The Feasibility of a Text-Messaging Intervention Promoting Physical Activity in Shift Workers: A Process Evaluation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Recruitment and Participants
2.3. Intervention
2.3.1. Action Planning
2.3.2. Text Messages
2.3.3. Ecological Momentary Assessment Survey
2.4. Control Group
2.5. Data Collection
2.5.1. Questionnaires
2.5.2. Device-Based Accelerometer Measures
2.5.3. Researcher Logbook
2.5.4. Online Exit Questionnaire
2.5.5. Interviews
2.6. Data Analyses
2.6.1. Sample Size
2.6.2. Quantitative Data
2.6.3. Qualitative Data Analysis
3. Results
3.1. Process Outcome Results
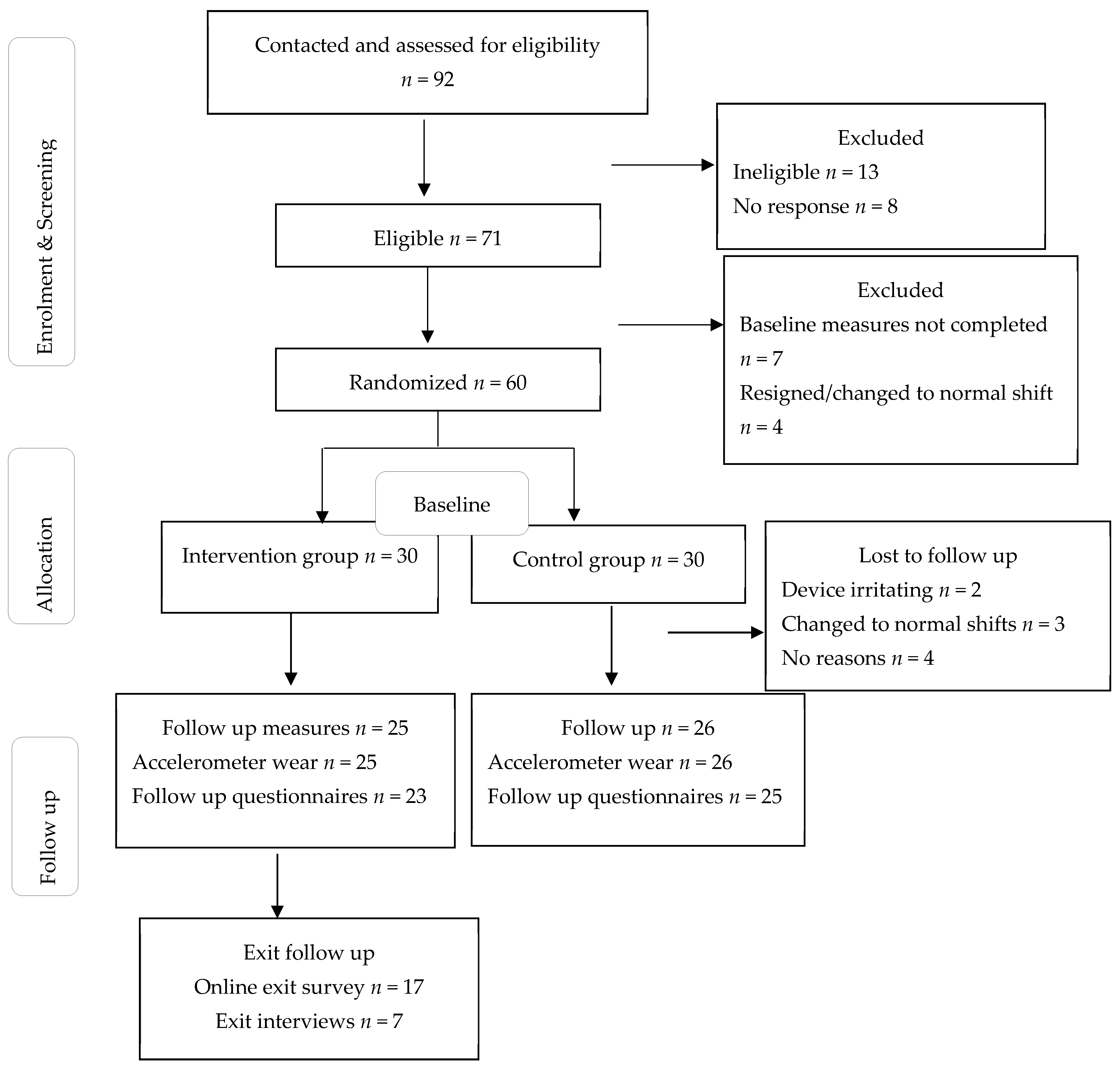
3.1.1. Reach
3.1.2. Adoption
3.1.3. Implementation
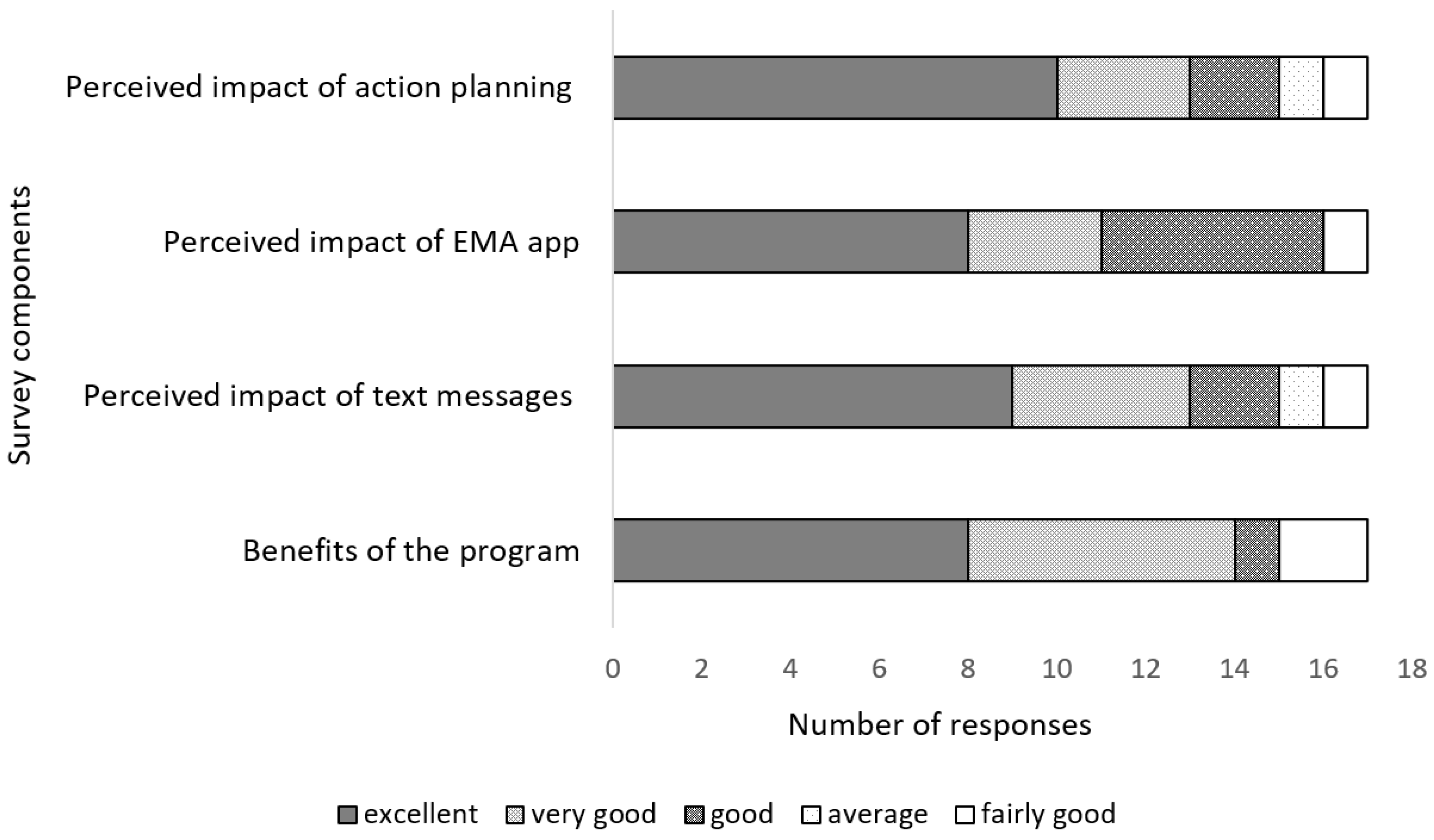
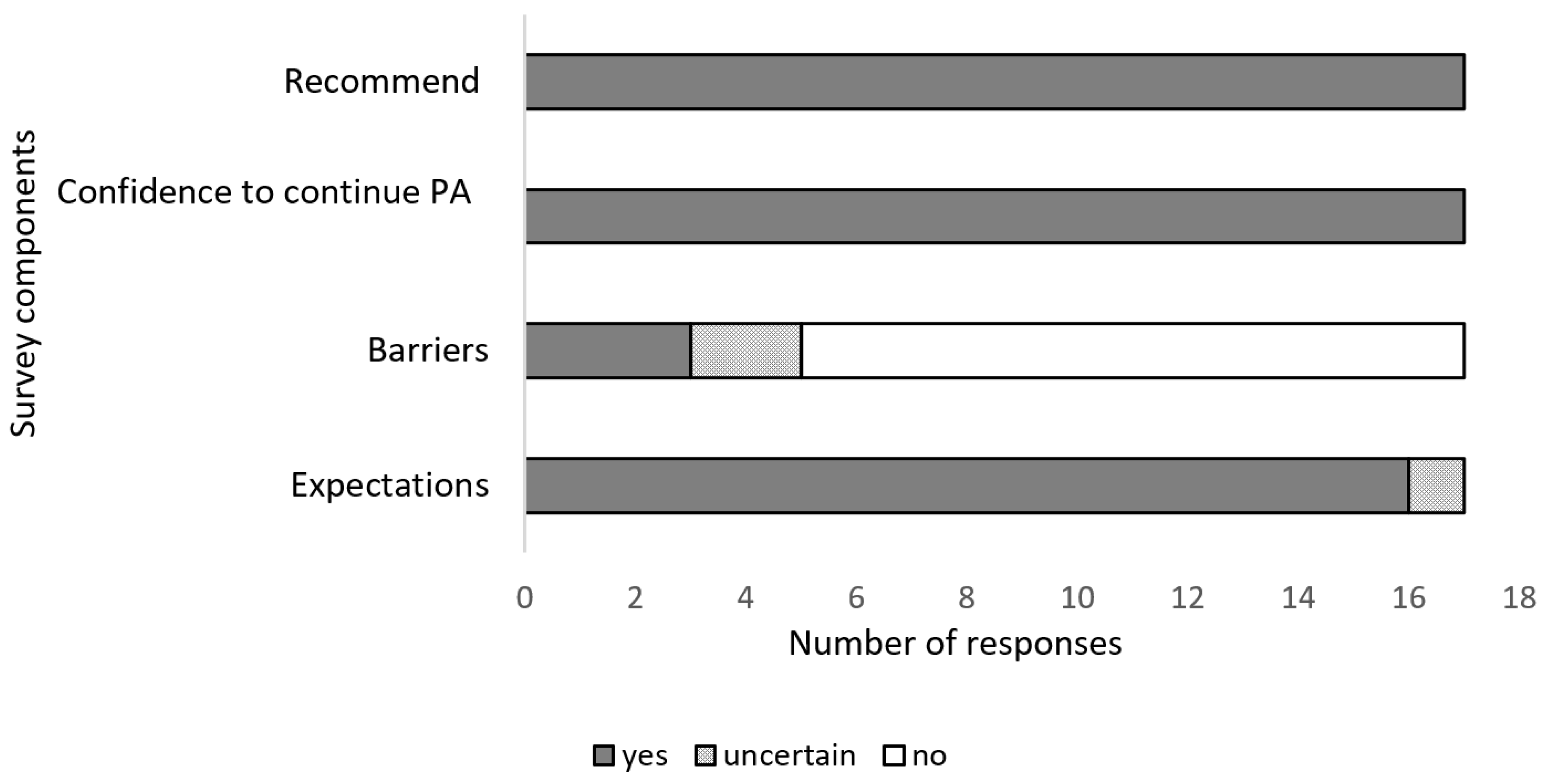
3.1.4. Maintenance
4. Discussion
4.1. Reach
4.2. Adoption
4.3. Implementation
4.4. Maintenance
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Min, A.; Hong, H.C.; Kim, Y.M. Work schedule characteristics and occupational fatigue/recovery among rotating-shift nurses: A cross-sectional study. J. Nurs. Manag. 2022, 30, 463–472. [Google Scholar] [CrossRef] [PubMed]
- Costa, G. Introduction to Problems of Shift Work. In Social and Family Issues in Shift Work and Non Standard Working Hours; Iskra-Golec, I., Barnes-Farrell, J., Bohle, P., Eds.; Springer: Cham, Switzerland, 2016; pp. 19–35. [Google Scholar]
- Williams, C.C.; Schneider, F. Measuring the Global Shadow Economy: The Prevalence of Informal Work and Labour; Edward Elgar Publishing: Cheltenham, UK, 2016. [Google Scholar]
- Brown, J.P.; Martin, D.; Nagaria, Z.; Verceles, A.C.; Jobe, S.L.; Wickwire, E.M. Mental Health Consequences of Shift Work: An Updated Review. Curr. Psychiatry Rep. 2020, 22, 7. [Google Scholar] [CrossRef] [PubMed]
- Sooriyaarachchi, P.; Jayawardena, R.; Pavey, T.; King, N.A. Shift work and the risk for metabolic syndrome among healthcare workers: A systematic review and meta-analysis. Obes. Rev. 2022, 23, e13489. [Google Scholar] [CrossRef]
- Su, F.; Huang, D.; Wang, H.; Yang, Z. Associations of shift work and night work with risk of all-cause, cardiovascular and cancer mortality: A meta-analysis of cohort studies. Sleep Med. 2021, 86, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Kassa, M.; Grace, J. The global burden and perspectives on non-communicable diseases (NCDs) and the prevention, data availability and systems approach of NCDs in low-resource countries. In Public Health in Developing Countries-Challenges and Opportunities; IntechOpen: London, UK, 2019. [Google Scholar]
- Saqib, Z.A.; Dai, J.; Menhas, R.; Mahmood, S.; Karim, M.; Sang, X.; Weng, Y. Physical Activity is a Medicine for Non-Communicable Diseases: A Survey Study Regarding the Perception of Physical Activity Impact on Health Wellbeing. Risk Manag. Healthc. Policy 2020, 13, 2949–2962. [Google Scholar] [CrossRef] [PubMed]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Monnaatsie, M.; Biddle, S.J.; Khan, S.; Kolbe-Alexander, T. Physical activity and sedentary behaviour in shift and non-shift workers: A systematic review and meta-analysis. Prev. Med. Rep. 2021, 24, 101597. [Google Scholar] [CrossRef]
- Ramezani, M.; Tayefi, B.; Zandian, E.; SoleimanvandiAzar, N.; Khalili, N.; Hoveidamanesh, S.; Massahikhaleghi, P.; Rampisheh, Z. Workplace interventions for increasing physical activity in employees: A systematic review. J. Occup. Health 2022, 64, e12358. [Google Scholar] [CrossRef]
- Malik, S.H.; Blake, H.; Suggs, L.S. A systematic review of workplace health promotion interventions for increasing physical activity. Br. J. Health Psychol. 2014, 19, 149–180. [Google Scholar] [CrossRef]
- Tunwattanapong, P.; Kongkasuwan, R.; Kuptniratsaikul, V. The effectiveness of a neck and shoulder stretching exercise program among office workers with neck pain: A randomized controlled trial. Clin. Rehabil. 2016, 30, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Freak-Poli, R.; Cumpston, M.; Albarqouni, L.; Clemes, S.A.; Peeters, A. Workplace pedometer interventions for increasing physical activity. Cochrane Database Syst. Rev. 2020, 7, Cd009209. [Google Scholar] [CrossRef] [PubMed]
- Gutermuth, L.K.; Hager, E.R.; Pollack Porter, K. Using the CDC’s Worksite Health ScoreCard as a Framework to Examine Worksite Health Promotion and Physical Activity. Prev. Chronic Dis. 2018, 15, E84. [Google Scholar] [CrossRef] [PubMed]
- To, Q.G.; Chen, T.T.; Magnussen, C.G.; To, K.G. Workplace physical activity interventions: A systematic review. Am. J. Health Promot. 2013, 27, e113–e123. [Google Scholar] [CrossRef] [PubMed]
- Kaveh, M.H.; Layeghiasl, M.; Nazari, M.; Ghahremani, L.; Karimi, M. What Are the Determinants of a Workplace Health Promotion? Application of a Social Marketing Model in Identifying Determinants of Physical Activity in the Workplace (a Qualitative Study). Front. Public Health 2020, 8, 614631. [Google Scholar] [CrossRef]
- Jain, R.; Verma, V.; Rana, K.B.; Meena, M.L. Effect of physical activity intervention on the musculoskeletal health of university student computer users during homestay. Int. J. Occup. Saf. Ergon. 2023, 29, 25–30. [Google Scholar] [CrossRef]
- Kelly, C.; Nea, F.M.; Pourshahidi, L.K.; Kearney, J.M.; O’Brien, V.; Livingstone, M.B.E.; Corish, C.A. Adherence to dietary and physical activity guidelines among shift workers: Associations with individual and work-related factors. BMJ Nutr. Prev. Health 2020, 3, 229–238. [Google Scholar] [CrossRef]
- Beringer, C.; Wells, M.; Goldstein, L. Let’s get physical: A prospective pedometer study of doctors working in a South African emergency department. SAMJ S. Afr. Med. J. 2020, 110, 1124–1127. [Google Scholar] [CrossRef]
- Krüger, K.; Petermann, C.; Pilat, C.; Schubert, E.; Pons-Kühnemann, J.; Mooren, F.C. Preventive strength training improves working ergonomics during welding. Int. J. Occup. Saf. Ergon. 2015, 21, 150–157. [Google Scholar] [CrossRef]
- Neil-Sztramko, S.E.; Gotay, C.C.; Sabiston, C.M.; Demers, P.A.; Campbell, K.C. Feasibility of a telephone and web-based physical activity intervention for women shift workers. Transl. Behav. Med. 2017, 7, 268–276. [Google Scholar] [CrossRef] [Green Version]
- Thøgersen-Ntoumani, C.; Quested, E.; Biddle, S.J.H.; Kritz, M.; Olson, J.; Burton, E.; Cerin, E.; Hill, K.D.; McVeigh, J.; Ntoumanis, N. Trial feasibility and process evaluation of a motivationally-embellished group peer led walking intervention in retirement villages using the RE-AIM framework: The residents in action trial (RiAT). Health Psychol. Behav. Med. 2019, 7, 202–233. [Google Scholar] [CrossRef]
- Guest, A.J.; Paine, N.J.; Chen, Y.L.; Chalkley, A.; Munir, F.; Edwardson, C.L.; Gray, L.J.; Johnson, V.; Ruettger, K.; Sayyah, M.; et al. The structured health intervention for truckers (SHIFT) cluster randomised controlled trial: A mixed methods process evaluation. Int. J. Behav. Nutr. Phys. Act. 2022, 19, 79. [Google Scholar] [CrossRef] [PubMed]
- Varela-Mato, V.; Caddick, N.; King, J.A.; Yates, T.; Stensel, D.J.; Nimmo, M.A.; Clemes, S.A. A Structured Health Intervention for Truckers (SHIFT): A Process Evaluation of a Pilot Health Intervention in a Transport Company. J. Occup. Environ. Med. 2018, 60, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Punnett, L.; Nobrega, S.; Zhang, Y.; Rice, S.; Gore, R.; Kurowski, A. Safety and Health through Integrated, Facilitated Teams (SHIFT): Stepped-wedge protocol for prospective, mixed-methods evaluation of the Healthy Workplace Participatory Program. BMC Public Health 2020, 20, 1463. [Google Scholar] [CrossRef]
- Antikainen, I.; Ellis, R. A RE-AIM evaluation of theory-based physical activity interventions. J. Sport Exerc. Psychol. 2011, 33, 198–214. [Google Scholar] [CrossRef]
- Caperchione, C.M.; Duncan, M.; Kolt, G.S.; Vandelanotte, C.; Rosenkranz, R.R.; Maeder, A.; Noakes, M.; Karunanithi, M.; Mummery, W.K. Examining an Australian physical activity and nutrition intervention using RE-AIM. Health Promot. Int. 2015, 31, 450–458. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E.; Harden, S.M.; Gaglio, B.; Rabin, B.; Smith, M.L.; Porter, G.C.; Ory, M.G.; Estabrooks, P.A. RE-AIM planning and evaluation framework: Adapting to new science and practice with a 20-year review. Front. Public Health 2019, 7, 64. [Google Scholar] [CrossRef]
- Kwan, B.M.; McGinnes, H.L.; Ory, M.G.; Estabrooks, P.A.; Waxmonsky, J.A.; Glasgow, R.E. RE-AIM in the Real World: Use of the RE-AIM Framework for Program Planning and Evaluation in Clinical and Community Settings. Front. Public Health 2019, 7, 345. [Google Scholar] [CrossRef]
- Brinkley, A.; McDermott, H.; Munir, F. Team Sport in the Workplace? A RE-AIM Process Evaluation of ‘Changing the Game’. AIMS Public Health 2017, 4, 466–489. [Google Scholar] [CrossRef]
- Robinson, K.; Allen, F.; Darby, J.; Fox, C.; Gordon, A.L.; Horne, J.C.; Leighton, P.; Sims, E.; Logan, P.A. Contamination in complex healthcare trials: The falls in care homes (FinCH) study experience. BMC Med. Res. Methodol. 2020, 20, 46. [Google Scholar] [CrossRef] [Green Version]
- Concheiro-Moscoso, P.; Martínez-Martínez, F.J.; Miranda-Duro, M.D.C.; Pousada, T.; Nieto-Riveiro, L.; Groba, B.; Mejuto-Muiño, F.J.; Pereira, J. Study Protocol on the Validation of the Quality of Sleep Data from Xiaomi Domestic Wristbands. Int. J. Environ. Res. Public Health 2021, 18, 1106. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E.; Emont, S.; Miller, D.C. Assessing delivery of the five ‘As’ for patient-centered counseling. Health Promot. Int. 2006, 21, 245–255. [Google Scholar] [CrossRef]
- Schroé, H.; Van Dyck, D.; De Paepe, A.; Poppe, L.; Loh, W.W.; Verloigne, M.; Loeys, T.; De Bourdeaudhuij, I.; Crombez, G. Which behaviour change techniques are effective to promote physical activity and reduce sedentary behaviour in adults: A factorial randomized trial of an e- and m-health intervention. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 127. [Google Scholar] [CrossRef]
- Michie, S.; Van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef]
- Burke, L.E.; Shiffman, S.; Music, E.; Styn, M.A.; Kriska, A.; Smailagic, A.; Siewiorek, D.; Ewing, L.J.; Chasens, E.; French, B.; et al. Ecological Momentary Assessment in Behavioral Research: Addressing Technological and Human Participant Challenges. J. Med. Internet Res. 2017, 19, e77. [Google Scholar] [CrossRef] [PubMed]
- Kolbe-Alexander, T.L.; Gomersall, S.; Clark, B.; Torquati, L.; Pavey, T.; Brown, W.J. A hard day’s night: Time use in shift workers. BMC Public Health 2019, 19, 452. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Maslin, T.S.; Armstrong, T. Global physical activity questionnaire (GPAQ): Nine country reliability and validity study. J. Phys. Act. Health 2009, 6, 790–804. [Google Scholar] [CrossRef] [PubMed]
- Forman, J.; Heisler, M.; Damschroder, L.J.; Kaselitz, E.; Kerr, E.A. Development and application of the RE-AIM QuEST mixed methods framework for program evaluation. Prev. Med. Rep. 2017, 6, 322–328. [Google Scholar] [CrossRef]
- Dall, P.M.; Ellis, S.L.H.; Ellis, B.M.; Grant, P.M.; Colyer, A.; Gee, N.R.; Granat, M.H.; Mills, D.S. The influence of dog ownership on objective measures of free-living physical activity and sedentary behaviour in community-dwelling older adults: A longitudinal case-controlled study. BMC Public Health 2017, 17, 496. [Google Scholar] [CrossRef]
- Carr, L.J.; Bartee, R.T.; Dorozynski, C.; Broomfield, J.F.; Smith, M.L.; Smith, D.T. Internet-delivered behavior change program increases physical activity and improves cardiometabolic disease risk factors in sedentary adults: Results of a randomized controlled trial. Prev. Med. 2008, 46, 431–438. [Google Scholar] [CrossRef]
- De Muth, J.E. Overview of biostatistics used in clinical research. Am. J. Health Syst. Pharm. 2009, 66, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Ritchie, J.; Lewis, J.; Nicholls, C.M.; Ormston, R. Qualitative Research Practice: A Guide for Social Science Students and Researchers; Sage: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Blake, H.; Lai, B.; Coman, E.; Houdmont, J.; Griffiths, A. Move-It: A Cluster-Randomised Digital Worksite Exercise Intervention in China: Outcome and Process Evaluation. Int. J. Environ. Res. Public Health 2019, 16, 3451. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, B.; Gibson, A.M.; Janssen, X.; Hutchinson, J.; Headley, S.; Matthews, T.; Kirk, A. Should We Scale-Up? A Mixed Methods Process Evaluation of an Intervention Targeting Sedentary Office Workers Using the RE-AIM QuEST Framework. Int. J. Environ. Res. Public Health 2019, 17, 239. [Google Scholar] [CrossRef] [PubMed]
- Ryde, G.C.; Gilson, N.D.; Burton, N.W.; Brown, W.J. Recruitment Rates in Workplace Physical Activity Interventions: Characteristics for Success. Am. J. Health Promot. 2013, 27, e101–e112. [Google Scholar] [CrossRef] [PubMed]
- Buchholz, S.W.; Wilbur, J.; Ingram, D.; Fogg, L. Physical activity text messaging interventions in adults: A systematic review. Worldviews Evid. Based Nurs. 2013, 10, 163–173. [Google Scholar] [CrossRef]
- Patterson, K.; Davey, R.; Keegan, R.; Freene, N. Smartphone applications for physical activity and sedentary behaviour change in people with cardiovascular disease: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0258460. [Google Scholar] [CrossRef]
- Rathbone, A.L.; Prescott, J. The Use of Mobile Apps and SMS Messaging as Physical and Mental Health Interventions: Systematic Review. J. Med. Internet Res. 2017, 19, e295. [Google Scholar] [CrossRef]
- Schunk, D.H.; Usher, E.L. Social cognitive theory and motivation. Oxf. Handb. Hum. Motiv. 2012, 2, 11–26. [Google Scholar]
- De Cocker, K.; De Bourdeaudhuij, I.; Cardon, G.; Vandelanotte, C. What are the working mechanisms of a web-based workplace sitting intervention targeting psychosocial factors and action planning? BMC Public Health 2017, 17, 382. [Google Scholar] [CrossRef]
- Sanaeinasab, H.; Saffari, M.; Valipour, F.; Alipour, H.R.; Sepandi, M.; Al Zaben, F.; Koenig, H.G. The effectiveness of a model-based health education intervention to improve ergonomic posture in office computer workers: A randomized controlled trial. Int. Arch. Occup. Environ. Health 2018, 91, 951–962. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Huang, W.Y.; Yu, J.J.; Sheridan, S.; Sit, C.H.-P.; Wong, S.H.-S. Compliance and Practical Utility of Continuous Wearing of activPAL™ in Adolescents. Pediatr. Exerc. Sci. 2019, 31, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Schrack, J.A.; Cooper, R.; Koster, A.; Shiroma, E.J.; Murabito, J.M.; Rejeski, W.J.; Ferrucci, L.; Harris, T.B. Assessing Daily Physical Activity in Older Adults: Unraveling the Complexity of Monitors, Measures, and Methods. J. Gerontol. Ser. A 2016, 71, 1039–1048. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Farias, N.; Martino-Fuentealba, P.; Salom-Diaz, N.; Brown, W.J. How many days are enough for measuring weekly activity behaviours with the ActivPAL in adults? J. Sci. Med. Sport 2019, 22, 684–688. [Google Scholar] [CrossRef]
- Beres, L.K.; Mbabali, I.; Anok, A.; Katabalwa, C.; Mulamba, J.; Thomas, A.G.; Bugos, E.; Grabowski, M.K.; Nakigozi, G.; Chang, L. Acceptability and feasibility of mobile phone-based ecological momentary assessment and intervention in Uganda: A pilot randomized controlled trial. PLoS ONE 2022, 17, e0273228. [Google Scholar] [CrossRef]
- Ponnada, A.; Thapa-Chhetry, B.; Manjourides, J.; Intille, S. Measuring criterion validity of microinteraction ecological momentary assessment (micro-ema): Exploratory pilot study with physical activity measurement. JMIR mHealth uHealth 2021, 9, e23391. [Google Scholar] [CrossRef]
- Walthouwer, M.J.; Oenema, A.; Lechner, L.; de Vries, H. Comparing a Video and Text Version of a Web-Based Computer-Tailored Intervention for Obesity Prevention: A Randomized Controlled Trial. J. Med. Internet Res. 2015, 17, e236. [Google Scholar] [CrossRef]
- Lewis, M.; Bromley, K.; Sutton, C.J.; McCray, G.; Myers, H.L.; Lancaster, G.A. Determining sample size for progression criteria for pragmatic pilot RCTs: The hypothesis test strikes back! Pilot Feasibility Stud. 2021, 7, 40. [Google Scholar] [CrossRef]
| Dimension | Indicator | Data Source |
|---|---|---|
| Reach | Participation rate | Researcher logbook |
| Dropout rate | Recorded number of enrolled and completed assessment workers | |
| Individual reasons for non-participation | Researcher logbook and online questionnaires and interviews | |
| Barriers and facilitators for participation | Online questionnaires and interviews | |
| Adoption | Representativeness of work departments and drop-out | Researcher logbook |
| Factors that affect individual participation and engagement with intervention components | Online questionnaires and interviews | |
| Method used to target various departments | Researcher logbook | |
| Implementation | Barriers and facilitators of intervention process | Online questionnaires and interviews |
| Expectations of intervention components | Researcher logbook and online questionnaires | |
| Maintenance | Individual reporting on the continuation of intervention beyond the intervention period | Online questionnaires and interviews |
| Barriers to maintaining the program | Online questionnaires and interviews |
| Characteristics | Total (n = 51) | Intervention Group (n = 25) | Control Group (n = 26) | p-Value |
|---|---|---|---|---|
| Age years (mean, SD) | 39.3 (5.4) | 39.1 (5.8) | 39.4 (5.2) | 0.89 |
| BMI kg/m2 (mean, SD) | 26.2 (5.8) | 26.0 (7.2) | 26.4 (4.2) | 0.42 |
| Gender (n, %) | 0.39 | |||
| Male | 27.0 (53.0) | 12.0 (44) | 15.0 (55.5) | |
| Female | 24.0 (47.0) | 13.0 (54.2) | 11.0 (45.8) | |
| Marital status (n, %) | 0.06 | |||
| Living with partner | 20.0 (41.0) | 12.0 (27.1) | 8 (17.0) | |
| Health status (n, %) | 0.07 | |||
| Poor | 15.0 (30.6) | 10 (20.8) | 5 (10.4) | |
| Average | 20.0 (40.8) | 10 (20.8) | 10 (20.8) | |
| Excellent | 2.0 (4.1) | 0 (0) | 2 (4.2) | |
| Number of participants reporting LTPA (n, %) | 30.0 (56) | 16.0 (29) | 14.0 (27) | 0.77 |
| Department | Total Number of Employees Who Signed Up for the Intervention | Total Dropout Rate |
|---|---|---|
| Hospital mine | 30 | 6 |
| Mining processing | 18 | 2 |
| Mining pit | 12 | 1 |
| RE-AIM Components | Theme | Facilitator /Barrier | Quotes |
|---|---|---|---|
| Reach | Incentive promised | Facilitator | Female hospital nurse: “Well, I saw one on the colleagues wearing the fitness band, honestly, I got excited and felt you know, I really need to get this myself. Remember I even approached you and asked you to give me one before I can even join program”. |
| Aware of the benefits | Facilitator | Male pit mine worker: “Once I heard the program was about wellness, I joined because I am some who likes being active. But I haven’t exerciced since COVID. I thought this is the chance to improve my physical activity”. | |
| No work management involvement | Barrier | Male mine processing worker: “I think because you are a researcher from outside. People in the mine are usually keen if the employer was more involved. Maybe in future the mine management should be involved so more people will participate than just you alone”. | |
| ActivPAL wear skin irritations | Barrier | Female hospital nurse: “I wish there could be something else to use than the stickers because some skin are very sensitive causing some irritation”. | |
| Implementation | Text messages useful | Facilitator | Male mine pit worker: “The text messages were helpful. They were a reminder especially on a lazy day and I receive a text. Then I will get up and something. They assisted me to be active”. |
| Program beneficial | Facilitator | Male hospital nurse: “This program is very reliable to shift workers because they can do their physical activity in a planned manner and time”. | |
| Work factors | Barrier | Female hospital nurse: “I wanted to do more, but because of work, I get home really tired”. | |
| Maintenance | Continuation in use of information from program | Facilitator | Male mine processing worker: “The program has helped with the monitoring, so it motivated me to be active. These days I hardly skip gym. Had a slow week last week, but back to gym this week”. |
| Continuation use of the Mi fitness band | Facilitator | Male mine pit worker: “I set myself a standard that it should be 10,000 steps a day so if I haven’t done those 10,000 steps so I stand up and start doing some exercises. Even if it’s not walking now. I have a machine step that I use.” | |
| Recommendation to use the program for the company | Facilitator | Female hospital nurse: “It was a very beneficial program for me personally and for the company. I have been regularly engaging in physical activity ever since participating in the study. I also hope the results will reach relevant authorities.” |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Monnaatsie, M.; Biddle, S.J.H.; Kolbe-Alexander, T. The Feasibility of a Text-Messaging Intervention Promoting Physical Activity in Shift Workers: A Process Evaluation. Int. J. Environ. Res. Public Health 2023, 20, 3260. https://doi.org/10.3390/ijerph20043260
Monnaatsie M, Biddle SJH, Kolbe-Alexander T. The Feasibility of a Text-Messaging Intervention Promoting Physical Activity in Shift Workers: A Process Evaluation. International Journal of Environmental Research and Public Health. 2023; 20(4):3260. https://doi.org/10.3390/ijerph20043260
Chicago/Turabian StyleMonnaatsie, Malebogo, Stuart J. H. Biddle, and Tracy Kolbe-Alexander. 2023. "The Feasibility of a Text-Messaging Intervention Promoting Physical Activity in Shift Workers: A Process Evaluation" International Journal of Environmental Research and Public Health 20, no. 4: 3260. https://doi.org/10.3390/ijerph20043260
APA StyleMonnaatsie, M., Biddle, S. J. H., & Kolbe-Alexander, T. (2023). The Feasibility of a Text-Messaging Intervention Promoting Physical Activity in Shift Workers: A Process Evaluation. International Journal of Environmental Research and Public Health, 20(4), 3260. https://doi.org/10.3390/ijerph20043260







