Effects of Medical Education Program Using Virtual Reality: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Inclusion Criteria
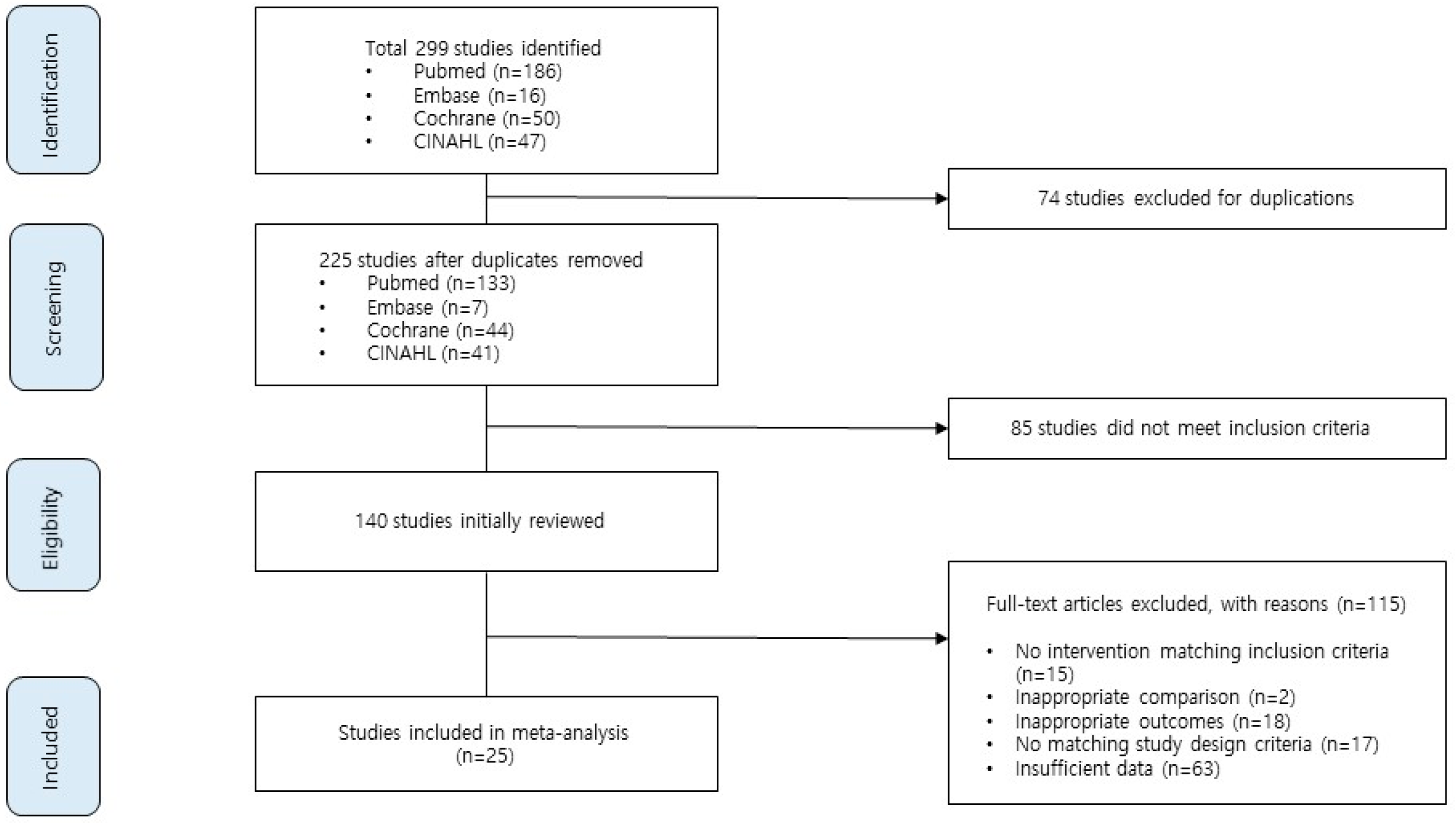
2.4. Study Selection
2.5. Data Extraction
2.6. Risk of Bias
2.7. Synthesis of Results
3. Results
3.1. Characteristics of the Research Targets (Study Selection)
3.2. Characteristics of Educational Intervention Studies Using VR Conducted on Current and Prospective Health Personnel (Study Characteristics)
3.3. Details of Training
3.4. Methodological Quality Assessment of Intervention Studies
3.5. Effect of Educational Intervention Using VR
3.5.1. Effect Size According to Skills
3.5.2. Effect Size According to Knowledge
3.5.3. Self-Efficacy
3.5.4. Satisfaction
3.5.5. Anxiety
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sherman, W.; Craig, A. Understanding Virtual Reality: Interface, Application, and Design; Morgan Kaufmann: Cambridge, MA, USA, 2018. [Google Scholar]
- Pribeanu, C.; Balog, A.; Iordache, D.D. Measuring the perceived quality of an AR-based learning application: A multidimensional model. Interact. Learn. Environ. 2017, 25, 482–495. [Google Scholar] [CrossRef]
- Hahn, J.S.; Lee, K.S. A theoretical review on designing virtual reality in the teaching-learning process. J. Educ. Technol. 2001, 17, 133–163. [Google Scholar] [CrossRef]
- Sherwood, R.J.; Francis, G. The effect of mannequin fidelity on the achievement of learning outcomes for nursing, midwifery and allied healthcare practitioners: Systematic review and meta-analysis. Nurse Educ. Today 2018, 69, 81–94. [Google Scholar] [CrossRef]
- Moro, C.; Štromberga, Z.; Raikos, A.; Stirling, A. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat. Sci. Educ. 2017, 10, 549–559. [Google Scholar] [CrossRef] [Green Version]
- Lövquist, E.; Shorten, G.; Aboulafia, A. Virtual reality-based medical training and assessment: The multidisciplinary relationship between clinicians, educators and developers. Med. Teach. 2012, 34, 59–64. [Google Scholar] [CrossRef]
- Jung, E.Y.; Park, D.K.; Lee, Y.H.; Jo, H.S.; Lim, Y.S.; Park, R.W. Evaluation of practical exercises using an intravenous simulator incorporating virtual reality and haptics device technologies. Nurse Educ. Today 2012, 32, 458–463. [Google Scholar] [CrossRef]
- Işık, B.; Kaya, H. The efect of simulation software on learning of psychomotor skills and anxiety level in nursing education. Procedia-Soc. Behav. Sci. 2014, 116, 3864–3868. [Google Scholar] [CrossRef] [Green Version]
- Rourke, S. How does virtual reality simulation compare to simulated practice in the acquisition of clinical psychomotor skills for pre-registration student nurses? A systematic review. Int. J. Nurs. Stud. 2020, 102, 103466. [Google Scholar] [CrossRef]
- Kim, S.K.; Eom, M.R.; Park, M.H. Effects of nursing education using virtual reality: A systematic review. J. Korea Contents Assoc. 2019, 19, 661–670. [Google Scholar] [CrossRef]
- Walsh, C.M.; Sherlock, M.E.; Ling, S.C.; Carnahan, H. Virtual reality simulation training for health professions trainees in gastrointestinal endoscopy. Cochrane Database Syst. Rev. 2012, 6, CD008237. [Google Scholar] [CrossRef]
- Khan, R.; Plahouras, J.; Johnston, B.C.; Scaffidi, M.A.; Grover, S.C.; Walsh, C.M. Virtual reality simulation training in endoscopy: A Cochrane review and meta-analysis. Endoscopy 2019, 51, 653–664. [Google Scholar] [CrossRef]
- Kyaw, B.M.; Saxena, N.; Posadzki, P.; Vseteckova, J.; Nikolaou, C.K.; George, P.P.; Car, L.T. Virtual reality for health professions education: Systematic review and meta-analysis by the digital health education collaboration. J. Med. Internet Res. 2019, 21, e12959. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Sterne, J.A. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, 889–893. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. 2011. Available online: http://handbook-5-1.cochrane.org (accessed on 15 March 2020).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: London, UK, 2013. [Google Scholar] [CrossRef]
- Kononowicz, A.A.; Woodham, L.A.; Edelbring, S.; Stathakarou, N.; Davies, D.; Saxena, N.; Zary, N. Virtual patient simulations in health professions education: Systematic review and meta-analysis by the digital health education collaboration. J. Med. Internet Res. 2019, 21, e14676. [Google Scholar] [CrossRef]
- Woon, A.P.; Mok, W.Q.; Chieng, Y.J.; Zhang, H.M.; Ramos, P.; Mustadi, H.B.; Lau, Y. Effectiveness of virtual reality training in improving knowledge among nursing students: A systematic review, meta-analysis and meta-regression. Nurse Educ. Today 2021, 98, 104655. [Google Scholar] [CrossRef]
- Hayre, C.M.; Kilgour, A. Diagnostic radiography education amidst the COVID-19 pandemic: Current and future use of virtual reality (VR). J. Med. Imaging Radiat. Sci. 2021, 52, S20–S23. [Google Scholar] [CrossRef]
- Birrenbach, T.; Zbinden, J.; Papagiannakis, G.; Exadaktylos, A.K.; Müller, M.; Hautz, W.E.; Sauter, T.C. Effectiveness and utility of virtual reality simulation as an educational tool for safe performance of COVID-19 diagnostics: Prospective, randomized pilot trial. JMIR Serious Games 2021, 9, e29586. [Google Scholar] [CrossRef]
- Hyun, J.S.; Kim, E.J.; Han, J.H.; Kim, N. Effects of Simulation-Based Education for Emergency Patient Nursing Care in Korea: A Meta Analysis. J. Korean Biol. Nurs. Sci. 2019, 21, 1–11. [Google Scholar] [CrossRef]
- Pottle, J. Virtual reality and the transformation of medical education. Future Healthc. J. 2019, 6, 181. [Google Scholar] [CrossRef] [Green Version]
- Al-Saud, L.M.; Mushtaq, F.; Allsop, M.J.; Culmer, P.C.; Mirghani, I.; Yates, E.; Manogue, M. Feedback and motor skill acquisition using a haptic dental simulator. Eur. J. Dent. Educ. 2017, 21, 240–247. [Google Scholar] [CrossRef] [Green Version]
- Våpenstad, C.; Hofstad, E.F.; Langø, T.; Mårvik, R.; Chmarra, M.K. Perceiving haptic feedback in virtual reality simulators. Surg. Endosc. 2013, 27, 2391–2397. [Google Scholar] [CrossRef]
- Alhalabi, W. Virtual reality systems enhance students’ achievements in engineering education. Behav. Inf. Technol. 2016, 35, 919–925. [Google Scholar] [CrossRef]
- Kourtesis, P.; Collina, S.; Doumas, L.A.; MacPherson, S.E. Validation of the virtual reality neuroscience questionnaire: Maximum duration of immersive virtual reality sessions without the presence of pertinent adverse symptomatology. Front. Hum. Neurosci. 2019, 13, 417. [Google Scholar] [CrossRef] [Green Version]
- Jensen, L.; Konradsen, F. A review of the use of virtual reality head-mounted displays in education and training. Educ. Inf. Technol. 2017, 23, 1515–1529. [Google Scholar] [CrossRef] [Green Version]
- Weech, S.; Kenny, S.; Barnett-Cowan, M. Presence and cybersickness in virtual reality are negatively related: A review. Front. Psychol. 2019, 10, 158. [Google Scholar] [CrossRef] [Green Version]
- Farmani, Y.; Teather, R.J. Evaluating discrete viewpoint control to reduce cybersickness in virtual reality. Virtual Real. 2020, 24, 645–664. [Google Scholar] [CrossRef]
- Tiiro, A. Effect of Visual Realism on Cybersickness in Virtual Reality; University of Oulu: Oulu, Finland, 2018. [Google Scholar]
- Hsiao, S. Effects of the Application of Virtual Reality to Experiential Education on Self-Efficacy and Learning Motivation of Social Workers. Front. Psychol. 2021, 12, 770481. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Choi, J.Y.; Kweon, Y.R. Correlations among learning self-efficacy, confidence in performance, perception of importance and transfer intention for core basic nursing skill in nursing students at a nursing university. J. Korea Contents Assoc. 2017, 17, 661–671. [Google Scholar] [CrossRef]
- Checa, D.; Miguel-Alonso, I.; Bustillo, A. Immersive virtual-reality computer-assembly serious game to enhance autonomous learning. Virtual Real. 2021, 1–18. [Google Scholar] [CrossRef]
- Jallad, S.T.; Işık, B. The effectiveness of virtual reality simulation as learning strategy in the acquisition of medical skills in nursing education: A systematic review. Ir. J. Med. Sci. 2021, 191, 1407–1426. [Google Scholar] [CrossRef]
- Halloran, D.A. Examining the Effect of Virtual Simulation on Anxiety Experienced by Pediatric Nursing Students. Ph.D. Thesis, Cappella University, Minneapolis, MN, USA, 2017. [Google Scholar]
- Wang, Y.; Guo, L.; Xiong, X. Effects of Virtual Reality-Based Distraction of Pain, Fear, and Anxiety during Needle-Related Procedures in Children and Adolescents. Front. Psychol. 2022, 13, 1603. [Google Scholar] [CrossRef]
- Gold, J.I.; Mahrer, N.E. Is virtual reality ready for prime time in the medical space? A randomized control trial of pediatric virtual reality for acute procedural pain management. J. Pediatr. Psychol. 2018, 43, 266–275. [Google Scholar] [CrossRef] [Green Version]


| Author (Year) /Country | Study Design | Sample Size | Participants | Age [Mean/Median] (SD/Range) | VR Device (FI/LI) | Feedback | Intervention | Comparator | Session (Total Time) | Outcome | Measurement Tool (Items) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Exp. | Cont. | |||||||||||
| Andreatta et al. (2010)/ USA | RCT | 15 | 7 | 8 | postgraduate year 1 to 4 emergency medicine residents | NR | VR CAVE (FI) | NR | VR triage training | SP (standardized patient) | 1 (NR) | Knowledge | Self-developed MCQ (24) |
| Brinkmann et al. (2017)/ Germany | RCT | 36 | 18 | 18 | medical students | E 23 (21–29) C 23.5 (22–40) | Lap Mentor; Simbionix (LI) | Intensive feedback and individual coaching | VR laparoscopic cholecystectomy | FLS Program | 8 (NR) | Skill Self-efficacy | GOALS (5) self-assessment (6) |
| Cannon et al. (2014)/ USA | RCT | 48 | 27 | 21 | postgraduate year 3 orthopedic residents | NR | ArthroSim (LI) | Tactile feedback | VR arthroscopic knee surgery | standard education | 4 (11 h) | Skill | GRS (7) Procedural checklist (21) |
| Chou et al. (2006)/ USA | RCT | 16 | 8 | 8 | first-year medical students | E 23.9 (2.2) C 23.4 (1.7) | UROMentor; Simbionix (LI) | Tactile feedback | VR ureteroscopy training | TMU (mannequin) | 1 (2 h) | Skill | OSATS (6) |
| Farra et al. (2013)/ USA | RCT | 47 | 22 | 25 | 2nd-year associate degree nursing students | (18–57) | 3-D Second Life platform (FI) | Provided to the learner note cards and message | VRS in disaster training | web-based modules | 1 (20 min) | Knowledge | Validated MCQ (20) |
| Feifer et al. (2011)/USA | RCT | 20 | E1:5 E2:5 | C1:5 C2:5 | medical students | (20–46) | LapSIM; daVinci robotic platform (LI) | NR | VR for robotic surgical training | C1:ProMIS C2:no training | 5 (NR) | Skill | MISTELS |
| Halloran et al. (2017)/ USA | RCT | 137 | 70 | 67 | undergraduate nursing students | 27.75 (6.43) | ATI Real Life modules (LI) | NR | Virtual patient simulation for pediatric | no training | 2 (2.5 h) | Anxiety | STAI (40) |
| Jiang et al. (2018)/ China | RCT | 46 | 23 | 23 | 3-years anesthesia residents | E 25.1 (1.8) C 25.0 (1.6) | GI-Bronch Mentor; Simbionix (LI) | Tactile feedback and oral instructions | VR fiberoptic bronchoscope manipulation | high-fidelity mannequin | 25 (NR) | Skill Confidence | GRS (6) 5-point Likert rating scale |
| Jung et al. (2012)/ Korea | RCT | 114 | E1:38 E2:38 | 38 | 1-years nursing students | E1 21.13 (3.53) E2 19.08 (0.71) C 19.26 (1.22) | ARSim IV-100 (LI) | Haptic feedback | VR intravenous practical exercise | catheterization on mannequins | 1 (10 min) | Anxiety Procedure score | VAS Checklist score (10) |
| Ko et al. (2018)/ China | RCT | 36 | 12 | C1:12 C2:12 | junior residents, interns, and elective students | NR | LAP Mentor; Simbionix (LI) | Unclear | VRS for gynecology laparoscopic suturing training | C1:box training C2:no training | 2 (4 h) | Skill | GOALS (4) |
| Kowalewski et al. (2018)/ Germany | RCT | 64 | 33 | 31 | postgraduate year 3–6 senior residents | E 28.1 (2.4) C 28.5 (2.6) | Lap Mentor II; Simbionix (LI) | NR | Multi-modality training (VR with box training) for laparoscopic cholecystectomy | no training | 8 (12 h) | Skill | GOALS (5) |
| Leblanc et al. (2013)/ Canada | RCT | 22 | 11 | 11 | orthopedic surgery residents | (25–40) | Tabs with the haptic device; PHANTOM (LI) | Haptic feedback | VR surgical fixation for ulnar fracture | Sawbones simulator | NR | Skill | GRS (6) |
| Lucas et al. (2008)/ USA | RCT | 32 | 16 | 16 | first- and second-year medical students | NR | Lap Mentor; Simbionix (LI) | NR | VRT for laparoscopic cholecystectomy | no training | 6 (3 h) | Skill Knowledge | OSATS (8) |
| Nickel et al. (2015)/ Germany | RCT | 84 | 42 | 42 | medical students | E 24.5 (2.6) C 24.1 (2.1) | Lap Mentor; Simbionix (LI) | NR | VRT for laparoscopic cholecystectomy | Blended Learning (10 h of box training + 2 h of E-learning) | 3 (12 h) | Skill Knowledge | OSATS (7) |
| Padilha et al. (2019)/ Portugal | RCT | 42 | 21 | 21 | second-year nursing students | E 19.29 (0.46) C 20.29 (2.19) | VSIM (LI) | NR | Clinical virtual simulation scenario using case-based learning | low-fidelity simulator | 1 (45 min) | Knowledge Self-efficacy Satisfaction | True/false and multiple-choice test General self-efficacy scale (10) learner satisfaction with simulation tool (20) |
| Park et al. (2007)/ Canada | RCT | 24 | 12 | 12 | general surgery and internal medicine residents | NR | AccuTouch colonoscopy simulator (LI) | Haptic feedback | VRT for colonoscopy | no further training | 1 (2–3 h) | Skill | GRS (7) |
| Rossler et al. (2018)/ USA | RCT | 20 | 5 | 15 | prelicensure baccalaureate nursing students | NR | Virtual Electrosurgery Skill Trainer (LI) | NR | VRS for OR fire drill scenario | traditional programmatic education | NR | Knowledge | Self-developed MCQ (7) + true/false test (3) |
| Stepan et al. (2017)/ USA | RCT | 66 | 33 | 33 | first- and second-year medical students | NR | Oculus Rift VR system, LLC, a VR head-mounted display (FI) | NR | VRS for neuroanatomy | online textbook | 1 (20 min) | Knowledge Self-efficacy Satisfaction | Self-developed MCQ (10/30) + fill-in-the-blank questions IMMS (36) |
| Suebnukarn et al. (2011)/ Thailand | RCT | 32 | 16 | 16 | fourth-year dental students | NR | 2.8-GHz Pentium 4PC, with 256 MB RAM and a 13-in computer monitor, connected to two haptic devices (LI) | Haptic feedback | VR for cavity preparation training | training using extracted teeth and phantom head | 3 (2 h) | Skill | 4-point scale (4) |
| Tubelo et al. (2016)/ Brazil | RCT | 18 | 9 | 9 | undergraduate dentistry students | NR | Articulate Storyline 2 (LI) | Positive or negative message feedback | Virtual simulation for dentistry | traditional method of education (book) | 1 (20 min) | Knowledge | True/false question (10) |
| Vaccaro et al. (2013)/ USA | RCT | 18 | 9 | 9 | postgraduate years 2–5 resident physicians | NR | DaVinci surgical simulator (FI) | NR | Robotic VRS for surgical skill | Standard Robotic Orientation | 1 (3 h) | Skill | GRS (5) |
| Vargas et al. (2016)/ USA | RCT | 36 | 19 | 19 | medical students | 24.9 | daVinci Surgical Simulator (FI) | Expert surgeon provided instruction to all participants | VRT for gynecologic surgery of a cystotomy closure | standard education | 10 (NR) | Skill | GEARS (5) |
| Waterman et al. (2016)/ USA | RCT | 22 | 12 | 10 | orthopedic surgery trainees | E (32) C (33) | Arthro VR shoulder simulator; Smbionix (LI) | Haptic feedback | VRS for diagnostic shoulder arthroscopy | standard practice | 4 (1 h) | Skill | ASSET (8) |
| Wilhelm et al. (2002)/ | RCT | 21 | 11 | 10 | medical students | E 23.7 (1.8) C 24.2 (1.4) | UROMentor; Simbionix (LI) | Expert endoscopists provided supervised training to the training group | VR case scenario for basic endoscopic performance | no further training | 5 (2 h 30) | Skill Self-efficacy | GRS (5) 5-point self-evaluation (10) |
| Wong et al. (2019)/ | RCT | 31 | 16 | 16 | medical students, anesthesia assistants, anesthesia residents | E 54.8 (10) C 55.1 (18) | ORSIM airway simulator (LI) | NR | VR bronchoscopy simulator training to FOB | no further training | 1 (1 h) | Skill | GRS (8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.-Y.; Kim, E.-Y. Effects of Medical Education Program Using Virtual Reality: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 3895. https://doi.org/10.3390/ijerph20053895
Kim H-Y, Kim E-Y. Effects of Medical Education Program Using Virtual Reality: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2023; 20(5):3895. https://doi.org/10.3390/ijerph20053895
Chicago/Turabian StyleKim, Hyeon-Young, and Eun-Young Kim. 2023. "Effects of Medical Education Program Using Virtual Reality: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 20, no. 5: 3895. https://doi.org/10.3390/ijerph20053895
APA StyleKim, H.-Y., & Kim, E.-Y. (2023). Effects of Medical Education Program Using Virtual Reality: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 20(5), 3895. https://doi.org/10.3390/ijerph20053895









