Stress Coping in Awake Bruxism. Front. Neurol. 2020, 11, 564431. [Google Scholar] [CrossRef] [PubMed]
- Goulart, A.C.; Arap, A.M.; Bufarah, H.B.; Bismarchi, D.; Rienzo, M.; Syllos, D.H.; Wang, Y.-P. Anxiety, Depression, and Anger in Bruxism: A Cross-sectional Study among Adult Attendees of a Preventive Center. Psychiatry Res. 2021, 299, 113844. [Google Scholar] [CrossRef] [PubMed]
- Rofaeel, M.; Chow, J.C.-F.; Cioffi, I. The intensity of awake bruxism episodes is increased in individuals with high trait anxiety. Clin. Oral Investig. 2021, 25, 3197–3206. [Google Scholar] [CrossRef] [PubMed]
- Melo, G.; Duarte, J.; Pauletto, P.; Porporatti, A.L.; Stuginski-Barbosa, J.; Winocur, E.; Flores-Mir, C.; De Luca Canto, G. Bruxism: An umbrella review of systematic reviews. J. Oral Rehabil. 2019, 46, 666–690. [Google Scholar] [CrossRef]
- Paesani, D.A. Bruxismo: Teoría y Práctica, 1st ed.; Quintessence Publishing: Barcelona, Spain, 2012; 540p, ISBN 978-84-89873-50-6. [Google Scholar]
- Sánchez Romero, E.A.; Martínez-Pozas, O.; García-González, M.; de-Pedro, M.; González-Álvarez, M.E.; Esteban-González, P.; Cid-Verdejo, R.; Villafañe, J.H. Association between Sleep Disorders and Sleep Quality in Patients with Temporomandibular Joint Osteoarthritis: A Systematic Review. Biomedicines 2022, 10, 2143. [Google Scholar] [CrossRef]
- Tsai, C.-M.; Chou, S.-L.; Gale, E.N.; Mccall, W.D. Human masticatory muscle activity and jaw position under experimental stress. J. Oral Rehabil. 2002, 29, 44–51. [Google Scholar] [CrossRef]
- Imbriglio, T.V.; Moayedi, M.; Freeman, B.V.; Tenenbaum, H.C.; Thaut, M.; Cioffi, I. Music Modulates Awake Bruxism in Chronic Painful Temporomandibular Disorders. Headache J. Head Face Pain 2020, 60, 2389–2405. [Google Scholar] [CrossRef]
- Soto-Goñi, X.; García-Gonzalez, M.; Ardizone-García, I.; Sánchez-Sánchez, T.; Jiménez-Ortega, L. Altered electromyographic responses to emotional and pain information in awake bruxers: Case–control study. Clin. Oral Investig. 2022, 26, 4427–4435. [Google Scholar] [CrossRef]
- Haidar, S.A.; de Vries, N.K.; Karavetian, M.; El-Rassi, R. Stress, Anxiety, and Weight Gain among University and College Students: A Systematic Review. J. Acad. Nutr. Diet. 2018, 118, 261–274. [Google Scholar] [CrossRef]
- Berryhill, M.B.; Smith, J. College Student Chaotically-Disengaged Family Functioning, Depression, and Anxiety: The Indirect Effects of Positive Family Communication and Self-Compassion. Marriage Fam. Rev. 2021, 57, 1–23. [Google Scholar] [CrossRef]
- Fardin, M.A. COVID-19 and Anxiety: A Review of Psychological Impacts of Infectious Disease Outbreaks. Arch. Clin. Infect. Dis. 2020, 15, e102779. [Google Scholar] [CrossRef] [Green Version]
- Lakhan, R.; Agrawal, A.; Sharma, M. Prevalence of Depression, Anxiety, and Stress during COVID-19 Pandemic. J. Neurosci. Rural Pract. 2020, 11, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Romero, E.A.; Martínez Rolando, L.; Villafañe, J.H. Impact of Lockdown on Patients with Fibromyalgia. Electron. J. Gen. Med. 2022, 19, em366. [Google Scholar] [CrossRef] [PubMed]
- Castaldelli-Maia, J.M.; Marziali, M.E.; Lu, Z.; Martins, S.S. Investigating the effect of national government physical distancing measures on depression and anxiety during the COVID-19 pandemic through meta-analysis and meta-regression. Psychol. Med. 2021, 51, 881–893. [Google Scholar] [CrossRef] [PubMed]
- Winocur-Arias, O.; Winocur, E.; Shalev-Antsel, T.; Reiter, S.; Shifra, L.; Emodi-Perlman, A.; Friedman-Rubin, P. Painful Temporomandibular Disorders, Bruxism and Oral Parafunctions before and during the COVID-19 Pandemic Era: A Sex Comparison among Dental Patients. J. Clin. Med. 2022, 11, 589. [Google Scholar] [CrossRef]
- Emodi-Perlman, A.; Eli, I.; Smardz, J.; Uziel, N.; Wieckiewicz, G.; Gilon, E.; Grychowska, N.; Wieckiewicz, M. Temporomandibular Disorders and Bruxism Outbreak as a Possible Factor of Orofacial Pain Worsening during the COVID-19 Pandemic—Concomitant Research in Two Countries. J. Clin. Med. 2020, 9, 3250. [Google Scholar] [CrossRef]
- Pintado, M.R.; Anderson, G.C.; DeLong, R.; Douglas, W.H. Variation in tooth wear in young adults over a two-year period. J. Prosthet. Dent. 1997, 77, 313–320. [Google Scholar] [CrossRef]
- Przystańska, A.; Jasielska, A.; Ziarko, M.; Pobudek-Radzikowska, M.; Maciejewska-Szaniec, Z.; Prylińska-Czyżewska, A.; Wierzbik-Strońska, M.; Gorajska, M.; Czajka-Jakubowska, A. Psychosocial Predictors of Bruxism. BioMed Res. Int. 2019, 2019, 2069716. [Google Scholar] [CrossRef] [Green Version]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.E. STAI. Cuestionario de Ansiedad Estado-Rasgo, 9th ed.; TEA Ediciones: Madrid, Spain, 2015; ISBN 978-84-16231-15-7. [Google Scholar]
- Spielberger, C.D. IDER. Inventario de Depresión Estado/Rasgo; TEA Ediciones: Madrid, Spain, 2008; ISBN 978-84-7174-913-0. [Google Scholar]
- Derogatis, L. BSI-18, Inventario Breve de 18 Síntomas; Pearson—Clinical: Valencia, Spain, 2013; ISBN 978-84-15552-87-1. [Google Scholar]
- Moos, R.H. CRI-A: Inventario de Respuestas de Afrontamiento Para Adultos; TEA Ediciones: Madrid, Spain, 2010; ISBN 978-84-7174-885-0. [Google Scholar]
- Costa, P.T.; Mccrae, R.R. NEO PI-R. Inventario de Personalidad NEO Revisado. Inventario NEO Reducido de Cinco Factores (NEO-FII), 3rd ed.; TEA Ediciones: Madrid, Spain, 2008; ISBN 978-84-7174-917-8. [Google Scholar]
- Knowles, K.A.; Olatunji, B.O. Specificity of trait anxiety in anxiety and depression: Meta-analysis of the State-Trait Anxiety Inventory. Clin. Psychol. Rev. 2020, 82, 101928. [Google Scholar] [CrossRef]
- Agudelo Vélez, D.M.; Gómez Maquet, Y.; López, P.L. Propiedades Psicométricas del Inventario de Depresión Estado Rasgo (IDER) con una muestra de población general colombiana. Av. Psicol. Latinoam. 2014, 32, 71–84. [Google Scholar] [CrossRef]
- Govindasamy, P.; Green, K.E.; Olmos, A. Meta-analysis of the factor structure of the Brief Symptom Inventory (BSI-18) using an aggregated co-occurrence matrix approach. Ment. Health Rev. J. 2020, 25, 367–378. [Google Scholar] [CrossRef]
- Derogatis, L. SCL-90-R, Test de los 90 Síntomas; Pearson—Clinical: Valencia, Spain, 2012; ISBN 978-84-938543-8-6. [Google Scholar]
- Kirchner, T.; Forns, M.; Muñoz, D.; Pereda, N. Psychometric properties and dimensional structure of the Spanish version of the Coping Responses Inventory—Adult Form. Psicothema 2008, 20, 902–909. [Google Scholar] [PubMed]
- Aluja, A.; Blanch, A.; Solé, D.; Dolcet, J.-M.; Gallart, S. Versiones cortas del NEO-PI-R: El NEO-FFI frente al NEO-FFI-R. Behav. Psychol. Psicol. Conduct. 2009, 17, 335–350. [Google Scholar]
- Naing, N.N. Determination of sample size. Malays. J. Med. Sci. MJMS 2003, 10, 84–86. [Google Scholar]
- Chang, J.-J.; Ji, Y.; Li, Y.-H.; Pan, H.-F.; Su, P.-Y. Prevalence of anxiety symptom and depressive symptom among college students during COVID-19 pandemic: A meta-analysis. J. Affect. Disord. 2021, 292, 242–254. [Google Scholar] [CrossRef]
- Mehareen, J.; Rahman, M.A.; Dhira, T.A.; Sarker, A.R. Prevalence and socio-demographic correlates of depression, anxiety, and co-morbidity during COVID-19: A cross-sectional study among public and private university students of Bangladesh. J. Affect. Disord. Rep. 2021, 5, 100179. [Google Scholar] [CrossRef]
- Zhou, S.-J.; Wang, L.-L.; Qi, M.; Yang, X.-J.; Gao, L.; Zhang, S.-Y.; Zhang, L.-G.; Yang, R.; Chen, J.-X. Depression, Anxiety, and Suicidal Ideation in Chinese University Students During the COVID-19 Pandemic. Front. Psychol. 2021, 12, 669833. [Google Scholar] [CrossRef]
- Gambin, M.; Sękowski, M.; Woźniak-Prus, M.; Wnuk, A.; Oleksy, T.; Cudo, A.; Hansen, K.; Huflejt-Łukasik, M.; Kubicka, K.; Łyś, A.E.; et al. Generalized anxiety and depressive symptoms in various age groups during the COVID-19 lockdown in Poland. Specific predictors and differences in symptoms severity. Compr. Psychiatry 2021, 105, 152222. [Google Scholar] [CrossRef]
- Bellingtier, J.A.; Mund, M.; Wrzus, C. The role of extraversion and neuroticism for experiencing stress during the third wave of the COVID-19 pandemic. Curr. Psychol. 2021, 1–11. [Google Scholar] [CrossRef]
- Kroencke, L.; Geukes, K.; Utesch, T.; Kuper, N.; Back, M.D. Neuroticism and emotional risk during the COVID-19 pandemic. J. Res. Personal. 2020, 89, 104038. [Google Scholar] [CrossRef]
- Chopik, W.J.; Kitayama, S. Personality change across the life span: Insights from a cross-cultural, longitudinal study. J. Pers. 2018, 86, 508–521. [Google Scholar] [CrossRef] [PubMed]
- Allik, J.; Laidra, K.; Realo, A.; Pullmann, H. Personality development from 12 to 18 years of age: Changes in mean levels and structure of traits. Eur. J. Personal. 2004, 18, 445–462. [Google Scholar] [CrossRef]
- Lazarus, R.S. Stress, coping, and illness. In Personality and Disease; Wiley series on health psychology/behavioral medicine; John Wiley & Sons: Oxford, UK, 1990; pp. 97–120. ISBN 0-471-61805-5. [Google Scholar]
- Cavallo, P.; Carpinelli, L.; Savarese, G. Perceived stress and bruxism in university students. BMC Res. Notes 2016, 9, 514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serra-Negra, J.M.; Scarpelli, A.C.; Tirsa-Costa, D.; Guimarães, F.H.; Pordeus, I.A.; Paiva, S.M. Sleep Bruxism, Awake Bruxism and Sleep Quality among Brazilian Dental Students: A Cross-Sectional Study. Braz. Dent. J. 2014, 25, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Soares, L.G.; Costa, I.R.; Dos Santos Brum Júnior, J.; Cerqueira, W.S.B.; de Oliveira, E.S.; de Oliveira, D.W.D.; Gonçalves, P.F.; Glória, J.C.R.; Tavano, K.T.A.; Flecha, O.D. Prevalence of bruxism in undergraduate students. Cranio 2017, 35, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Yıldırım, B.; Kırarslan Karagoz, O.; Tekeli Simsek, A.; Koca, C.; Cicek, M.F. Associations between self-reported bruxism, sleep quality, and psychological status among dental students in Turkey. Cranio 2021, 1–6. [Google Scholar] [CrossRef]
- Koolhaas, J.M. Coping style and immunity in animals: Making sense of individual variation. Brain. Behav. Immun. 2008, 22, 662–667. [Google Scholar] [CrossRef] [Green Version]
- Koolhaas, J.M.; Bartolomucci, A.; Buwalda, B.; de Boer, S.F.; Flügge, G.; Korte, S.M.; Meerlo, P.; Murison, R.; Olivier, B.; Palanza, P.; et al. Stress revisited: A critical evaluation of the stress concept. Neurosci. Biobehav. Rev. 2011, 35, 1291–1301. [Google Scholar] [CrossRef]
- Zozulya, A.A.; Gabaeva, M.V.; Sokolov, O.Y.; Surkina, I.D.; Kost, N.V. Personality, Coping Style, and Constitutional Neuroimmunology. J. Immunotoxicol. 2008, 5, 221–225. [Google Scholar] [CrossRef]
- Genco, R.J.; Ho, A.W.; Grossi, S.G.; Dunford, R.G.; Tedesco, L.A. Relationship of Stress, Distress, and Inadequate Coping Behaviors to Periodontal Disease. J. Periodontol. 1999, 70, 711–723. [Google Scholar] [CrossRef]
- Manfredini, D.; Serra-Negra, J.; Carboncini, F.; Lobbezoo, F. Current Concepts of Bruxism. Int. J. Prosthodont. 2017, 30, 437–438. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jonsgar, C.; Hordvik, P.-A.; Berge, M.E.; Johansson, A.-K.; Svensson, P.; Johansson, A. Sleep bruxism in individuals with and without attrition-type tooth wear: An exploratory matched case-control electromyographic study. J. Dent. 2015, 43, 1504–1510. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Yu, F.; Niu, L.; Hu, W.; Long, Y.; Tay, F.R.; Chen, J. Associations among bruxism, gastroesophageal reflux disease, and tooth wear. J. Clin. Med. 2018, 7, 417. [Google Scholar] [CrossRef] [Green Version]
- Potvin, J.; Ramos Socarras, L.; Forest, G. Sleeping through a lockdown: How adolescents and young adults struggle with lifestyle and sleep habits upheaval during a pandemic. Behav. Sleep Med. 2022, 20, 304–320. [Google Scholar] [CrossRef]



| Scale (Questionnaire) Group | Average | Std | Square-Chi | p | Post-Hoc | z | p | |
|---|---|---|---|---|---|---|---|---|
| Anxiety State (STAI) | Pre-Pandemic (1) | 16.26 | 7.971 | 14.447 | 0.001 | (1) vs. (2) | −1.064 | 0.287 |
| Pandemic (2) | 18.29 | 10.314 | (2) vs. (3) | −2.375 | 0.018 | |||
| Post-restrictions (3) | 21.87 | 10.254 | (1) vs. (3) | −3.861 | 0.000 | |||
| Total | 18.81 | 9.816 | ||||||
| Anxiety Trait (STAI) | Pre-Pandemic (1) | 20.55 | 9.084 | 13.88 | 0.001 | (1) vs. (2) | −1.898 | 0.058 |
| Pandemic (2) | 23.07 | 9.102 | (2) vs. (3) | −2.061 | 0.039 | |||
| Post-restrictions (3) | 26.05 | 10.248 | (1) vs. (3) | −3.600 | 0.000 | |||
| Total | 23.22 | 9.726 | ||||||
| State Euthymia (ST/DEP) | Pre-Pandemic (1) | 10.82 | 3.147 | 2.26 | 0.323 | (1) vs. (2) | −1.476 | 0.140 |
| Pandemic (2) | 11.61 | 3.908 | (2) vs. (3) | −0.439 | 0.661 | |||
| Post-restrictions (3) | 11.44 | 4.177 | (1) vs. (3) | −1.006 | 0.315 | |||
| Total | 11.29 | 3.770 | ||||||
| State Dysthymia (ST/DEP) | Pre-Pandemic (1) | 6.65 | 1.997 | 3.162 | 0.206 | (1) vs. (2) | −0.241 | 0.810 |
| Pandemic (2) | 6.72 | 2.422 | (2) vs. (3) | −1.574 | 0.115 | |||
| Post-restrictions (3) | 7.20 | 2.544 | (1) vs. (3) | −1.481 | 0.139 | |||
| Total | 6.86 | 2.336 | ||||||
| Trait Euthymia (ST/DEP) | Pre-Pandemic (1) | 10.31 | 3.316 | 2.153 | 0.341 | (1) vs. (2) | −1.571 | 0.116 |
| Pandemic (2) | 10.80 | 3.209 | (2) vs. (3) | −0.400 | 0.689 | |||
| Post-restrictions (3) | 10.68 | 3.687 | (1) vs. (3) | −0.805 | 0.421 | |||
| Total | 10.60 | 3.405 | ||||||
| Trait Dysthymia (ST/DEP) | Pre-Pandemic (1) | 6.97 | 1.816 | 1.298 | 0.523 | (1) vs. (2) | −0.980 | 0.327 |
| Pandemic (2) | 7.33 | 2.293 | (2) vs. (3) | −0.074 | 0.941 | |||
| Post-restrictions (3) | 7.30 | 2.111 | (1) vs. (3) | −0.989 | 0.323 | |||
| Total | 7.20 | 2.081 | ||||||
| Somatization (BSI) | Pre-Pandemic (1) | 7.53 | 4.586 | 1.689 | 0.43 | (1) vs. (2) | −0.541 | 0.588 |
| Pandemic (2) | 8.57 | 7.196 | (2) vs. (3) | −0.615 | 0.539 | |||
| Post-restrictions (3) | 8.51 | 4.981 | (1) vs. (3) | −1.368 | 0.171 | |||
| Total | 8.20 | 5.697 | ||||||
| Depression (BSI) | Pre-Pandemic (1) | 6.66 | 4.890 | 7.128 | 0.028 | (1) vs. (2) | −2.404 | 0.016 |
| Pandemic (2) | 8.91 | 7.466 | (2) vs. (3) | −0.128 | 0.898 | |||
| Post-restrictions (3) | 8.33 | 5.398 | (1) vs. (3) | −2.207 | 0.027 | |||
| Total | 7.96 | 6.070 | ||||||
| Anxiety (BSI) | Pre-Pandemic (1) | 7.52 | 4.254 | 4.263 | 0.119 | (1) vs. (2) | −1.161 | 0.246 |
| Pandemic (2) | 9.24 | 7.967 | (2) vs. (3) | −0.714 | 0.475 | |||
| Post-restrictions (3) | 8.82 | 4.301 | (1) vs. (3) | −2.131 | 0.083 | |||
| Total | 8.53 | 5.792 | ||||||
| Logical Analysis (CRI) | Pre-Pandemic (1) | 11.131 | 2.8586 | 1.701 | 0.427 | (1) vs. (2) | −0.051 | 0.959 |
| Pandemic (2) | 11.156 | 3.1903 | (2) vs. (3) | −1.067 | 0.286 | |||
| Post-restrictions (3) | 11.612 | 3.1464 | (1) vs. (3) | −1.185 | 0.236 | |||
| Total | 11.300 | 3.0648 | ||||||
| Positive Reappraisal (CRI) | Pre-Pandemic (1) | 11.000 | 2.8206 | 6.421 | 0.04 | (1) vs. (2) | −0.831 | 0.406 |
| Pandemic (2) | 11.311 | 3.8443 | (2) vs. (3) | −1.559 | 0.119 | |||
| Post-restrictions (3) | 12.119 | 3.7183 | (1) vs. (3) | −2.551 | 0.011 | |||
| Total | 11.477 | 3.5087 | ||||||
| Seeking Guidance (CRI) | Pre-Pandemic (1) | 9.802 | 3.3241 | 0.363 | 0.834 | (1) vs. (2) | −0.517 | 0.605 |
| Pandemic (2) | 9.544 | 3.4516 | (2) vs. (3) | −0.277 | 0.782 | |||
| Post-restrictions (3) | 9.897 | 3.2118 | (1) vs. (3) | −0.464 | 0.642 | |||
| Total | 9.749 | 3.3212 | ||||||
| Problem Solving (CRI) | Pre-Pandemic (1) | 12.071 | 3.0492 | 1.238 | 0.538 | (1) vs. (2) | −0.143 | 0.886 |
| Pandemic (2) | 12.056 | 3.1493 | (2) vs. (3) | −1.002 | 0.317 | |||
| Post-restrictions (3) | 12.421 | 3.7580 | (1) vs. (3) | −0.913 | 0.361 | |||
| Total | 12.183 | 3.3262 | ||||||
| Cognitive Avoidance (CRI) | Pre-Pandemic (1) | 9.440 | 3.2803 | 1.61 | 0.447 | (1) vs. (2) | −1.248 | 0.212 |
| Pandemic (2) | 10.089 | 3.7286 | (2) vs. (3) | −0.244 | 0.807 | |||
| Post-restrictions (3) | 9.857 | 3.5373 | (1) vs. (3) | −0.892 | 0.372 | |||
| Total | 9.794 | 3.5167 | ||||||
| Acceptance/Resignation (CRI) | Pre-Pandemic (1) | 7.725 | 3.2492 | 9.028 | 0.011 | (1) vs. (2) | −2.524 | 0.012 |
| Pandemic (2) | 8.967 | 3.4882 | (2) vs. (3) | −0.264 | 0.792 | |||
| Post-restrictions (3) | 9.052 | 3.5152 | (1) vs. (3) | −2.658 | 0.008 | |||
| Total | 8.580 | 3.4606 | ||||||
| Seeking Alternative Reward (CRI) | Pre-Pandemic (1) | 8.104 | 3.5391 | 0.282 | 0.869 | (1) vs. (2) | −0.308 | 0.758 |
| Pandemic (2) | 8.267 | 3.4505 | (2) vs. (3) | −0.270 | 0.787 | |||
| Post-restrictions (3) | 8.459 | 3.4475 | (1) vs. (3) | −0.505 | 0.613 | |||
| Total | 8.277 | 3.4696 | ||||||
| Emotional Discharge (CRI) | Pre-Pandemic (1) | 7.093 | 3.1893 | 3.275 | 0.194 | (1) vs. (2) | −0.184 | 0.854 |
| Pandemic (2) | 6.967 | 3.3569 | (2) vs. (3) | −1.621 | 0.105 | |||
| Post-restrictions (3) | 7.759 | 3.1255 | (1) vs. (3) | −1.500 | 0.134 | |||
| Total | 7.274 | 3.2318 | ||||||
| Neuroticism (NEO) | Pre-Pandemic (1) | 21.21 | 7.894 | 9.722 | 0.008 | (1) vs. (2) | −1.639 | 0.101 |
| Pandemic (2) | 23.33 | 7.635 | (2) vs. (3) | −1.490 | 0.136 | |||
| Post-restrictions (3) | 24.84 | 6.534 | (1) vs. (3) | −3.105 | 0.002 | |||
| Total | 23.13 | 7.500 | ||||||
| Extraversion (NEO) | Pre-Pandemic (1) | 32.22 | 10.718 | 1.853 | 0.396 | (1) vs. (2) | −1.232 | 0.218 |
| Pandemic (2) | 30.28 | 8.148 | (2) vs. (3) | −0.442 | 0.658 | |||
| Post-restrictions (3) | 31.32 | 7.043 | (1) vs. (3) | −1.038 | 0.299 | |||
| Total | 31.28 | 8.778 | ||||||
| Openness (NEO) | Pre-Pandemic (1) | 29.80 | 7.140 | 3.546 | 0.17 | (1) vs. (2) | −1.808 | 0.071 |
| Pandemic (2) | 27.60 | 6.775 | (2) vs. (3) | −0.865 | 0.387 | |||
| Post-restrictions (3) | 28.54 | 6.588 | (1) vs. (3) | −1.140 | 0.254 | |||
| Total | 28.65 | 6.873 | ||||||
| Agreeableness (NEO) | Pre-Pandemic (1) | 30.65 | 5.890 | 6.42 | 0.04 | (1) vs. (2) | −1.415 | 0.157 |
| Pandemic (2) | 29.66 | 4.968 | (2) vs. (3) | −1.292 | 0.196 | |||
| Post-restrictions (3) | 28.42 | 5.879 | (1) vs. (3) | −2.441 | 0.015 | |||
| Total | 29.57 | 5.652 | ||||||
| Conscientiousness (NEO) | Pre-Pandemic (1) | 33.56 | 6.620 | 0.007 | 0.996 | (1) vs. (2) | −0.020 | 0.984 |
| Pandemic (2) | 33.67 | 6.316 | (2) vs. (3) | −0.121 | 0.904 | |||
| Post-restrictions (3) | 33.65 | 6.043 | (1) vs. (3) | −0.006 | 0.996 | |||
| Total | 33.63 | 6.308 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osses-Anguita, Á.E.; Sánchez-Sánchez, T.; Soto-Goñi, X.A.; García-González, M.; Alén Fariñas, F.; Cid-Verdejo, R.; Sánchez Romero, E.A.; Jiménez-Ortega, L. Awake and Sleep Bruxism Prevalence and Their Associated Psychological Factors in First-Year University Students: A Pre-Mid-Post COVID-19 Pandemic Comparison. Int. J. Environ. Res. Public Health 2023, 20, 2452. https://doi.org/10.3390/ijerph20032452
Osses-Anguita ÁE, Sánchez-Sánchez T, Soto-Goñi XA, García-González M, Alén Fariñas F, Cid-Verdejo R, Sánchez Romero EA, Jiménez-Ortega L. Awake and Sleep Bruxism Prevalence and Their Associated Psychological Factors in First-Year University Students: A Pre-Mid-Post COVID-19 Pandemic Comparison. International Journal of Environmental Research and Public Health. 2023; 20(3):2452. https://doi.org/10.3390/ijerph20032452
Chicago/Turabian StyleOsses-Anguita, Álvaro Edgardo, Teresa Sánchez-Sánchez, Xabier A. Soto-Goñi, María García-González, Francisco Alén Fariñas, Rosana Cid-Verdejo, Eleuterio A. Sánchez Romero, and Laura Jiménez-Ortega. 2023. "Awake and Sleep Bruxism Prevalence and Their Associated Psychological Factors in First-Year University Students: A Pre-Mid-Post COVID-19 Pandemic Comparison" International Journal of Environmental Research and Public Health 20, no. 3: 2452. https://doi.org/10.3390/ijerph20032452






