Spine Alignment in Standing and Maximal Upper Limb Elevation in Baseball Players with Lumbar Spondylolysis and Those without Low Back Pain
Abstract
1. Introduction
2. Subjects and Methods
2.1. Subjects
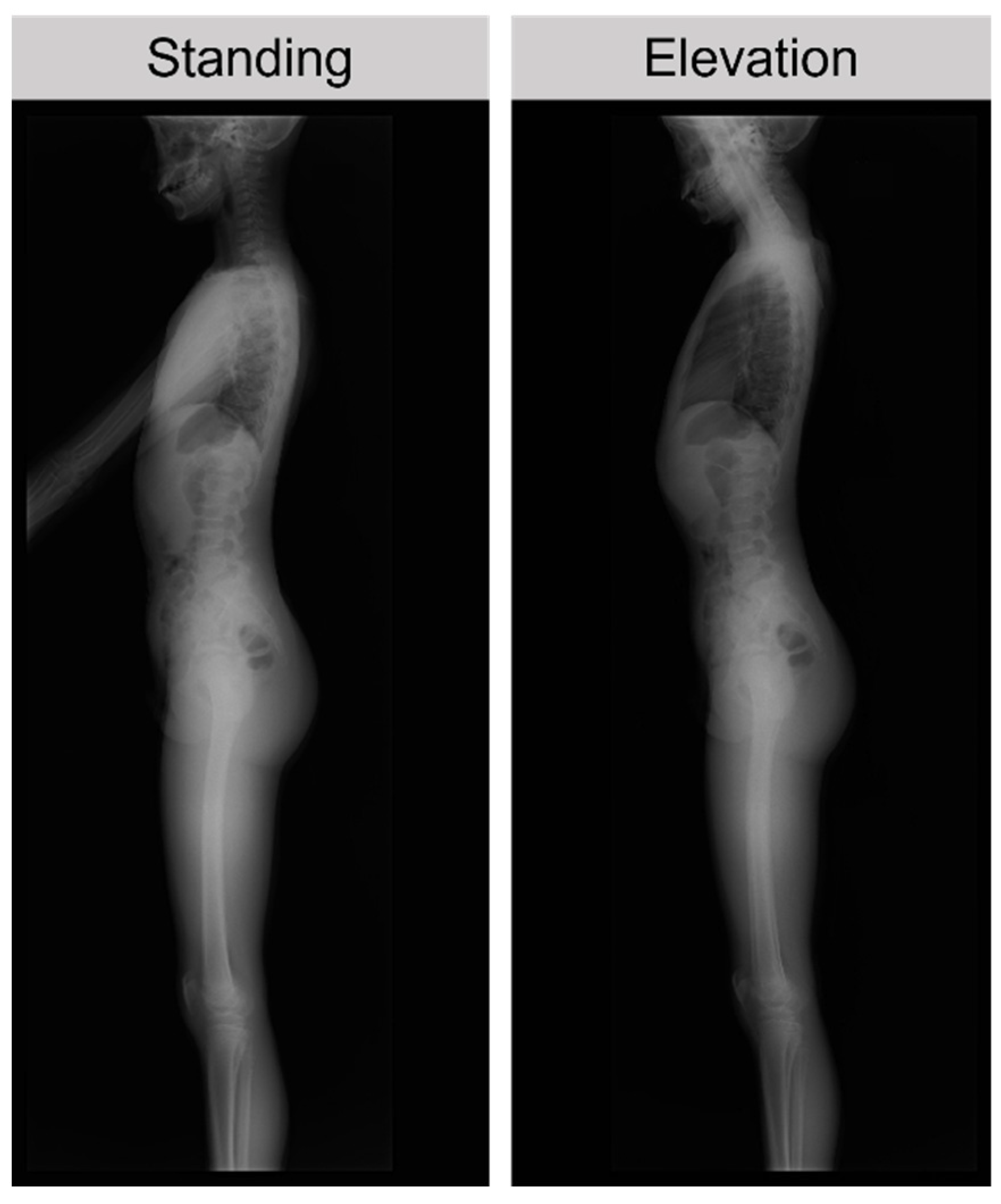
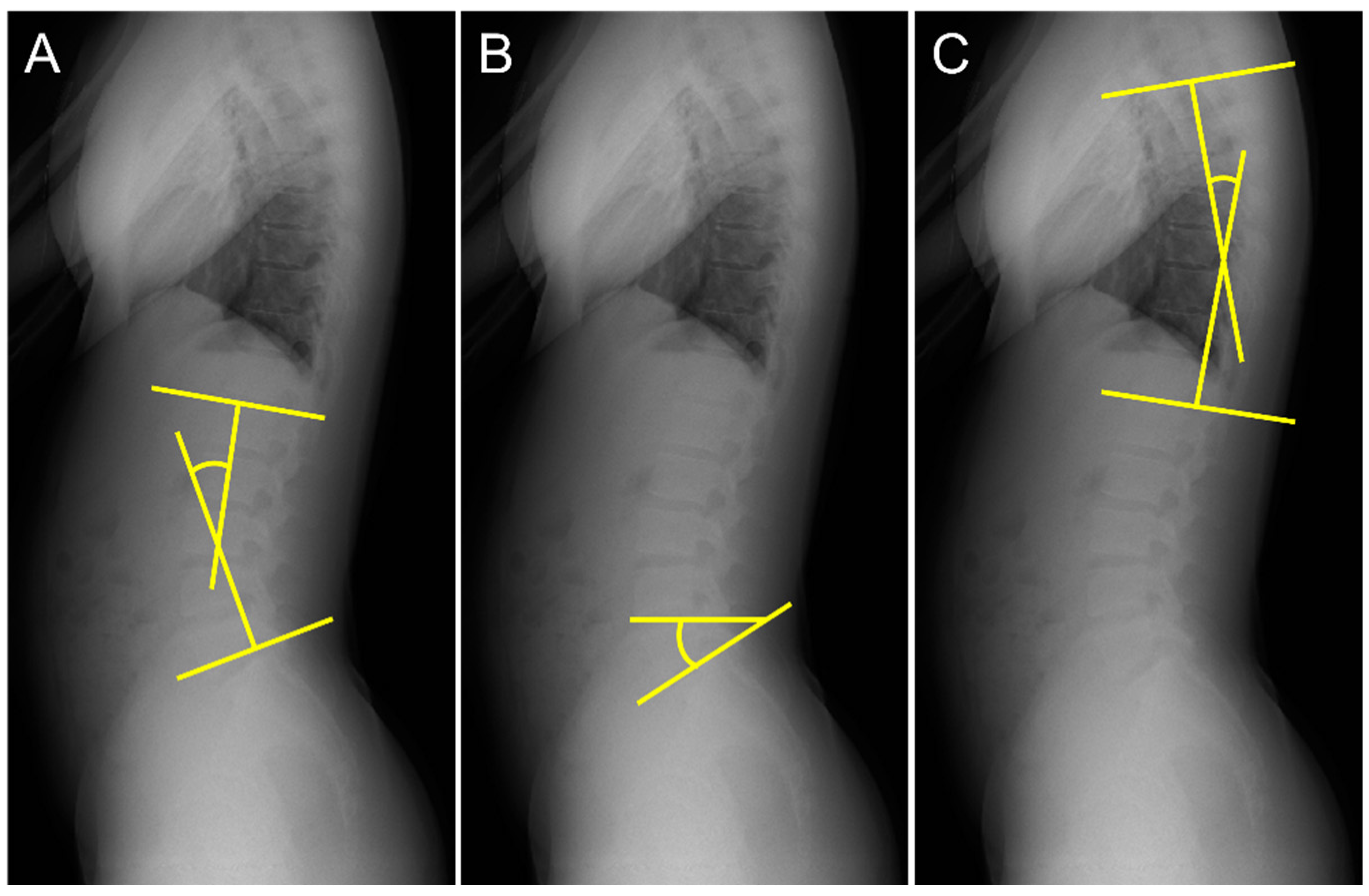
2.2. Measurements
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wasser, J.G.; Zaremski, J.L.; Herman, D.C.; Vincent, H.K. Prevalence and proposed mechanisms of chronic low back pain in baseball: Part i. Res. Sports Med. 2017, 25, 219–230. [Google Scholar] [CrossRef] [PubMed]
- Wiltse, L.L.; Widell, E.H.; Jackson, D.W. Fatigue fracture: The basic lesion is inthmic spondylolisthesis. J. Bone Jt. Surg. 1975, 57, 17–22. [Google Scholar] [CrossRef]
- Randall, R.M.; Silverstein, M.; Goodwin, R. Review of Pediatric Spondylolysis and Spondylolisthesis. Sports Med. Arthrosc. Rev. 2016, 24, 184–187. [Google Scholar] [CrossRef] [PubMed]
- Grazina, R.; Andrade, R.; Santos, F.L.; Marinhas, J.; Pereira, R.; Bastos, R.; Espregueira-Mendes, J. Return to play after conservative and surgical treatment in athletes with spondylolysis: A systematic review. Phys. Ther. Sport 2019, 37, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Sakai, T.; Tezuka, F.; Yamashita, K.; Takata, Y.; Higashino, K.; Nagamachi, A.; Sairyo, K. Conservative Treatment for Bony Healing in Pediatric Lumbar Spondylolysis. Spine 2017, 42, E716–E720. [Google Scholar] [CrossRef] [PubMed]
- Cooper, G. Non-Operative Treatment of the Lumbar Spine; Springer: Cham, Switzerland, 2015. [Google Scholar] [CrossRef]
- El Rassi, G.; Takemitsu, M.; Glutting, J.; Shah, S.A. Effect of Sports Modification on Clinical Outcome in Children and Adolescent Athletes with Symptomatic Lumbar Spondylolysis. Am. J. Phys. Med. Rehabil. 2013, 92, 1070–1074. [Google Scholar] [CrossRef] [PubMed]
- Matsuzawa, K.; Matsui, T.; Azuma, Y.; Miyazaki, T.; Hiramoto, M.; Hashimoto, R.; Kida, N.; Morihara, T. Comparison of alignment and spondylolysis fracture angle in bilateral and unilateral spondylolysis. PLoS ONE 2022, 17, e0276337. [Google Scholar] [CrossRef] [PubMed]
- Roussouly, P.; Gollogly, S.; Berthonnaud, E.; Labelle, H.; Weidenbaum, M. Sagittal Alignment of the Spine and Pelvis in the Presence of L5–S1 Isthmic Lysis and Low-Grade Spondylolisthesis. Spine 2006, 31, 2484–2490. [Google Scholar] [CrossRef] [PubMed]
- Iwaki, K.; Sakai, T.; Hatayama, D.; Hayashi, Y.; Inoue, N.; Matsumoto, M.; Hattori, Y.; Goto, T.; Sairyo, K.; Tsuji, S.; et al. Physical features of pediatric patients with lumbar spondylolysis and effectiveness of rehabilitation. J. Med. Investig. 2018, 65, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Sato, M.; Mase, Y.; Sairyo, K. Active stretching for lower extremity muscle tightness in pediatric patients with lumbar spondylolysis. J. Med. Investig. 2017, 64, 136–139. [Google Scholar] [CrossRef] [PubMed]
- Thein-Nissenbaum, J.; Boissonnault, W.G. Differential Diagnosis of Spondylolysis in a Patient with Chronic Low Back Pain. J. Orthop. Sports Phys. Ther. 2005, 35, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Sugawara, K.; Iesato, N.; Katayose, M. Segmental Lordosis of the Spondylolytic Vertebrae in Adolescent Lumbar Spondylolysis: Differences between Bilateral L5 and L4 Spondylolysis. Asian Spine J. 2018, 12, 1037–1042. [Google Scholar] [CrossRef] [PubMed]
- Labelle, H.; Mac-Thiong, J.-M.; Roussouly, P. Spino-pelvic sagittal balance of spondylolisthesis: A review and classification. Eur. Spine J. 2011, 20, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Nissen, C.W.; Westwell, M.; Õunpuu, S.; Patel, M.; Tate, J.P.; Pierz, K.; Burns, J.P.; Bicos, J. Adolescent baseball pitching technique: A detailed three-dimensional biomechanical analysis. Med. Sci. Sports Exerc. 2007, 39, 1347–1357. [Google Scholar] [CrossRef] [PubMed]
- Kapandji, I.A. The Physiology of the Joints, Volume I, Upper Limb. Am. J. Phys. Med. Rehabil. 1971, 50, 96. [Google Scholar]
- Barrett, E.; O’Keeffe, M.; O’Sullivan, K.; Lewis, J.; McCreesh, K. Is thoracic spine posture associated with shoulder pain, range of motion and function? A systematic review. Man. Ther. 2016, 26, 38–46. [Google Scholar] [CrossRef]
- Sairyo, K. Spondylolysis Fracture Angle in Children and Adolescents on CT Indicates the Facture Producing Force Vector: A Biomechanical Rationale. Internet J. Spine Surg. 2005, 1, 2. [Google Scholar]
- Matsumoto, M.E.; Czerniecki, J.M.; Shakir, A.; Suri, P.; Orendurff, M.; Morgenroth, D.C. The relationship between lumbar lordosis angle and low back pain in individuals with transfemoral amputation. Prosthetics Orthot. Int. 2018, 43, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Marty, C.; Boisaubert, B.; Descamps, H.; Montigny, J.; Hecquet, J.; Legaye, J.; Duval-Beaupère, G. The sagittal anatomy of the sacrum among young adults, infants, and spondylolisthesis patients. Eur. Spine J. 2002, 11, 119–125. [Google Scholar] [CrossRef]
- Richardson, J.T.E. Eta squared and partial eta squared as measures of effect size in educational research. Educ. Res. Rev. 2011, 6, 135–147. [Google Scholar] [CrossRef]
- Bernhardt, M.; Bridwell, K.H. Segmental Analysis of the Sagittal Plane Alignment of the Normal Thoracic and Lumbar Spines and Thoracolumbar Junction. Spine 1989, 14, 717–721. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.; Lafage, V.; Boyce, R.; Skalli, W.; Farcy, J.-P. Gravity Line Analysis in Adult Volunteers. Spine 2006, 31, E959–E967. [Google Scholar] [CrossRef] [PubMed]
- Roussouly, P.; Gollogly, S.; Berthonnaud, E.; Dimnet, J. Classification of the Normal Variation in the Sagittal Alignment of the Human Lumbar Spine and Pelvis in the Standing Position. Spine 2005, 30, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Abelin-Genevois, K. Sagittal balance of the spine. Orthop. Traumatol. Surg. Res. 2020, 107, 102769. [Google Scholar] [CrossRef]
| Spondylolysis | Control | ||
| Lumbar lordosis angle (LL, °) | Standing | 36.9 ± 5.1 a | 29.0 ± 5.2 |
| Elevation position | 39.9 ± 7.9 a | 30.5 ± 4.7 | |
| Sacral slope angle (SS, °) | Standing | 35.1 ± 6.4 b | 26.9 ± 5.3 c |
| Elevation position | 36.6 ± 5.8 | 31.8 ± 6.3 | |
| Thoracic kyphosis angle (TK, °) | Standing | 22.1 ± 5.2 | 23.4 ± 3.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsuzawa, K.; Matsui, T.; Azuma, Y.; Miyazaki, T.; Hiramoto, M.; Hashimoto, R.; Kida, N.; Morihara, T. Spine Alignment in Standing and Maximal Upper Limb Elevation in Baseball Players with Lumbar Spondylolysis and Those without Low Back Pain. Int. J. Environ. Res. Public Health 2023, 20, 3231. https://doi.org/10.3390/ijerph20043231
Matsuzawa K, Matsui T, Azuma Y, Miyazaki T, Hiramoto M, Hashimoto R, Kida N, Morihara T. Spine Alignment in Standing and Maximal Upper Limb Elevation in Baseball Players with Lumbar Spondylolysis and Those without Low Back Pain. International Journal of Environmental Research and Public Health. 2023; 20(4):3231. https://doi.org/10.3390/ijerph20043231
Chicago/Turabian StyleMatsuzawa, Kanta, Tomoyuki Matsui, Yoshikazu Azuma, Tetsuya Miyazaki, Machiko Hiramoto, Ruo Hashimoto, Noriyuki Kida, and Toru Morihara. 2023. "Spine Alignment in Standing and Maximal Upper Limb Elevation in Baseball Players with Lumbar Spondylolysis and Those without Low Back Pain" International Journal of Environmental Research and Public Health 20, no. 4: 3231. https://doi.org/10.3390/ijerph20043231
APA StyleMatsuzawa, K., Matsui, T., Azuma, Y., Miyazaki, T., Hiramoto, M., Hashimoto, R., Kida, N., & Morihara, T. (2023). Spine Alignment in Standing and Maximal Upper Limb Elevation in Baseball Players with Lumbar Spondylolysis and Those without Low Back Pain. International Journal of Environmental Research and Public Health, 20(4), 3231. https://doi.org/10.3390/ijerph20043231






