Increased Substance Use among Nurses during the COVID-19 Pandemic
Abstract
:1. Introduction
1.1. Workplace Cognitive Failure
1.2. Substance Use
1.3. Present Study
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Measures
2.3.1. Patient Health Questionnaire–9 (PHQ-9)
2.3.2. Generalized Anxiety Disorder–7 (GAD-7)
2.3.3. PTSD Checklist (PCL-6)
2.3.4. Stress and Sleep Quality
2.3.5. Secondary Trauma
2.3.6. Work-Related Exhaustion
2.3.7. Workplace Cognitive Failure Scale (WCFS)
2.4. Statistical Analysis
3. Results
3.1. Description of the Sample
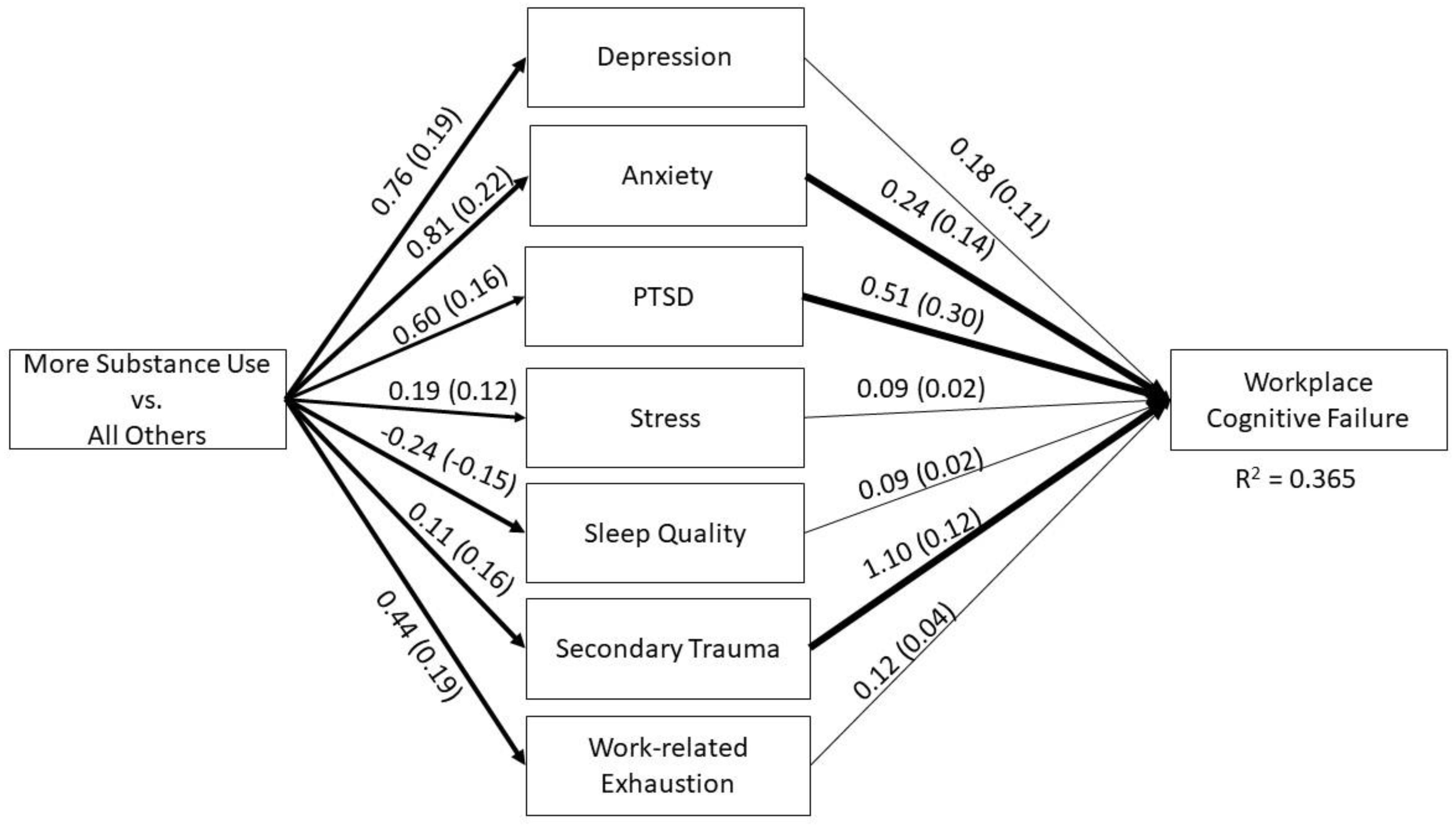
3.2. Psycho-Affective Symptoms Mediate Effects of Increased Substance Use on Workplace Cognitive Failure
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sun, N.; Wei, L.; Shi, S.; Jiao, D.; Song, R.; Ma, L.; Wang, H. A Qualitative Study on the Psychological Experience of Caregivers of COVID-19 Patients. Am. J. Infect. Control 2020, 48, 592–598. [Google Scholar] [CrossRef]
- Arnetz, J.E.; Goetz, C.M.; Arnetz, B.B.; Arble, E. Nurse Reports of Stressful Situations during the COVID-19 Pandemic: Qualitative Analysis of Survey Responses. Int. J. Environ. Res. Public Health 2020, 17, 8126. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of Depression, Anxiety, and Insomnia among Healthcare Workers during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Pacitti, F.; Lorenzo, G.; Marco, A.; Siracusano, A.; Rossi, A. Mental Health Outcomes among Frontline and Second-Line Health Care Workers during the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Netw. Open 2020, 3, 2010185. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Hu, S. Factors Associated with Mental Health Outcomes among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, 203976. [Google Scholar] [CrossRef] [PubMed]
- Marvaldi, M.; Mallet, J.; Dubertret, C.; Moro, M.R.; Guessoum, S.B. Anxiety, Depression, Trauma-Related, and Sleep Disorders among Healthcare Workers during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Neurosci. Biobehav. Rev. 2021, 126, 252–264. [Google Scholar] [CrossRef] [PubMed]
- Murat, M.; Köse, S.; Savaşer, S. Determination of Stress, Depression and Burnout Levels of Front-line Nurses during the COVID-19 Pandemic. Int. J. Ment. Health Nurs. 2021, 30, 533–543. [Google Scholar] [CrossRef]
- Arnetz, J.E.; Arble, E.; Sudan, S.; Arnetz, B.B. Workplace Cognitive Failure among Nurses during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 10394. [Google Scholar] [CrossRef]
- Park, Y.M.; Kim, S.Y. Impacts of Job Stress and Cognitive Failure on Patient Safety Incidents among Hospital Nurses. Saf. Health Work 2013, 4, 210–215. [Google Scholar] [CrossRef]
- Broadbent, D.E.; Cooper, P.F.; FitzGerald, P.; Parkes, K.R. The Cognitive Failures Questionnaire (CFQ) and Its Correlates. Br. J. Clin. Psychol. 1982, 21, 1–16. [Google Scholar] [CrossRef]
- Hodgkinson, G.P. The Interface of Cognitive and Industrial, Work and Organizational Psychology. J. Occup. Organ. Psychol. 2003, 76, 1–25. [Google Scholar] [CrossRef]
- Day, A.J.; Brasher, K.; Bridger, R.S. Accident Proneness Revisited: The Role of Psychological Stress and Cognitive Failure. Accid. Anal. Prev. 2012, 49, 532–535. [Google Scholar] [CrossRef]
- Wallace, J.C.; Chen, G. Development and Validation of a Work-specific Measure of Cognitive Failure: Implications for Occupational Safety. J. Occup. Organ. Psychol. 2005, 78, 615–632. [Google Scholar] [CrossRef]
- Elfering, A.; Grebner, S.; Dudan, A. Job Characteristics in Nursing and Cognitive Failure at Work. Saf. Health Work 2011, 2, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Kakemam, E.; Kalhor, R.; Khakdel, Z.; Khezri, A.; West, S.; Visentin, D.; Cleary, M. Occupational Stress and Cognitive Failure of Nurses and Associations with Self-reported Adverse Events: A National Cross-sectional Survey. J. Adv. Nurs. 2019, 75, 3609–3618. [Google Scholar] [CrossRef] [PubMed]
- Martínez-López, J.Á.; Lázaro-Pérez, C.; Gómez-Galán, J.; Fernández-Martínez, M.D.M. Psychological Impact of COVID-19 Emergency on Health Professionals: Burnout Incidence at the Most Critical Period in Spain. J. Clin. Med. 2020, 9, 3029. [Google Scholar] [CrossRef] [PubMed]
- González-Gil, M.T.; González-Blázquez, C.; Parro-Moreno, A.I.; Pedraz-Marcos, A.; Palmar-Santos, A.; Otero-García, L.; Oter-Quintana, C. Nurses’ Perceptions and Demands Regarding COVID-19 Care Delivery in Critical Care Units and Hospital Emergency Services. Intensive Crit. Care Nurs. 2021, 62, 102966. [Google Scholar] [CrossRef]
- Maben, J.; Bridges, J. Covid-19: Supporting Nurses’ Psychological and Mental Health. J. Clin. Nurs. Accept.-Artic. 2020, 29, 2742. [Google Scholar] [CrossRef]
- Ramaci, T.; Barattucci, M.; Ledda, C.; Rapisarda, V. Social Stigma during COVID-19 and Its Impact on HCWs Outcomes. Sustainability 2020, 12, 3834. [Google Scholar] [CrossRef]
- Foli, K.J.; Zhang, L.; Reddick, B. Predictors of Substance Use in Registered Nurses: The Role of Psychological Trauma. West. J. Nurs. Res. 2021, 43, 1023–1033. [Google Scholar] [CrossRef]
- Brady, K.T.; Back, S.E.; Coffey, S.F. Substance abuse and posttraumatic stress disorder. Curr. Dir. Psychol. Sci. 2004, 13, 206–209. [Google Scholar] [CrossRef]
- Pietrzak, R.H.; Goldstein, R.B.; Southwick, S.M.; Grant, B.F. Prevalence and Axis I Comorbidity of Full and Partial Posttraumatic Stress Disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J. Anxiety Disord. 2011, 25, 456–465. [Google Scholar] [CrossRef]
- Reynolds, M.; Hinchliffe, K.; Asamoah, V.; Kouimtsidis, C. Trauma and Post-Traumatic Stress Disorder in a Drug Treatment Community Service. Psychiatrist 2011, 35, 256–260. [Google Scholar] [CrossRef]
- Schäfer, I.; Najavits, L.M. Clinical Challenges in the Treatment of Patients with Posttraumatic Stress Disorder and Substance Abuse. Curr. Opin. Psychiatry 2007, 20, 614–618. [Google Scholar] [CrossRef]
- Kline, A.; Weiner, M.D.; Ciccone, D.S.; Interian, A.; Hill, L.S.; Losonczy, M. Increased Risk of Alcohol Dependency in a Cohort of National Guard Troops with PTSD: A Longitudinal Study. J. Psychiatr. Res. 2014, 50, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Ehring, T.; Quack, D. Emotion Regulation Difficulties in Trauma Survivors: The Role of Trauma Type and PTSD Symptom Severity. Behav. Ther. 2010, 41, 587–598. [Google Scholar] [CrossRef]
- Kober, H. Emotion Regulation in Substance Use Disorders. In Handbook of Emotion Regulation; Gross, J.J., Ed.; The Guilford Press: New York, NY, USA, 2014; pp. 428–446. [Google Scholar]
- Arble, E.; Arnetz, B.B. A Model of First-responder Coping: An Approach/Avoidance Bifurcation. Stress Health 2017, 33, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Trinkoff, A.M.; Storr, C.L. Substance Use among Nurses: Differences between Specialties. Am. J. Public Health 1998, 88, 581–585. [Google Scholar] [CrossRef] [PubMed]
- Worley, J. Nurses with Substance Use Disorders: Where We Are and What Needs to Be Done. J. Psychosoc. Nurs. Ment. Health Serv. 2017, 55, 11. [Google Scholar] [CrossRef] [PubMed]
- Foli, K.J.; Reddick, B.; Zhang, L.; Krcelich, K. Substance Use in Registered Nurses: “I Heard About a Nurse Who …”. J. Am. Psychiatr. Nurses Assoc. 2020, 26, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Choflet, A.; Davidson, J.; Lee, K.C.; Ye, G.; Barnes, A.; Zisook, S. A Comparative Analysis of the Substance Use and Mental Health Characteristics of Nurses Who Complete Suicide. J. Clin. Nurs. 2021, 30, 1963–1972. [Google Scholar] [CrossRef] [PubMed]
- Foli, K.J.; Forster, A.; Cheng, C.; Zhang, L.; Chiu, Y.C. Voices from the COVID-19 Frontline: Nurses’ Trauma and Coping. J. Adv. Nurs. 2021, 77, 3853–3866. [Google Scholar] [CrossRef]
- Rathburn, J. Destigmatizing alcohol use disorder among nurses. Nursing 2022, 52, 23. [Google Scholar] [CrossRef] [PubMed]
- Regehr, C.; LeBlanc, V.R. PTSD, Acute Stress, Performance and Decision-Making in Emergency Service Workers. J. Am. Acad. Psychiatry Law 2017, 45, 184–192. [Google Scholar]
- Carrigan, N.; Barkus, E. A Systematic Review of the Relationship between Psychological Disorders or Substance Use and Self-Reported Cognitive Failures. Cogn. Neuropsychiatry 2016, 21, 539–564. [Google Scholar] [CrossRef] [PubMed]
- Dalgaard, L.; Eskildsen, A.; Carstensen, O.; Willert, M.V.; Andersen, J.H.; Glasscock, D.J. Changes in Self-Reported Sleep and Cognitive Failures: A Randomized Controlled Trial of a Stress Management Intervention. Scand. J. Work Environ. Health 2014, 40, 569–581. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092. [Google Scholar] [CrossRef]
- Lang, A.J.; Stein, M.B. An Abbreviated PTSD Checklist for Use as a Screening Instrument in Primary Care. Behav. Res. Ther. 2005, 43, 585–594. [Google Scholar] [CrossRef]
- Arnetz, B.B.; Broadbridge, C.L.; Ghosh, S. Longitudinal determinants of energy levels in knowledge workers. J. Occup. Environ. Med. 2014, 56, 79–85. [Google Scholar] [CrossRef]
- Stamm, B.H. The Concise ProQOL Manual; The ProQOL. org.: Pocatello, ID, USA, 2011. [Google Scholar]
- Arnetz, B.B. Physicians’ View of Their Work Environment and Organisation. Psychother. Psychosom. 1997, 66, 155–162. [Google Scholar] [CrossRef]
- IBM. SPSS Statistics for Windows; IBM: Armonk, NY, USA, 2020. [Google Scholar]
- Muthen, L.; Muthen, B. Mplus User’s Guide, 7th ed.; Muthen & Muthen: Los Angeles, CA, USA, 2012. [Google Scholar]
- Bentler, P.M.; Bonett, D.G. Significance Tests and Goodness of Fit in the Analysis of Covariance Structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- Raykov, T.; Marcoulides, G.A. A First Course in Structural Equation Modeling, 2nd ed.; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 2006; ISBN 978-0-8058-5587-6. [Google Scholar]
- Hayes, A.F.; Scharkow, M. The Relative Trustworthiness of Inferential Tests of the Indirect Effect in Statistical Mediation Analysis: Does Method Really Matter? Psychol. Sci. 2013, 24, 1918–1927. [Google Scholar] [CrossRef]
- Little, T.D.; Jorgensen, T.D.; Lang, K.M.; Moore, E.W.G. On the Joys of Missing Data. J. Pediatr. Psychol. 2014, 39, 151–162. [Google Scholar] [CrossRef]
- Monroe, T.B.; Kenaga, H.; Dietrich, M.S.; Carter, M.A.; Cowan, R.L. The Prevalence of Employed Nurses Identified or Enrolled in Substance Use Monitoring Programs. Nurs. Res. 2013, 62, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Richter, K.; Peter, L.; Rodenbeck, A.; Weess, H.G.; Riedel-Heller, S.G.; Hillemacher, T. Shiftwork and Alcohol Consumption: A Systematic Review of the Literature. Eur. Addict. Res. 2021, 27, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Kunyk, D. Substance Use Disorders among Registered Nurses: Prevalence, Risks and Perceptions in a Disciplinary Jurisdiction. J. Nurs. Manag. 2015, 23, 54–64. [Google Scholar] [CrossRef]
- Melnyk, B.M.; Orsolini, L.; Tan, A.; Arslanian-Engoren, C.; Melkus, G.D.E.; Dunbar-Jacob, J.; Lewis, L.M. A National Study Links Nurses’ Physical and Mental Health to Medical Errors and Perceived Worksite Wellness. J. Occup. Environ. Med. 2018, 60, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Spinhoven, P.; Penninx, B.W.; Hemert, A.M.; Rooij, M.; Elzinga, B.M. Comorbidity of PTSD in Anxiety and Depressive Disorders: Prevalence and Shared Risk Factors. Child Abus. Negl. 2014, 38, 1320–1330. [Google Scholar] [CrossRef]
- American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders; DSM-5-TR; American Psychiatric Association Publishing: Washington, DC, USA, 2022; ISBN 978-0-89042-575-6.
- Beck, C.T. Secondary Traumatic Stress in Nurses: A Systematic Review. Arch. Psychiatr. Nurs. 2011, 25, 1–10. [Google Scholar] [CrossRef]
- Morrison, L.E.; Joy, J.P. Secondary Traumatic Stress in the Emergency Department. J. Adv. Nurs. 2016, 72, 2894–2906. [Google Scholar] [CrossRef] [Green Version]
- Daugherty, A.M.; Arble, E.P. Prevalence of Mental Health Symptoms in Residential Healthcare Workers in Michigan during the COVID-19 Pandemic. Psychiatry Res. 2020, 291, 113266. [Google Scholar] [CrossRef] [PubMed]
- Jarrad, R.; Hammad, S.; Shawashi, T.; Mahmoud, N. Compassion Fatigue and Substance Use among Nurses. Ann. Gen. Psychiatry 2018, 17, 1–8. [Google Scholar] [CrossRef]
- De Oliveira, S.M.; de Alcantara Sousa, L.V.; Vieira Gadelha, M.d.S.; do Nascimento, V.B. Prevention Actions of Burnout Syndrome in Nurses: An Integrating Literature Review. Clin. Pract. Epidemiol. Ment. Health 2019, 15, 64–73. [Google Scholar] [CrossRef] [PubMed]
- Arble, E.P.; Shankar, S.; Steinert, S.W.; Daugherty, A.M. Mental Health in Residential Healthcare Workers During the COVID-19 Pandemic: The Moderating Role of Selfobject Needs. Front. Psychiatry 2021, 12, 596618. [Google Scholar] [CrossRef] [PubMed]
| Variable | n | % |
|---|---|---|
| Self-identified female | 574 | 93.3 |
| Race/Ethnicity | ||
| Non-Hispanic White | 541 | 88 |
| Black and African American | 34 | 5.5 |
| Asian | 15 | 2.4 |
| Age | ||
| 18–34 years | 123 | 20 |
| 35–44 years | 151 | 24.6 |
| 45–54 years | 139 | 22.6 |
| 55–64 years | 157 | 25.5 |
| 65 years and older | 43 | 7 |
| Current Work Schedule | ||
| Less than 20 h | 38 | 6.2 |
| 20–40 h | 335 | 54.5 |
| 41–60 h | 181 | 29.4 |
| 61–80 h | 32 | 5.2 |
| More than 80 h | 1 | 0.2 |
| Substance Use | ||
| Drinking | 442 | 71.9 |
| Marijuana use | 29 | 4.7 |
| Other drug | 80 | 13 |
| Variable | Median (Q1, Q3) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Age † | |||||||||
| 2 | Stress | 6.00 (5.00, 7.50) | −0.16 | |||||||
| 3 | Sleep | 5.00 (4.00, 7.00) | 0.10 | −0.43 | ||||||
| 4 | Secondary Trauma | 2.00 (1.00, 3.00) | −0.15 | 0.28 | −0.23 | |||||
| 5 | Exhaustion | 11.00 (8.00, 13.00) | −0.15 | 0.51 | −0.39 | 0.36 | ||||
| 6 | Depression | 6.00 (2.00, 9.00) | −0.13 | 0.53 | −0.53 | 0.35 | 0.57 | |||
| 7 | PTSD | 10.00 (8.00, 14.00) | −0.14 | 0.42 | −0.36 | 0.42 | 0.51 | 0.71 | ||
| 8 | Anxiety | 5.00 (2.00, 9.00) | −0.21 | 0.61 | −0.42 | 0.39 | 0.56 | 0.75 | 0.73 | |
| 9 | Workplace | 28.00 (22.00, 34.00) | −0.07 (ns) | 0.30 | −0.25 | 0.36 | 0.37 | 0.49 | 0.54 | 0.51 |
| Cognitive Failure |
| Indirect Effect | ||||
|---|---|---|---|---|
| Mediator | Unstandardized Coeff. | Sobel z-Test (p-Value) | 95% CI (LL, UL) | % of Cumulative Effect |
| PTSD | 0.306 | 2.84 (0.005) | 0.095, 0.516 | 31.10 |
| Anxiety | 0.191 | 2.01 (0.045) | 0.004, 0.379 | 19.41 |
| Depression | 0.139 | 1.79 (0.073) | −0.013, 0.292 | 14.13 |
| Secondary Trauma | 0.123 | 2.28 (0.023) | 0.017, 0.229 | 12.50 |
| Exhaustion | 0.053 | 0.98 (0.327) | −0.053, 0.159 | 5.39 |
| Sleep | −0.022 | −0.56 (0.574) | −0.100, 0.056 | 2.24 |
| Stress | 0.017 | 0.56 (0.574) | −0.043, 0.078 | 1.73 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arble, E.; Manning, D.; Arnetz, B.B.; Arnetz, J.E. Increased Substance Use among Nurses during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 2674. https://doi.org/10.3390/ijerph20032674
Arble E, Manning D, Arnetz BB, Arnetz JE. Increased Substance Use among Nurses during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2023; 20(3):2674. https://doi.org/10.3390/ijerph20032674
Chicago/Turabian StyleArble, Eamonn, Dana Manning, Bengt B. Arnetz, and Judith E. Arnetz. 2023. "Increased Substance Use among Nurses during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 20, no. 3: 2674. https://doi.org/10.3390/ijerph20032674







