Development and Internal Validation of Risk Assessment Models for Chronic Obstructive Pulmonary Disease in Coal Workers
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Object
2.2. Data Collection
2.3. Physical Examination
- (1)
- Height and weight: measurements were obtained with the Dekang DK-08-C height and weight meter, for which the subjects should remove shoes, hats, watches, and other items that affect the test results and the measurements should be obtained in the correct position according to the instructions of the relevant personnel.
- (2)
- Pulmonary function test: pulmonary function measurements were obtained as instructed by the staff, where the subject should sit quietly, sit with the upper body straight, keep the head horizontal, clip on the nose clip, and put on the mouthpiece according to the instructions of the professional staff before the test, while ensuring that the tongue cannot block the mouthpiece or leak air.
2.4. Definition of Ending
2.5. Variable Definitions
2.5.1. Body Mass Index(BMI)
2.5.2. Smoking Index (SI)
2.5.3. Drinking Status
2.5.4. Physical Exercise
2.5.5. Physical Activity
2.5.6. Sleep Quality
2.5.7. Cumulative Dust Exposure (CDE)
2.5.8. Shift Situation
2.5.9. Ventilation and Dust Removal Measures
2.6. Statistical Methods
2.7. Model Establishment
2.8. Model Evaluation
2.9. Establishment of a Risk Scoring System
2.9.1. Risk Scoring System
- ①
- When the variable is dichotomous, it is assigned to 0, Sn;
- ②
- When the variable is a trivial variable, it is assigned to 0, Sn/2, Sn;
- ③
- When the variable is a four-category variable, it is assigned as 0, Sn/3, 2Sn/3, Sn;
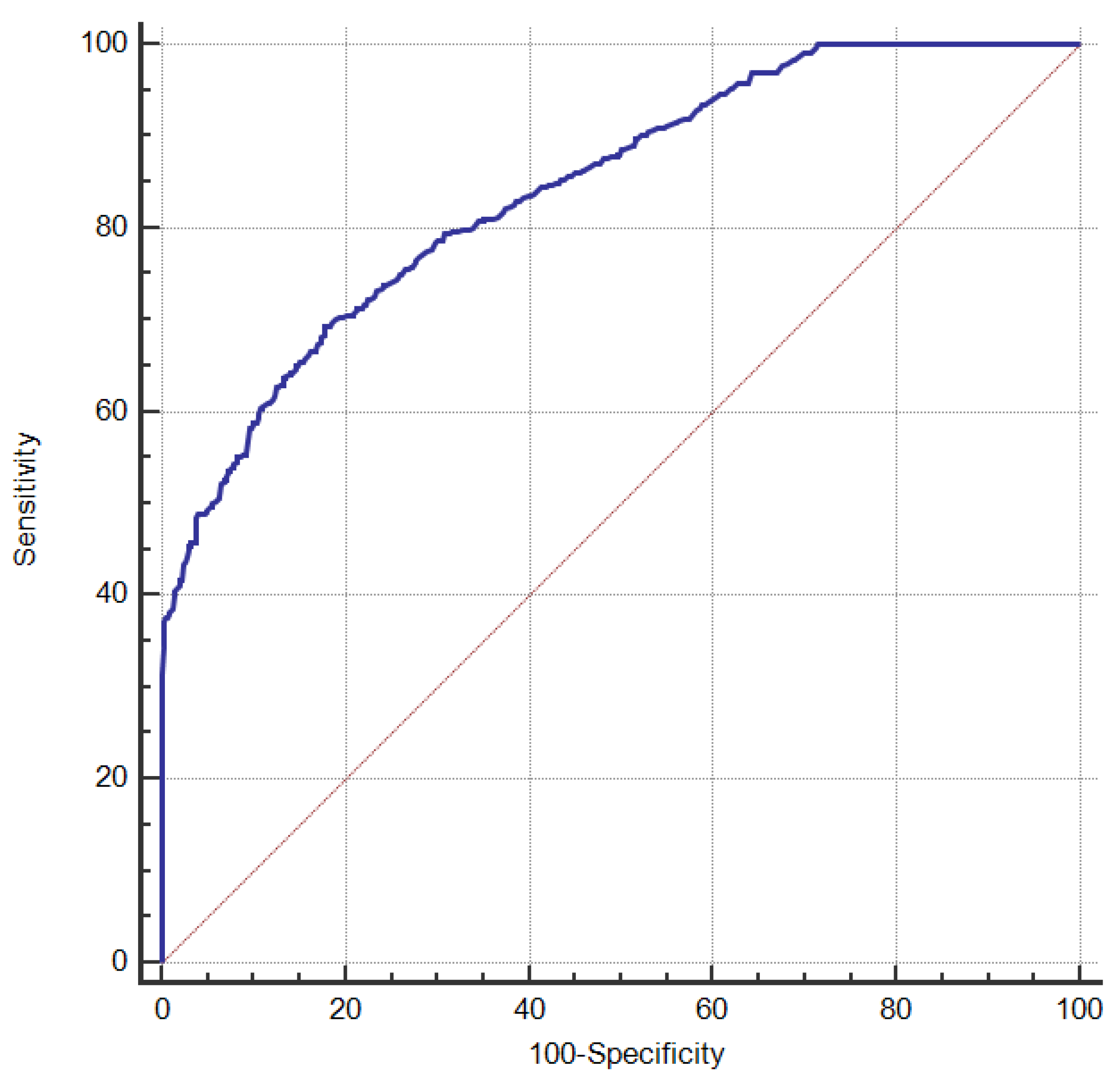
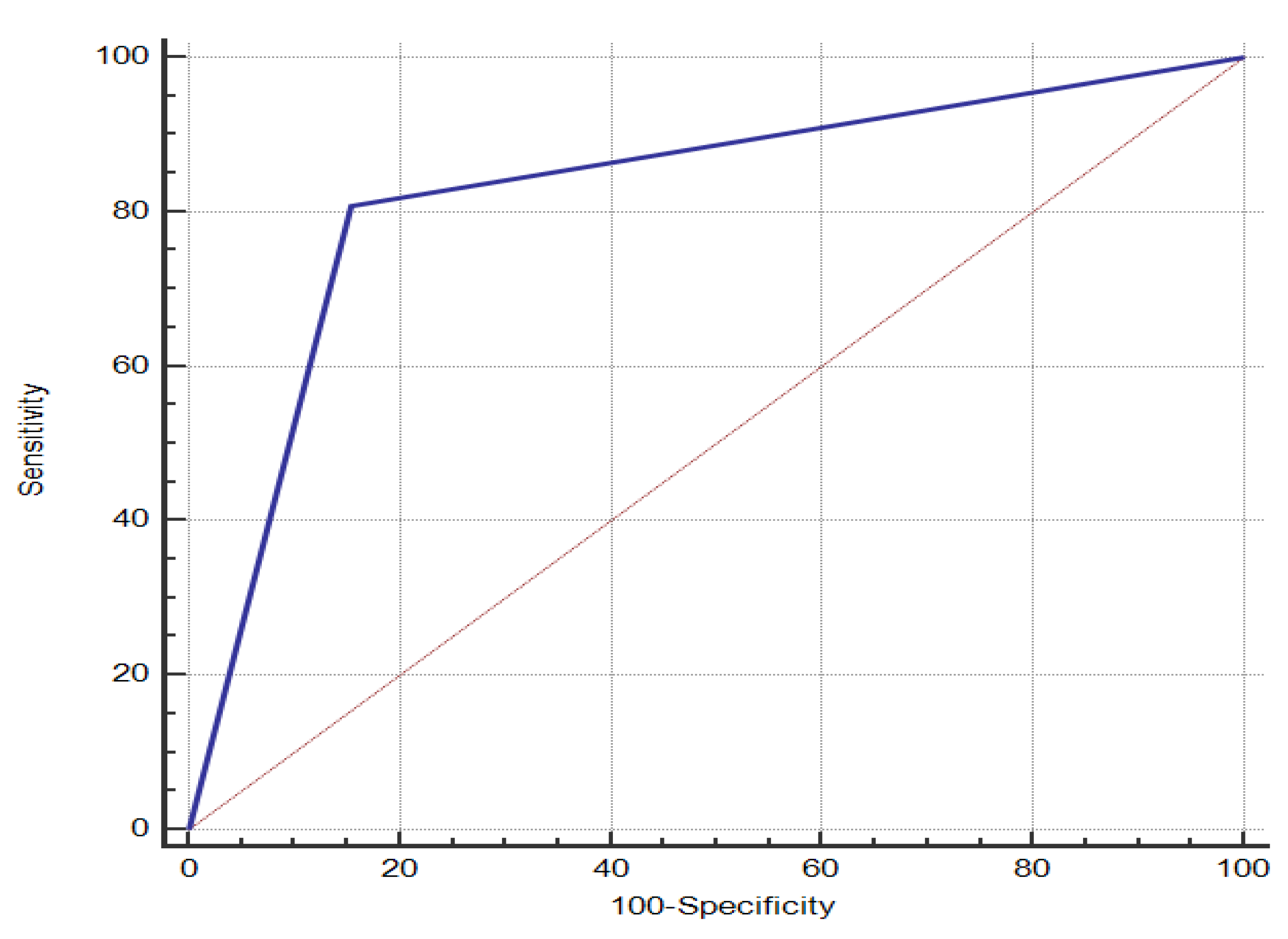
2.9.2. Mapping the ROC Curve of a COPD Risk Scoring System for Coal Workers
2.9.3. Setting up Hazard Stratification
2.9.4. Performance Evaluation of Risk Scoring Systems
- The remaining 30% of workers, classified according to the above classification criteria, were used to calculate the accuracy rate of the risk scoring system.
- The area under the ROC curve was used to determine the diagnostic value of the risk scoring system.
2.10. Quality Control
3. Results
3.1. Analysis of General Demographic Characteristics
3.2. Analysis of the Health Status of Coal Workers
3.3. Lifestyle Analysis of Coal Worker Behavior
3.4. Analysis of Occupational Harmful Factors of Coal Workers
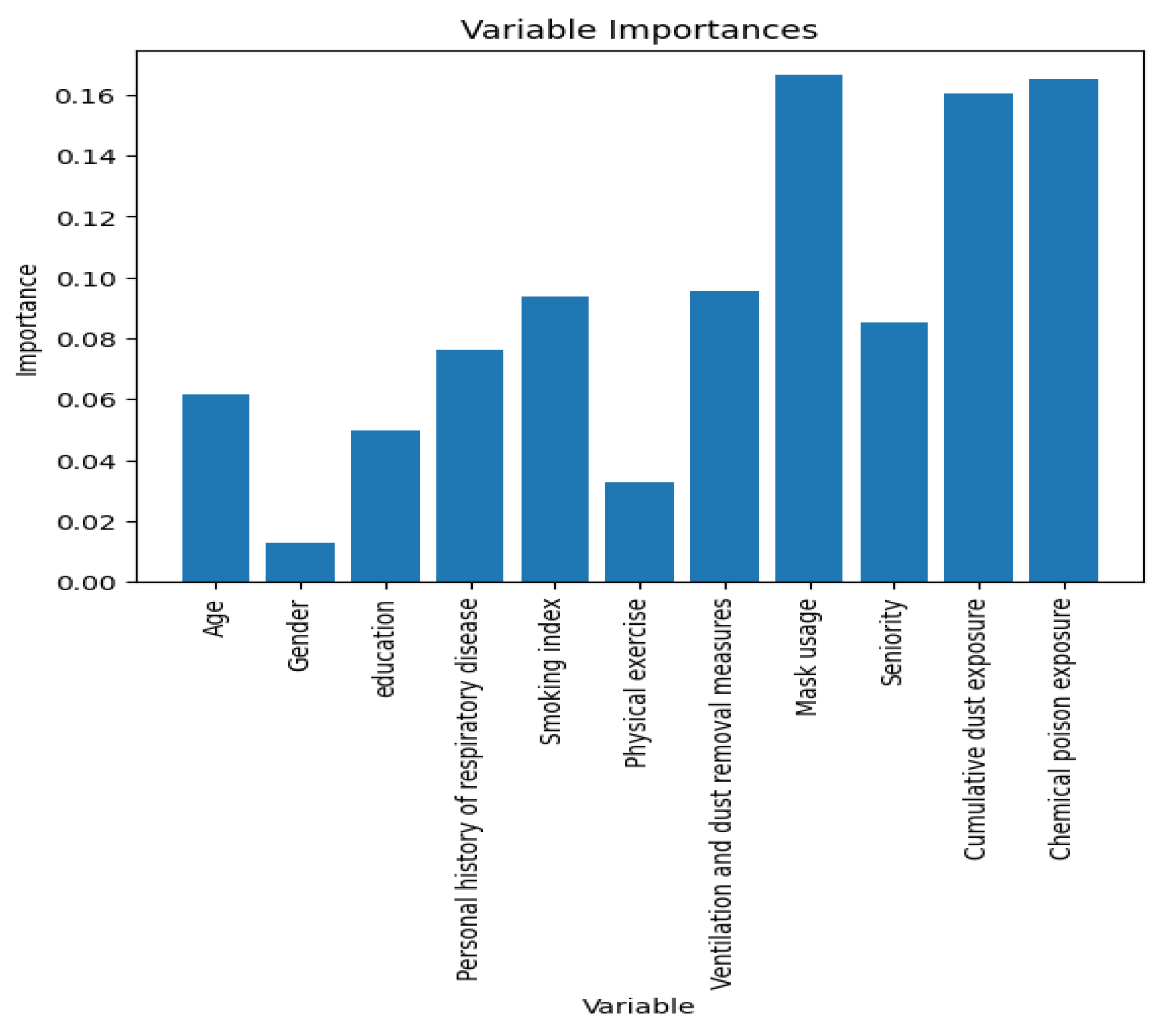
3.5. Multivariate Analysis of Influencing Factors of COPD among Coal Workers
3.6. Model Results
3.7. Risk Scoring System
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Murray, C.J.; Lopez, A.D. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet 1997, 349, 1498–1504. [Google Scholar] [CrossRef] [PubMed]
- Barnes, P.J.; Celli, B.R. Systemic manifestations and comorbidities of COPD. Eur. Respir. J. 2009, 33, 1165–1185. [Google Scholar] [CrossRef] [PubMed]
- Rothnie, K.J.; Mullerova, H.; Smeeth, L.; Quint, J. Natural History of Chronic Obstructive Pulmonary Disease Exacerbations in a General Practice-based Population with Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care. Med. 2018, 198, 464–471. [Google Scholar] [CrossRef]
- Go, L.; Krefft, S.; Cohen, R.; Rose, C. Lung disease and coal mining: What pulmonologists need to know. Curr. Opin. Pulm. Med. 2016, 22, 170–178. [Google Scholar] [CrossRef]
- Zhang, X.; Tang, F.; Ji, J.; Han, W.; Lu, P. Risk Prediction of Dyslipidemia for Chinese Han Adults Using Random Forest Survival Model. Clin. Epidemiol. 2019, 11, 1047–1055. [Google Scholar] [CrossRef] [PubMed]
- Deng, F.; Peng, M.; Li, J.; Chen, Y.; Zhang, B.; Zhao, S. Nomogram to predict the risk of septic acute kidney injury in the first 24 h of admission: An analysis of intensive care unit data. Ren. Fail 2020, 42, 428–436. [Google Scholar] [CrossRef]
- Parde, C.J.; Hu, Y.; Castillo, C.; Sankaranarayanan, S.; O’Toole, A.J. Social Trait Information in Deep Convolutional Neural Networks Trained for Face Identification. Cogn. Sci. 2019, 43, e12729. [Google Scholar] [CrossRef]
- Vives-Boix, V.; Ruiz-Fernandez, D. Diabetic retinopathy detection through convolutional neural networks with synaptic metaplasticity. Comput. Methods Programs Biomed. 2021, 206, 106094. [Google Scholar] [CrossRef]
- Vogelmeier, C.; Criner, G.; Martinez, F.; Anzueto, A.; Barnes, P.; Bourbeau, J.; Celli, B.; Chen, R.; Decramer, M.; Fabbri, L.; et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report. GOLD Executive Summary. Am. J. Respir. Crit. Care Med. 2017, 195, 557–582. [Google Scholar] [CrossRef]
- Lou, X.; He, Q. Validity and Reliability of the International Physical Activity Questionnaire in Chinese Hemodialysis Patients: A Multicenter Study in China. Med. Sci. Monit. 2019, 25, 9402–9408. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Cheng, A.; Nejati, B.; Imani, V.; Ulander, M.; Browall, M.; Griffiths, M.; Broström, A.; Pakpour, A. A thorough psychometric comparison between Athens Insomnia Scale and Insomnia Severity Index among patients with advanced cancer. J. Sleep. Res. 2020, 29, e12891. [Google Scholar] [CrossRef]
- Qian, Q.-Z.; Cao, X.-K.; Qian, Q.-Q.; Shen, F.-H.; Wang, Q.; Liu, H.-Y.; Tong, J.-W. Relationship of cumulative dust exposure dose and cumulative abnormal rate of pulmonary function in coal mixture workers. Kaohsiung J. Med. Sci. 2016, 32, 44–49. [Google Scholar] [CrossRef]
- Hansen, A.; Stayner, L.; Hansen, J.; Andersen, Z. Night shift work and incidence of diabetes in the Danish Nurse Cohort. Occup. Environ. Med. 2016, 73, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Santo, T.L. Emphysema and chronic obstructive pulmonary disease in coal miners. Curr. Opin. Pulm. Med. 2011, 17, 123–125. [Google Scholar] [CrossRef]
- Shen, F.; Yuan, J.; Sun, Z.; Hua, Z.; Qin, T.; Yao, S.; Fan, X.; Chen, W.; Liu, H.; Chen, J. Risk identification and prediction of coal workers’ pneumoconiosis in Kailuan Colliery Group in China: A historical cohort study. PLoS ONE 2013, 8, e82181. [Google Scholar] [CrossRef] [PubMed]
- Petsonk, E.L.; Rose, C.; Cohen, R. Coal mine dust lung disease. New lessons from old exposure. Am. J. Respir. Crit. Care Med. 2013, 187, 1178–1185. [Google Scholar] [CrossRef] [PubMed]
- Zhu, B.; Wang, Y.; Ming, J.; Chen, W.; Zhang, L. Disease burden of COPD in China: A systematic review. Int. J. Chron. Obstruct. Pulmon. Dis. 2018, 13, 1353–1364. [Google Scholar] [CrossRef]
- Wang, C.; Xu, J.; Yang, L.; Xu, Y.; Zhang, X.; Bai, C.; Kang, J.; Ran, P.; Shen, H.; Wen, F.; et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): A national cross-sectional study. Lancet 2018, 391, 1706–1717. [Google Scholar] [CrossRef]
- Mercado, N.; Ito, K.; Barnes, P.J. Accelerated ageing of the lung in COPD: New concepts. Thorax 2015, 70, 482–489. [Google Scholar] [CrossRef]
- Gut-Gobert, C.; Cavaillès, A.; Dixmier, A.; Guillot, S.; Jouneau, S.; Leroyer, C.; Marchand-Adam, S.; Marquette, D.; Meurice, J.-C.; Desvigne, N.; et al. Women and COPD: Do we need more evidence? Eur. Respir. Rev. 2019, 28, 180055. [Google Scholar] [CrossRef]
- Miller, M.R.; Jordan, R.E.; Adab, P. Gender differences in COPD: Are women more susceptible to smoking effects than men? Thorax 2011, 66, 921–922. [Google Scholar] [CrossRef] [PubMed]
- Gan, W.Q.; Man, P.; Postma, D.; Camp, P.; Sin, D. Female smokers beyond the perimenopausal period are at increased risk of chronic obstructive pulmonary disease: A systematic review and meta-analysis. Respir. Res. 2006, 7, 52. [Google Scholar] [CrossRef] [PubMed]
- Silva, G.; Sherrill, D.; Guerra, S.; Barbee, R. Asthma as a risk factor for COPD in a longitudinal study. Chest 2004, 126, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Xing, Z.; Sun, T.; Janssens, J.-P.; Chai, D.; Liu, W.; Tong, Y.; Wang, Y.; Ma, Y.; Pan, M.; Cui, J.; et al. Airflow obstruction and small airway dysfunction following pulmonary tuberculosis: A cross-sectional survey. Thorax 2022, 78, 274–280. [Google Scholar] [CrossRef]
- Willcox, P.A.; Ferguson, A.D. Chronic obstructive airways disease following treated pulmonary tuberculosis. Respir. Med. 1989, 83, 195–198. [Google Scholar] [CrossRef]
- Wheaton, A.; Liu, Y.; Croft, J.; VanFrank, B.; Croxton, T.; Punturieri, A.; Postow, L.; Greenlund, K. Chronic Obstructive Pulmonary Disease and Smoking Status—United States, 2017. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 533–538. [Google Scholar] [CrossRef]
- Alam, D.; Chowdhury, M.A.; Siddiquee, A.; Ahmed, S.; Clemens, J. Prevalence and Determinants of Chronic Obstructive Pulmonary Disease (COPD) in Bangladesh. COPD 2015, 12, 658–667. [Google Scholar]
- Moon, H.-G.; Zheng, Y.; An, C.H.; Kim, Y.-K.; Jin, Y. CCN1 secretion induced by cigarette smoking extracts augments IL-8 release from bronchial epithelial cells. PLoS ONE 2013, 8, e68199. [Google Scholar] [CrossRef]
- Rusznak, C.; Mills, P.R.; Devalia, J.L.; Sapsford, R.J.; Davies, R.J.; Lozewicz, S. Effect of cigarette smoke on the permeability and IL-1beta and sICAM-1 release from cultured human bronchial epithelial cells of never-smokers, smokers, and patients with chronic obstructive pulmonary disease. Am. J. Respir. Cell Mol. Biol. 2000, 23, 530–536. [Google Scholar] [CrossRef]
- Huang, X.; Laurent, R.; Zalma, R.; Pezerat, H. Inactivation of alpha 1-antitrypsin by aqueous coal solutions: Possible relation to the emphysema of coal workers. Chem. Res. Toxicol. 1993, 6, 452–458. [Google Scholar] [CrossRef]
- Weinmann, S.; Vollmer, W.; Breen, V.; Heumann, M.; Hnizdo, E.; Villnave, J.; Doney, B.; Graziani, M.; McBurnie, M.A.; Buist, S. COPD and occupational exposures: A case-control study. J. Occup. Environ. Med. 2008, 50, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Weeks, J.L. Occupational health and safety regulation in the coal mining industry: Public health at the workplace. Annu. Rev. Public Health 1991, 12, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Hartman, J.; Boezen, M.; de Greef, M.; Bossenbroek, L.; Hacken, N. Consequences of physical inactivity in chronic obstructive pulmonary disease. Expert Rev. Respir. Med. 2010, 4, 735–745. [Google Scholar] [CrossRef]
- Waschki, B.; Kirsten, A.; Holz, O.; Müller, K.-C.; Meyer, T.; Watz, H.; Magnussen, H. Physical activity is the strongest predictor of all-cause mortality in patients with COPD: A prospective cohort study. Chest 2011, 140, 331–342. [Google Scholar] [CrossRef]
- Spruit, M.; Pitta, F.; McAuley, E.; ZuWallack, R.; Nici, L. Pulmonary Rehabilitation and Physical Activity in Patients with Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2015, 192, 924–933. [Google Scholar] [CrossRef]
- Zhang, D.-D.; Liu, J.-N.; Ye, Q.; Chen, Z.; Wu, L.; Peng, X.-Q.; Lu, G.; Zhou, J.-Y.; Tao, R.; Ding, Z.; et al. Association between socioeconomic status and chronic obstructive pulmonary disease in Jiangsu province, China: A population-based study. Chin. Med. J. 2021, 134, 1552–1560. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, C.; Li, J.; Qin, S.; Liu, C.; Wang, J.; Chen, Z.; Wu, J.; Wang, G. Development and internal validation of risk prediction model of metabolic syndrome in oil workers. BMC Public Health 2020, 20, 1828. [Google Scholar] [CrossRef]
- Xing, F.; Luo, R.; Liu, M.; Zhou, Z.; Xiang, Z.; Duan, X. A New Random Forest Algorithm-Based Prediction Model of Post-operative Mortality in Geriatric Patients With Hip Fractures. Front. Med. 2022, 9, 829977. [Google Scholar] [CrossRef]
- Bodduluri, S.; Nakhmani, A.; Reinhardt, J.; Wilson, C.; McDonald, M.-L.; Rudraraju, R.; Jaeger, B.; Bhakta, N.; Castaldi, P.; Sciurba, F.; et al. Deep neural network analyses of spirometry for structural phenotyping of chronic obstructive pulmonary disease. JCI Insight 2020, 5, e132781. [Google Scholar] [CrossRef]
- Salvi, S. Tobacco smoking and environmental risk factors for chronic obstructive pulmonary disease. Clin. Chest Med. 2014, 35, 17–27. [Google Scholar] [CrossRef]
| Variable | Classify | Number | COPD | χ2 | p | |
|---|---|---|---|---|---|---|
| Number | Proportion (%) | |||||
| Age | <30 | 341 | 30 | 8.8 | 93.746 | <0.001 |
| 30~ | 1931 | 400 | 20.7 | |||
| 40~ | 1079 | 280 | 25.9 | |||
| 50~ | 604 | 208 | 34.4 | |||
| Gender | Female | 283 | 22 | 7.8 | 40.755 | 0.044 |
| Male | 3672 | 896 | 24.4 | |||
| Marital status | Unmarried | 149 | 27 | 18.1 | 5.139 | 0.077 |
| Married | 3748 | 872 | 23.3 | |||
| Others | 58 | 19 | 32.8 | |||
| Education | Junior high school and below | 1751 | 495 | 28.3 | 66.413 | <0.001 |
| High School/technical secondary school | 1222 | 280 | 22.9 | |||
| College and above | 982 | 143 | 14.6 | |||
| Household income | <5000 | 760 | 195 | 25.7 | 6.767 | 0.034 |
| 5000~ | 2600 | 606 | 23.3 | |||
| 10,000~ | 595 | 117 | 19.7 | |||
| BMI (kg/m2) | <18.5 | 83 | 26 | 31.3 | 11.083 | 0.011 |
| 18.5~ | 1234 | 307 | 25.7 | |||
| 24~ | 1723 | 404 | 23.4 | |||
| 28~ | 915 | 181 | 23.2 | |||
| Variable | Classify | Number | COPD | χ2 | p | |
|---|---|---|---|---|---|---|
| Number | Proportion (%) | |||||
| Diabetes | Yes | 364 | 97 | 26.6 | 2.657 | 0.103 |
| No | 3591 | 821 | 22.9 | |||
| Hypertension | Yes | 339 | 70 | 20.6 | 1.366 | 0.243 |
| No | 3616 | 848 | 23.5 | |||
| Personal history of respiratory disease | Yes | 1238 | 392 | 31.7 | 72.242 | <0.001 |
| No | 2717 | 526 | 19.4 | |||
| Variable | Classify | Number | COPD | χ2 | p | |
|---|---|---|---|---|---|---|
| Number | Proportion (%) | |||||
| Smoking index | 0 | 1505 | 222 | 14.8 | 112.051 | <0.001 |
| 1~ | 890 | 219 | 24.6 | |||
| 100~ | 722 | 206 | 28.5 | |||
| 200~ | 838 | 271 | 32.3 | |||
| Drinking status | Never | 1218 | 262 | 21.5 | 3.645 | 0.162 |
| Once | 82 | 23 | 28.0 | |||
| Now | 2655 | 633 | 23.8 | |||
| Physical exercise | No | 2665 | 710 | 26.6 | 53.949 | <0.001 |
| Yes | 1290 | 208 | 16.1 | |||
| Physical activity | Low | 489 | 130 | 26.6 | 3.852 | 0.146 |
| Middle | 316 | 68 | 21.5 | |||
| High | 3150 | 720 | 22.9 | |||
| Sleep quality | Accessibility | 3296 | 771 | 23.4 | 2.180 | 0.336 |
| Suspicious Insomnia | 469 | 98 | 20.9 | |||
| Insomnia | 190 | 49 | 25.8 | |||
| Vegetable intake | Never | 103 | 31 | 30.1 | 12.771 | 0.005 |
| Occasionally | 323 | 88 | 27.2 | |||
| Often | 843 | 218 | 25.9 | |||
| Every day | 2686 | 581 | 21.6 | |||
| Fruit intake | Never | 123 | 35 | 28.5 | 19.334 | <0.001 |
| Occasionally | 849 | 234 | 27.6 | |||
| Often | 1069 | 257 | 24.0 | |||
| Every day | 1914 | 392 | 20.5 | |||
| Meat intake | Never | 479 | 122 | 25.5 | 3.829 | 0.281 |
| Occasionally | 2245 | 511 | 22.8 | |||
| Often | 914 | 202 | 22.1 | |||
| Every day | 317 | 83 | 26.2 | |||
| Salt | Light | 736 | 161 | 21.9 | 0.912 | 0.634 |
| Moderate | 1935 | 456 | 23.6 | |||
| Salty | 1284 | 301 | 23.4 | |||
| Soy products | Never | 260 | 61 | 23.5 | 2.609 | 0.456 |
| Often | 1539 | 377 | 24.5 | |||
| Occasionally | 1073 | 236 | 22.0 | |||
| Every day | 1083 | 244 | 22.5 | |||
| Variable | Classify | Number | COPD | χ2 | p | |
|---|---|---|---|---|---|---|
| Number | Proportion (%) | |||||
| Shift situation | Never | 1228 | 282 | 23.0 | 0.067 | 0.967 |
| Once | 191 | 45 | 23.6 | |||
| Now | 2536 | 591 | 23.3 | |||
| Seniority (years) | <10 | 1208 | 171 | 14.2 | 142.547 | <0.001 |
| 10~ | 1748 | 407 | 23.3 | |||
| 20~ | 580 | 167 | 28.8 | |||
| 30~ | 419 | 173 | 41.3 | |||
| Cumulative dust exposure (mg/m3.years) | <50 | 546 | 79 | 14.5 | 232.826 | <0.001 |
| 50~ | 2433 | 439 | 18.0 | |||
| 100~ | 976 | 400 | 41.0 | |||
| Ventilation and dust removal measures | Difference | 214 | 101 | 47.2 | 119.244 | <0.001 |
| Ordinary | 341 | 125 | 36.7 | |||
| Good | 3400 | 692 | 20.4 | |||
| Mask usage | Never | 176 | 89 | 50.6 | 115.800 | <0.001 |
| 1–2 days/weeks | 568 | 161 | 28.3 | |||
| 3–4 days/weeks | 266 | 87 | 32.7 | |||
| Every day | 2945 | 581 | 19.7 | |||
| Chemical poison exposure | No | 2311 | 323 | 14.0 | 265.997 | <0.001 |
| Yes | 1644 | 595 | 23.2 | |||
| Variable Name | Variable Meaning | Assignment Method |
|---|---|---|
| Y | COPD | 0 = no, 1 = yes |
| X1 | Age | <30 = 1, 30~ = 2, 40~ = 3, 50~ = 4 |
| X2 | Gender | 1 = female, 2 = male |
| X3 | Education | 1 = junior high school and below, 2 = high school/technical secondary school, 3 = college and above; |
| X4 | Household income | < 5000 = 1, 5000~ = 2, 10,000~ = 3 |
| X5 | Personal history of respiratory disease | 0 = no, 1 = yes |
| X6 | Smoking index | 0 = 1, 1~ = 2, 100~ = 3, 200~ = 4 |
| X7 | Vegetable intake | Never = 0, occasionally = 1, often = 2, every day = 3 |
| X8 | Fruit intake | Never = 0, occasionally = 1, often = 2, every day = 3 |
| X9 | BMI | 1 = <18.5, 2 = 18.5~, 3 = 24~, 4 = 28~ |
| X10 | Physical exercise | 0 = No, 1 = yes |
| X11 | Ventilation and dust removal measures | Difference = 1, ordinary = 2, good = 3 |
| X12 | Mask usage | 0 = never, 1 = 1–2 days/weeks, 2 = 3–4 days/weeks, 3 = every day |
| X13 | Seniority (years) | <10 = 1, 10~ = 1, 20~ = 2, 30~ = 3 |
| X14 | Cumulative dust exposure | <50~ = 1, 50~ = 1100~ = 3 |
| X15 | Chemical poison exposure | 0 = no, 1 = yes |
| Variable | Tolerance | VIF |
|---|---|---|
| Age | 0.540 | 1.850 |
| Gender | 0.723 | 1.383 |
| Education | 0.874 | 1.144 |
| Personal history of respiratory disease | 0.965 | 1.037 |
| Smoking index | 0.906 | 1.104 |
| Physical exercise | 0.918 | 1.089 |
| Ventilation and dust removal measures | 0.678 | 1.475 |
| Mask usage | 0.710 | 1.409 |
| Seniority (years) | 0.554 | 1.804 |
| Cumulative dust exposure | 0.844 | 1.184 |
| Chemical poison exposure | 0.901 | 1.110 |
| Variable | β | SEβ | Waldχ2 | p | OR (95%CI) |
|---|---|---|---|---|---|
| Age | |||||
| <30 | - | - | - | - | 1.00 |
| 30~ | 0.595 | 0.218 | 7.410 | 0.006 | 1.812 (1.181–2.781) |
| 40~ | 0.645 | 0.216 | 8.888 | 0.003 | 1.833 (1.146–2.932) |
| 50~ | 0.501 | 0.235 | 4.553 | 0.033 | 1.770 (1.063–2.948) |
| Gender | |||||
| Female | - | - | - | - | 1.00 |
| Male | 1.378 | 0.307 | 20.108 | p < 0.001 | 3.965 (2.172–7.247) |
| Education | |||||
| Junior high school and below | — | — | — | — | 1.00 |
| High school/technical secondary school | −0.186 | 0.099 | 3.529 | 0.060 | 0.830 (0.684–1.008) |
| College and above | −0.320 | 0.1123 | 6.756 | 0.009 | 0.726 (0.570–0.924) |
| Personal history of respiratory disease | |||||
| No | — | — | — | — | 1.00 |
| Yes | 0.919 | 0.092 | 99.049 | p < 0.001 | 2.506 (2.092–3.004) |
| Household income | |||||
| <5000 | — | — | — | — | 1.00 |
| 5000~ | 0.019 | 0.111 | 0.030 | 0.863 | 1.019 (0.820–1.266) |
| 10,000~ | 0.055 | 0.156 | 0.125 | 0.724 | 1.057 (0.779–1.434) |
| Smoking index | |||||
| 0 | — | — | — | — | 1.00 |
| 1~ | 0.481 | 0.119 | 16.442 | p < 0.001 | 1.618 (1.282–2.041) |
| 100~ | 0.542 | 0.124 | 19.265 | p < 0.001 | 1.720 (1.350–2.191) |
| 200~ | 0.380 | 0.119 | 10.175 | 0.001 | 1.462 (1.158–1.847) |
| Vegetable intake | |||||
| Never | — | — | — | — | 1.00 |
| Occasionally | 0.303 | 0.379 | 0.640 | 0.424 | 1.354 (0.644–2.845) |
| Often | 0.320 | 0.361 | 0.788 | 0.375 | 1.377 (0.679–2.793) |
| Every day | 0.528 | 0.356 | 2.203 | 0.138 | 1.696 (0.844–3.408) |
| Fruit intake | |||||
| Never | — | — | — | — | 1.00 |
| Occasionally | −0.189 | 0.258 | 0.534 | 0.465 | 0.828 (0.499–1.373) |
| Often | −0.222 | 0.257 | 0.743 | 0.389 | 0.801 (0.484–1.326) |
| Every day | −0.312 | 0.252 | 1.535 | 0.215 | 0.732 (0.447–1.199) |
| BMI | |||||
| <18.5 | — | — | — | — | 1.00 |
| 18.5~ | 0.246 | 0.329 | 0.558 | 0.455 | 0.828 (0.499–1.373) |
| 24~ | 0.141 | 0.326 | 0.186 | 0.666 | 0.801 (0.484–1.326) |
| 28~ | −0.064 | 0.333 | 0.036 | 0.849 | 0.732 (0.447–1.199) |
| Physical exercise | |||||
| No | — | — | — | — | 1.00 |
| Yes | −0.321 | 0.098 | 10.748 | 0.001 | 0.726 (0.599–0.879) |
| Ventilation and dust removal measures | |||||
| Difference | — | — | — | — | 1.00 |
| Ordinary | −1.041 | 0.292 | 12.709 | p < 0.001 | 0.353 (0.199–0.626) |
| Good | −1.692 | 0.277 | 37.190 | p < 0.001 | 0.184 (0.107–0.317) |
| Mask usage | |||||
| Never | — | — | — | — | 1.00 |
| 1–2 days/weeks | −0.061 | 0.236 | 0.068 | 0.795 | 0.940 (0.592–1.496) |
| 3–4 days/weeks | −0.811 | 0.255 | 10.097 | 0.001 | 0.445 (0.270–0.733) |
| Every day | −0.532 | 0.218 | 5.996 | 0.015 | 0.588 (0.384–0.900) |
| Seniority (years) | |||||
| <10 | — | — | — | — | 1.00 |
| 10~ | 0.362 | 0.121 | 8.933 | 0.003 | 1.437 (1.133–1.822) |
| 20~ | 0.429 | 0.170 | 6.397 | 0.011 | 1.536 (1.101–2.143) |
| 30~ | 0.597 | 0.195 | 9.408 | 0.002 | 1.817 (1.241–2.662) |
| Cumulative dust exposure (mg/m3.years) | |||||
| <50 | — | — | — | — | 1.00 |
| 50~ | 0.323 | 0.145 | 4.957 | 0.026 | 1.382 (1.039–1.837) |
| 100~ | 0.801 | 0.157 | 26.102 | p < 0.001 | 2.228 (1.638–3.029) |
| Chemical poison exposure | |||||
| No | — | — | — | — | 1.00 |
| Yes | 1.091 | 0.092 | 140.818 | p < 0.001 | 2.976 (2.486–3.564) |
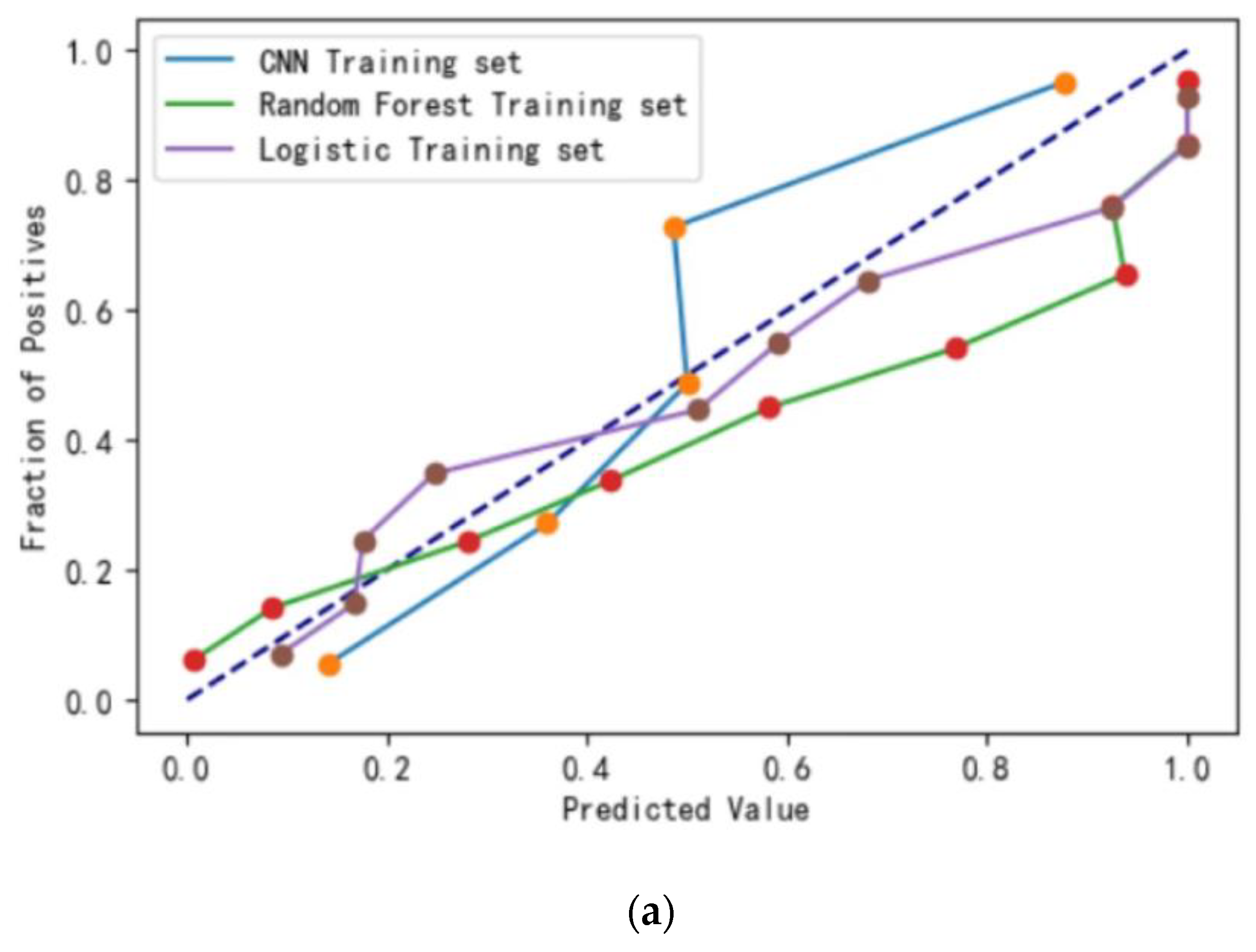
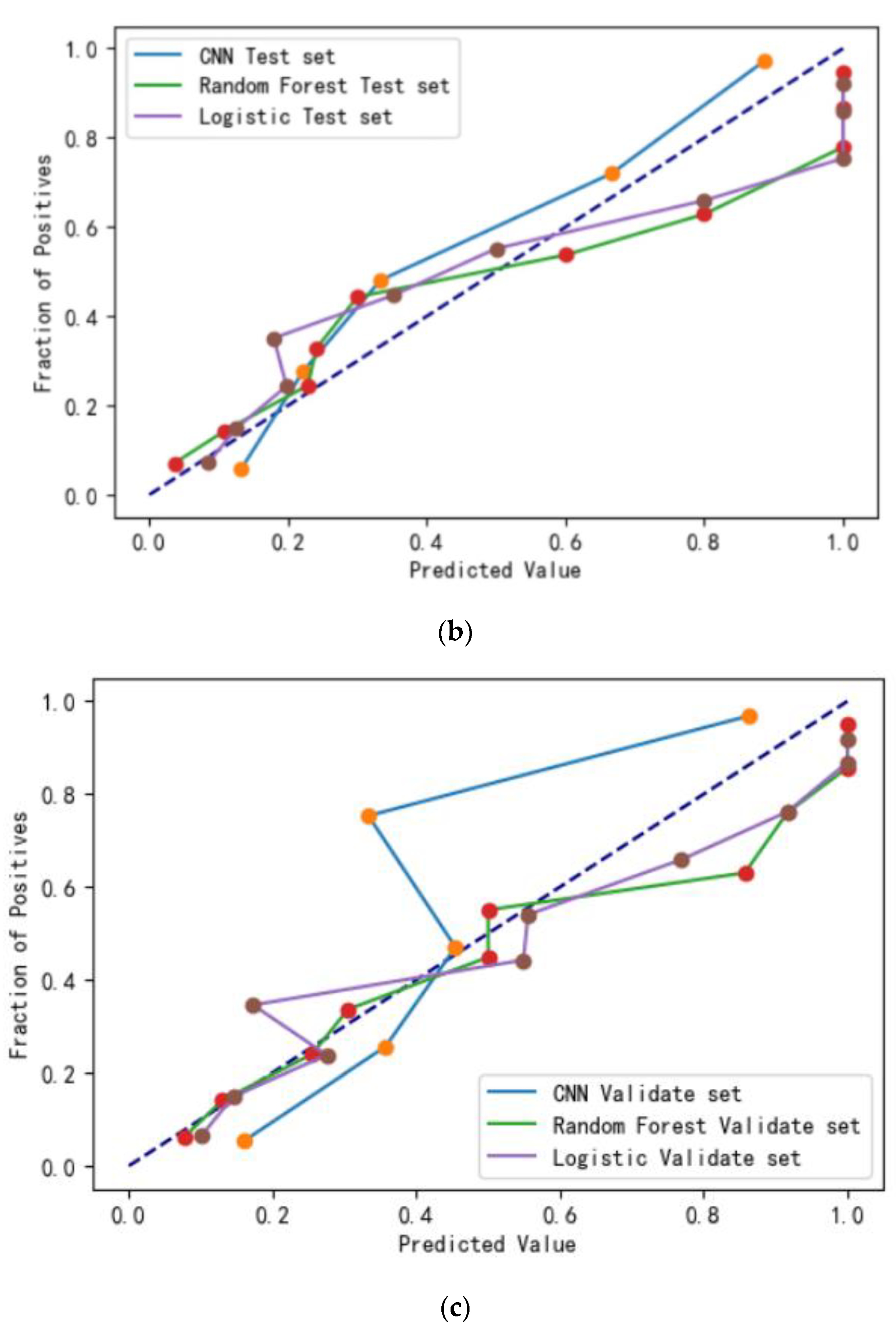
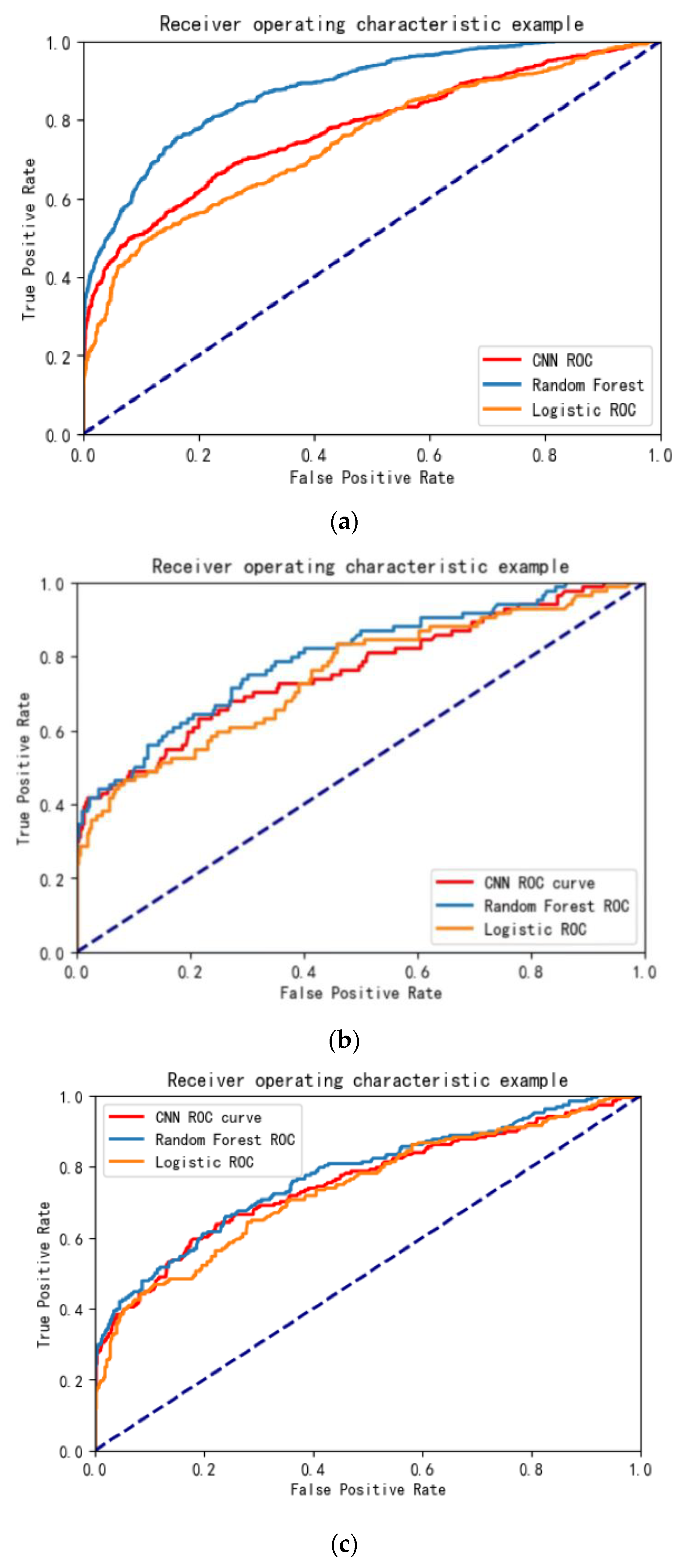
| Evaluation Indicator | Training Set | Test Set | Validation Set | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Logistic | Random Forest | CNN | Logistic | Random forest | CNN | Logistic | Random Forest | CNN | |
| Sensitivity (%) | 78.55 | 86.89 | 77.18 | 66.94 | 81.86 | 75.26 | 62.90 | 82.93 | 74.53 |
| Specificity (%) | 85.23 | 92.32 | 87.61 | 79.32 | 87.06 | 83.21 | 81.46 | 84.30 | 82.19 |
| Accuracy (%) | 81.21 | 85.40 | 83.02 | 84.10 | 85.10 | 82.55 | 80.40 | 83.11 | 85.10 |
| Brier score | 0.14 | 0.10 | 0.14 | 0.15 | 0.13 | 0.15 | 0.13 | 0.11 | 0.13 |
| AUC | 0.76 | 0.88 | 0.78 | 0.74 | 0.82 | 0.76 | 0.75 | 0.78 | 0.77 |
| Log Loss | 0.45 | 0.35 | 0.43 | 0.43 | 0.41 | 0.44 | 0.46 | 0.37 | 0.43 |
| Variable | Hazard Score |
|---|---|
| Age | <30 = 0, 30~ = 1.1, 40~ = 2.2, 50~ = 3.5 |
| Gender | Female = 0, male = 1 |
| Education | Junior high school and below = 2.5, high school/technical secondary school = 1.25, college and above = 0 |
| Personal history of respiratory disease | No = 0, yes = 4 |
| Smoking Index | 0 = 0, 1~ = 1.5, 100~ = 3, 200~ = 4.5 |
| Physical exercise | No = 2, yes = 0 |
| Ventilation and dust removal measures | Difference = 4.5, ordinary = 2.25, good = 0 |
| Mask usage | Never = 8, 1–2 days/weeks = 5.3, 3–4 days/weeks = 2.7, every day = 0 |
| Cumulative dust exposure | <50~ = 0, 50~ = 4, 100~ = 8 |
| Seniority | <10 = 0, 10~ = 1.3, 20~ = 2.6, 30~ = 4 |
| Chemical poison exposure | No = 0, yes = 8 |
| Hazard Stratification | COPD [n(%)] | Total | |
|---|---|---|---|
| Yes | No | ||
| <23.05 | 52 (19.12) | 774 (84.59) | 826 |
| ≥23.05 | 220 (80.88) | 141 (15.41) | 361 |
| Total | 272 | 915 | 1187 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, H.; Meng, R.; Wang, X.; Si, Z.; Zhao, Z.; Lu, H.; Wang, H.; Hu, J.; Zheng, Y.; Chen, J.; et al. Development and Internal Validation of Risk Assessment Models for Chronic Obstructive Pulmonary Disease in Coal Workers. Int. J. Environ. Res. Public Health 2023, 20, 3655. https://doi.org/10.3390/ijerph20043655
Wang H, Meng R, Wang X, Si Z, Zhao Z, Lu H, Wang H, Hu J, Zheng Y, Chen J, et al. Development and Internal Validation of Risk Assessment Models for Chronic Obstructive Pulmonary Disease in Coal Workers. International Journal of Environmental Research and Public Health. 2023; 20(4):3655. https://doi.org/10.3390/ijerph20043655
Chicago/Turabian StyleWang, Hui, Rui Meng, Xuelin Wang, Zhikang Si, Zekun Zhao, Haipeng Lu, Huan Wang, Jiaqi Hu, Yizhan Zheng, Jiaqi Chen, and et al. 2023. "Development and Internal Validation of Risk Assessment Models for Chronic Obstructive Pulmonary Disease in Coal Workers" International Journal of Environmental Research and Public Health 20, no. 4: 3655. https://doi.org/10.3390/ijerph20043655
APA StyleWang, H., Meng, R., Wang, X., Si, Z., Zhao, Z., Lu, H., Wang, H., Hu, J., Zheng, Y., Chen, J., Zheng, Z., Chen, Y., Yang, Y., Li, X., Xue, L., Sun, J., & Wu, J. (2023). Development and Internal Validation of Risk Assessment Models for Chronic Obstructive Pulmonary Disease in Coal Workers. International Journal of Environmental Research and Public Health, 20(4), 3655. https://doi.org/10.3390/ijerph20043655






