Assessment of Oral Health in Long-Term Enteral and Parenteral Nutrition Patients: Significant Aspects of Nursing Care
Abstract
:1. Introduction
2. Oral Health Status in Patients Receiving Long-Term Nutritional Treatment
3. Oral Microflora
4. The Importance of Chewing
5. The Role and Functions of Saliva
6. Xerostomia and Methods of Evaluation
7. Role of Nursing in Oral Health Assessment and Patient Education
8. Conclusions
9. Recommendation for Practice
- Comprehensive care for enterally and parenterally fed patients must take into account oral care, especially when disease is active.
- Patients in the hospital and in primary care should be supported by nursing and caring staff trained to accurately recognize symptoms of poor oral health and implement appropriate measures.
- An oral health care assessment should be a standard examination in long-term nutritional therapy.
- The implementation of professional training for nurses in the field of oral cavity assessment and care would improve the activities promoting oral health among adult patients treated with enteral and parenteral nutrition and other groups of chronically ill patients.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mędrzycka-Dąbrowska, W.; Dąbrowski, S.; Basiński, A. Aktualne zalecenia w pielęgnacji jamy ustnej u pacjentów zaintubowanych i wentylowanych mechanicznie-przegląd piśmiennictwa. Anestezjol. I Ratow. 2012, 2, 221. Available online: http://www.anestezjologiairatownictwo.pl/ (accessed on 10 August 2022).
- Qi, X.; Northridge, M.E.; Hu, M.; Wu, B. Oral health conditions and COVID-19: A systematic review and meta-analysis of the current evidence. Aging Health Res. 2022, 2, 100064. [Google Scholar] [CrossRef] [PubMed]
- Kozeniecki, M.; Fritzshall, R. Enteral nutrition for adults in the hospital setting. Nutr. Clin. Pract. 2015, 30, 634–651. [Google Scholar] [CrossRef] [PubMed]
- Lappas, B.; Patel, D.; Kumpf, V.; Adams, D.; Seidner, D. Parenteral nutrition: Indications, access, and complications. Gastroenterol. Clin. N. Am. 2018, 47, 39–59. [Google Scholar] [CrossRef] [PubMed]
- Hadefi, A.; Arvanitakis, M. How to approach long-term enteral and parenteral nutrition. Gastroenterology 2021, 161, 1780–1786. [Google Scholar] [CrossRef]
- Lopes, S.; Tavares, V.; Mascarenhas, P.; Lopes, M.; Cardote, C.; Godinho, C.; Oliveira, C.; Santos, C.; Oom, M.; Grillo-Evangelista, J.; et al. Oral health status of adult dysphagic patients that undergo endoscopic gastrostomy for long term enteral feeding. Int. J. Environ. Res. Public Health 2022, 19, 4827. [Google Scholar] [CrossRef]
- Pedersen, A.; Belstrøm, D. The role of natural salivary defences in maintaining a healthy oral microbiota. J. Dent. 2019, 80, S3–S12. [Google Scholar] [CrossRef]
- Seo, K.; Kim, H. Effects of oral health programmes on xerostomia in community-dwelling elderly: A systematic review and meta-analysis. Int. J. Dent. Hyg. 2020, 18, 52–61. [Google Scholar] [CrossRef]
- Pironi, L.; Boeykens, K.; Bozzetti, F.; Joly, F.; Klek, S.; Lal, S.; Lichota, M.; Mühlebach, S.; Van Gossu, A.; Wanten, G.; et al. ESPEN guideline on home parenteral nutrition. Clin. Nutr. 2020, 39, 1645–1666. [Google Scholar] [CrossRef]
- Bischoff, S.; Austin, P.; Boeykens, K.; Chourdakis, M.; Cuerda, C.; Jonkers-Schuitema, C.; Lichota, M.; Nyulasi, I.; Schneider, S.; Stanga, Z.; et al. ESPEN guideline on home enteral nutrition. Clin. Nutr. 2020, 39, 5–22. [Google Scholar] [CrossRef] [Green Version]
- Preiser, J.; Arabi, Y.; Berger, M.; Casaer, M.; McClave, S.; Montejo-Gonzalez, J.C.; Peake, S.; Blaser, A.; Van den Berghe, G.; van Zanten, A.; et al. A guide to enteral nutrition in intensive care units: 10 expert tips for the daily practice. Crit. Care 2021, 25, 424. [Google Scholar] [CrossRef] [PubMed]
- Kisely, S. No mental health without oral health. Can. J. Psychiatry 2016, 61, 277–282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drancourt, N.; El Osta, N.; Decerle, N.; Hennequin, M. Relationship between Oral Health Status and Oropharyngeal Dysphagia in Older People: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 13618. [Google Scholar] [CrossRef] [PubMed]
- Maeda, K.; Akagi, J. Oral care may reduce pneumonia in the tube-fed elderly: A preliminary study. Dysphagia 2014, 29, 616–621. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Gabe, S.; Nightingale, J.; Burke, M. Intestinal failure and home parenteral nutrition: Implications for oral health and dental care. Clin. Nutr. 2012, 32, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Gabe, S.; Nightingale, J.; Burke, M. Oral health, dental prophylaxis and catheter related bloodstream infections in home parenteral nutrition patients: Results of a UK survey and cohort study. Br. Dent. J. 2012, 212, E4. [Google Scholar] [CrossRef]
- Folwarski, M.; Kłęk, S.; Szlagatys-Sidorkiewicz, A.; Wyszomirski, A.; Brzeziński, M.; Skotnicka, M. Trend observations in home parenteral nutrition. Prevalence, hospitalizations and costs: Results from a Nationwide Analysis of Health Care Provider Data. Nutrients 2021, 13, 3465. [Google Scholar] [CrossRef] [PubMed]
- Leung, K.-M.; Chu, C.-H. Dental care for older adults. Int. J. Environ. Res. Public Health 2023, 20, 214. [Google Scholar] [CrossRef]
- Graves, D.; Corrêa, J.; Silva, T. The oral microbiota is modified by systemic diseases. J. Dent. Res. 2019, 98, 148–156. [Google Scholar] [CrossRef]
- Suzuki, H.; Furuya, J.; Nakagawa, K.; Hidaka, R.; Nakane, A.; Yoshimi, K.; Shimizu, Y.; Saito, K.; Itsui, Y.; Tohara, H.; et al. Changes in nutrition-intake method and oral health through a multidisciplinary team approach in malnourished older patients admitted to an acute care hospital. Int. J. Environ. Res. Public Health 2022, 19, 9784. [Google Scholar] [CrossRef]
- Katagiri, S.; Shiba, T.; Tohara, H.; Yamaguchi, K.; Hara, K.; Nakagawa, K.; Komatsu, K.; Watanabe, K.; Ohsugi, Y.; Maekawa, S.; et al. Re-initiation of oral food intake following enteral nutrition alters oral and gut microbiota communities. Front. Cell. Infect. Microbiol. 2019, 9, 434. [Google Scholar] [CrossRef] [PubMed]
- Peng, X.; Cheng, L.; You, Y.; Tang, C.; Ren, B.; Li, Y.; Xu, X.; Zhou, X. Oral microbiota in human systematic diseases. Int. J. Oral. Sci. 2022, 14, 14. [Google Scholar] [CrossRef] [PubMed]
- Hollis, J. The effect of mastication on food intake, satiety and body weight. Physiol. Behav. 2018, 193 (Pt B), 242–245. [Google Scholar] [CrossRef]
- Olczak-Kowalczyk, D.; Danko, M.; Banaś, E.; Gozdowski, D.; Popińska, K.; Krasuska-Sławińska, E.; Książyk, J. Parenteral nutrition in childhood and consequences for dentition and gingivae. Eur. J. Paediatr. Dent. 2017, 18, 69–76. [Google Scholar] [CrossRef]
- Pedersen, A.; Sørensen, C.; Proctor, G.; Carpenter, G. Salivary functions in mastication, taste and textural perception, swallowing and initial digestion. Oral. Dis. 2018, 24, 1399–1416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chuhuaicura, P.; Dias, F.; Arias, A.; Lezcano, M.; Fuentes, R. Mastication as a protective factor of the cognitive decline in adults: A qualitative systematic review. Int. Dent. J. 2019, 69, 334–340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, B.; Kashyap, N.; Avinash, A.; Chevvuri, R.; Sagar, M.; Shrikant, K. The composition, function and role of saliva in maintainingoral health: A review. Int. J. Contemp. Dent. Med. Rev. 2017, 2017, 1–6. [Google Scholar]
- Tanasiewicz, M.; Hildebrandt, T.; Obersztyn, I. Xerostomia of various etiologies: A review of the literaturę. Adv. Clin. Exp. Med. 2016, 25, 199–206. [Google Scholar] [CrossRef] [Green Version]
- Villa, A.; Connell, C.; Abati, S. Diagnosis and management of xerostomia and hyposalivation. Ther. Clin. Risk Manag. 2014, 11, 45–51. [Google Scholar] [CrossRef] [Green Version]
- Anil, S.; Vellappally, S.; Hashem, M.; Preethanath, R.S.; Patil, S.; Samaranayake, L. Xerostomia in geriatric patients: A burgeoning global concern. J. Investig. Clin. Dent. 2016, 7, 5–12. [Google Scholar] [CrossRef]
- Bressan, V.; Stevanin, S.; Bianchi, M.; Aleo, G.; Bagnasco, A.; Sasso, L. The effects of swallowing disorders, dysgeusia, oral mucositis and xerostomia on nutritional status, oral intake and weight loss in head and neck cancer patients: A systematic review. Cancer Treat. Rev. 2016, 45, 105–119. [Google Scholar] [CrossRef] [PubMed]
- Khalid, A.; Elahi, S.; Qurban, A.; Atif, S. Xerostomia diagnosis—A narrative review. J. Pak. Dent. Assoc. 2022, 31, 49–54. [Google Scholar] [CrossRef]
- Chengappa, R.; Narayanan, V.; Khan, A.; Rakaraddi, M.; Puttaswamy, K.; Puttabuddi, J. Utility of two methodologies in the clinical assessment of oral dryness in postmenopausal women. J. Midlife Health 2016, 7, 114–118. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Oral Health. Available online: https://www.who.int/news-room/fact-sheets/detail/oral-health (accessed on 3 December 2022).
- Ministerstwo Zdrowia. Programy polityki zdrowotnej. Monitorowanie stanu zdrowia jamy ustnej populacji polskiej na lata. 2016. Available online: https://www.gov.pl/web/zdrowie/monitorowanie-stanu-zdrowia-jamy-ustnej-populacji-polskiej-w-latach-2016-2020 (accessed on 14 August 2022).
- Gibney, J.M.; Wright, F.A.; D’Souza, M.; Naganathan, V. Improving the oral health of older people in hospital. Australas. J. Ageing 2019, 38, 33–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhagat, V.; Hoang, H.; Crocombe, L.A.; Goldberg, L.R. Incorporating oral health care education in undergraduate nursing curricula - a systematic review. BMC Nurs. 2020, 19, 66. [Google Scholar] [CrossRef] [PubMed]
- Haresaku, S.; Uchida, S.; Aoki, H.; Akinaga, K.; Yoshida, R.; Kubota, K.; Naito, T. Factors associated with nurses’ performance of oral assessments and dental referrals for hospital inpatients. BMC Oral. Health 2020, 20, 68. [Google Scholar] [CrossRef]
- Kohli, R.; Arora, G.; Blanc, A.; Pham, E.; Gubrud-Howe, P. Oral health clinical training and dental referral program for nurses: An interprofessional collaborative project. Geriatr. Nurs. 2021, 42, 880–886. [Google Scholar] [CrossRef]
| Habitat | Genera/Predominant Bacterium |
|---|---|
| Lips | Candida albicans (corners of the mouth) |
| Micrococcus spp. | |
| Corynebacterium spp. | |
| Neisseria spp. | |
| Staphylococcus spp. | |
| Tongue | Streptococcus salivarius |
| Peptostreptococcus spp. | |
| Veillonella spp. | |
| Actinomyces viscosus | |
| Capnocythophaga spp. | |
| Lactobacillus spp. | |
| Treponema spp. | |
| Fusobacterium spp. | |
| Buccal mucosa (cheek) | Actinomyces viscosus |
| Streptococcus mittis | |
| Capnocytophaga spp. | |
| Fusobacterium spp. | |
| Prevotella intermedia | |
| Palate | Actinomyces spp. |
| Lactobacillus spp. | |
| Streptococcus spp. | |
| Veillonella spp. | |
| Candida spp. | |
| Bacteroides spp. |
| Type of Symptom | Symptom |
|---|---|
| Subjective |
|
| Objective |
|
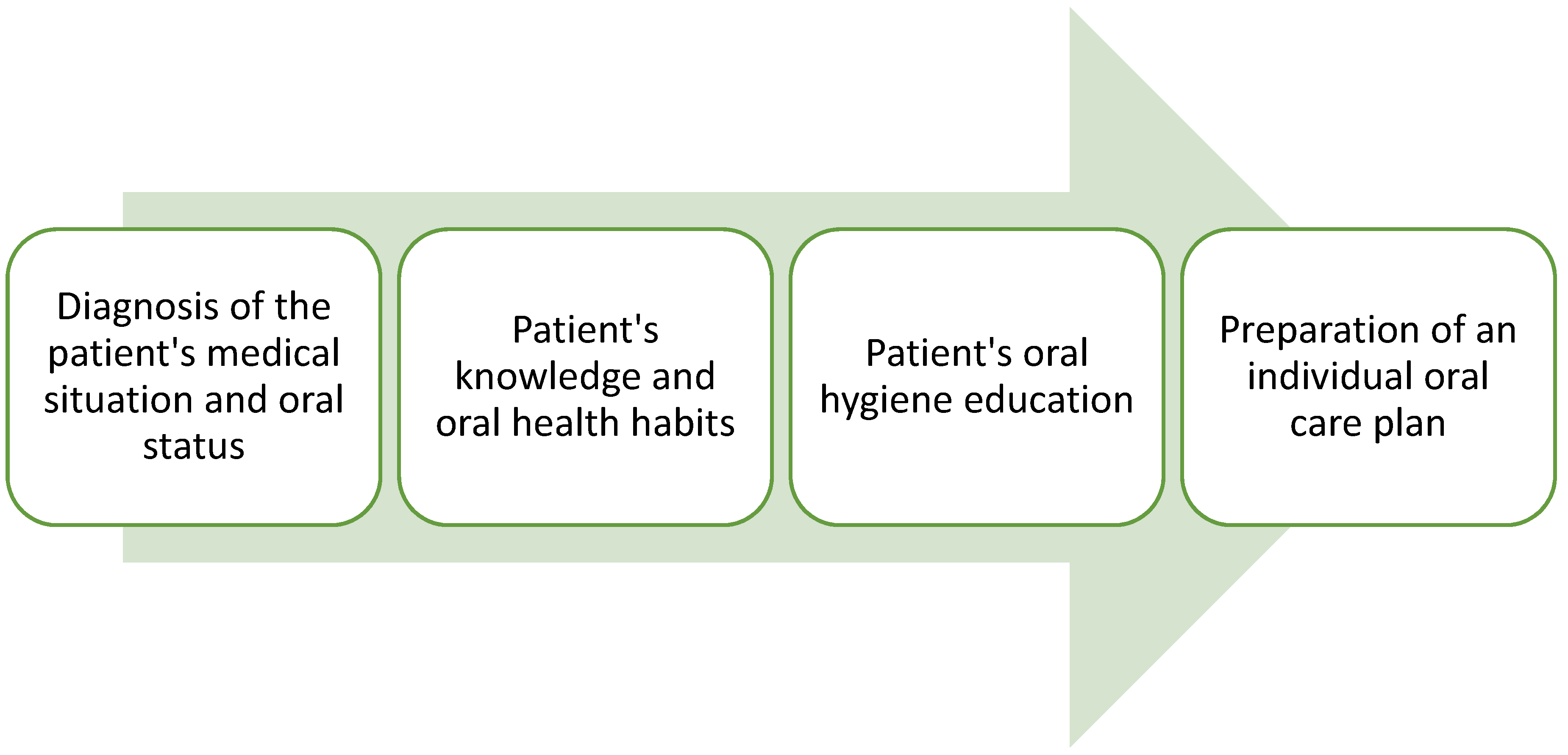
| Assessment Categories | Objectives |
|---|---|
| Medical interview |
|
| Oral health examination |
|
| Assessment of knowledge and oral care habits |
|
| Changing or correct oral health behavior | The teaching of oral health includes:
|
| Individual oral care plan | Assessment oral hygiene depends on:
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Terech-Skóra, S.; Kasprzyk-Mazur, J.; Leyk-Kolańczak, M.; Kruk, A.; Piotrkowska, R.; Mędrzycka-Dąbrowska, W.; Książek, J. Assessment of Oral Health in Long-Term Enteral and Parenteral Nutrition Patients: Significant Aspects of Nursing Care. Int. J. Environ. Res. Public Health 2023, 20, 3381. https://doi.org/10.3390/ijerph20043381
Terech-Skóra S, Kasprzyk-Mazur J, Leyk-Kolańczak M, Kruk A, Piotrkowska R, Mędrzycka-Dąbrowska W, Książek J. Assessment of Oral Health in Long-Term Enteral and Parenteral Nutrition Patients: Significant Aspects of Nursing Care. International Journal of Environmental Research and Public Health. 2023; 20(4):3381. https://doi.org/10.3390/ijerph20043381
Chicago/Turabian StyleTerech-Skóra, Sylwia, Joanna Kasprzyk-Mazur, Magdalena Leyk-Kolańczak, Agnieszka Kruk, Renata Piotrkowska, Wioletta Mędrzycka-Dąbrowska, and Janina Książek. 2023. "Assessment of Oral Health in Long-Term Enteral and Parenteral Nutrition Patients: Significant Aspects of Nursing Care" International Journal of Environmental Research and Public Health 20, no. 4: 3381. https://doi.org/10.3390/ijerph20043381





