Designing Digital COVID-19 Screening: Insights and Deliberations
Abstract
1. Introduction
2. Augmenting the Health Screening Process
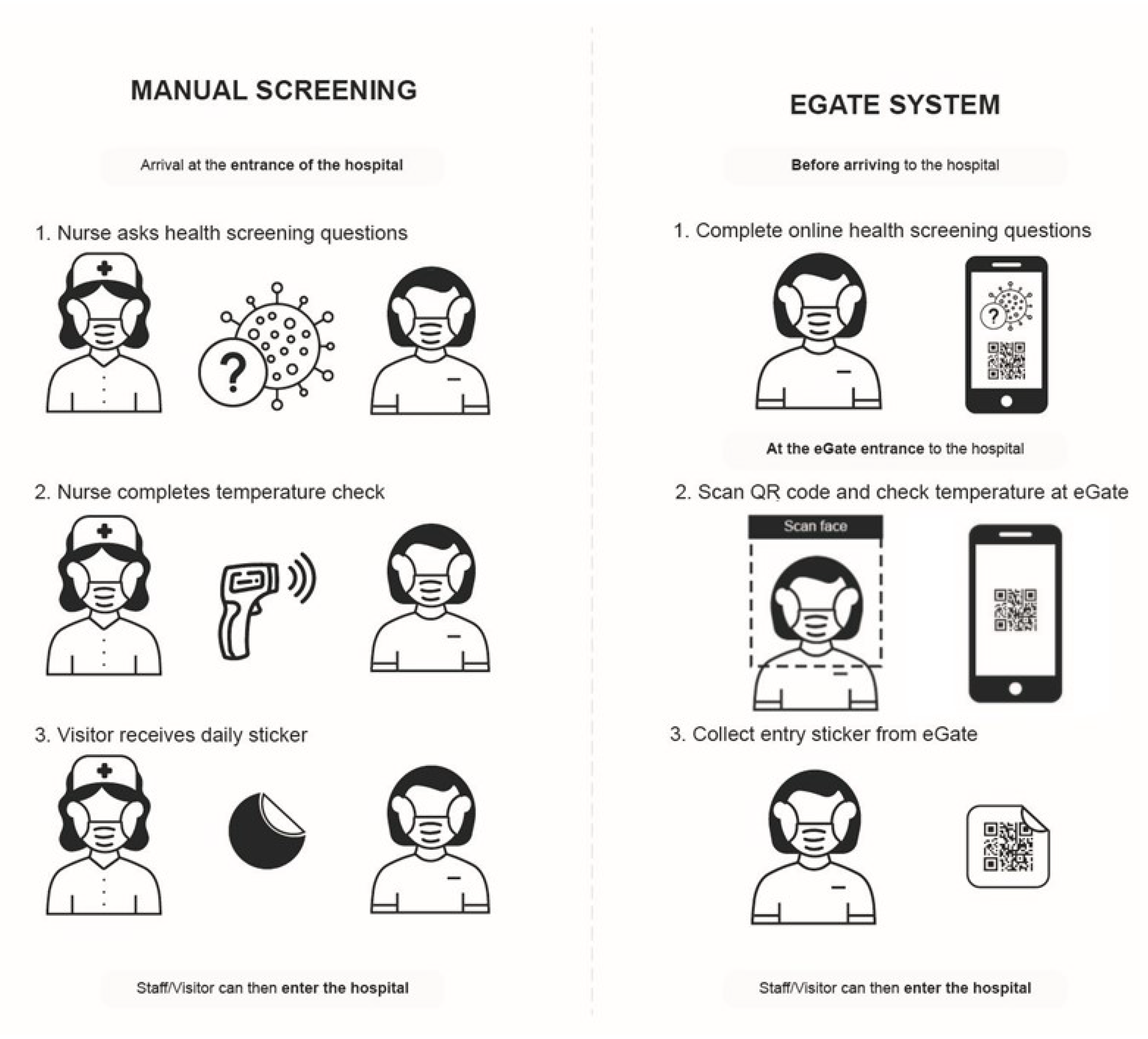
2.1. Manual Screening Process
2.2. Egate Digital-Screening Process
- ALLOWED ENTRY: If temperature was below the pre-determined threshold e.g., less than 37.4 °C/99.32 °F, the physical gate opens to allow hospital entry. The profile behind the unique QR code is updated with temperature data and hospital pass entry is validated for the day. The QR code is printed on a physical sticker and collected by the participant as they enter the hospital. The printed sticker QR code is valid for one day and can be used as a way to gain faster entry through the gate without the need to go through the screening process again.
- PROHIBITED ENTRY: If temperature is out of the valid range e.g., more than 37.4 °C/99.32 °F, physical gate remains closed and the person is advised to see the screening staff. The profile behind the unique QR code is updated with temperature data and the hospital pass is defined as no entry for the day unless overridden by screening staff with an updated temperature reading from tympanic (ear-reading) temperature or overridden using the exception system by senior screening staff.
3. Methods
3.1. Egate Setup
3.2. Data Collection Procedure
3.2.1. Interviews
3.2.2. Questionnaire
3.3. Qualitative Data Analysis
4. Findings and Recommendations
4.1. Considerations for People
4.1.1. Shifting Authority and Accountability
| Design Recommendation:Balance of power Aligning the authority afforded to both the eGate and screening staff team can reduce the risk of total perceived authority being misconstrued to either party. Should the eGate be entirely undermined, pressure will return to the screening staff team to manually screen all individuals entering the hospital–an inconvenient and unsustainable system that positions multiple screening staff members on the metaphoric “front lines”. However, should all authority and power be given to only the eGate, individuals who find a way to “cheat” (be dishonest in their responses or strong-arm their way through the gate) could go unchecked. Therefore, ensuring that the screening staff team and eGate system work in tandem, presenting a united front of equal authority, is essential. This could look like: making the physical presence of the screening staff team more imposing by positioning them as a component of the eGate rather than behind it, or the inclusion of a concealed button that directs users from the gate to the screening staff, allowing for the manual confirmation of a visitor’s screening. |
4.1.2. Learnability
| Design Recommendation:Developing literacy through training Despite initial attempts and distributing instructional material, this projects highlights the importance of planned and considered training initiatives alongside new technologies. Ensuring that training materials are consistently available to staff and visitors is a reasonable first step. However, careful consideration to the types of material offered is similarly worthwhile. As these resources serve to develop the digital literacy skills of a range of screening staff participants (e.g., casual staff who may not be exposed to the eGate frequently, visitors to the hospital who have limited digital and technological literacy skills) who will not only use the eGate themselves but also be responsible for supporting unfamiliar users. This could look like: a dedicated series of training workshops courses or the provision of supplementary training material (i.e., videos and guides) which are accessible to staff offsite. |
4.1.3. Troubleshooting and “Hacking” the System
| Design Recommendation:Facilitate crowdsourced knowledge The initiative demonstrated by screening staff to continuously adapt to and problem-solve with the eGate is an admirable reflection of the team. As such, the cultivation of these “hacks”, developed by those who worked the closest to the system is something that should be supported rather than stifled. In order to do this, facilitating the communication and dissemination of these “hacks” amongst screening staff and other staff is imperative. This could look like: having a dedicated channel for communicating and sharing system management “hacks” or fostering a community within the hospital of dedicated “hackers”. |
4.1.4. Accessibility
| Design Recommendation:Inclusivity Inclusive design is generally important in the design and development of various interventions. However, given that the eGate is deployed in a hospital, whereby visitors with a greater diversity of abilities is common, these principles are particularly notable. This could look like: developing and abiding by an accessibility guideline relevant to the hospital or increasing the diversity of participants in testing stages. |
4.2. Considerations for the System
4.2.1. Ergonomics and Interactive Affordances
| Design Recommendation:Towards reactive systems Similar to the recommendation previously detailed (Inclusivity), this recommendation focuses on ensuring the system can be utilised by the diverse range of visitors who frequent the hospital. By this, we mean that it is important for the system to not only effectively communicate how it should be used to its audience, but also respond to multiple forms of interaction in order to seamlessly guide an individual through its operations. This could look like: integrating responsive feedback that makes individuals aware of and supports them in recovering from errors, or the facilitation of rapidly adaptable components that can be customised to the needs of each user. |
4.2.2. Efficiency
| Design recommendation:Redundancies When critical eGate hardware or software was not functional, it was not always feasible for screening staff to address the problem at that time (e.g., during busy peak periods there is not enough time to try and reset the system lest they produce an even larger queue). In these scenarios, screening staff resort to a manual screening process without the eGate, instead writing down the staff or visitor’s details with pen and paper, and then providing them a coloured sticker (which alternated daily) to show they have passed screening for the day. This fallback was also used when a visitor arrived without a smartphone or had a smartphone that was not working properly. To preserve the function of the eGate, additional fallback measures should be integrated into the system, allowing for partial rather than full system failure. This could look like: an additional set of controls which operate each feature in isolation or a partial-failure fallback whereby the system operates at partial capacity. |
5. Discussion
5.1. Deliberations for Designing Screening Systems
5.1.1. Prior Efforts and Preparation
5.1.2. System Redundancies
5.1.3. Visibility and Accuracy of Data
5.1.4. Scalability and Sustainability
5.1.5. Lowering the Risk of Exposure
“[The eGate] helps with social distancing - I don’t need to get closer with the person to check the temperature and I just need to hand over the sticker so it that way it is very efficient”(P1)
“It is good because we have a less contact its quicker system as well”(P2)
“Good thing is we don’t need to get up close and touch them, our role is to just guide them through the system”(P4)
“The concierge staff doesn’t need to stay close to check visitor’s temperature - able to maintain social distancing.”(P18)
“I think it is better in regard to social distancing and keeping screening staff safer”(P9)
5.2. Interrelationship of Considerations
5.3. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chang, S.L.; Harding, N.; Zachreson, C.; Cliff, O.M.; Prokopenko, M. Modelling transmission and control of the COVID-19 pandemic in Australia. Nat. Commun. 2020, 11, 5710. [Google Scholar] [CrossRef]
- Danon, L.; Brooks-Pollock, E.; Bailey, M.; Keeling, M. A spatial model of COVID-19 transmission in England and Wales: Early spread, peak timing and the impact of seasonality. Philos. Trans. R. Soc. B 2021, 376, 20200272. [Google Scholar] [CrossRef]
- Haldane, V.; De Foo, C.; Abdalla, S.M.; Jung, A.S.; Tan, M.; Wu, S.; Chua, A.; Verma, M.; Shrestha, P.; Singh, S.; et al. Health systems resilience in managing the COVID-19 pandemic: Lessons from 28 countries. Nat. Med. 2021, 27, 964–980. [Google Scholar] [CrossRef]
- Sun, S.; Xie, Z.; Yu, K.; Jiang, B.; Zheng, S.; Pan, X. COVID-19 and healthcare system in China: Challenges and progression for a sustainable future. Glob. Health 2021, 17, 14. [Google Scholar] [CrossRef]
- Islam, M.S.; Rahman, K.M.; Sun, Y.; Qureshi, M.O.; Abdi, I.; Chughtai, A.A.; Seale, H. Current knowledge of COVID-19 and infection prevention and control strategies in healthcare settings: A global analysis. Infect. Control Hosp. Epidemiol. 2020, 41, 1196–1206. [Google Scholar] [CrossRef]
- Alhumaid, S.; Al Mutair, A.; Al Alawi, Z.; Alsuliman, M.; Ahmed, G.Y.; Rabaan, A.A.; Al-Tawfiq, J.A.; Al-Omari, A. Knowledge of infection prevention and control among healthcare workers and factors influencing compliance: A systematic review. Antimicrob. Resist. Infect. Control 2021, 10, 86. [Google Scholar] [CrossRef]
- Webster, P. Virtual health care in the era of COVID-19. Lancet 2020, 395, 1180–1181. [Google Scholar] [CrossRef]
- Budd, J.; Miller, B.S.; Manning, E.M.; Lampos, V.; Zhuang, M.; Edelstein, M.; Rees, G.; Emery, V.C.; Stevens, M.M.; Keegan, N.; et al. Digital technologies in the public-health response to COVID-19. Nat. Med. 2020, 26, 1183–1192. [Google Scholar] [CrossRef]
- Mroz, G.; Papoutsi, C.; Greenhalgh, T. ‘From disaster, miracles are wrought’: A narrative analysis of UK media depictions of remote GP consulting in the COVID-19 pandemic using Burke’s pentad. Med. Humanit. 2021, 47, 292–301. [Google Scholar] [CrossRef]
- Blandford, A.; Wesson, J.; Amalberti, R.; AlHazme, R.; Allwihan, R. Opportunities and challenges for telehealth within, and beyond, a pandemic. Lancet Glob. Health 2020, 8, e1364–e1365. [Google Scholar] [CrossRef]
- Utz, C.; Becker, S.; Schnitzler, T.; Farke, F.M.; Herbert, F.; Schaewitz, L.; Degeling, M.; Dürmuth, M. Apps against the spread: Privacy implications and user acceptance of COVID-19-related smartphone apps on three continents. In Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems, Yokohama, Japan, 8–13 May 2021; pp. 1–22. [Google Scholar]
- Wymant, C.; Ferretti, L.; Tsallis, D.; Charalambides, M.; Abeler-Dörner, L.; Bonsall, D.; Hinch, R.; Kendall, M.; Milsom, L.; Ayres, M.; et al. The epidemiological impact of the NHS COVID-19 app. Nature 2021, 594, 408–412. [Google Scholar] [CrossRef]
- Garrett, P.; Dennis, S. Australia Has All but Abandoned the COVIDSafe App in Favour of QR Codes (So Make Sure You Check In). Available online: https://theconversation.com/australia-has-all-but-abandoned-the-covidsafe-app-in-favour-of-qr-codes-so-make-sure-you-check-in-161880 (accessed on 25 November 2022).
- Arzt, S.; Poller, A.; Vallejo, G. Tracing Contacts With Mobile Phones to Curb the Pandemic: Topics and Stances in People’s Online Comments About the Official German Contact-Tracing App. In Proceedings of the Extended Abstracts of the 2021 CHI Conference on Human Factors in Computing Systems, Yokohama, Japan, 8–13 May 2021; pp. 1–7. [Google Scholar]
- Lu, X.; Reynolds, T.L.; Jo, E.; Hong, H.; Page, X.; Chen, Y.; Epstein, D.A. Comparing Perspectives Around Human and Technology Support for Contact Tracing. In Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems, Yokohama, Japan, 8–13 May 2021; pp. 1–15. [Google Scholar]
- Jarrom, D.; Elston, L.; Washington, J.; Prettyjohns, M.; Cann, K.; Myles, S.; Groves, P. Effectiveness of tests to detect the presence of SARS-CoV-2 virus, and antibodies to SARS-CoV-2, to inform COVID-19 diagnosis: A rapid systematic review. BMJ Evid.-Based Med. 2020, 1, 33–45. [Google Scholar] [CrossRef]
- Cobb, N.; Papali, A.; Pisani, L.; Schultz, M.J.; Ferreira, J.C. Pragmatic recommendations for infection prevention and control practices for healthcare facilities in low-and middle-income countries during the COVID-19 pandemic. Am. J. Trop. Med. Hyg. 2021, 104, 25. [Google Scholar] [CrossRef]
- Nomura, S.; Yoneoka, D.; Shi, S.; Tanoue, Y.; Kawashima, T.; Eguchi, A.; Matsuura, K.; Makiyama, K.; Ejima, K.; Taniguchi, T.; et al. An assessment of self-reported COVID-19 related symptoms of 227,898 users of a social networking service in Japan: Has the regional risk changed after the declaration of the state of emergency? Lancet Reg. Health-West. Pac. 2020, 1, 100011. [Google Scholar] [CrossRef]
- Parrella, A.; Dalton, C.B.; Pearce, R.; Litt, J.C.; Stocks, N. ASPREN surveillance system for influenza-like illness: A comparison with FluTracking and the National Notifiable Diseases Surveillance System. Aust. Fam. Physician 2009, 38, 932–936. [Google Scholar]
- Bourgeois, F.T.; Porter, S.C.; Valim, C.; Jackson, T.; Cook, E.F.; Mandl, K.D. The value of patient self-report for disease surveillance. J. Am. Med. Inform. Assoc. 2007, 14, 765–771. [Google Scholar] [CrossRef]
- Moss, R.; Zarebski, A.E.; Carlson, S.J.; McCaw, J.M. Accounting for healthcare-seeking behaviours and testing practices in real-time influenza forecasts. Trop. Med. Infect. Dis. 2019, 4, 12. [Google Scholar] [CrossRef]
- McDonald, S.A.; Van Den Wijngaard, C.C.; Wielders, C.C.; Friesema, I.H.; Soetens, L.; Paolotti, D.; Van Den Hof, S.; Van Hoek, A.J. Risk factors associated with the incidence of self-reported COVID-19-like illness: Data from a web-based syndromic surveillance system in the Netherlands. Epidemiol. Infect. 2021, 149, e129. [Google Scholar] [CrossRef]
- Adorni, F.; Prinelli, F.; Bianchi, F.; Giacomelli, A.; Pagani, G.; Bernacchia, D.; Rusconi, S.; Maggi, S.; Trevisan, C.; Noale, M.; et al. Self-reported symptoms of SARS-CoV-2 infection in a nonhospitalized population in Italy: Cross-sectional study of the EPICOVID19 web-based survey. JMIR Public Health Surveill. 2020, 6, e21866. [Google Scholar] [CrossRef]
- Judson, T.J.; Odisho, A.Y.; Young, J.J.; Bigazzi, O.; Steuer, D.; Gonzales, R.; Neinstein, A.B. Implementation of a digital chatbot to screen health system employees during the COVID-19 pandemic. J. Am. Med. Inform. Assoc. 2020, 27, 1450–1455. [Google Scholar] [CrossRef]
- Sudre, C.H.; Keshet, A.; Graham, M.S.; Joshi, A.D.; Shilo, S.; Rossman, H.; Murray, B.; Molten, E.; Klaser, K.; Canas, L.D.; et al. Anosmia, ageusia, and other COVID-19-like symptoms in association with a positive SARS-CoV-2 test, across six national digital surveillance platforms: An observational study. Lancet Digit. Health 2021, 3, e577–e586. [Google Scholar] [CrossRef]
- Menni, C.; Valdes, A.M.; Freidin, M.B.; Sudre, C.H.; Nguyen, L.H.; Drew, D.A.; Ganesh, S.; Varsavsky, T.; Cardoso, M.J.; Moustafa, J.S.E.S.; et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat. Med. 2020, 26, 1037–1040. [Google Scholar] [CrossRef]
- Izquierdo-Domínguez, A.; Rojas-Lechuga, M.; Chiesa-Estomba, C.; Calvo-Henríquez, C.; Ninchritz-Becerra, E.; Soriano-Reixach, M.; Poletti-Serafini, D.; Villarreal, I.M.; Maza-Solano, J.; Moreno-Luna, R.; et al. Smell and taste dysfunction in covid-19 is associated with younger age in ambulatory settings: A multicenter cross-sectional study. J. Investig. Allergol. Clin. Immunol. 2020, 30, 346–357. [Google Scholar] [CrossRef]
- Leung, G.M.; Quah, S.; Ho, L.M.; Ho, S.Y.; Hedley, A.J.; Lee, H.P.; Lam, T.H. A tale of two cities: Community psychobehavioral surveillance and related impact on outbreak control in Hong Kong and Singapore during the severe acute respiratory syndrome epidemic. Infect. Control Hosp. Epidemiol. 2004, 25, 1033–1041. [Google Scholar] [CrossRef]
- Johnson, E.J.; Hariharan, S. Public health awareness: Knowledge, attitude and behaviour of the general public on health risks during the H1N1 influenza pandemic. J. Public Health 2017, 25, 333–337. [Google Scholar] [CrossRef]
- Emanuel, E.J.; Persad, G.; Upshur, R.; Thome, B.; Parker, M.; Glickman, A.; Zhang, C.; Boyle, C.; Smith, M.; Phillips, J.P. Fair allocation of scarce medical resources in the time of Covid-19. N. Engl. J. Med. 2020, 382, 2049–2055. [Google Scholar] [CrossRef]
- Quigley, A.L.; Stone, H.; Nguyen, P.Y.; Chughtai, A.A.; MacIntyre, C.R. Estimating the burden of COVID-19 on the Australian healthcare workers and health system during the first six months of the pandemic. Int. J. Nurs. Stud. 2021, 114, 103811. [Google Scholar] [CrossRef]
- Nooraie, R.Y.; Shelton, R.C.; Fiscella, K.; Kwan, B.M.; McMahon, J.M. The pragmatic, rapid, and iterative dissemination and implementation (PRIDI) cycle: Adapting to the dynamic nature of public health emergencies. Health Res. Policy Syst. 2021, 19, 110. [Google Scholar] [CrossRef]
- Elwy, A.R.; Wasan, A.D.; Gillman, A.G.; Johnston, K.L.; Dodds, N.; McFarland, C.; Greco, C.M. Using formative evaluation methods to improve clinical implementation efforts: Description and an example. Psychiatry Res. 2020, 283, 112532. [Google Scholar] [CrossRef]
- Dopp, A.R.; Parisi, K.E.; Munson, S.A.; Lyon, A.R. Aligning implementation and user-centered design strategies to enhance the impact of health services: Results from a concept mapping study. Implement. Sci. Commun. 2020, 1, 173. [Google Scholar] [CrossRef] [PubMed]
- Gulbransen-Diaz, N.; Yoo, S.; Wang, A.P. Nurse, Give Me the News! Understanding Support for and Opposition to a COVID-19 Health Screening System. Int. J. Environ. Res. Public Health 2023, 20, 1164. [Google Scholar] [CrossRef]
- Kvale, S. Doing Interviews; SAGE Publications, Ltd.: Southend Oaks, CA, USA, 2007. [Google Scholar] [CrossRef]
- Galletta, A. The Semi-Structured Interview as a Repertoire of Possibilities. In Mastering the Semi-Structured Interview and Beyond: From Research Design to Analysis and Publication; NYU Press: New York, NY, USA, 2013. [Google Scholar]
- Mills, A.; Durepos, G.; Wiebe, E. Encyclopedia of Case Study Research; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2010. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Parker, C.; Fredericks, J.; Tomitsch, M.; Yoo, S. Towards adaptive height-aware public interactive displays. In Proceedings of the Adjunct Publication of the 25th Conference on User Modeling, Adaptation and Personalization, Bratislava, Slovakia, 9–12 July 2017; pp. 257–260. [Google Scholar]
- Parker, C.; Hoggenmueller, M.; Tomitsch, M. Design strategies for overcoming failures on public interactive displays. In Proceedings of the 7th ACM International Symposium on Pervasive Displays, Munich, Germany, 6–8 June 2018; pp. 1–7. [Google Scholar]
- Jabs, J.; Schwabe, A.; Wollkopf, A.; Gebel, B.; Stadelmaier, J.; Erdmann, S.; Radicke, F.; Grundmann, H.; Kramer, A.; Monsef, I.; et al. The role of routine SARS-CoV-2 screening of healthcare-workers in acute care hospitals in 2020: A systematic review and meta-analysis. BMC Infect. Dis. 2022, 22, 587. [Google Scholar] [CrossRef]
- Gifford, B.D.; Zammuto, R.F.; Goodman, E.A.; Hill, K.S. The relationship between hospital unit culture and nurses’ quality of work life/practitioner application. J. Healthc. Manag. 2002, 47, 13. [Google Scholar]
- Tong, A.; Sorrell, T.C.; Black, A.J.; Caillaud, C.; Chrzanowski, W.; Li, E.; Martinez-Martin, D.; McEwan, A.; Wang, R.; Motion, A.; et al. Research priorities for COVID-19 sensor technology. Nat. Biotechnol. 2021, 39, 144–147. [Google Scholar] [CrossRef]

| Age Group | Role | Study Group | |
|---|---|---|---|
| P1 | 18–25 | UG AIN | Interview |
| P2 | 18–25 | UG AIN | Interview |
| P3 | 18–25 | AIN | Interview |
| P4 | 26–30 | AIN | Interview |
| P5 | 31–40 | AIN | Interview |
| P6 | 18–25 | AIN | Online survey |
| P7 | 18–25 | AIN | Online survey |
| P8 | 18–25 | AIN | Online survey |
| P9 | 18–25 | UG AIN | Online survey |
| P10 | 18–25 | UG AIN | Online survey |
| P11 | 18–25 | UG AIN | Online survey |
| P12 | 18–25 | UG AIN | Online survey |
| P13 | 26–30 | EN | Online survey |
| P14 | 26–30 | EN | Online survey |
| P15 | 31–40 | EN | Online survey |
| P16 | 31–40 | Nurse manager | Online survey |
| P17 | 40+ | RN | Online survey |
| P18 | 40+ | Pre-admission nurse | Online survey |
| P19 | 40+ | Clinical nurse Specialist | Online survey |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoo, S.; Gulbransen-Diaz, N.; Parker, C.; Wang, A.P. Designing Digital COVID-19 Screening: Insights and Deliberations. Int. J. Environ. Res. Public Health 2023, 20, 3899. https://doi.org/10.3390/ijerph20053899
Yoo S, Gulbransen-Diaz N, Parker C, Wang AP. Designing Digital COVID-19 Screening: Insights and Deliberations. International Journal of Environmental Research and Public Health. 2023; 20(5):3899. https://doi.org/10.3390/ijerph20053899
Chicago/Turabian StyleYoo, Soojeong, Natalia Gulbransen-Diaz, Callum Parker, and Audrey P. Wang. 2023. "Designing Digital COVID-19 Screening: Insights and Deliberations" International Journal of Environmental Research and Public Health 20, no. 5: 3899. https://doi.org/10.3390/ijerph20053899
APA StyleYoo, S., Gulbransen-Diaz, N., Parker, C., & Wang, A. P. (2023). Designing Digital COVID-19 Screening: Insights and Deliberations. International Journal of Environmental Research and Public Health, 20(5), 3899. https://doi.org/10.3390/ijerph20053899









