The Efficacy and Safety of the GATT Procedure in Open-Angle Glaucoma—6-Month Results
Abstract
:1. Introduction
2. Material and Methods
Studied Group
3. Methods
3.1. GATT Procedure
3.2. Combined Procedure—GATT with Cataract Extraction
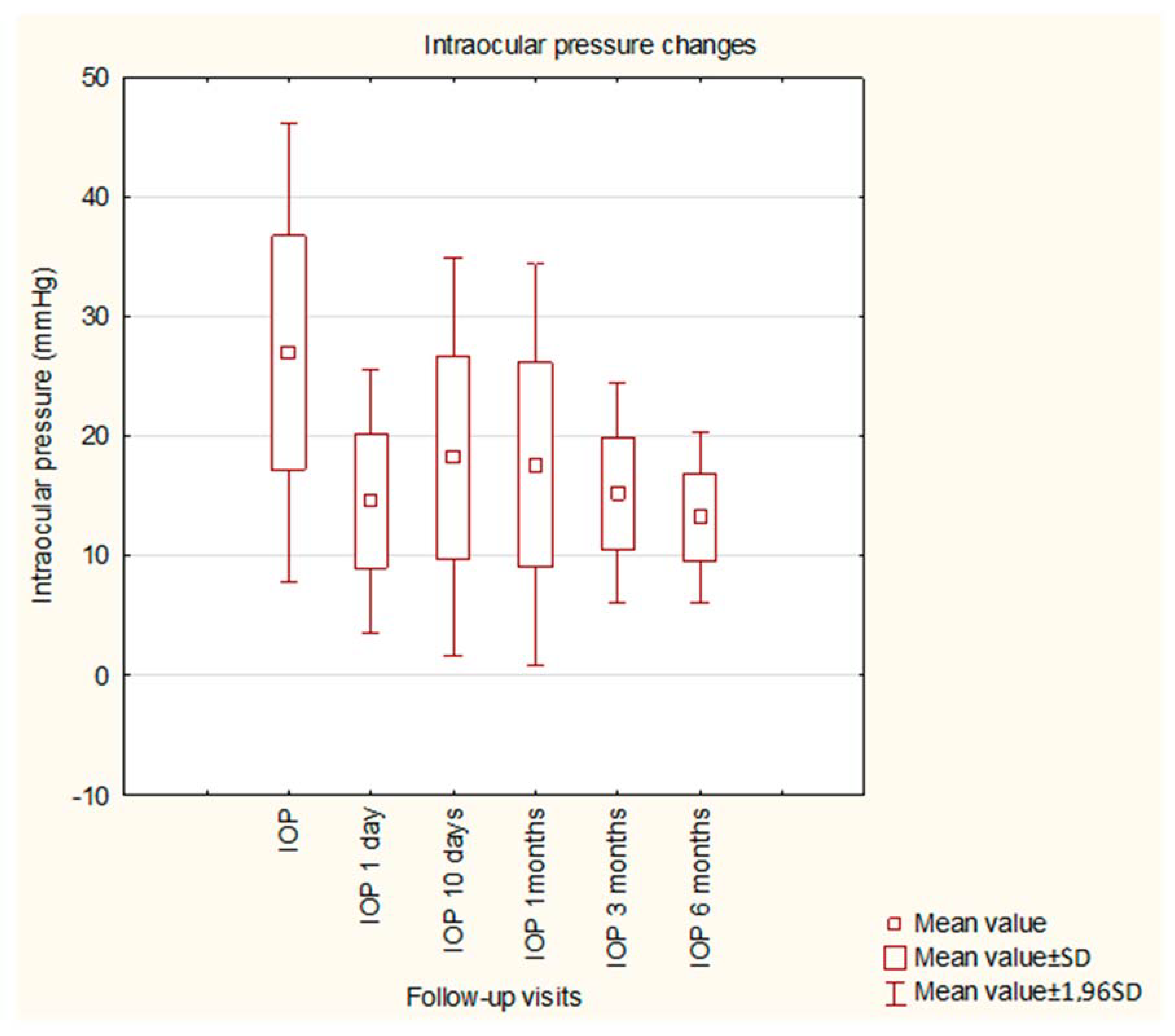
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jonas, J.B.; Aung, T.; Bourne, R.R.; Bron, A.M.; Ritch, R.; Panda-Jonas, S. Glaucoma. Lancet 2017, 390, 2183–2193. [Google Scholar] [CrossRef] [PubMed]
- Rulli, E.; Biagioli, E.; Riva, I.; Gambirasio, G.; De Simone, I.; Floriani, I.; Quaranta, L. Efficacy and Safety of Trabeculectomy vs Nonpenetrating Surgical Procedures: A systematic review and meta-analysis. JAMA Ophthalmol 2013, 131, 1573–1582. [Google Scholar] [CrossRef] [PubMed]
- Leung, D.Y.L.; Tham, C.C.Y. Management of Bleb Complications after Trabeculectomy. Semin. Ophthalmol. 2013, 28, 144–156. [Google Scholar] [CrossRef] [PubMed]
- Edmunds, B.; Thompson, J.R.; Salmon, J.F.; Wormald, R.P. The National Survey of Trabeculectomy. III. Early and late complications. Eye 2002, 16, 297–303. [Google Scholar] [CrossRef]
- Sihota, R.; Angmo, D.; Ramaswamy, D.; Dada, T. Simplifying “target” intraocular pressure for different stages of primary open-angle glaucoma and primary angle-closure glaucoma. Indian J. Ophthalmol. 2018, 66, 495–505. [Google Scholar] [CrossRef]
- Grover, D.S.; Godfrey, D.G.; Smith, O.; Feuer, W.J.; de Oca, I.M.; Fellman, R.L. Gonioscopy-Assisted Transluminal Trabeculotomy, Ab Interno Trabeculotomy: Technique report and preliminary results. Ophthalmology 2014, 121, 855–861. [Google Scholar] [CrossRef]
- Aktas, Z.M.; Zeydanli, E.M.O.; Uysal, B.S.; Yigiter, A. Outcomes of Prolene Gonioscopy-assisted Transluminal Trabeculotomy in Primary Open-angle Glaucoma and Pseudoexfoliative Glaucoma: A Comparative Study. Eur. J. Gastroenterol. Hepatol. 2022. [Google Scholar] [CrossRef]
- Aktas, Z.; Ucgul, A.Y.; Ozdek, S.; Boluk, C.E. Outcomes of Gonioscopy-assisted Transluminal Trabeculotomy in Vitrectomized Patients With Secondary Glaucoma After Silicone Oil Removal. Eur. J. Gastroenterol. Hepatol. 2021, 30, e114–e118. [Google Scholar] [CrossRef]
- Belkin, A.; Chaban, Y.V.; Waldner, D.; Samet, S.; Ahmed, I.I.K.; Gooi, P.; Schlenker, M.B. Gonioscopy-assisted transluminal trabeculotomy is an effective surgical treatment for uveitic glaucoma. Br. J. Ophthalmol. 2021. [Google Scholar] [CrossRef]
- Quan, A.V.; Chen, J.; Wang, Y.E.; Vanner, E.A.; Grajewski, A.L.; Hodapp, E.A.; Chang, T.C. Factors Associated With Gonioscopy-Assisted Transluminal Trabeculotomy (GATT) Complications and Failure in Children. Am. J. Ophthalmol. 2022, 241, 168–178. [Google Scholar] [CrossRef]
- Vizzeri, G.; Weinreb, R.N. Cataract surgery and glaucoma. Curr. Opin. Ophthalmol. 2010, 21, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.; Law, G.; Ahmed, I.I.K. Glaucoma and cataract surgery: Two roads merging into one. Curr. Opin. Ophthalmol. 2016, 27, 51–57. [Google Scholar] [CrossRef]
- Zhang, M.L.; Hirunyachote, P.; Jampel, H. Combined surgery versus cataract surgery alone for eyes with cataract and glaucoma. Cochrane Database Syst. Rev. 2015, 2015, CD008671. [Google Scholar] [CrossRef] [PubMed]
- Casson, R.J.; Salmon, J.F. Combined surgery in the treatment of patients with cataract and primary open-angle glaucoma. J. Cataract. Refract. Surg. 2001, 27, 1854–1863. [Google Scholar] [CrossRef]
- Lazcano-Gomez, G.; SooHoo, J.R.; Jung, J.L.; Isida-Llerandi, C.G.; Kahook, M.Y. Intraocular Pressure Control after Trabeculectomy, Phacotrabeculectomy and Phacoemulsification in a Hispanic Population. Curr. J. Glaucoma Pr. DVD 2014, 8, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Lam, D.; Wechsler, D.Z. Five-Year Outcomes of Trabeculectomy and Phacotrabeculectomy. Cureus 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Ahmadzadeh, A.; Kessel, L.; Subhi, Y.; Bach-Holm, D. Comparative Efficacy of Phacotrabeculectomy versus Trabeculectomy with or without Later Phacoemulsification: A Systematic Review with Meta-Analyses. J. Ophthalmol. 2021, 2021, 1–17. [Google Scholar] [CrossRef]
- Grover, D.S.; Smith, O.; Fellman, R.L.; Godfrey, D.G.; Gupta, A.; Montes de Oca, I.; Feuer, W.J. Gonioscopy-assisted transluminal tra-beculotomy: An ab interno circumferential trabeculotomy: 24 months follow-up. J. Glaucoma. 2018, 27, 393–401. [Google Scholar] [CrossRef]
- Aktas, Z.; Ucgul, A.Y.; Bektas, C.; Karamert, S.S. Surgical Outcomes of Prolene Gonioscopy-assisted Transluminal Trabeculotomy in Patients With Moderate to Advanced Open-Angle Glaucoma. Eur. J. Gastroenterol. Hepatol. 2019, 28, 884–888. [Google Scholar] [CrossRef]
- Rahmatnejad, K.; Pruzan, N.L.; Amanullah, S.; Shaukat, B.A.; Resende, A.F.; Waisbourd, M.; Zhan, T.; Moster, M.R. Surgical Outcomes of Gonioscopy-assisted Transluminal Trabeculotomy (GATT) in Patients With Open-angle Glaucoma. Eur. J. Gastroenterol. Hepatol. 2017, 26, 1137–1143. [Google Scholar] [CrossRef]
- Grover, D.S.; Smith, O.; Fellman, R.L.; Godfrey, D.G.; Butler, M.R.; de Oca, I.M.; Feuer, W.J. Gonioscopy assisted transluminal trabeculotomy: An ab interno circumferential trabeculotomy for the treatment of primary congenital glaucoma and juvenile open angle glaucoma. Br. J. Ophthalmol. 2015, 99, 1092–1096. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.-Y.; Qi, X.-H.; Qi, J.-M. Systematic review and Meta-analysis of treating open angle glaucoma with gonioscopy-assisted transluminal trabeculotomy. Int. J. Ophthalmol. 2020, 13, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Fontana, L.; De Maria, M.; Caristia, A.; Mastrofilippo, V.; Braglia, L.; Iannetta, D.; Scarale, G.P. Comparison of Gonioscopy-assisted Transluminal Trabeculotomy Versus Trabeculectomy With Mitomycin C in Patients With Open-angle Glaucoma. Eur. J. Gastroenterol. Hepatol. 2021, 30, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Bao, W.; Kawase, K.; Huang, H.; Sawada, A.; Yamamoto, T. The long-term outcome of trabeculotomy: Comparison with filtering surgery in Japan. BMC Ophthalmol. 2019, 19, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Inoue, K. Managing adverse effects of glaucoma medications. Clin. Ophthalmol. 2014, 8, 903–913. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.L.; Ellyson, A.C.; Kim, W.I. Trabectome-Initiated Gonioscopy-Assisted Transluminal Trabeculotomy. Mil. Med. 2018, 183 (Suppl. 1), 146–149. [Google Scholar] [CrossRef]
- Sato, T.; Hirata, A.; Mizoguchi, T. Prospective, noncomparative, nonrandomized case study of short-term outcomes of 360° suture trabeculotomy ab interno in patients with open-angle glaucoma. Clin Ophthalmol. 2015, 9, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Sarkisian, S.R.; Mathews, B.; Ding, K.; Patel, A.; Nicek, Z. 360° ab-interno trabeculotomy in refractory primary open-angle glaucoma. Clin. Ophthalmol. 2019, 13, 161–168. [Google Scholar] [CrossRef]
- de Faria, B.M.; Melillo, G.H.D.L.; Daga, F.; Kanadani, F.N.; Prata, T.S. Short-term endothelial cell density changes after gonioscopy-assisted transluminal trabeculotomy. Arq. Bras. de Oftalmol. 2021, 85, 344–350. [Google Scholar] [CrossRef]
- Johnson, D.H.; Matsumoto, Y. Schlemm’s canal becomes smaller after successful filtration surgery. Arch Ophthalmol. 2000, 118, 1251–1256. [Google Scholar] [CrossRef]
- Grover, D.S.; Godfrey, D.G.; Smith, O.; Shi, W.; Feuer, W.J.; Fellman, R.L. Outcomes of Gonioscopy-assisted Transluminal Trabeculotomy (GATT) in Eyes With Prior Incisional Glaucoma Surgery. Eur. J. Gastroenterol. Hepatol. 2017, 26, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Cubuk, M.O.; Ucgul, A.Y.; Unsal, E. Gonioscopy-assisted transluminal trabeculotomy as an option after failed trabeculectomy. Int. Ophthalmol. 2020, 40, 1923–1930. [Google Scholar] [CrossRef] [PubMed]

| Feature | |
|---|---|
| Number of patients | 69 |
| Age | 69.48 +/− 11.30 years |
| Gender | 35 F; 34 M |
| Type of glaucoma | 48 POAG; 21 PEXG |
| IOP before surgery | 26.94 mmHg +/− 9.70 |
| VFI before surgery | 58.36 % +/− 23.91 |
| MD before surgery | −8.20 dB +/− 12.38 |
| Number of drugs before surgery | 2.59 |
| BCVA before surgery (decimal scale) | 0.47 +/− 0.32 |
| Previous intraocular surgery | Cataract surgery: 27 Previous antiglaucoma surgery: 8 (trabeculectomy: 6; NPDS: 1; XEN: 1; MiniExpress: 1, revision of the bleb: 3) |
| 30% Decrease in IOP | 1D | 10D | 1M | 3M | 6M |
|---|---|---|---|---|---|
| S | 79.7% (55) | 66.7% (46) | 62.3% (43) | 59.4% (41) | 57.9% (40) |
| QS | 1.4% (1) | 7.2% (5) | 20.4% (14) | 36.2% (25) | 37.7% (26) |
| F | 18.9% (13) | 26.1% (18) | 17.3% (12) | 4.4% (3) | 4.4% (3) |
| IOP ≤ 18 mmHg | 1D | 10D | 1M | 3M | 6M |
|---|---|---|---|---|---|
| S | 78.3% (54) | 62.3% (43) | 59.4% (41) | 55.1% (38) | 58.0% (40) |
| QS | 1.4% (1) | 4.3% (3) | 18.8% (13) | 36.2% (25) | 33.3% (23) |
| F | 20.3% (14) | 33.4% (23) | 21.8% (15) | 8.7% (6) | 8.7% (6) |
| Complication | Number/Percentage |
|---|---|
| Hyphema | 35/69 (50.7%) |
| Transient visual loss | 3/69 (4.3%) |
| Irydodialisis | 2/69 (2.9%) |
| Corneal oedema | 2/69 (2.9%) |
| Vitreous hemorrhage | 1/69 (1.4%) |
| Additional antiglaucoma surgery | 3/69 (4.3%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ćwiklińska-Haszcz, A.; Żarnowski, T.; Wróbel-Dudzińska, D.; Kosior-Jarecka, E. The Efficacy and Safety of the GATT Procedure in Open-Angle Glaucoma—6-Month Results. Int. J. Environ. Res. Public Health 2023, 20, 2759. https://doi.org/10.3390/ijerph20032759
Ćwiklińska-Haszcz A, Żarnowski T, Wróbel-Dudzińska D, Kosior-Jarecka E. The Efficacy and Safety of the GATT Procedure in Open-Angle Glaucoma—6-Month Results. International Journal of Environmental Research and Public Health. 2023; 20(3):2759. https://doi.org/10.3390/ijerph20032759
Chicago/Turabian StyleĆwiklińska-Haszcz, Agnieszka, Tomasz Żarnowski, Dominika Wróbel-Dudzińska, and Ewa Kosior-Jarecka. 2023. "The Efficacy and Safety of the GATT Procedure in Open-Angle Glaucoma—6-Month Results" International Journal of Environmental Research and Public Health 20, no. 3: 2759. https://doi.org/10.3390/ijerph20032759
APA StyleĆwiklińska-Haszcz, A., Żarnowski, T., Wróbel-Dudzińska, D., & Kosior-Jarecka, E. (2023). The Efficacy and Safety of the GATT Procedure in Open-Angle Glaucoma—6-Month Results. International Journal of Environmental Research and Public Health, 20(3), 2759. https://doi.org/10.3390/ijerph20032759






