Models of Support for Caregivers and Patients with the Post-COVID-19 Condition: A Scoping Review
Abstract
1. Introduction
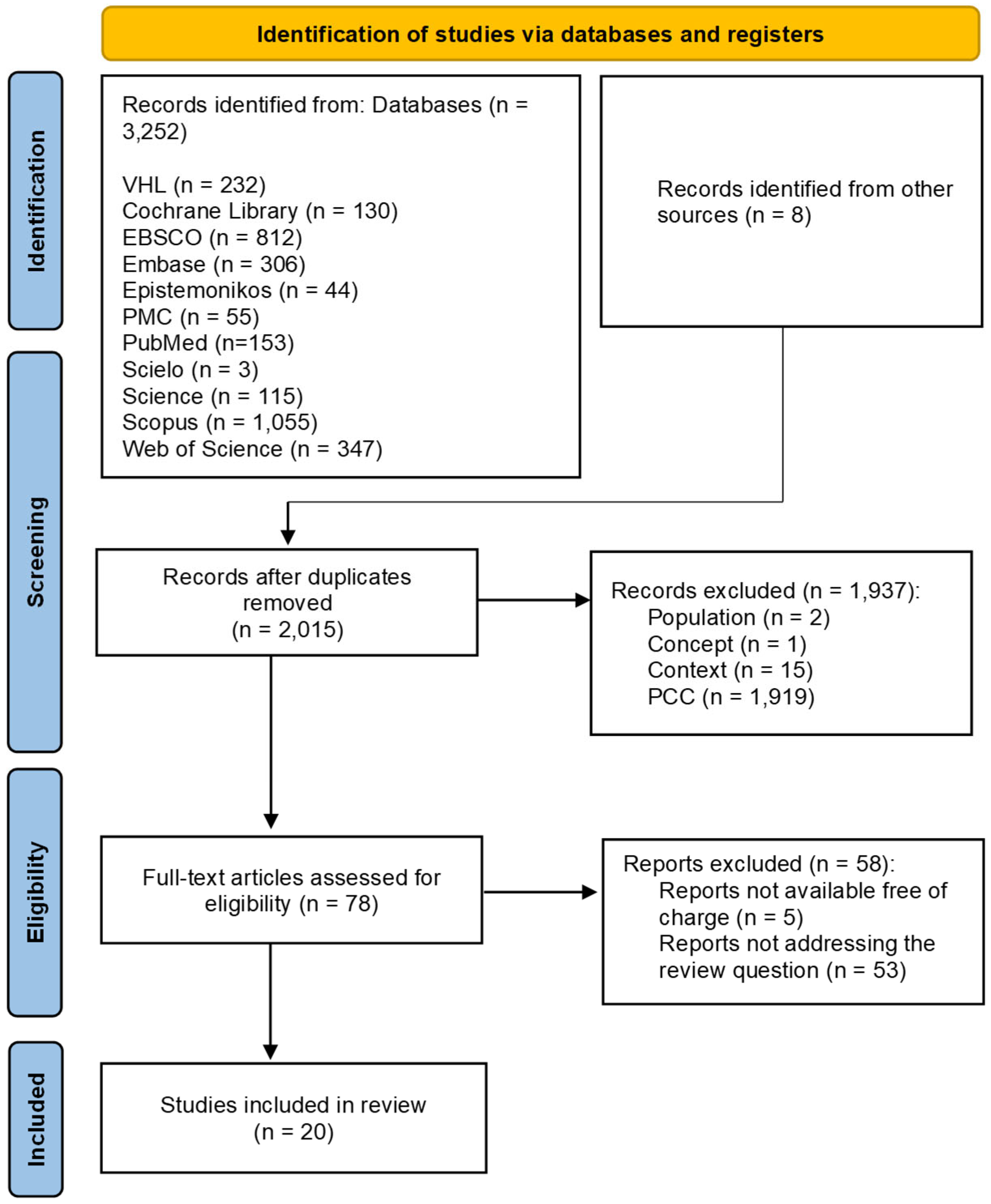
2. Materials and Methods
2.1. Study Design
2.2. Research Question
2.3. Search Strategy and Information Sources
2.4. Eligibility Criteria and Study Selection
2.5. Variables and Strategies to Avoid Bias
2.6. Presentation of Results
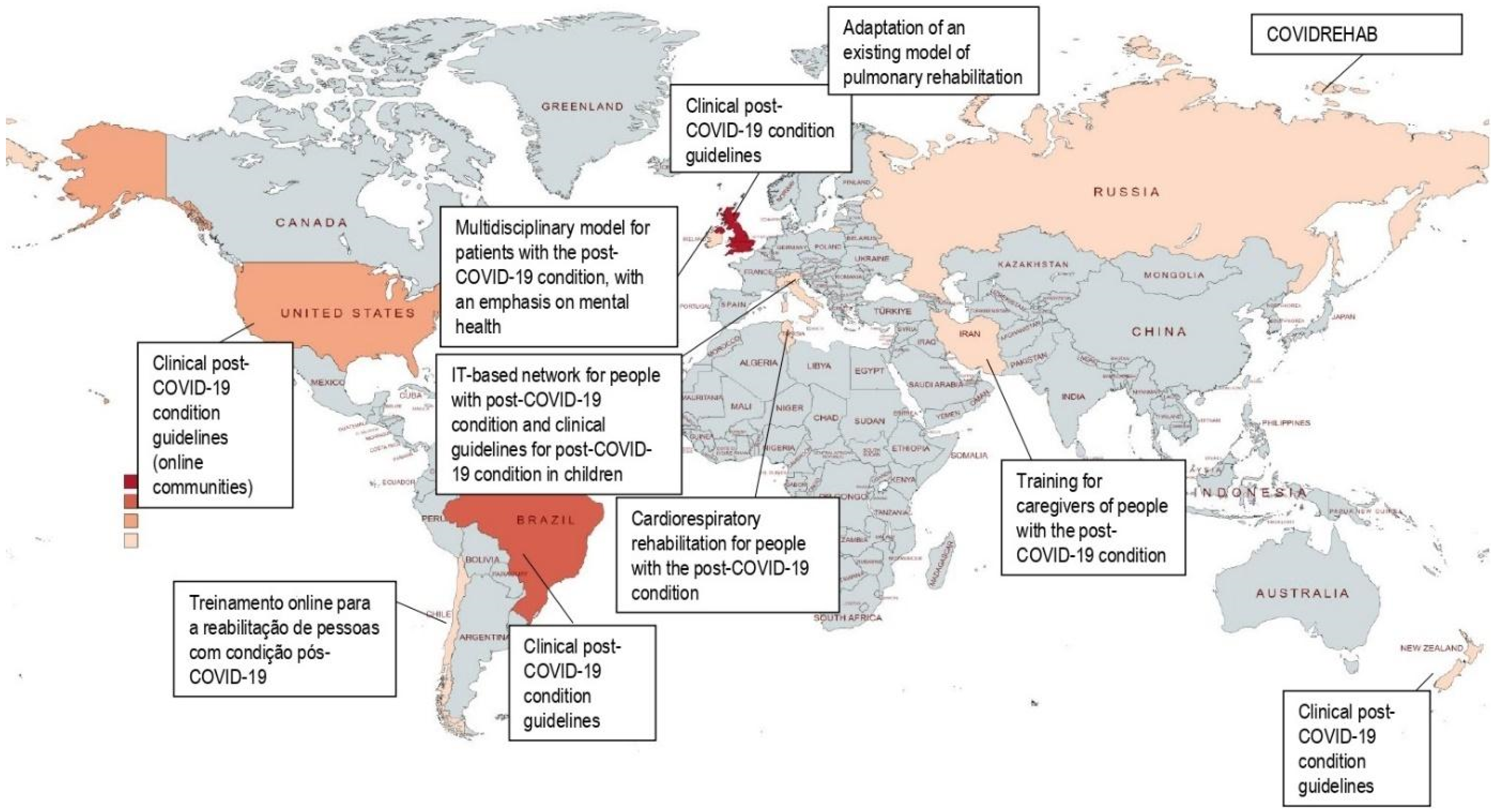
3. Results
3.1. Guidelines and Health Policies for the Post-COVID-19 Condition
3.2. Services and Home Support for Post-COVID-19 Condition Patients
3.3. Support Services for Home Caregivers of Patients with the Post-COVID-19 Condition
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Huang, L.; Yao, Q.; Gu, X.; Wang, Q.; Ren, L.; Wang, Y.; Hu, P.; Guo, L.; Liu, M.; Xu, J.; et al. 1-year outcomes in hospital survivors with COVID-19: A longitudinal cohort study. Lancet 2021, 398, 747–758. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Li, X.; Gu, X.; Zhang, H.; Ren, L.; Guo, L.; Liu, M.; Wang, Y.; Cui, D.; Wang, Y.; et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: A longitudinal cohort study. Lancet Respir Med. 2022, 10, 863–876. [Google Scholar] [CrossRef]
- Logue, J.K.; Franko, N.M.; McCulloch, D.J.; McDonald, D.; Magedson, A.; Wolf, C.R.; Chu, H.Y. Sequelae in adults at 6 months after COVID-19 infection. JAMA Netw. Open 2021, 4, e210830. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J. Clinical characteristics of 138 hospitalized patients with 2019 Novel Coronavirus—Infected Pneumonia in Wuhan, China. JAMA 2019, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Halaçli, B.; Topeli, A. Implementation of post-intensive care outpatient clinic (I-POINT) for critically ill COVID-19 survivors. Turk. J. Med. Sci. 2021, 51, 3350–3358. [Google Scholar] [CrossRef]
- De Felice, F.G.; Tovar-Moll, F.; Moll, J.; Munoz, D.P.; Ferreira, S.T. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the central nervous system. Trends Neurosci. 2020, 43, 355–357. [Google Scholar] [CrossRef]
- Besnier, F.; Bérubé, B.; Malo, J.; Gagnon, C.; Grégoire, C.-A.; Juneau, M.; Simard, F.; L’Allier, P.; Nigam, A.; Iglésies-Grau, J.; et al. Cardiopulmonary rehabilitation in long-COVID-19 patients with persistent breathlessness and fatigue: The COVID-rehab study. Int. J. Environ. Res. Public Health 2022, 19, 4133. [Google Scholar] [CrossRef]
- Sosa, J.V.C.; Gonzales, F.M.M.; Ramirez, Z.E.A.; Castro, M.C.; Huancahuire-Vega, S. Depression associated with caregiver quality of life in post-COVID-19 patients in two regions of Peru. Healthcare 2022, 10, 1219. [Google Scholar] [CrossRef]
- Azadvari, M.; Razavi, S.Z.E.; Hosseini, M.; Mayeli, M. Evaluation of the impact of the rehabilitation training on the knowledge and attitude of caregivers of COVID-19 patients in Iran. Acta Med. Iran. 2021, 59, 587–595. [Google Scholar] [CrossRef]
- Dias, J.F.; Grossi, J.B.; Costa, L.A.; Furtado, S.R.C.; Mancini, M.C.; Sampaio, R.F. Home care in rehabilitation and family-centered practice: Approaching theories to improve results. Rev. Ter. Ocup. Univ. São Paulo 2017, 28, 206–213. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Scoping reviews (2020 version). In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; Joanna Briggs Institute: Adelaide, Australia, 2020. [Google Scholar] [CrossRef]
- Brazilian Ministry of Health. Guia Prático do Cuidador—Série A—normas e Manuais Técnicos [Practical Guide for Caregivers—Volume A—Standards and Technical Manuals]; Brazilin Ministry of Health: Brasilia, Brazil, 2008. Available online: https://bvsms.saude.gov.br/bvs/publicacoes/guia_pratico_cuidador.pdf (accessed on 5 July 2022).
- World Health Organization. Clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. 2021. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1 (accessed on 5 July 2022).
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Pinto, M.; Gimigliano, F.; De Simone, S.; Costa, M.; Bianchi, A.A.M.; Iolascon, G. Post-acute COVID-19 rehabilitation network proposal: From intensive to extensive and home-based IT supported services. Int. J. Environ. Res. Public Health 2020, 17, 9335. [Google Scholar] [CrossRef]
- Munblit, D.; Nicholson, T.R.; Needham, D.M.; Seylanova, N.; Parr, C.; Chen, J.; Kokorina, A.; Sigfrid, L.; Buonsenso, D.; Bhatnagar, S.; et al. Studying the post-COVID-19 condition: Research challenges, strategies, and importance of Core Outcome Set development. BMC Med. 2022, 20, 50. [Google Scholar] [CrossRef]
- Brazilian Ministry of Health. Nota Técnica Nº 133/2021-CGAHD/DAHU/SAES/MS [Technical Note No. 133/2021-CGAHD/DAHU/SAES/MS]; Brazilian Ministry of Health: Brasilia, Brazil, 2021. Available online: https://www.gov.br/saude/pt-br/composicao/saes/dahu/arquivos/2022/nota-tecnica-133-2021-pos-covid-orientacoes.pdf (accessed on 10 October 2022).
- Center for Disease Control and Prevention. Long COVID or Post-COVID Conditions; Center for Disease Control and Prevention: Atlanta, Australia, 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html#print (accessed on 20 September 2022).
- United Kingdom National Health Service. Long COVID: The NHS Plan for 2021/2022; National Health Service: London, UK, 2021; Available online: https://www.england.nhs.uk/coronavirus/publication/long-covid-the-nhs-plan-for-2021-22/ (accessed on 16 August 2022).
- Ministry of Health of New Zealand. Long COVID: Funding for Primary Care; Ministry of Health of New Zealand: Auckland, New Zealand, 2021. Available online: https://www.health.govt.nz/ (accessed on 31 July 2022).
- Esposito, S.; Principi, N.; Azzari, C.; Cardinale, F.; Di Mauro, G.; Galli, L.; Gattinara, G.C.; Fainardi, V.; Guarino, A.; Lancella, L.; et al. Italian intersociety consensus on management of long COVID in children. Ital. J. Pediatr. 2022, 48, 42. [Google Scholar] [CrossRef]
- Singh, S.J.; Barradell, A.C.; Greening, N.J.; Bolton, C.; Jenkins, G.; Preston, L.; Hurst, J.R. British Thoracic Society survey of rehabilitation to support recovery of the post-COVID-19 population. BMJ Open 2020, 10, e040213. [Google Scholar] [CrossRef]
- Fowler-Davis, S.; Young, R.; Maden-Wilkinson, T.; Hameed, W.; Dracas, E.; Hurrell, E.; Bahl, R.; Kilcourse, E.; Robinson, R.; Copeland, R. Assessing the acceptability of a co-produced long COVID intervention in an underserved community in the UK. Int. J. Environ. Res. Public Health 2021, 18, 13191. [Google Scholar] [CrossRef]
- Gilmutdinova, I.R.; Kolyshenkov, V.A.; Lapickaya, K.A.; Trepova, A.S.; Vasileva, V.A.; Prosvirnin, A.N.; Marchenkova, L.A.; Terentev, K.V.; Yakovlev, M.Y.; Rachin, A.P.; et al. Telemedicine platform COVIDREHAB for remote rehabilitation of patients after COVID-19. Eur. J. Transl. Myol. 2021, 31, 9783. [Google Scholar] [CrossRef]
- O’Brien, H.; Tracey, M.J.; Ottewill, C.; O’Brien, M.E.; Morgan, R.K.; Costello, R.W.; Gunaratnam, C.; Ryan, D.; McElvaney, N.G.; McConkey, S.J.; et al. An integrated multidisciplinary model of COVID-19 recovery care. Ir. J. Med. Sci. 2021, 190, 461–468. [Google Scholar] [CrossRef]
- Razai, M.S.; Al-Bedaery, R.; Anand, L.; Fitch, K.; Okechukwu, H.; Saraki, T.M.; Oakeshott, P. Patients’ experiences of “long COVID” in the community and recommendations for improving services: A quality improvement survey. J. Prim. Care Community Health 2021, 12, 21501327211041846. [Google Scholar] [CrossRef]
- Salawu, A.; Green, A.; Crooks, M.G.; Brixey, N.; Ross, D.H.; Sivan, M. A Proposal for multidisciplinary tele-rehabilitation in the assessment and rehabilitation of COVID-19 survivors. Int. J. Environ. Res. Public Health 2020, 17, 4890. [Google Scholar] [CrossRef] [PubMed]
- Santana, A.V.; Fontana, A.D.; Pitta, F. Pulmonary rehabilitation after COVID-19. J. Bras. Pneumol. 2021, 47, e20210034. [Google Scholar] [CrossRef] [PubMed]
- Santos Filho, A.; Dourado, P.; Lima, A.; Vieira, L. Reabilitação pós COVID-19 [Post COVID-19 Rehabilitation]; Health Department: Goiania, Brazil, 2020. Available online: https://www.saude.go.gov.br/files//conecta-sus/produtos-tecnicos/III%20-%202020/COVID-19%20-%20S%C3%ADndrome%20P%C3%B3s%20COVID-19%20Reabilita%C3%A7%C3%A3o.pdf (accessed on 4 November 2022).
- Benzarti, W.; Toulgui, E.; Prefaut, C.; Chamari, K.; Ben Saad, H. General practitioners should provide the cardiorespiratory rehabilitation’ ‘minimum advice’ for long COVID-19 patients. Libyan J. Med. 2022, 17, 2009101. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health of Chile. Hospital Digital Inicia Ciclo de Charlas en Línea Dirigido a Personas en Rehabilitación Post COVID-19 [Hospital Digital Starts a Cycle of Online Talks Aimed at People Undergoing Post-COVID-19 Rehabilitation]; Ministry of Health of Chile: Santiago, Chile, 2021; Available online: https://www.minsal.cl/ (accessed on 17 July 2021).
- Russell, D.; Spence, N.J.; Chase, J.-A.D.; Schwartz, T.; Tumminello, C.M.; Bouldin, E. Support amid uncertainty: Long COVID illness experiences and the role of online communities. SSM Qual. Res. Health 2022, 2, 100177. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Rehabilitation 2030 Initiative; World Health Organization: Goiania, Brazil, 2017; Available online: https://www.who.int/initiatives/rehabilitation-2030 (accessed on 4 November 2022).
- Pan American Health Organization. Rehabilitation Considerations during the COVID-19 Outbreak; Pan American Health Organization: Washington, DC, USA, 2020; Available online: https://iris.paho.org/handle/10665.2/52035 (accessed on 10 October 2022).
- Dias, C.S.; Camelier, F.W.R.; Santos, M.L.M. Recomendações Para a Atuação dos Fisioterapeutas no âmbito da Atenção Primária à Saúde (APS) de Pacientes Suspeitos ou Diagnosticados com COVID-19 [Recommendations for the Intervention of Two Physiotherapists Outside the Scope of Primary Health Care of Patients Suspected or Diagnosed with COVID-19]; Brazilian Association of Cardiorespiratory Physiotherapy and Intensive Care Physiotherapy: Sao Paulo, Brazil, 2020; Available online: https://assobrafir.com.br/wp-content/uploads/2020/06/ASSOBRAFIR_COVID-19_APS_2020.06.01.pdf (accessed on 10 October 2022).
- Smith, B.; Magnani, J.W. New technologies, new disparities: The intersection of electronic health and digital health literacy. Int. J. Cardiol. 2019, 292, 280–282. [Google Scholar] [CrossRef]
- Kim, Y.; Carver, C.S.; Ting, A. Family caregivers’ unmet needs in long-term cancer survivorship. Semin. Oncol. Nurs. 2019, 35, 380–383. [Google Scholar] [CrossRef]
- Nobre, I.N.; Lemos, C.S.; Pardini, A.C.G.; Carvalho, J.; Salles, I.C.D. Anxiety, depression, and hopelessness in family caregivers of patients with neuropsychoological sequelae. Acta Fisiatr. 2015, 22, 160–165. [Google Scholar] [CrossRef]
- Yoon, H.K.; Kim, G.S. An empowerment program for family caregivers of people with dementia. Public Health Nurs. 2019, 37, 222–233. [Google Scholar] [CrossRef]
- Berry, L.L.; Dalwadi, S.M.; Jacobson, J.O. Supporting the Supporters: What family caregivers need to care for a loved one with cancer. J. Oncol. Pract. 2017, 13, 35–41. [Google Scholar] [CrossRef]
- Khan, T.S.; Hirschman, K.B.; McHugh, M.D.; Naylor, M.D. Self-efficacy of family caregivers of older adults with cognitive impairment: A concept analysis. Nurs. Forum. 2021, 56, 112–126. [Google Scholar] [CrossRef]
| PCC | Definitions | |
|---|---|---|
| Population | Patients with the post-COVID-19 condition | People with neuropsychiatric, motor, or cardiopulmonary sequelae due to COVID-19 infection and who, from this, have some functional dependence to perform their daily activities [1]. |
| Home caregiver | Someone who takes care of the objectives established by a specialized institution or a directly responsible person. Their function ensures the assisted person’s well-being, health, food, personal hygiene, education, culture, recreation, and leisure. The person in the family or community provides care to another person of any age who requires care due to physical or mental limitations, with or without remuneration [13]. | |
| Concept | Models of organization of support and home support | Structured services include specific care actions for people, families, and caregivers to offer adequate conditions for care to preserve family and social life [13]. |
| Context | Post-COVID-19 Condition | Illness that occurs in individuals with a history of probable or confirmed infection with SARS-CoV-2, usually 3 months after the onset of COVID-19, with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis. Common symptoms include fatigue, shortness of breath, and cognitive dysfunction [14]. |
| Search | Query | Results |
|---|---|---|
| #1 | “Caregivers”[mh] OR Caregiver*[tiab] OR Carer**[tiab] OR “Care Givers”[tiab] OR “Care Giver”[tiab] OR family care*[tiab] OR “unpaid care”[tiab] OR informal care*[tiab] OR “Family”[mh] OR Families[tiab] OR Filiation[tiab] OR relatives[tiab] OR Stepfamil*[tiab] OR Parent*[tiab] OR “Step Parents”[tiab] OR Step-Parent[tiab] OR Step-Parent*[tiab] OR Stepparent*[tiab] OR maternity[tiab] OR motherhood[tiab] OR parenthood[tiab] OR paternity[tiab] OR “mothers”[mh] OR “Fathers”[mh] OR “mothers”[tiab] OR ”Fathers”[tiab] Sort by: Most Recent | 1,128,550 |
| #2 | “Social Support”[mh] OR “Social Support”[tiab] OR “Social Care”[tiab] OR “Psychosocial Support Systems”[tiab] OR “Psychological Support System”[tiab] OR “Psychological Support Systems”[tiab] OR “Psychosocial Support”[tiab] OR “Psychosocial Support System”[tiab] OR “Psychosocial Supports”[tiab] OR “Social Support System”[tiab] OR “Social Support Systems”[tiab] OR “Home Nursing”[mh] OR “home nursing”[tiab] OR “Non-Professional Home Care”[tiab] OR “Nonprofessional Home Care”[tiab] OR “Home Care Services”[tiab] OR “Domiciliary Care”[tiab] OR “Domiciliary Care”[tiab]”Home Care”[tiab] OR “Home Care Service” OR “Home Health Care” OR “Home Care Services, Hospital-Based”[mh] OR “Hospital Based Home Care”[tiab] OR “Hospital Based Home Care Services”[tiab] OR “Hospital Based Home Cares”[tiab] OR “Hospital Home Care Services”[tiab] OR “Hospital-Based Home Care”[tiab] OR “Hospital-Based Home Care Services”[tiab] OR “Hospital-Based Home Cares”[tiab] OR “Orientation”[mh] OR Orientation*[tiab] OR support[tiab] OR “Patient Care”[mh] OR “Informal care”[tiab] OR “Informal cares”[tiab] OR “Health Services”[mh] OR “Health Service”[tiab] OR “Rehabilitation”[mh] OR “Rehabilitation Centers”[mh] OR Rehabilitation Center*[tiab] OR Long-term care facilities[tiab] OR “Long term care”[tiab] OR “Long-Term Care”[mh] Sort by: Most Recent | 3,730,959 |
| #3 | ((COVID-19[mh] OR “COVID 19”[tiab] OR “SARS-CoV-2”[tiab] OR “Novel Coronavirus”[tiab] OR 2019-nCoV[tiab] OR “Coronavirus Disease 2019”[tiab] OR “Coronavirus Disease-19”[tiab] OR “Coronavirus Disease 19”[tiab] OR “Severe Acute Respiratory Syndrome Coronavirus 2 Infection”[tiab] OR “SARS Coronavirus 2 Infection”[tiab] OR “2019 nCoV”[tiab] OR COVID19[tiab] OR SARS-CoV-2[tiab] OR “SARS Coronavirus 2 Infection”[tiab] OR “Wuhan Coronavirus”[tiab] OR SARS-CoV-2[tiab]) AND (complication[tiab] OR “associated conditions”[tiab] OR “associated disease”[tiab] OR “coexistent conditions”[tiab] OR “coexistent disease”[tiab] OR “concomitant conditions”[tiab] OR “concomitant disease”[tiab] OR sequelae[tiab] OR sequel*[tiab])) OR “COVID-19 sequalae”[tiab] OR “Core Outcome Set”[tiab] OR “Long COVID”[tiab] OR Post-COVID-19[tiab] OR “Post-acute sequelae of SARS-CoV-2 infection”[tiab] OR “Post COVID 19”[tiab] OR “chronic COVID syndrome”[tiab] OR “chronic COVID-19”[tiab] OR “COVID long-hauler”[tiab] OR “long haul COVID”[tiab] OR “long hauler COVID”[tiab] OR “post COVID 19 fatigue”[tiab] OR “post COVID 19 neurological syndrome”[tiab] OR “post COVID 19 syndrome”[tiab] OR “post COVID fatigue”[tiab] OR “post COVID syndrome”[tiab] OR “post-acute COVID syndrome”[tiab] OR “post-acute COVID-19”[tiab] OR “post-acute COVID-19 syndrome”[nm] OR “post-acute COVID-19 syndrome”[tiab] OR long-COVID [tiab] OR “long-haul COVID”[tiab] OR “persistent COVID-19”[tiab] OR “post-acute COVID19 syndrome”[tiab] Sort by: Most Recent | 10,299 |
| #4 | #1 AND #2 AND #3 Sort by: Most Recent | 142 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cavalcante, T.F.; Lourenço, C.E.; Ferreira, J.E.d.S.M.; Oliveira, L.R.; Neto, J.C.; Amaro, J.P.; Moreira, R.P. Models of Support for Caregivers and Patients with the Post-COVID-19 Condition: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 2563. https://doi.org/10.3390/ijerph20032563
Cavalcante TF, Lourenço CE, Ferreira JEdSM, Oliveira LR, Neto JC, Amaro JP, Moreira RP. Models of Support for Caregivers and Patients with the Post-COVID-19 Condition: A Scoping Review. International Journal of Environmental Research and Public Health. 2023; 20(3):2563. https://doi.org/10.3390/ijerph20032563
Chicago/Turabian StyleCavalcante, Tahissa Frota, Caroline Evaristo Lourenço, José Erivelton de Souza Maciel Ferreira, Lídia Rocha Oliveira, João Cruz Neto, Josemberg Pereira Amaro, and Rafaella Pessoa Moreira. 2023. "Models of Support for Caregivers and Patients with the Post-COVID-19 Condition: A Scoping Review" International Journal of Environmental Research and Public Health 20, no. 3: 2563. https://doi.org/10.3390/ijerph20032563
APA StyleCavalcante, T. F., Lourenço, C. E., Ferreira, J. E. d. S. M., Oliveira, L. R., Neto, J. C., Amaro, J. P., & Moreira, R. P. (2023). Models of Support for Caregivers and Patients with the Post-COVID-19 Condition: A Scoping Review. International Journal of Environmental Research and Public Health, 20(3), 2563. https://doi.org/10.3390/ijerph20032563










