TeleRehabilitation of Social-Pragmatic Skills in Children with Autism Spectrum Disorder: A Principal Component Analysis
Abstract
:1. Introduction
2. Materials and Methods
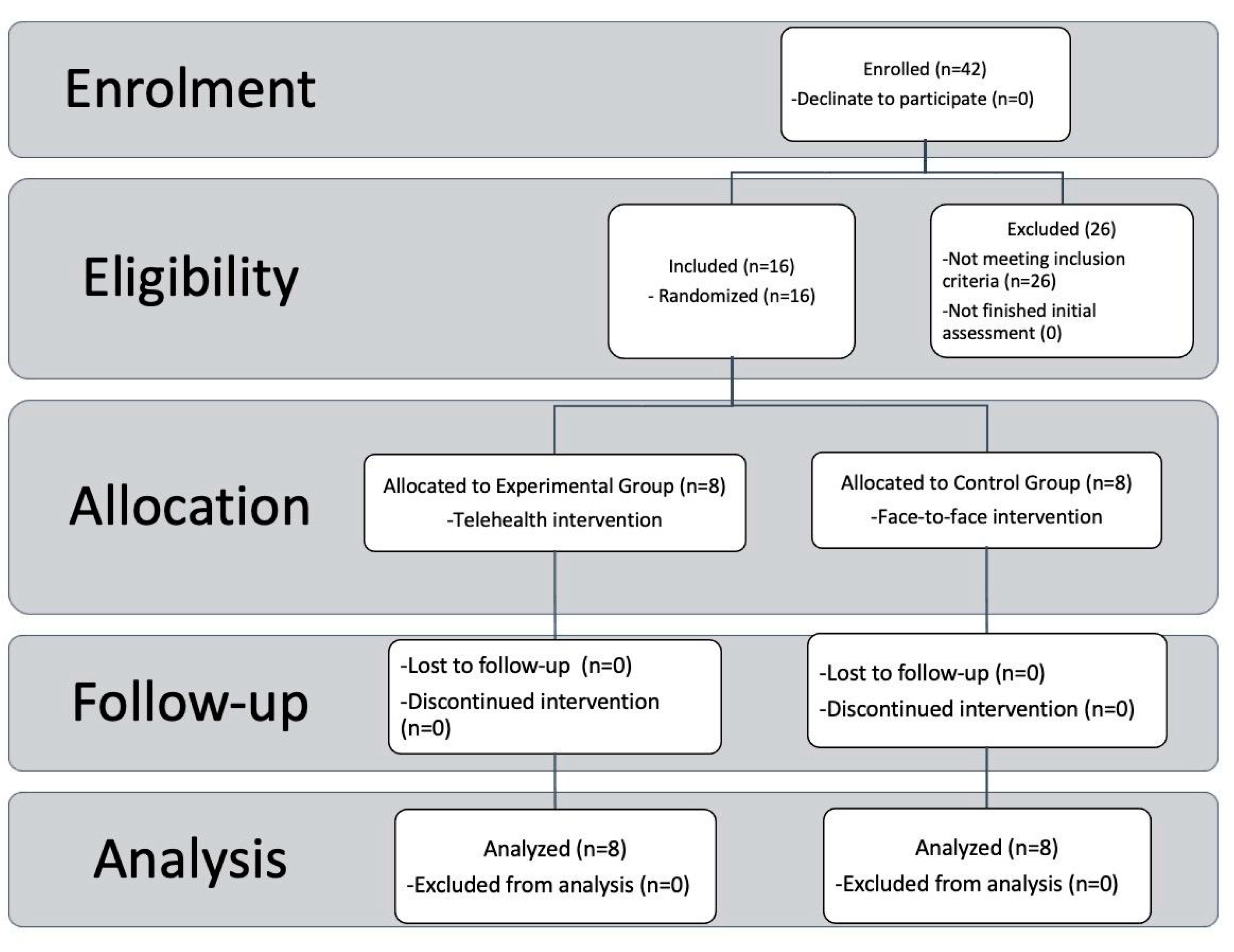
2.1. Enrollment
2.2. Study Design
2.3. Treatment
2.4. Protocol Phases
2.5. Training Experience and Setting
2.6. Outcome Measurements
- Metaphors (M), divided into Verbal Metaphors (MV) and Figured Metaphors (MF): investigate the ability to understand metaphorical language.
- Understanding of implied meaning (CSI): evaluates the ability to draw inferences on non-explicit content.
- Comics (C): evaluates the ability to understand and respect the dialogic structure in communication.
- Situations (S): evaluates the ability to understand and embrace the meaning assumed by particular expressions in social interaction.
- The color game (CG): evaluates the ability to use language in a referential way and to use skills related to the “Theory of Mind”.
2.7. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ellis, T.D.; Earhart, G.M. Digital therapeutics in Parkinson’s disease: Practical applications and future potential. J. Park. Dis. 2021, 11, S95–S101. [Google Scholar] [CrossRef] [PubMed]
- Katz, M. Telehealth increases access to palliative care for people with Parkinson’s disease and related disorders. Ann. Palliat. Med. 2020, 9 (Suppl. 1), S75–S79. [Google Scholar] [CrossRef] [PubMed]
- Lindauer, A.; Messecar, D.; McKenzie, G.; Gibson, A.; Wharton, W.; Bianchi, A.; Tarter, R.; Tadesse, R.; Boardman, C.; Golonka, O.; et al. The Tele-STELLA protocol: Telehealth-based support for families living with later-stage Alzheimer’s disease. J. Adv. Nurs. 2021, 77, 4254–4267. [Google Scholar] [CrossRef] [PubMed]
- Yousaf, K.; Mehmood, Z.; Awan, I.A.; Saba, T.; Alharbey, R.; Qadah, T.; Alrige, M.A. A comprehensive study of mobile-health based assistive technology for the healthcare of dementia and Alzheimer’s disease (AD). Health Care Manag. Sci. 2020, 23, 287–309. [Google Scholar] [CrossRef]
- Xiang, X.M.; Bernard, J. Telehealth in multiple sclerosis clinical care and research. Curr. Neurol. Neurosci. Rep. 2021, 21, 14. [Google Scholar] [CrossRef]
- Zasadzka, E.; Trzmiel, T.; Pieczyńska, A.; Hojan, K. Modern Technologies in the Rehabilitation of Patients with Multiple Sclerosis and Their Potential Application in Times of COVID-19. Medicina 2021, 57, 549. [Google Scholar] [CrossRef]
- Talbott, M.R.; Dufek, S.; Zwaigenbaum, L.; Bryson, S.; Brian, J.; Smith, I.M.; Rogers, S.J. Brief Report: Preliminary Feasibility of the TEDI: A Novel Parent-Administered Telehealth Assessment for Autism Spectrum Disorder Symptoms in the First Year of Life. J. Autism Dev. Disord. 2020, 50, 3432–3439. [Google Scholar] [CrossRef]
- Smith, C.J.; Rozga, A.; Matthews, N.; Oberleitner, R.; Nazneen, N.; Abowd, G. Investigating the accuracy of a novel telehealth diagnostic approach for autism spectrum disorder. Psychol. Assess. 2017, 29, 245–252. [Google Scholar] [CrossRef]
- Marino, F.; Chilà, P.; Failla, C.; Minutoli, R.; Vetrano, N.; Luraschi, C.; Carrozza, C.; Leonardi, E.; Busà, M.; Genovese, S.; et al. Psychological Interventions for Children with Autism during the COVID-19 Pandemic through a Remote Behavioral Skills Training Program. J. Clin. Med. 2022, 11, 1194. [Google Scholar] [CrossRef]
- Ferguson, J.L.; Majeski, M.J.; McEachin, J.; Leaf, R.; Cihon, J.H.; Leaf, J.B. Evaluating discrete trial teaching with instructive feedback delivered in a dyad arrangement via telehealth. J. Appl. Behav. Anal. 2020, 53, 1876–1888. [Google Scholar] [CrossRef]
- Neely, L.; MacNaul, H.; Gregori, E.; Cantrell, K. Effects of telehealth-mediated behavioral assessments and interventions on client outcomes: A quality review. J. Appl. Behav. Anal. 2021, 54, 484–510. [Google Scholar] [CrossRef] [PubMed]
- Lindgren, S.; Wacker, D.; Suess, A.; Schieltz, K.; Pelzel, K.; Kopelman, T.; Lee, J.; Romani, P.; Waldron, D. Telehealth and Autism: Treating Challenging Behavior at Lower Cost. Pediatrics 2016, 137, S167–S175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simacek, J.; Dimian, A.F.; McComas, J.J. Communication intervention for young children with severe neurodevelopmental disabilities via telehealth. J. Autism Dev. Disord. 2017, 47, 744–767. [Google Scholar] [CrossRef] [PubMed]
- Wallisch, A.; Little, L.; Pope, E.; Dunn, W. Parent perspectives of an occupational therapy telehealth intervention. Int. J. Telerehabil. 2019, 11, 15. [Google Scholar] [CrossRef] [PubMed]
- Little, L.M.; Wallisch, A.; Pope, E.; Dunn, W. Acceptability and cost comparison of a telehealth intervention for families of children with autism. Infants Young Child. 2018, 31, 275–286. [Google Scholar] [CrossRef]
- Vismara, L.A.; Young, G.S.; Rogers, S.J. Telehealth for expanding the reach of early autism training to parents. Autism Res. Treat. 2012, 2012, 121878. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vismara, L.A.; McCormick, C.E.B.; Wagner, A.L.; Monlux, K.; Nadhan, A.; Young, G.S. Telehealth Parent Training in the Early Start Denver Model: Results from a Randomized Controlled Study. Focus Autism Other Dev. Disabil. 2016, 33, 67–79. [Google Scholar] [CrossRef]
- Estabillo, J.A.; Moody, C.T.; Poulhazan, S.J.; Adery, L.H.; Denluck, E.M.; Laugeson, E.A. Efficacy of PEERS® for Adolescents via Telehealth Delivery. J. Autism Dev. Disord. 2022, 52, 5232–5242. [Google Scholar] [CrossRef]
- Tang, J.S.; Falkmer, M.; Chen, N.; Bölte, S.; Girdler, S. Development and feasibility of MindChip™: A social emotional telehealth intervention for autistic adults. J. Autism Dev. Disord. 2020, 51, 1107–1130. [Google Scholar] [CrossRef]
- Dai, Y.G.; Thomas, R.P.; Brennan, L.; Helt, M.S.; Barton, M.L.; Dumont-Mathieu, T.; Fein, D.A. Development and acceptability of a new program for caregivers of children with Autism Spectrum Disorder: Online parent training in early behavioral intervention. J. Autism Dev. Disord. 2021, 51, 4166–4185. [Google Scholar] [CrossRef]
- Vismara, L.A.; McCormick, C.; Young, G.S.; Nadhan, A.; Monlux, K. Preliminary findings of a telehealth approach to parent training in autism. J. Autism Dev. Disord. 2013, 43, 2953–2969. [Google Scholar] [CrossRef] [PubMed]
- Bearss, K.; Burrell, T.L.; Challa, S.A.; Postorino, V.; Gillespie, S.E.; Crooks, C.; Scahill, L. Feasibility of parent training via telehealth for children with autism spectrum disorder and disruptive behavior: A demonstration pilot. J. Autism Dev. Disord. 2018, 48, 1020–1030. [Google Scholar] [CrossRef] [PubMed]
- Paul, R.; Norbury, C. Language Disorders from Infancy through Adolescence-E-Book: Listening, Speaking, Reading, Writing, and Communicating; Elsevier Health Sciences: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Parsons, L.; Cordier, R.; Munro, N.; Joosten, A.; Speyer, R. A systematic review of pragmatic language interventions for children with autism spectrum disorder. PLoS ONE 2017, 12, e0172242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wechsler, D. Wechsler Intelligence Scale for Children-Fourth Edition (WISC-IV); CITAZIONE WISC-IV; Psychological Corporation: San Antonio, TX, USA, 2003. [Google Scholar]
- Rosati, S.; Urbinati, N. Allenare le abilità socio-pragmatiche. In Storie Illustrate per Bambini con Disturbi dello Spettro Autistico e Altri Deficit di Comunicazione; Erickson: Trento, Italy, 2016; ISBN 9788859010616. [Google Scholar]
- Lorusso, M.T. APL-Medea. In Abilità Pragmatiche del Linguaggio; Giunti OS: Firenze, Italy, 2007. [Google Scholar]
- Togashi, K.; Minagawa, Y.; Hata, M.; Yamamoto, J. Evaluation of a Telehealth Parent-Training Program in Japan: Collaboration with Parents to Teach Novel Mand Skills to Children Diagnosed with Autism Spectrum Disorder. Behav. Anal. Pract. 2022, 1–12. [Google Scholar] [CrossRef]
- Craig, E.A.; Dounavi, K.; Ferguson, J. Telehealth to train interventionists teaching functional living skills to children with autism spectrum disorder. J. Appl. Behav. Anal. 2021, 54, 511–529. [Google Scholar] [CrossRef]
- Ferguson, J.; Dounavi, K.; Craig, E.A. The impact of a telehealth platform on ABA-based parent training targeting social communication in children with autism spectrum disorder. J. Dev. Phys. Disabil. 2022, 34, 1089–1120. [Google Scholar] [CrossRef]
- Ruble, L.A.; McGrew, J.H.; Toland, M.D.; Dalrymple, N.J.; Jung, L.A. A randomized controlled trial of COMPASS web-based and face-to-face teacher coaching in autism. J. Consult. Clin. Psychol. 2013, 81, 566. [Google Scholar] [CrossRef] [Green Version]


| Pragmatic Categories | Video 1 | Video 2 |
|---|---|---|
| Children see a rabbit playing with a teddy bear, pretending that a wooden cube is a car. | The child sees a monkey pretending to iron using a pack of rice as an iron |
| Children see a bunny in the classroom with his classmates while he tells a lie about having a puppy at home because the rest of his class tells of having a pet. | The child sees a skit of a monkey who blames the fox for spilling a cup of chocolate instead of him to defend himself from his mother’s reproach. |
| Children see a little monkey pointing to his friend the fox a cloud and say that it is a sheep because the shape of the cloud is the same as a sheep. | Children see a teddy bear who is afraid to go to bed and tells his mom that there is a witch outside her door because the shadow of the plant that is near her room looks like a witch. |
| Children see a donkey giving an ugly sweater to his piggy friend. In order not to upset the donkey, the piggy says that the sweater is very beautiful. | Children see grandmother bear giving her granddaughter a pink sweater, but the granddaughter dislikes pink. The granddaughter tells her grandmother that she really likes her gift. |
| Children see a bunny rushing out of the house in the morning and accidentally taking her husband’s car keys. She says no when her husband asks if she has seen his car keys. | Children see a piggy preparing the bag to go to sea. The piggy forgets the swimsuit on the bed and leaves his room without seeing it. When his mother asks him if he has taken everything he needs to go to sea, the piggy answers yes. |
| Children see a wedding scene between a piggy and a little monkey. Among the wedding guests, there is a rabbit who is in love with the monkey. The rabbit, to hide his emotion, tells everyone that he is very happy for the little monkey who is marrying the piggy. | Children see a little piggy teasing a bear because the bear has a very large nose. Piggy’s mother scolds her son even if she thinks that big nose is really a lot of fun. |
| Children see two bunnies in the classroom near their teacher. The teacher tells the bunny that she is not just a rabbit but a princess because she is very pretty. | Children see two bears enter the monkey house. The house is very messy because the monkeys’ son has just finished playing. When the bears enter the living room, they inquire whether there has recently been an earthquake. |
| Children see a teddy bear and a piggy studying together. The two friends have to solve a difficult math problem, and they do not know how to do it. At one point, the bear says a light bulb went on, and his friend the piggy asks him where this light bulb is. | Children see a donkey and a mouse sitting in the living room. While they are talking about their neighbor monkey, the little donkey says he cannot see him at all, so the mouse suggests the little donkey put on his glasses. |
| Children see a donkey with a dirty car. The bear friend when he sees him exclaims: “How clean is your car!” | Children see a little monkey all jeweled up who meets two friends and asks them for their opinion on her appearance. The friends tell her that she is as beautiful as a Christmas tree. |
| Children see a little monkey who longs to have a motorcycle. The little monkey is still too young to ride however he goes to his daddy and asks him to buy a real motorcycle. Daddy tells him “Who put these shackles on your head?” | Children see a very hungry piggy. The piggy while talking to his fox friend says he would like to eat a mountain of chips. The fox thinks of a mountain made of chips and does not understand what the piggy means. |
| Children see a bear meeting a couple of rabbits. The couple of rabbits tell the bear that every Thursday night they go dancing. The bunny, however, says “my husband is a disaster when he dances, he is such a bear.” | Children see a little monkey meeting a rabbit. The monkey tells the rabbit that he and his friend the bear went on a roller coaster. The little monkey says that the little bear was so afraid and for that reason he was really a rabbit. |
| Children see a little monkey giving a banana to a bunny friend. The bunny says she does not like bananas. Mother rabbit tells her daughter that if she does not accept the banana, the monkey will not want to be her friend anymore. | Children see a little piggy sitting at the table who does not want to eat the spinach that their mother has cooked for him. Mother tells him that he will never be strong if he does not eat the spinach. |
| Children see a little donkey and a little bear watching a soccer game on TV. The little donkey says the national team player is a real monster. The little bear replies that she thinks the player is not so ugly. | Children see a little monkey making a smoothie with licorice and vegetables for his little donkey friend. The little monkey asks the donkey if the smoothie was good, and the donkey replies, “Sure it was, it was the end of the world!”. |
| Step | Activity | Goals |
|---|---|---|
| 1° Step | Welcome phase and greetings between group members | Increase the social area |
| 2° Step | Discussion of previous phases and administration of the history provided for within the phase | Specific skill training |
| 3° Step | Role play among the participants of the stories viewed | Skill consolidation |
| 4° Step | Identification and sharing among group members of experiences similar to those faced during the administered phase | Generalization in life contexts |
| Phases | Intervention | Meeting |
|---|---|---|
| Phase 0 | Protocol Explanation | 1 |
| Phase 1 | Pre-Assessment | 2/3 |
| Phase 2 | Pretend | 4/5 |
| Phase 3 | Lie | 6/7 |
| Phase 4 | Appearance/Reality | 8/9 |
| Phase 5 | Courtesy Lie | 10/11 |
| Phase 6 | Forgetfulness/Distraction | 12/13 |
| Phase 7 | Contrary emotion | 14/15 |
| Phase 8 | Strike | 16/17 |
| Phase 9 | Misunderstanding/Double meaning | 18/19 |
| Phase 10 | Irony/Sarcasm | 20/21 |
| Phase 11 | Figurative Language | 22/23 |
| Phase 12 | Gaffe | 24/25 |
| Phase 13 | Persuasion | 26/27 |
| Phase 14 | Complex stories | 28/29 |
| Phase 15 | Post-Assessment | 30/31 |
| Measure | Control Group (n°8) | Experimental Group (n°8) | p-Level (Chi2/Mann-Whitney) |
|---|---|---|---|
| Gender (M/F) | 7/1 | 8/0 | 0.302 |
| Age (Years) | 9.62 ± 1.92 9 (8–13) | 9.12 ± 1.46 8.5 (8–12) | 0.659 |
| Total IQ (WISC-IV) | 94 ± 9.15 92.5 (82–110) | 97 ± 11.24 102.5 (78–110) | 0.493 |
| APL-M | 3.75 ± 2.25 3 (2–8) | 6.63 ± 4.24 7 (2–14) | 0.159 |
| APL-CSI | 4.31 ± 1.96 5.25 (2–6.5) | 4.88 ± 2.7 5.25 (1–10) | 0.957 |
| APL-C | 4.75 ± 3.41 3.5 (1–10) | 2.5 ± 2.62 2 (0–7) | 0.109 |
| APL-S | 1 ± 1.19 0.5 (0–3) | 1.63 ± 2.07 1 (0–6) | 0.659 |
| APL-GC | 1.5 ± 2.82 0 (0–8) | 1.5 ± 3.85 0 (0–11) | 0.701 |
| Group | N | Mean | Median | SD | Variance | Range | Min | Max | |
|---|---|---|---|---|---|---|---|---|---|
| APL-M | Online | 8 | 2.25 | 2.00 | 1.28 | 1.64 | 4 | 0 | 4 |
| In-Presence | 8 | 3.13 | 4.00 | 1.25 | 1.55 | 3 | 1 | 4 | |
| APL-CSI | Online | 8 | 3.44 | 3.50 | 2.18 | 4.75 | 7.50 | 0.00 | 7.50 |
| In-Presence | 8 | 3.94 | 3.75 | 2.77 | 7.67 | 7.00 | 1.00 | 8.00 | |
| APL-F | Online | 8 | 3.13 | 3.00 | 3.72 | 13.84 | 12 | −2 | 10 |
| In-Presence | 8 | 2.13 | 2.00 | 2.64 | 6.98 | 9 | −2 | 7 | |
| APL-S | Online | 8 | 2.00 | 2.00 | 1.93 | 3.71 | 5 | 0 | 5 |
| In-Presence | 8 | 2.50 | 2.50 | 1.85 | 3.43 | 5 | 0 | 5 | |
| APL-GC | Online | 8 | 2.75 | 2.50 | 2.87 | 8.21 | 8 | 0 | 8 |
| In-Presence | 8 | 5.50 | 5.00 | 2.83 | 8.00 | 7 | 2 | 9 |
| Control | Experimental | |||
|---|---|---|---|---|
| Statistic | p | Statistic | p | |
| APL-M | 0.00 | 0.01 | 0.00 | 0.01 |
| APL-CSI | 0.00 | 0.01 | 0.00 | 0.02 |
| APL-F | 3.00 | 0.06 | 2.50 | 0.06 |
| APL-S | 0.00 | 0.03 | 0.00 | 0.06 |
| APL-GC | 0.00 | 0.01 | 0.00 | 0.06 |
| Scores | Statistic | p | Effect Size |
|---|---|---|---|
| APL-M | 21.00 | 0.228 | 0.345 |
| APL-CSI | 29.50 | 0.833 | 0.078 |
| APL-F | 27.50 | 0.669 | 0.140 |
| APL-S | 27.00 | 0.627 | 0.156 |
| APL-GC | 15.00 | 0.080 | 0.531 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marino, F.; Failla, C.; Bruschetta, R.; Vetrano, N.; Scarcella, I.; Doria, G.; Chilà, P.; Minutoli, R.; Vagni, D.; Tartarisco, G.; et al. TeleRehabilitation of Social-Pragmatic Skills in Children with Autism Spectrum Disorder: A Principal Component Analysis. Int. J. Environ. Res. Public Health 2023, 20, 3486. https://doi.org/10.3390/ijerph20043486
Marino F, Failla C, Bruschetta R, Vetrano N, Scarcella I, Doria G, Chilà P, Minutoli R, Vagni D, Tartarisco G, et al. TeleRehabilitation of Social-Pragmatic Skills in Children with Autism Spectrum Disorder: A Principal Component Analysis. International Journal of Environmental Research and Public Health. 2023; 20(4):3486. https://doi.org/10.3390/ijerph20043486
Chicago/Turabian StyleMarino, Flavia, Chiara Failla, Roberta Bruschetta, Noemi Vetrano, Ileana Scarcella, Germana Doria, Paola Chilà, Roberta Minutoli, David Vagni, Gennaro Tartarisco, and et al. 2023. "TeleRehabilitation of Social-Pragmatic Skills in Children with Autism Spectrum Disorder: A Principal Component Analysis" International Journal of Environmental Research and Public Health 20, no. 4: 3486. https://doi.org/10.3390/ijerph20043486







