Implementing a Community-Led Arsenic Mitigation Intervention for Private Well Users in American Indian Communities: A Qualitative Evaluation of the Strong Heart Water Study Program
Abstract
:1. Introduction
2. Materials and Methods
2.1. Conceptual Frameworks
| Construct | Definition | Examples | |
|---|---|---|---|
| Implementer Level | |||
| Intervention characteristics | Attributes of the program itself, either as a whole or individual components | Complexity of the program; Relative advantage over comparable interventions | |
| Implementing individuals | Attributes of the personnel implementing the program | Knowledge or beliefs about the POU arsenic filters; Personal commitment to the organization or program | |
| Inner setting | Attributes of the organization implementing the program | Organizational communication systems and norms; Available resources for implementation | |
| Outer setting | Attributes of organizations, policies, and other factors outside the implementing organization | External policy and regulatory environment; Needs and resources of the recipient population | |
| Process | Actions or activities taken to facilitate implementation | Monitoring and learning processes; Engaging local champions to promote the program | |
| Recipient level | |||
| Risks | Understanding and awareness of health risks (both perceived and factual knowledge) | Perceived health risks of arsenic; Knowledge and beliefs about arsenic prevalence in groundwater | |
| Attitudes | Beliefs about the costs and benefits of a behavior, feelings towards a particular behavior, health risk, or program | Beliefs about the extent to which the POU arsenic filter can reduce arsenic exposure and mitigate health impacts | |
| Norms | Personal approval/disapproval of a particular behavior, health risk, or program component; perceptions of societal approval/disapproval; and perceptions of to what extent others perform a given behavior | Perceptions of whether others also use the POU arsenic filter; Endorsements from community leaders | |
| Abilities | Capacity, both actual and perceived, to perform the behavior | Perceived and actual ability to use the POU arsenic filter for drinking and cooking, and to perform maintenance on the filter | |
| Self-regulation | Ability to develop plans and routines to facilitate the behavior; cues and feedback to support the behavior | Visual cues to use the POU arsenic filter device; Burden of other household duties that interfere with filter use | |
2.2. Intervention Design and Study Setting
2.3. Sampling and Recruitment
2.4. Data Collection
2.5. Data Analysis
3. Results
3.1. Study Sample
3.2. Perceptions of Success
“We wanted to be safe and trusted the study—that it was going to help, not only us, but our people. So we’re grateful for you guys being here.”(Recipient, mHealth/filter arm).
“Some things [are] just out of our control. We can’t persuade them but at least give thanks for giving it a try.”(Implementer, health promoter).
3.3. Barriers and Facilitators among Implementers
3.3.1. Intervention Characteristics
3.3.2. Implementing Individuals
“I know where they come from, and we all grew up the same. And so once you go in there and you’re comfortable with your surroundings, and they’re comfortable with you, I think things are a lot easier…. And there’s a certain amount of respect or standards that we have too, so it’s not like somebody… younger going in there.”(Implementer, health promoter).
3.3.3. Inner Setting
“Away from the reservation you have to have that open communication. And some of the guys, a couple of guys, they don’t have that. They never left the reservation. So the communication was a little bit low.”(Implementer, plumber).
3.3.4. Outer Setting
3.3.5. Process
3.4. Barriers and Facilitators among Recipients
3.4.1. Risks
“It was kind of a lot to try reading. I’m just overwhelmed with Google searches... There’s a lot of stuff to scroll through and try to find what would be more informative.”(Recipient, mHealth/filter arm).
I wasn’t very concerned because like I said, we’ve lived here all this time, and no one’s died of arsenic poisoning that I know of yet.”(Recipient, intensive arm).
3.4.2. Attitudes
“I guess I learned a long time ago, you kind of have to pay attention to what’s in black and white, because not always is the word truthful. So we did see the results in black and white, and that gave us some assurance.”(Recipient, mHealth/filter arm).
“I’m getting old and am going to die soon anyway… I try not to think about it. When I die, I die.”(Recipient, intensive arm).
3.4.3. Norms
“Some people, if they don’t want to use it, they won’t, no matter how much you convince them. You can suggest it… But if they’re not going to use it, that’s not my problem.”(Recipient, intensive arm).
3.4.4. Ability
3.4.5. Self-Regulation
“The kids, I think they got used to it right away because the little ones, they just jump up there, and just turn it on and get their water.”(Recipient, mHealth/filter arm).
“Well, I’ve never had a problem with the unit. Well, I guess I did have a, you know, just minor things. A lot of times the batteries come loose or just pop out [from water meter]... The filter itself never had any flow problems that was fine. Still has the same flow that it did when we first installed it. So I had never had any problem with it giving me problems of not delivering water or anything like that.”(Recipient, intensive arm).
4. Discussion
4.1. Implementation Successes and Associated Barriers and Facilitators
4.2. Implementation Challenges and Associated Barriers and Facilitators
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Carlin, D.J.; Naujokas, M.F.; Bradham, K.D.; Cowden, J.; Heacock, M.; Henry, H.F.; Lee, J.S.; Thomas, D.J.; Thompson, C.; Tokar, E.J.; et al. Arsenic and Environmental Health: State of the Science and Future Research Opportunities. Environ. Health Perspect. 2015, 124, 890–899. [Google Scholar] [CrossRef] [PubMed]
- Ratnaike, R.N. Acute and Chronic Arsenic Toxicity. Postgrad. Med. J. 2003, 79, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Naujokas, M.F.; Anderson, B.; Ahsan, H.; Vasken Aposhian, H.; Graziano, J.H.; Thompson, C.; Suk, W.A. The Broad Scope of Health Effects from Chronic Arsenic Exposure: Update on a Worldwide Public Health Problem. Environ. Health Perspect. 2013, 121, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Mohammed Abdul, K.S.; Jayasinghe, S.S.; Chandana, E.P.S.; Jayasumana, C.; de Silva, P.M.C.S. Arsenic and Human Health Effects: A Review. Environ. Toxicol. Pharmacol. 2015, 40, 828–846. [Google Scholar] [CrossRef]
- United States Environmental Protection Agency. Drinking Water Requirements for States and Public Water Systems—Arsenic Rule; EPA: Washington, DC, USA, 2001.
- Nigra, A.E.; Sanchez, T.R.; Nachman, K.E.; Harvey, D.E.; Chillrud, S.N.; Graziano, J.H.; Navas-Acien, A. The Effect of the Environmental Protection Agency Maximum Contaminant Level on Arsenic Exposure in the USA from 2003 to 2014: An Analysis of the National Health and Nutrition Examination Survey (NHANES). Lancet Public Health 2017, 2, e513–e521. [Google Scholar] [CrossRef]
- Gribble, M.O.; Howard, B.V.; Umans, J.G.; Shara, N.M.; Francesconi, K.A.; Goessler, W.; Crainiceanu, C.M.; Silbergeld, E.K.; Guallar, E.; Navas-Acien, A. Arsenic Exposure, Diabetes Prevalence, and Diabetes Control in the Strong Heart Study. Am. J. Epidemiol. 2012, 176, 865–874. [Google Scholar] [CrossRef]
- Carroll, C.R.; Noonan, C.; Garroutte, E.M.; Navas-Acien, A.; Verney, S.P.; Buchwald, D. Low-Level Inorganic Arsenic Exposure and Neuropsychological Functioning in American Indian Elders. Environ. Res. 2017, 156, 74–79. [Google Scholar] [CrossRef]
- Navas-Acien, A.; Umans, J.G.; Howard, B.V.; Goessler, W.; Francesconi, K.A.; Crainiceanu, C.M.; Silbergeld, E.K.; Guallar, E. Urine Arsenic Concentrations and Species Excretion Patterns in American Indian Communities Over a 10-Year Period: The Strong Heart Study. Environ. Health Perspect. 2009, 117, 1428–1433. [Google Scholar] [CrossRef]
- Nigra, A.E.; Olmedo, P.; Grau-Perez, M.; O’Leary, R.; O’Leary, M.; Fretts, A.M.; Umans, J.G.; Best, L.G.; Francesconi, K.A.; Goessler, W.; et al. Dietary Determinants of Inorganic Arsenic Exposure in the Strong Heart Family Study. Environ. Res. 2019, 177, 108616. [Google Scholar] [CrossRef]
- Powers, M.; Yracheta, J.; Harvey, D.; O’Leary, M.; Best, L.G.; Black Bear, A.; MacDonald, L.; Susan, J.; Hasan, K.; Thomas, E.; et al. Arsenic in Groundwater in Private Wells in Rural North Dakota and South Dakota: Water Quality Assessment for an Intervention Trial. Environ. Res. 2019, 168, 41–47. [Google Scholar] [CrossRef]
- Sobel, M.; Sanchez, T.R.; Zacher, T.; Mailloux, B.; Powers, M.; Yracheta, J.; Harvey, D.; Best, L.G.; Bear, A.B.; Hasan, K.; et al. Spatial Relationship between Well Water Arsenic and Uranium in Northern Plains Native Lands. Environ. Pollut. 2021, 287, 117655. [Google Scholar] [CrossRef] [PubMed]
- May, T.W.; Wiedmeyer, R.H.; Gober, J.; Larson, S. Influence of Mining-Related Activities on Concentrations of Metals in Water and Sediment from Streams of the Black Hills, South Dakota. Arch. Environ. Contam. Toxicol. 2001, 40, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Spaur, M.; Lombard, M.A.; Ayotte, J.D.; Harvey, D.E.; Bostick, B.C.; Chillrud, S.N.; Navas-Acien, A.; Nigra, A.E. Associations between Private Well Water and Community Water Supply Arsenic Concentrations in the Conterminous United States. Sci. Total Environ. 2021, 787, 147555. [Google Scholar] [CrossRef] [PubMed]
- Thomas, E.D.; Gittelsohn, J.; Yracheta, J.; Powers, M.; O’Leary, M.; Harvey, D.E.; Red Cloud, R.; Best, L.G.; Black Bear, A.; Navas-Acien, A.; et al. The Strong Heart Water Study: Informing and Designing a Multi-Level Intervention to Reduce Arsenic Exposure among Private Well Users in Great Plains Indian Nations. Sci. Total Environ. 2019, 650, 3120–3133. [Google Scholar] [CrossRef] [PubMed]
- George, C.M.; Zacher, T.; Endres, K.; Richards, F.; Bear Robe, L.; Harvey, D.; Best, L.G.; Red Cloud, R.; Black Bear, A.; Skinner, L.; et al. Evaluation of a Multi-Level, Participatory Intervention to Reduce Arsenic Exposure in American Indian Communities: A Cluster Randomized Controlled Trial of the Strong Heart Water Study Program. Environ. Health Perspect. under review.
- Haque, S.S.; Freeman, M.C. The Applications of Implementation Science in Water, Sanitation, and Hygiene (WASH) Research and Practice. Environ. Health Perspect. 2021, 129, 65002. [Google Scholar] [CrossRef]
- Saunders, R.P.; Evans, M.H.; Joshi, P. Developing a Process-Evaluation Plan for Assessing Health Promotion Program Implementation: A How-To Guide. Health Promot. Pract. 2016, 6, 134–147. [Google Scholar] [CrossRef]
- Setty, K.; Cronk, R.; George, S.; Anderson, D.; O’Flaherty, G.; Bartram, J. Adapting Translational Research Methods to Water, Sanitation, and Hygiene. Int. J. Environ. Res. Public Health 2019, 16, 4049. [Google Scholar] [CrossRef]
- Brown, C.H.; Curran, G.; Palinkas, L.A.; Aarons, G.A.; Wells, K.B.; Jones, L.; Collins, L.M.; Duan, N.; Mittman, B.S.; Wallace, A.; et al. An Overview of Research and Evaluation Designs for Dissemination and Implementation. Annu. Rev. Public Health 2017, 38, 1–22. [Google Scholar] [CrossRef]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering Implementation of Health Services Research Findings into Practice: A Consolidated Framework for Advancing Implementation Science. Implement. Sci. 2009, 4, 50. [Google Scholar] [CrossRef]
- Mosler, H.J. A Systematic Approach to Behavior Change Interventions for the Water and Sanitation Sector in Developing Countries: A Conceptual Model, a Review, and a Guideline. Int. J. Environ. Health Res. 2012, 22, 431–449. [Google Scholar] [CrossRef]
- Proctor, E.; Silmere, H.; Raghavan, R.; Hovmand, P.; Aarons, G.; Bunger, A.; Griffey, R.; Hensley, M. Outcomes for Implementation Research: Conceptual Distinctions, Measurement Challenges, and Research Agenda. Adm. Policy Ment. Health Ment. Health Serv. Res. 2011, 38, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.M.; Gupta, A.K.; Birken, S.; Sakas, Z.; Freeman, M.C. Successes, Challenges, and Support for Men versus Women Implementers in Water, Sanitation, and Hygiene Programs: A Qualitative Study in Rural Nepal. Int. J. Hyg. Environ. Health 2021, 236, 113792. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.M.; Gupta, A.K.; Birken, S.A.; Sakas, Z.; Freeman, M.C. Adaptation in Rural Water, Sanitation, and Hygiene Programs: A Qualitative Study in Nepal. Int. J. Hyg. Environ. Health 2022, 240, 113919. [Google Scholar] [CrossRef] [PubMed]
- Kirk, M.A.; Kelley, C.; Yankey, N.; Birken, S.A.; Abadie, B.; Damschroder, L. A Systematic Review of the Use of the Consolidated Framework for Implementation Research. Implement. Sci. 2015, 11, 72. [Google Scholar] [CrossRef]
- George, C.M.; Inauen, J.; Perin, J.; Tighe, J.; Hasan, K.; Zheng, Y. Behavioral Determinants of Switching to Arsenic-Safe Water Wells: An Analysis of a Randomized Controlled Trial of Health Education Interventions Coupled with Water Arsenic Testing. Health Educ. Behav. 2017, 44, 92–102. [Google Scholar] [CrossRef]
- Inauen, J.; Tobias, R.; Mosler, H.-J. The Role of Commitment Strength in Enhancing Safe Water Consumption: Mediation Analysis of a Cluster-Randomized Trial. Br. J. Health Psychol. 2014, 19, 701–719. [Google Scholar] [CrossRef]
- Mosler, H.J.; Blochliger, O.R.; Inauen, J. Personal, Social, and Situational Factors Influencing the Consumption of Drinking Water from Arsenic-Safe Deep Tubewells in Bangladesh. J. Environ. Manag. 2010, 91, 1316–1323. [Google Scholar] [CrossRef]
- Sclar, G.D.; Bauza, V.; Mosler, H.J.; Bisoyi, A.; Chang, H.H.; Clasen, T.F. Study Design and Rationale for a Cluster Randomized Trial of a Safe Child Feces Management Intervention in Rural Odisha, India. BMC Public Health 2022, 22, 106. [Google Scholar] [CrossRef]
- Sclar, G.D.; Mosler, H.-J. Caregiver Social Support and Child Toilet Training in Rural Odisha, India: What Types of Support Facilitate Training and How? Appl. Psychol. Health Well Being 2022, 14, 413–433. [Google Scholar] [CrossRef]
- Sclar, G.D.; Bauza, V.; Bisoyi, A.; Clasen, T.F.; Mosler, H.J. Contextual and Psychosocial Factors Influencing Caregiver Safe Disposal of Child Feces and Child Latrine Training in Rural Odisha, India. PLoS ONE 2022, 17, e0274069. [Google Scholar] [CrossRef] [PubMed]
- Bauer, M.S.; Kirchner, J. Implementation Science: What Is It and Why Should I Care? Psychiatry Res. 2020, 283, 112376. [Google Scholar] [CrossRef] [PubMed]
- Nilsen, P. Making Sense of Implementation Theories, Models and Frameworks. Implement. Sci. 2015, 10, 53. [Google Scholar] [CrossRef] [PubMed]
- Zacher, T.; Endres, K.; Richards, F.; Robe, L.B.; Powers, M.; Yracheta, J.; Harvey, D.; Best, L.G.; Cloud, R.R.; Bear, A.B.; et al. Evaluation of Water Arsenic Filter Treatment in a Participatory Intervention to Reduce Arsenic Exposure in American Indian Communities: The Strong Heart Water Study. Sci. Total Environ. 2022, 862, 160217. [Google Scholar] [CrossRef]
- Devore, C.L.; Rodriguez-Freire, L.; Mehdi-Ali, A.; Ducheneaux, C.; Artyushkova, K.; Zhou, Z.; Latta, D.E.; Lueth, V.W.; Gonzales, M.; Lewis, J.; et al. Effect of Bicarbonate and Phosphate on Arsenic Release from Mining-Impacted Sediments in the Cheyenne River Watershed, South Dakota, USA. Environ. Sci. Process. Impacts 2019, 21, 456–468. [Google Scholar] [CrossRef]
- Swift Bird, K.; Navarre-Sitchler, A.; Singha, K. Hydrogeological Controls of Arsenic and Uranium Dissolution into Groundwater of the Pine Ridge Reservation, South Dakota. Appl. Geochem. 2020, 114, 104522. [Google Scholar] [CrossRef]
- Malolo, R.; Kumwenda, S.; Chidziwisano, K.; Kambala, C.; Morse, T. Social Outcomes of a Community-Based Water, Sanitation and Hygiene Intervention. J. Water Sanit. Hyg. Dev. 2021, 11, 483–493. [Google Scholar] [CrossRef]
- Farrell, J.; Burow, P.B.; McConnell, K.; Bayham, J.; Whyte, K.; Koss, G. Effects of Land Dispossession and Forced Migration on Indigenous Peoples in North America. Science 2021, 374, eabe4943. [Google Scholar] [CrossRef]
- Anderson, R.T. Water Rights, Water Quality, and Regulatory Jurisdiction in Indian Country. Stanf. Environ. Law J. 2015, 34, 195. [Google Scholar]
- Mitchell, F.M. Water (in) Security and American Indian Health: Social and Environmental Justice Implications for Policy, Practice, and Research. Public Health 2019, 176, 98–105. [Google Scholar] [CrossRef]
- Yablon, M. Property Rights and Sacred Sites: Federal Regulatory Responses to American Indian Religious Claims on Public Land. Yale Law J. 2003, 113, 1623–1662. [Google Scholar] [CrossRef]
- Breathett, K.; Sims, M.; Gross, M.; Jackson, E.A.; Jones, E.J.; Navas-Acien, A.; Taylor, H.; Thomas, K.L.; Howard, B.V. Cardiovascular Health in American Indians and Alaska Natives: A Scientific Statement From the American Heart Association. Circulation 2020, 141, E948–E959. [Google Scholar] [CrossRef] [PubMed]
- Leonard, B.; Parker, D.P.; Anderson, T.L. Land Quality, Land Rights, and Indigenous Poverty. J. Dev. Econ. 2020, 143, 102435. [Google Scholar] [CrossRef]
- Poudel, A.; Zhou, J.Y.; Story, D.; Li, L. Diabetes and Associated Cardiovascular Complications in American Indians/Alaskan Natives: A Review of Risks and Prevention Strategies. J. Diabetes Res. 2018, 2018, 2742565. [Google Scholar] [CrossRef] [PubMed]
- Deitz, S.; Meehan, K. Plumbing Poverty: Mapping Hot Spots of Racial and Geographic Inequality in U.S. Household Water Insecurity. Ann. Am. Assoc. Geogr. 2019, 109, 1092–1109. [Google Scholar] [CrossRef]
- Mathers, R.L. The Failure of State-Led Economic Development on American Indian Reservations. Indep. Rev. 2012, 17, 65–80. [Google Scholar]
- Belcourt-Dittloff, A.; Stewart, J. Historical Racism: Implications for Native Americans. Am. Psychol. 2000, 55, 1166–1167. [Google Scholar] [CrossRef]
- Koch, J.W. Racial Minorities’ Trust in Government and Government Decisionmakers. Soc. Sci. Q. 2019, 100, 19–37. [Google Scholar] [CrossRef]
- Endres, K.; Zacher, T.; Richards, F.; Bear Robe, L.; Powers, M.; Yratcheta, J.; Harvey, D.; Best, L.G.; Red Cloud, R.; Black Bear, A.; et al. Behavioral Determinants of Arsenic-Safe Water Use among Great Plains Indian Nation Private Well Users: Results from the Strong Heart Water Study. Environ. Health, 2022; in press. [Google Scholar]
- 100th United States Congress. Mni Wiconi Project Act of 1988; H.R. 2772; United States Congress: Washington, DC, USA, 1988.
- 113th United States Congress. Mni Wiconi Project Act Amendments; United States Senate: Washington, DC, USA, 2013; pp. 113–174.
- Flanagan, S.V.; Marvinney, R.G.; Zheng, Y. Influences on Domestic Well Water Testing Behavior in a Central Maine Area with Frequent Groundwater Arsenic Occurrence. Sci. Total Environ. 2015, 505, 1274–1281. [Google Scholar] [CrossRef]
- Flanagan, S.V.; Spayd, S.E.; Procopio, N.A.; Chillrud, S.N.; Braman, S.; Zheng, Y. Arsenic in Private Well Water Part 1 of 3: Impact of the New Jersey Private Well Testing Act on Household Testing and Mitigation Behavior. Sci. Total Environ. 2016, 562, 999–1009. [Google Scholar] [CrossRef]
- George, C.M.; Smith, A.H.; Kalman, D.A.; Steinmaus, C.M. Reverse Osmosis Filter Use and High Arsenic Levels in Private Well Water. Arch. Environ. Occup. Health 2006, 61, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Severtson, D.J.; Baumann, L.C.; Brown, R.L. Applying a Health Behavior Theory to Explore the Influence of Information and Experience on Arsenic Risk Representations, Policy Beliefs, and Protective Behavior. Risk Anal. 2006, 26, 353–368. [Google Scholar] [CrossRef] [PubMed]
- Shaw, W.D.; Walker, M.; Benson, M. Treating and Drinking Well Water in the Presence of Health Risks from Arsenic Contamination: Results from a U.S. Hot Spot. Risk Anal. 2005, 25, 1531–1543. [Google Scholar] [CrossRef] [PubMed]
- Slotnick, M.J.; Meliker, J.R.; Nriagu, J.O. Effects of Time and Point-of-Use Devices on Arsenic Levels in Southeastern Michigan Drinking Water, USA. Sci. Total Environ. 2006, 369, 42–50. [Google Scholar] [CrossRef]
- Spayd, S.E.; Robson, M.G.; Buckley, B.T. Whole-House Arsenic Water Treatment Provided More Effective Arsenic Exposure Reduction than Point-of-Use Water Treatment at New Jersey Homes with Arsenic in Well Water. Sci. Total Environ. 2015, 505, 1361–1369. [Google Scholar] [CrossRef]
- Yang, Q.; Flanagan, S.V.; Chillrud, S.; Ross, J.; Zeng, W.; Culbertson, C.; Spayd, S.; Backer, L.; Smith, A.E.; Zheng, Y. Reduction in Drinking Water Arsenic Exposure and Health Risk through Arsenic Treatment among Private Well Households in Maine and New Jersey, USA. Sci. Total Environ. 2020, 738, 139683. [Google Scholar] [CrossRef] [PubMed]
- Walker, M.; Seiler, R.L.; Meinert, M. Effectiveness of Household Reverse-Osmosis Systems in a Western U.S. Region with High Arsenic in Groundwater. Sci. Total Environ. 2008, 389, 245–252. [Google Scholar] [CrossRef] [PubMed]

| Outcome | Definition |
|---|---|
| Acceptability | Perception that the program, or its component parts, is agreeable and satisfactory |
| Adoption | Intention, decision, or action to uptake key behaviors for the program (e.g., obtaining an arsenic test, using arsenic-safe water) |
| Appropriateness | Perceived fit, relevance, or compatibility of the program with the context, or perceived fit of the intervention to address locally relevant issues or problems |
| Cost | Cost of the program and implementation efforts |
| Feasibility | The extent to which the program can be successfully delivered and/or used within with local context |
| Fidelity | The extent to which the program is delivered as originally developed and specified in program plans and protocols |
| Penetration | Coverage area and intensity of exposure to the program among the target population |
| Sustainability | The extent to which the POU arsenic filters and associated key behaviors are maintained within the target population |
| Demographic Trait | Number of Participants |
|---|---|
| Recipients (n = 35) | |
| Age | |
| 18–35 | 3 |
| 36–50 | 7 |
| 51–65 | 7 |
| 66+ | 18 |
| Gender | |
| Male | 17 |
| Female | 18 |
| Intervention arm | |
| mHealth/filter | 23 |
| Intensive | 12 |
| Self-reported filter use † | |
| Exclusive user | 8 |
| Partial user | 26 |
| Non-user | 1 |
| Implementers (n = 13) | |
| Behavior change implementers | |
| Health promoters | 6 |
| Study and intervention supervisors | 2 |
| Role of partner organizations | |
| Water quality testing | 3 |
| Filter installation | 1 |
| Intervention design and funding | 1 |
| Outcome | Implementer Perceptions | Recipient Perceptions | |
|---|---|---|---|
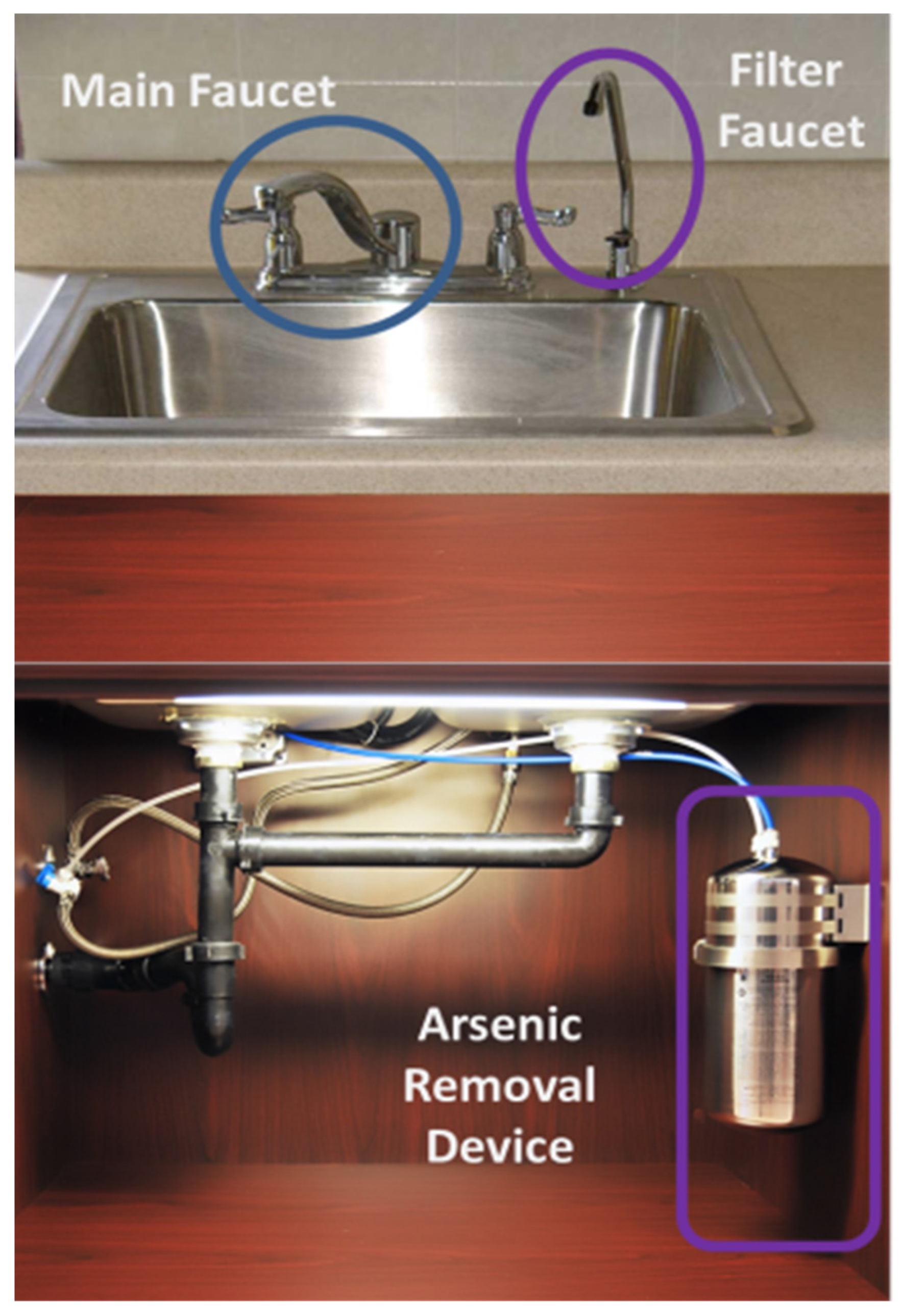
| Acceptability | Assessed at recipient level only. | Most recipients liked the POU arsenic filter. They described the installation as “professional” and “respectful”. Recipients reported that the filter gave them “peace of mind” for arsenic-safe water. Some recipients reported low acceptability associated with installation problems (e.g., filter faucet improperly secured on the kitchen sink leading to wobbling). | |
| Adoption | Implementers perceived that increased arsenic awareness and opportunities to access arsenic-safe water were successes. Some implementers reported that they had achieved success just by installing the filter, and whether recipients decided to use it was outside of their control. Others perceived that use of the filter device by even some recipients was a success, believing that some recipients would never change their behavior. | POU arsenic filters provided recipients that wanted to use arsenic-safe water with an opportunity to do so. Some recipients were concerned about arsenic in their well water but did not believe the filter device would effectively remove it. These individuals typically used bottled water. For recipients that were unconcerned about arsenic and did not intend to switch to arsenic-safe water, health communication did little to change their attitudes or practices. | |
| Appropriateness | Implementers believed that arsenic exposure was a locally relevant problem. Implementing organizations and agencies had missions and mandates to provide safe water and/or protect health, and the program was perceived to align well with those needs. Implementers perceived the program to be culturally competent because it was designed with input from community and tribal members, and many implementers were tribal members who were aware of community needs. | Many recipients were concerned about water contamination and associated health impacts from arsenic and other toxicants (e.g., solid waste dumping, farming and mining chemicals). Recipients believed that the filter addressed a relevant community need and that water quality testing and raising awareness about arsenic in the community was important. | |
| Cost | Some implementers were concerned about the affordability of replacement filter cartridges for low-income households, but otherwise cost was not a major concern mentioned by implementers. | Recipients appreciated that the filter was installed at no cost. Many expressed concerned over the high cost of replacement cartridges. Some reported that they may need to make cuts in other areas of the household budget to afford one, or that they would delay replacing an expired cartridge to save money. | |
| Fidelity | The short life of batteries in the water meter necessitated adaptation to communication regarding using the indicator light to signal filter cartridge changes. The COVID-19 pandemic also disrupted implementation and necessitated adaptation of in-person components to remote delivery. | Recipient reports confirmed implementer descriptions of some variation within study arms about the content and format of behavior change communication. | |
| Feasibility | Feasibility challenges centered around travel to remote households over poor quality roads for the installation of POU arsenic filters and in-person visits. Once at the household, implementers described the filter device cannister as well-designed and easy to install. | Some households reported initial difficulty changing habits to routinely use the filter faucet for drinking and cooking, but in the long-term reported few difficulties. Feasibility of maintenance was more challenging, with many households reporting trouble due to either lack of physical ability or sufficient information to change the filter cartridge. | |
| Penetration | Implementers perceived penetration to be good in terms of conducting water testing for a very high proportion of private well users in the target area, even those in remote or difficult to access areas due to poor road quality. Implementers reported challenges in penetration of behavior change communication with enrolled households (e.g., households not answering the phone). | Recipients corroborated difficulties receiving behavior change communication by phone. Many reported that they did not recognize phone numbers of the study team and believed they were spam calls. Study protocols dictated that health promoters should leave a voicemail message, but many recipients, particularly the elderly, did not have a voicemail setup. | |
| Sustainability | Mixed views on sustainability. Some implementers perceived that since the filter devices had been installed by the program, households could and should be responsible for maintaining them. Others believed that, since an affordable option for replacement cartridges was not readily available locally, the intervention would not be sustained. | Recipients expressed concerns over their ability to locally source and afford filter cartridges in the long-term. Many expected that the study would continue to provide them, and had no alternative plan to source filters when they were no longer available for free through the study. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anderson, D.M.; Bear, A.B.; Zacher, T.; Endres, K.; Saxton, R.; Richards, F.; Robe, L.B.; Harvey, D.; Best, L.G.; Cloud, R.R.; et al. Implementing a Community-Led Arsenic Mitigation Intervention for Private Well Users in American Indian Communities: A Qualitative Evaluation of the Strong Heart Water Study Program. Int. J. Environ. Res. Public Health 2023, 20, 2681. https://doi.org/10.3390/ijerph20032681
Anderson DM, Bear AB, Zacher T, Endres K, Saxton R, Richards F, Robe LB, Harvey D, Best LG, Cloud RR, et al. Implementing a Community-Led Arsenic Mitigation Intervention for Private Well Users in American Indian Communities: A Qualitative Evaluation of the Strong Heart Water Study Program. International Journal of Environmental Research and Public Health. 2023; 20(3):2681. https://doi.org/10.3390/ijerph20032681
Chicago/Turabian StyleAnderson, Darcy M., Annabelle Black Bear, Tracy Zacher, Kelly Endres, Ronald Saxton, Francine Richards, Lisa Bear Robe, David Harvey, Lyle G. Best, Reno Red Cloud, and et al. 2023. "Implementing a Community-Led Arsenic Mitigation Intervention for Private Well Users in American Indian Communities: A Qualitative Evaluation of the Strong Heart Water Study Program" International Journal of Environmental Research and Public Health 20, no. 3: 2681. https://doi.org/10.3390/ijerph20032681






