Factors Associated with Aging in Place among Community-Dwelling Older Adults in Korea: Findings from a National Survey
Abstract
1. Introduction
2. Materials and Methods
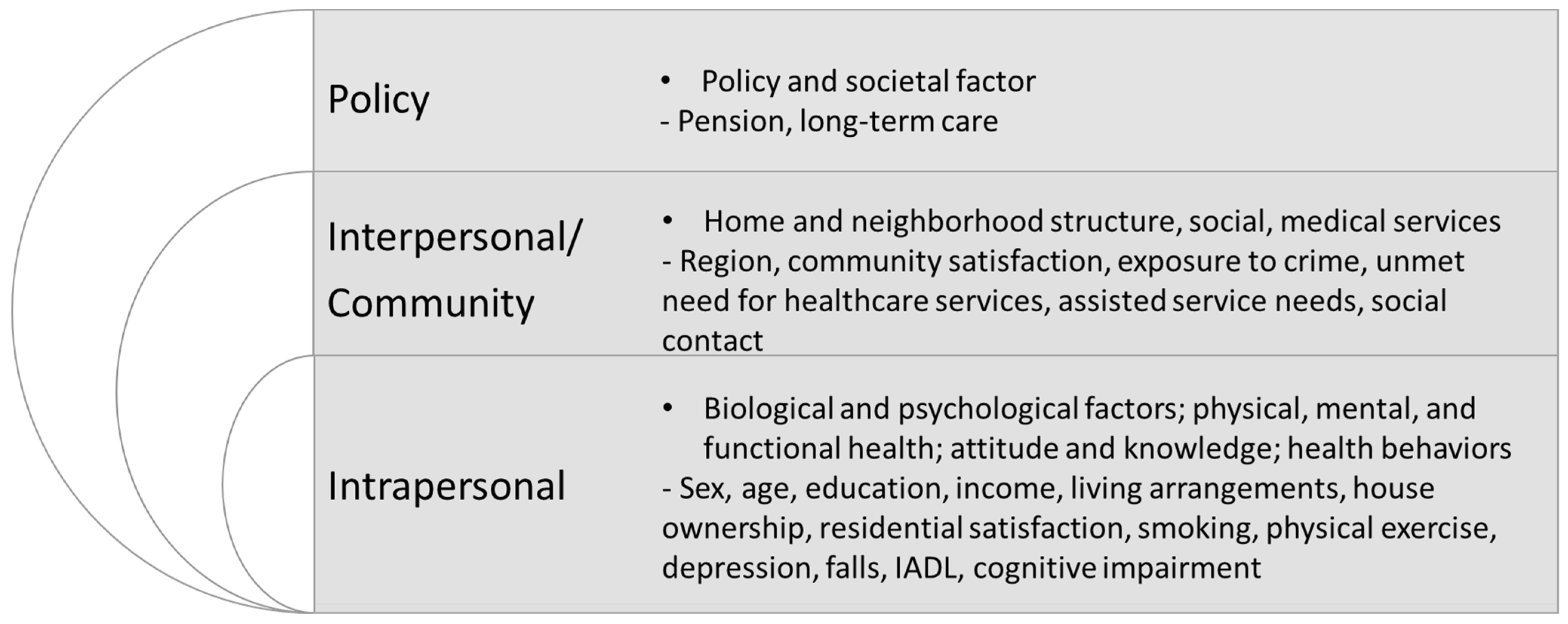
- The intrapersonal level refers to biological and sociodemographic characteristics.They include sex; age; education; income; health-risk behaviors; and mental, physical, and functional health.
- The interpersonal and community level refers to an individual’s social network, consisting of interactions with family and medical and social service systems.They include region, community satisfaction, exposure to crime, unmet needs for healthcare services, community care service needs, and social contact.
- The policy level refers to economic, social, and political policies and regulations including pension and long-term care.
2.1. Measurements
2.1.1. Dependent Variable
2.1.2. Independent Variable
2.2. Statistical Analysis
3. Results
3.1. General Characteristics of the Study Population
3.2. Differences in the Level of Community Care Service Needs
3.3. Factors Affecting AIP
4. Discussion
4.1. Basic Pension and Long-Term Care Service
4.2. Age
4.3. Health-Related Factors
4.4. Unmet Healthcare Needs and Community Care Service Needs
4.5. House Ownership and Residential Satisfaction
4.6. Social Network
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Statistics Korea. Estimated Future Population in Korea in 2017–2067. Available online: https://www.kostat.go.kr/portal/korea/kor_nw/1/2/6/index.board?bmode=read&aSeq=373873 (accessed on 9 September 2022).
- Statistics Korea. 2022 Statistics on the Aged. Available online: https://kostat.go.kr/portal/korea/kor_nw/1/1/index.board?bmode=read&aSeq=420896 (accessed on 9 September 2022).
- World Health Organization. World Report on Ageing and Health. 2015. Available online: https://apps.who.int/iris/handle/10665/186463 (accessed on 11 September 2022).
- Korea Institute for Health and Social Affairs. 2020 Survey of Living Conditions and Welfare Needs of Korean Older Persons. Available online: https://data.kihasa.re.kr/kihasa/kor/databank/DatabankDetail.html (accessed on 11 September 2022).
- National Health Insurance Service. 2020 National Health Insurance Statistical Yearbook. Available online: https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020045020000&brdScnBltNo=4&brdBltNo=2313&pageIndex=1 (accessed on 20 September 2022).
- World Health Organization. Decade of Healthy Ageing: Baseline Report. 2020. Available online: https://www.who.int/publications/i/item/9789240017900 (accessed on 20 September 2022).
- World Health Organization. United Nation’s Decade of Healthy Ageing (2021–2030). 2020. Available online: https://www.who.int/initiatives/decade-of-healthy-ageing (accessed on 20 September 2022).
- Means, R. Safe as houses? Ageing in place and vulnerable older people in the UK. Soc. Pol. Admin. 2007, 41, 65–85. [Google Scholar] [CrossRef]
- Kaye, H.S.; LaPlante, M.P.; Harrington, C. Do noninstitutional long-term care services reduce medicaid spending? Health Aff. 2009, 28, 262–272. [Google Scholar] [CrossRef] [PubMed]
- Wiles, J.L.; Leibing, A.; Guberman, N.; Reeve, J.; Allen, R.E. The meaning of “aging in place” to older people. Gerontologist 2012, 52, 357–366. [Google Scholar] [CrossRef] [PubMed]
- Chon, Y. The use and coordination of the medical, public health and social care services for the elderly in terms of continuum of care. Health Soc. Welf. Rev. 2018, 38, 10–39. [Google Scholar]
- Ministry of Health and Welfare. Integrated Community Care Guidebook; Ministry of Health and Welfare: Sejong, Republic of Korea, 2020.
- Hong, S. Housing management behavior of the elderly: Focus on the causal effects of housing satisfaction and housing selections. Korean Fam. Resour. Manag. Assoc. 2011, 15, 1–21. [Google Scholar]
- Kwon, O.; Kim, J.K. Intention in aging in place of middle aged and elderly and differences in characteristics of related variables. J. Korean Hous. Assoc. 2019, 30, 77–85. [Google Scholar] [CrossRef]
- Lee, M.; Lee, S. An analysis of the relationship between the settlement consciousness of local residents and community wellbeing: Applying Kee’s 6 capital model of community wellbeing. Korea Assoc. Policy Stud. 2016, 25, 1–28. [Google Scholar]
- Moon, K. The mediating effect of the satisfaction with life and local identity in the influence of the physical environmental conditions and local social capital on the settlement consciousness of the middle aged and elderly. Public Pol. Res. 2019, 35, 201–233. [Google Scholar]
- Kim, S.; Moon, K.; Oh, C. Searching for policy orientation by the analysis of factors affecting aging in place in the aging community. J. Reg. Stud. 2015, 23, 137–164. [Google Scholar]
- Matsumoto, H.; Naruse, T.; Sakai, M.; Nagata, S. Who prefers to age in place?: Cross-sectional survey of middle-aged people in Japan. Geriatri. Gerontol. Inter. 2016, 16, 631–637. [Google Scholar] [CrossRef]
- Park, J. Factors influencing the unmet healthcare needs of elderly with chronic diseases: Focusing on the 2017 Korean National Survey on Elderly. J. Korea Acad. Ind. Coop. Soc. 2019, 20, 306–313. [Google Scholar]
- Edemekong, P.F.; Bomgaars, D.L.; Sukumaran, S.; Schoo, C. Activities of daily living. In StatPearls; Anonymous; StatPearls Publishing LLC: St. Petersburg, FL, USA, 2022. [Google Scholar]
- Lim, Y. Are there ways of constructing ‘aging in place’: Comparison of aging in place model and paths between rural and urban dwelling elderly. Korean J. Gerontol. Soc. Welf. 2016, 71, 411–436. [Google Scholar]
- Woo, J.; Chan, R.; Leung, J.; Wong, M. Relative contributions of geographic, socioeconomic, and lifestyle factors to quality of life, frailty, and mortality in elderly. PLoS ONE 2010, 5, e8775. [Google Scholar] [CrossRef] [PubMed]
- Cutchin, M.P. The process of mediated aging-in-place: A theoretically and empirically based model. Soc. Sci. Med. 2003, 57, 1077–1090. [Google Scholar] [CrossRef]
- Choi, B.; Lee, M. Individual-environmental suitability perceived by the elderly, residential satisfaction, structural relationships between the subjective euphoria-focusing on the mediating effects of residential satisfaction. J. Korea Contents Assoc. 2021, 21, 520–536. [Google Scholar]
- Kim, J.; Lee, T.; Kim, C. The association between the basic old-age pension and depression of the older adults in Korea. J. Prev. Med. Public. Health 2020, 53, 332–341. [Google Scholar] [CrossRef]
- Luciano, A.; Pascale, F.; Polverino, F.; Pooley, A. Measuring age-friendly housing: A framework. Sustainability 2020, 12, 848. [Google Scholar] [CrossRef]
- Steels, S. Key characteristics of age-friendly cities and communities: A review. Cities 2015, 47, 45–52. [Google Scholar] [CrossRef]
- Park, S. A fundamental study on housing for the elderly through an analysis of senior adults’ needs. J. Archit. Inst. Korea 2007, 23, 49–58. [Google Scholar]
- Kwak, I. A study on the factors affecting decisions by the super-aged on their preference of living with their children and continuously living in their current houses. J. Korean Hous. Assoc. 2011, 22, 83–95. [Google Scholar] [CrossRef]
- Lee, S.; Park, D. The study on the causality between the elderly’s residential environment and the aging in place. J. Korean Urb. Manag. Assoc. 2015, 28, 287–308. [Google Scholar]
- Bronfenbrenner, U. Ecological models of human development. In International Encyclopedia of Education, 2nd ed.; Anonymous; Elsevier: Oxford, UK, 1994; Volume 3. [Google Scholar]
- Lau, M.K.; Borrett, S.R.; Baiser, B.; Gotelli, N.J.; Ellison, A.M. Ecological network metrics: Opportunities for synthesis. Ecosphere 2017, 8, e01900. [Google Scholar] [CrossRef]
- Suanet, B.; Van Tilburg, T.G.; van Broese Groenou, M.I. Login in older adults’ personal networks: More important among later cohorts? J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2013, 68, 633–643. [Google Scholar]
- Bae, J.N.; Cho, M.J. Development of the Korean version of the Geriatric Depression Scale and its Short Form among elderly psychiatric patients. J. Psychosom. Res. 2004, 57, 297–305. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Han, Y.; Kim, B.; Dunkle, R.E. Aging in place of vulnerable older adults: Person–environment fit perspective. J. App. Gerontol. 2017, 36, 1327–1350. [Google Scholar] [CrossRef]
- Won, C.W.; Rho, Y.G.; SunWoo, D.; Lee, Y.S. The validity and reliability of Korean Instrumental Activities of Daily Living (K-IADL) Scale. J. Korean Geriatr. Soc. 2002, 6, 273–280. [Google Scholar]
- Park, J. Standardization of Korean version of the Mini-Mental State Examination (MMSE-K) for use in the elderly. Part II. Diagnostic validity. J. Korean Neuropsychiatr. Assoc. 1989, 28, 508–513. [Google Scholar]
- Choi, H.; Nam, B. Frequency and pattern of contact with multiple children and subjective well-being in middle and later life. J. Korean Home Manag. Assoc. 2019, 37, 27–39. [Google Scholar] [CrossRef]
- OECD Publishing. Pensions at a Glance 2019: OECD and G20 Indicators; Organisation for Economic Co-operation and Development OECD: Paris, France, 2020.
- Ha, J. Health care policy for older Koreans. In Ageing in Korea: Today and Tomorrow, 3rd ed.; Elderly Information Center: Seoul, Republic of Korea, 2013; pp. 130–139. [Google Scholar]
- Lim, M. A study on the perception of urban satisfaction and the consciousness of inhabitant in Seoul -Focusing on the satisfaction of living environment and urban risk. Korea Real Est. Rev. 2015, 62, 107–120. [Google Scholar]
- Choe, J.; Hong, E. The effect of life satisfaction and emotions about the city on the settlement consciousness of Suwon inhabitants. Korean Reg. Sociol. 2016, 17, 89–122. [Google Scholar]
- Jeong, E. A study on the life characteristics and the factors affecting community attachment of oldest olds for community care. J. Korean Long Term Care 2018, 6, 32–54. [Google Scholar] [CrossRef]
- Pak, T. What are the effects of expanding social pension on health? Evidence from the basic pension in South Korea. J. Econ. Ageing 2021, 18, 100287. [Google Scholar] [CrossRef]
- Hansen, E.B.; Gottschalk, G. What makes older people consider moving house and what makes them move? Hous. Theory Soc. 2006, 23, 34–54. [Google Scholar] [CrossRef]
- Löfqvist, C.; Granbom, M.; Himmelsbach, I.; Iwarsson, S.; Oswald, F.; Haak, M. Voices on relocation and aging in place in very old age—A complex and ambivalent matter. Gerontologist 2013, 53, 919–927. [Google Scholar] [CrossRef]
- Lee, H.C.; Park, H.; Choung, W.I. An analysis on the factors to affect the settlement consciousness of inhabitants. Korea Assoc. Pol. Stud. 2004, 13, 147–168. [Google Scholar]
- Lee, Y.; Kang, E.; Kim, S.; Byun, J. Suggestion of Long-Term Care System Reform in View of Aging in Place (AIP); Korea Institute for Health and Social Affairs: Sejong, Republic of Korea, 2017. [Google Scholar]
- Park, G.; Choe, B. Association between unmet healthcare needs and unmet long-term care needs among the Korean elderly. Health Soc. Welf. Rev. 2018, 38, 40–56. [Google Scholar] [CrossRef]
- Béland, F.; Bergman, H.; Lebel, P.; Dallaire, L.; Fletcher, J.; Tousignant, P.; Contandriopoulos, A. Integrated services for frail elders (SIPA): A trial of a model for Canada. Can. J. Aging 2006, 25, 25–42. [Google Scholar] [CrossRef]
- World Health Organization. Integrated Care for Older People (ICOPE) Implementation Framework: Guidance for Systems and Services. 2019. Available online: https://www.who.int/publications/i/item/9789241515993 (accessed on 11 September 2022).
- Ministry of Land, Infrastructure and Transport. Korea Housing Survey. 2020. Available online: https://stat.molit.go.kr/portal/cate/statFileView.do?hRsId=327&hFormId=&hSelectId=&sStyleNum=&sStart=&sEnd=&hPoint=&hAppr= (accessed on 11 September 2022).
- Kim, H.S.; Park, S. Comparative analysis on domestic and overseas design guidelines for aging in place. J. Archit. Inst. Korea 2019, 35, 19–28. [Google Scholar]
- Pynoos, J.; Regnier, V. Housing the Aged: Design Directives and Policy Considerations; Elsevier Science Publishing Company Incorporated: New York, NY, USA, 1987. [Google Scholar]
- World Health Organization. WHO Clinical Consortium on Healthy Ageing 2021: Report of Consortium Meeting Held Virtually, 5-6 November 2021. Available online: https://www.who.int/news/item/02-11-2021-who-clinical-consortium-on-healthy-ageing-meeting-2021 (accessed on 20 September 2022).
| Factor | N (Weighted %) | t or f or χ2 | p-Value | |||
|---|---|---|---|---|---|---|
| Total (n = 9930) | Not AIP (n = 1605) | AIP (n = 8326) | ||||
| Sex | Male | 4282(43.1) | 671(41.8) | 3611(43.4) | 1.30 | 0.255 |
| Female | 5648(56.9) | 933(58.2) | 4715(56.6) | |||
| Age | 65–74 years | 5656(57.0) | 1004(62.6) | 4652(55.9) | 24.78 | <0.001 |
| ≥75 years | 4274(43.0) | 600(37.4) | 3674(44.1) | |||
| Educational level | Primary | 4157(41.9) | 561(35.0) | 3596(43.2) | 37.88 | <0.001 |
| Middle | 2322(23.4) | 430(26.8) | 1892(22.7) | |||
| High | 3451(34.8) | 613(38.2) | 2838(34.1) | |||
| Annual household income quartiles (10,000 Korean won) | 0–494 | 2466(24.8) | 431(26.9) | 2035(24.4) | 23.66 | <0.001 |
| 495–899 | 2481(25.0) | 331(20.6) | 2150(25.8) | |||
| 900–1999 | 2499(25.2) | 397(24.7) | 2102(25.2) | |||
| above 2000 | 2486(25.0) | 446(27.8) | 2040(24.5) | |||
| Living together | 7945(80.0) | 1188(74.1) | 6757(81.2) | 42.28 | <0.001 | |
| Living arrangements | Living alone | 1985(20.0) | 416(25.9) | 1569(18.8) | ||
| House ownership | No | 2008(20.2) | 718(44.8) | 1290(15.5) | 714.20 | <0.001 |
| Yes | 7922(79.8) | 886(55.2) | 7036(84.5) | |||
| Current smoker | No | 8747(88.1) | 1361(84.9) | 7386(88.7) | 19.09 | <0.001 |
| Yes | 1183(11.9) | 243(15.1) | 940(11.3) | |||
| Physical exercise | No | 4559(45.9) | 793(49.4) | 3766(45.2) | 9.45 | 0.002 |
| Yes | 5372(54.1) | 812(50.6) | 4560(54.8) | |||
| Depressive symptoms | No | 9105(91.7) | 1422(88.7) | 7683(92.3) | 23.18 | <0.001 |
| Yes | 825(8.3) | 182(11.3) | 643(7.7) | |||
| Fall experience | No | 9222(92.9) | 1429(89.1) | 7793(93.6) | 41.29 | <0.001 |
| Yes | 708(7.1) | 175(10.9) | 533(6.4) | |||
| Cognitive impairment | No | 6733(67.8) | 1108(69.1) | 5625(67.6) | 1.42 | 0.234 |
| Yes | 3197(32.2) | 496(30.9) | 2701(32.4) | |||
| Region | Urban | 7518(75.7) | 1309(81.6) | 6209(74.6) | 36.19 | <0.001 |
| Rural | 2412(24.3) | 295(18.4) | 2117(25.4) | |||
| Crime exposure | No | 9545(96.1) | 1467(91.4) | 8078(97) | 113.75 | <0.001 |
| Yes | 386(3.9) | 138(8.6) | 248(3) | |||
| Unmet healthcare needs | No | 9684(97.5) | 1541(96.1) | 8143(97.8) | 16.66 | <0.001 |
| Yes | 246(2.5) | 63(3.9) | 183(2.2) | |||
| Frequency of kin contact | None | 597(6.0) | 155(9.7) | 442(5.3) | 60.75 | <0.001 |
| <1/month | 891(9.0) | 97(6.0) | 794(9.5) | |||
| ≥1/month | 8444(85.0) | 1353(84.3) | 7091(85.2) | |||
| Basic pensioner | No | 2844(28.6) | 543(33.8) | 2301(27.6) | 25.27 | <0.001 |
| Yes | 7087(71.4) | 1062(66.2) | 6025(72.4) | |||
| Annual income | 1658.96 ± 55.21 | 1552.32 ± 28.62 | 1569.55 ± 25.60 | 1.53 | 0.125 | |
| Age (years) | 73.68 ± 6.46 | 73.10 ± 6.3 | 73.79 ± 6.48 | −3.92 | <0.001 | |
| Residential satisfaction | 3.82 ± 0.66 | 3.43 ± 0.75 | 3.89 ± 0.61 | −22.79 | <0.001 | |
| Number of comorbidities | 1.9 ± 1.53 | 2.01 ± 1.61 | 1.87 ± 1.51 | 3.29 | 0.001 | |
| K-IADL 1 | 10.63 ± 2.56 | 10.73 ± 2.73 | 10.61 ± 2.52 | 1.58 | 0.113 | |
| Community satisfaction | 25.87 ± 3.83 | 25.37 ± 3.96 | 25.96 ± 3.80 | −5.54 | <0.001 | |
| The total score of community care service needs | 22.29 ± 4.68 | 22.78 ± 4.73 | 22.20 ± 4.66 | 4.55 | <0.001 | |
| Number of long-term care services | 0.03 ± 0.29 | 0.03 ± 0.27 | 0.03 ± 0.30 | −0.26 | 0.794 | |
| Total | Not AIP | AIP | t | p-Value | |
|---|---|---|---|---|---|
| Improvement of living conditions such as home repairs | 2.35 ± 0.87 | 2.18 ± 0.82 | 2.38 ± 0.88 | −9.09 | <0.001 |
| Daily life support (housework, nursing, bathing, meal support, etc.) | 2.27 ± 0.99 | 2.23 ± 1.05 | 2.28 ± 0.98 | −1.72 | 0.086 |
| Safety support (regular safety checks, emergency referrals, etc.) | 2.24 ± 0.98 | 2.15 ± 0.98 | 2.26 ± 0.97 | −4.27 | <0.001 |
| Visiting medical and health services by doctors and nurses | 2.17 ± 0.98 | 2.15 ± 0.98 | 2.18 ± 0.98 | −1.04 | 0.298 |
| Transportation support services to a hospital | 2.24 ± 0.95 | 2.16 ± 0.98 | 2.25 ± 0.95 | −3.56 | <0.001 |
| Counseling services (providing necessary information for daily life, etc.) | 2.44 ± 0.88 | 2.36 ± 0.92 | 2.45 ± 0.88 | −3.78 | <0.001 |
| Factor | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | |
| Female (ref = male) | 0.87 (0.76–1.00) | 0.049 | 0.91 (0.79–1.04) | 0.162 | 0.9 (0.79–1.04) | 0.150 |
| ≥75 years (ref = 65–74 years) | 1.30 (1.13–1.49) | <0.001 | 1.30 (1.13–1.49) | <0.001 | 1.24 (1.07–1.42) | 0.003 |
| Educational level (ref = primary school) | ||||||
| Middle school | 0.63 (0.54–0.74) | <0.001 | 0.67 (0.57–0.79) | <0.001 | 0.68 (0.58–0.80) | <0.001 |
| High school | 0.56 (0.48–0.66) | <0.001 | 0.62 (0.52–0.73) | <0.001 | 0.67 (0.56–0.79) | <0.001 |
| Annual household income quartiles | 0.86 (0.81–0.91) | <0.001 | 0.86 (0.81–0.91) | <0.001 | 0.88 (0.83–0.93) | <0.001 |
| Living together (ref = living alone) | 0.89 (0.77–1.03) | 0.116 | 0.89 (0.76–1.03) | 0.107 | 0.88 (0.76–1.02) | 0.094 |
| House ownership (ref = no ownership) | 3.62 (3.19–4.12) | <0.001 | 3.58 (3.14–4.09) | <0.001 | 3.64 (3.19–4.16) | <0.001 |
| Residential satisfaction | 2.46 (2.26–2.69) | <0.001 | 2.45 (2.23–2.68) | <0.001 | 2.49 (2.27–2.73) | <0.001 |
| Smoking (ref = no smoking) | 0.79 (0.66–0.94) | 0.010 | 0.78 (0.65–0.94) | 0.009 | 0.79 (0.65–0.95) | 0.011 |
| Physical exercise (ref = no exercise) | 1.12 (0.99–1.26) | 0.062 | 1.12 (0.99–1.26) | 0.064 | 1.13 (1.00–1.28) | 0.048 |
| Depressive symptoms (ref = no symptom) | 0.65 (0.54–0.80) | <0.001 | 0.64 (0.5–0.78) | <0.001 | 0.64 (0.52–0.78) | <0.001 |
| Number of comorbidities | 1.00 (0.96–1.04) | 0.837 | 1.01 (0.9–1.05) | 0.528 | 1.01 (0.97–1.05) | 0.557 |
| Fall experience (ref = no) | 0.59 (0.48–0.72) | <0.001 | 0.63 (0.52–0.78) | <0.001 | 0.63 (0.51–0.77) | <0.001 |
| K-IADL | 1.02 (0.99–1.04) | 0.122 | 1.02 (1.00–1.05) | 0.057 | 1.02 (0.99–1.04) | 0.215 |
| Cognitive impairment (ref = no) | 1.08 (0.95–1.24) | 0.249 | 1.11 (0.96–1.27) | 0.155 | 1.09 (0.95–1.26) | 0.201 |
| Rural (ref = urban) | 1.39 (1.19–1.62) | <0.001 | 1.36 (1.17–1.58) | <0.001 | ||
| Community satisfaction | 1.01 (1.00–1.03) | 0.124 | 1.01 (1.00–1.03) | 0.116 | ||
| Crime exposure (ref = no) | 0.39 (0.30–0.49) | <0.001 | 0.41 (0.32–0.52) | <0.001 | ||
| Unmet healthcare service needs (ref = no) | 0.68 (0.49–0.94) | 0.021 | 0.66 (0.48–0.92) | 0.015 | ||
| The score for community care service needs | 0.97 (0.96–0.99) | <0.001 | 0.97 (0.96–0.99) | <0.001 | ||
| Frequency of kin contact (ref = none) | ||||||
| <1/month | 2.34 (1.71–3.19) | <0.001 | 2.29 (1.68–3.13) | <0.001 | ||
| ≥1/month | 1.18 (0.95–1.47) | 0.138 | 1.17 (0.94–1.46) | 0.165 | ||
| Basic pension (ref = no) | 1.42 (1.24–1.64) | <0.001 | ||||
| Number of long-term care services | 1.19 (0.94–1.52) | 0.148 | ||||
| R2 (p-value) | 0.196 (p < 0.001) | 0.217 (p < 0.001) | 0.221 (p < 0.001) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, M.S.; Kwon, M.Y. Factors Associated with Aging in Place among Community-Dwelling Older Adults in Korea: Findings from a National Survey. Int. J. Environ. Res. Public Health 2023, 20, 2740. https://doi.org/10.3390/ijerph20032740
Cho MS, Kwon MY. Factors Associated with Aging in Place among Community-Dwelling Older Adults in Korea: Findings from a National Survey. International Journal of Environmental Research and Public Health. 2023; 20(3):2740. https://doi.org/10.3390/ijerph20032740
Chicago/Turabian StyleCho, Myong Sun, and Mi Young Kwon. 2023. "Factors Associated with Aging in Place among Community-Dwelling Older Adults in Korea: Findings from a National Survey" International Journal of Environmental Research and Public Health 20, no. 3: 2740. https://doi.org/10.3390/ijerph20032740
APA StyleCho, M. S., & Kwon, M. Y. (2023). Factors Associated with Aging in Place among Community-Dwelling Older Adults in Korea: Findings from a National Survey. International Journal of Environmental Research and Public Health, 20(3), 2740. https://doi.org/10.3390/ijerph20032740








