Abstract
Background: We aimed to investigate the association between contextual-level social determinants of health (SDoH) and the use of novel antidiabetic drugs (ADD), including sodium-glucose cotransporter-2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP1a) for patients with type 2 diabetes (T2D), and whether the association varies across racial and ethnic groups. Methods: Using electronic health records from the OneFlorida+ network, we assembled a cohort of T2D patients who initiated a second-line ADD in 2015–2020. A set of 81 contextual-level SDoH documenting social and built environment were spatiotemporally linked to individuals based on their residential histories. We assessed the association between the contextual-level SDoH and initiation of SGTL2i/GLP1a and determined their effects across racial groups, adjusting for clinical factors. Results: Of 28,874 individuals, 61% were women, and the mean age was 58 (±15) years. Two contextual-level SDoH factors identified as significantly associated with SGLT2i/GLP1a use were neighborhood deprivation index (odds ratio [OR] 0.87, 95% confidence interval [CI] 0.81–0.94) and the percent of vacant addresses in the neighborhood (OR 0.91, 95% CI 0.85–0.98). Patients living in such neighborhoods are less likely to be prescribed with newer ADD. There was no interaction between race-ethnicity and SDoH on the use of newer ADD. However, in the overall cohort, the non-Hispanic Black individuals were less likely to use newer ADD than the non-Hispanic White individuals (OR 0.82, 95% CI 0.76–0.88). Conclusion: Using a data-driven approach, we identified the key contextual-level SDoH factors associated with not following evidence-based treatment of T2D. Further investigations are needed to examine the mechanisms underlying these associations.
1. Introduction
More than 100,000 individuals die from diabetes each year in the United States (US) [1]. Of these deaths, 60% are attributed to concurrent cardiovascular disease (CVD), with myocardial infarction being the most common cause [2]. Among the antidiabetic drugs (ADD) currently available on the US market, two relatively novel agents, sodium-glucose cotransporter-2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP1a), are associated with significant reductions in blood glucose levels and have been found particularly effective in reducing the risk of CVD in individuals with type 2 diabetes (T2D) [3]. In addition, these novel antidiabetic agents have been shown to associate with weight loss, reduced risk of hypoglycemia and cardiorenal protection, favorable benefits that are of great importance to patients with T2D [3]. The American Diabetes Association (ADA) recommends SGLT2i and GLP1a for patients with T2D who have CVD, heart failure, chronic kidney disease, or an increased risk of these conditions, regardless of their glycemic status [4,5].
However, the utilization of SGLT2i and GLP1a in real-world T2D patient populations is relatively low in the US compared to other ADD [6,7], especially among historically marginalized communities, such as racial and ethnic minority groups and individuals experiencing socioeconomic disadvantages. Data from commercial insurance and Medicare, for example, showed that Black patients were 10–20% less likely to receive newer ADD than White patients [7,8,9,10]. While such disparity can be explained overall by racial disparity as a distal cause, its proximal cause—the underlying mechanism whereby racial and ethnic groups have initiated SGLT2i/GLP1a—remains largely unknown.
In the past, research and clinical approaches centered on the individual-level have led improvements in self-management outcomes and reduction in cardiovascular risk among patients with T2D [11]. More recently, researchers have acknowledged the need to consider external factors, namely the social determinants of health (SDoH) to achieve the goal of sustainable improvement in diabetes outcomes [12]. SDoH refer to the various social, economic, and environmental factors, including access to healthcare, education, employment, housing, and social support that have an impact on people’s health, well-being, and quality of life [13]. Contextual-level SDoH refers to the broader social and built factors within community or region that influence health outcomes, and are increasingly recognized as a vital source of information to develop healthcare policies designed to improve population health management and value-based care [14,15]. Previous studies have demonstrated the association of contextual-level SDoH with geographic variation and diabetes risk [16]. However, minimal data exist on the extent to which contextual-level SDoH (e.g., residential segregation, food environment, and neighborhood walkability) may impact healthcare use, including initiating evidence-based treatment in T2D care [8]. A Dutch study published in 2012 examined the association of regional-level aging composition and socioeconomic status with spatial variation in ADD use but without a comprehensive evaluation of multiple contextual-level SDoH [17].
Given that race and ethnicity are social constructs [18], contextual-level SDoH can play important roles in the development of racial and ethnic disparities across geographic regions [19]. Therefore, understanding how contextual-level SDoH impact the adoption of these outcome-improving therapies in millions of Americans with T2D is imperative. Accordingly, this study aimed to examine the association between patients’ contextual-level SDoH and their initiation of the newer ADD, and how such associations may vary across racial and ethnic groups. With such empirical evidence, the racial disparity in SGLT2i/GLP1a utilization can be better understood, and relevant policymaking can be better guided.
2. Materials and Methods
2.1. Data Source and Study Population
This is a retrospective cohort study using data from the OneFlorida+ network, containing large collections of electronic health records (EHR) covering more than 19 million patients from Florida (~16.8 million), Georgia (~2.1 million), and Alabama (~9.1 thousand) [20]. We assembled a cohort of adults (i.e., aged ≥ 18) identified as having at least one inpatient or outpatient T2D diagnosis (using ICD-9 codes 250.x0 or 250.x2, or ICD-10 code E11) and ≥1 ADD prescription. The algorithm used to identify T2D has been validated in OneFlorida+ with a positive predictive value (PPV) > 94 [21] and is preferred over using only diagnosis codes, which can lead to misclassification error [22]. Among the T2D cohort, we identified individuals who initiated SGLT2i or GLP1a, or another second-line ADD (i.e., dipeptidyl-peptidase-4 inhibitors, sulfonylureas, thiazolidinediones, and basal insulin) in 2015–2020. The index date was the day of the first prescription of a second line ADD, defined as no use of the drug in three prior years. We restricted the study cohort by only including those individuals who had ≥ 2 inpatient or outpatient encounters per year in OneFlorida+ in the three years prior to the index date to obtain complete information for modelling.
2.2. Study Outcome and Covariates
The outcome was the initiation of a newer ADD (i.e., SGLT2i or GLP1a) versus another second-line drug. We collected baseline demographic and clinical information on or within the 3-year period prior to the index date, including age, sex, race-ethnicity (non-Hispanic White [NHW], non-Hispanic Black [NHB], Hispanic, and other), rurality (defined using linkage to rural–urban continuum codes [RUCC] based on patients’ residencies’ Federal Information Processing System [FIPS] county code and classified the rurality into three levels by the US Department of Agriculture’s (USDA) Economic Research Service: RUCC ≤ 3 as metropolitan; 3 < RUCC ≤ 7 as urban; and 7 < RUCC ≤ 9 as rural), primary payer (Medicare, Medicaid, private insurance, no insurance, and other), diabetes complications and comorbidities (such as cardiovascular disease and chronic kidney disease), co-medications (i.e., use of another ADD, antihypertensives, statins, and antidepressants), clinical presentation (most recent blood pressure and body mass index [BMI], identified in four categories: ≤25, 25–30, 30–100 kg/m2, or missing), and lab values (most recent hemoglobin A1c [HbA1c], identified in four categories: ≤7, 7–10, 10–21 mmHg, or missing). Clinical data were extracted from de-identified EHR records in the OneFlorida+ network.
2.3. Contextual-Level SDoH
We obtained data on built and social environment measures from six well-validated sources with different spatiotemporal scales, characterizing food access, walkability, vacant land, neighborhood disadvantage, social capital, crime and safety. All measures were spatiotemporally linked to each individual considering residential mobility during the study period. Area-weighted averages were first calculated according to a 250 m buffer around the centroid of each 9-digit ZIP code. Time-weighted averages were then calculated, accounting for each individual’s residential history.
Table 1 summarizes the contextual-level data sources and the corresponding spatiotemporal scales. A total of 43 food access measures at census tract level in 2015 and 2019 were obtained from USDA’s Food Access Research Atlas [23]. Walkability was assessed using the National Walkability Index developed by the US Environmental Protection Agency (EPA) [24], which assesses walkability on a scale from 1 to 20 for each census block group, with 1 indicating the least walkable and 20 the most walkable. Vacant land measures at the census-tract level from 2015 to 2019 were obtained from the US Department of Housing and Urban Development aggregated with US Postal Service administrative data [25] and a total of 18 measures that were available across all years were included. The neighborhood deprivation index (NDI), a socioeconomic status measure, was obtained at the census block group level based on data from the 2015 to 2019 American Community Survey (ACS). It yields information on the income, education, employment, and housing quality of a neighborhood and allows ranking by socioeconomic disadvantage [26]. In addition, ten social capital measures were constructed using the Census Business Pattern data based on the North American Industry Classification System (NAICS) codes [27] at the 5-digit ZIP code tabulation area (ZCTA5) level. Furthermore, eight county-level annual measures of crime and safety were obtained from the Uniform Crime Reporting Program from 2015 to 2019 [28]. A total of 81 SDoH measures were included in the analyses.

Table 1.
Summary of contextual-level SDoH measures.
2.4. Statistical Analysis
We conducted normalization transformations for all continuous contextual-level SDoH variables using the bestNormalize package in R, which implements several transformation methods, including log, square root, exponential, arcsinh, box cox, and Yeo-Johnson transformations [29]. The best transformation was determined based on Pearson P statistics. All continuous variables were also z-score standardized (mean = 0 and standard deviation = 1). All contextual-level SDoH factors and covariates of interest described above had missing values for <2% of the participants; Missing data for all contextual-level SDoH factors were imputed using the chained equations method of the MICE package in R. A variable was considered a predictor in the imputation model if its proportion of non-missing values among counties with missing values in the variable to be imputed was larger than 40% and they were correlated (i.e., with the absolute correlation value > 0.4) with the variable to be imputed or the probability of the variable being missing. We imputed a single dataset given the minimal impacts of the imputation procedure due to the large sample size and a small fraction of missing data. Missing information on BMI and HbA1c were not imputed and maintained as a separate category.
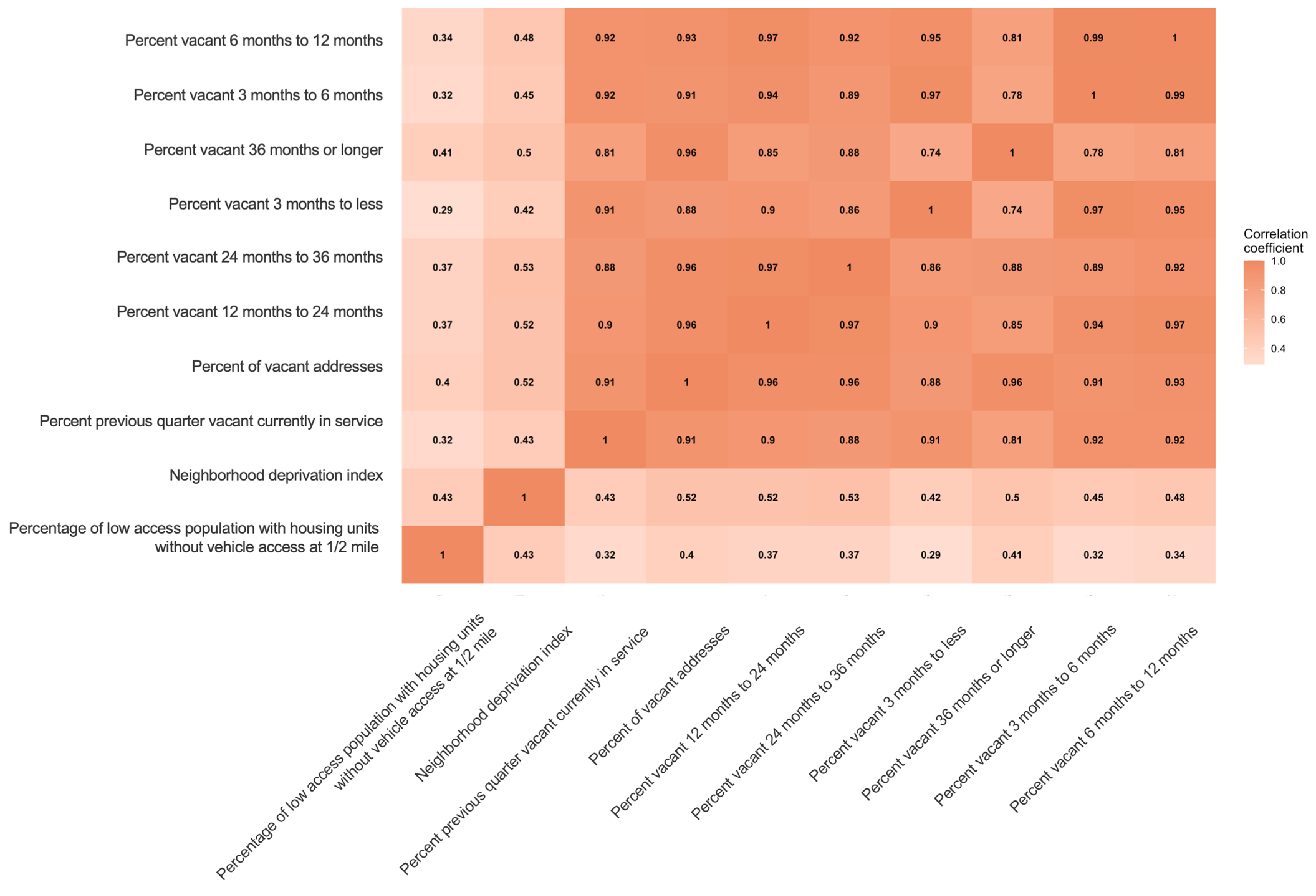
We used a two-phase approach to identify key contextual-level associated with initiation of SGTL2i/GLP1a versus other second-line ADD [30,31]. In Phase 1, we randomly split the data into a 50% discovery set and a 50% replication set. We considered all the 83 contextual-level SDoH for associations with newer ADD initiation after accounting for multiple comparisons. We built multivariable logistic regression models for each contextual-level factor after adjusting for demographics, urbanicity, diabetes complications, co-medications, clinical presentation, and primary payer. To account for the multiple testing, the Benjamin-Hochberg procedure was used to control the false discovery rate (FDR) at 5% [32]. A variable was considered significant if it had an FDR-adjusted p-value (or q-value) < 0.05 in both the discovery and the replication sets. A correlation heatmap was generated to show the pairwise Pearson correlations of the variables retained from Phase 1. Variables from highly correlated pairs (with the absolute value of correlation coefficients > 0.6) were removed to avoid collinearity between variables [33].
In Phase 2, we used a multivariable logistic regression model including all significant variables identified from Phase 1 as well as all the demographic and clinical information, including age, sex, primary payer, BMI, HbA1c, type of residence, cardiovascular disease, chronic kidney disease, use of insulin and non-insulin antidiabetic medications to estimate the effect sizes. Adjusted odds ratios (aOR) and 95% confidence intervals (CI) were reported.
For the key contextual-level SDoH identified using the two-phase approach, we dichotomized them using the 80th percentile from the key variables as the cutoff. A Higher numeric value in NDI and percent of vacant addresses indicates a neighborhood that is more disadvantaged in socioeconomic profile and has a larger vacancy in addresses. Therefore, we defined neighborhoods with the top 20th percentile in NDI as more deprived neighborhoods, and neighborhoods with the top 20th percentile in percent of vacant addresses as neighborhoods with more occupancy. We applied multilevel logistic regression and adjusted for demographic and clinical characteristics to determine the effect variation by race-ethnicity of key contextual-level SDoH in association with newer ADD initiation.
Analyses were performed using the R statistical software (version 3.6.1; R Development Core Team) and SAS 9.4 (Cary, North Carolina). The study was approved by the Institutional Review Board at the University of Florida (IRB202102283).
3. Results
3.1. Descriptive Analysis
Our final analysis comprised 28,874 patients in the cohort. Table 2 highlights the demographic and clinical characteristics of the study population by race and ethnicity. Overall, the mean age was 58 (±15) years, and 61% were women. The majority of the patients were enrolled in public insurance programs such as Medicare (37%) and Medicaid (35%). Compared with NHW patients, NHB patients were younger (54.6 vs. 58.5 years, p < 0.01) and more likely to be covered by Medicaid (41% vs. 28%, p < 0.01), while Hispanics and patients of other races were older (mean age of Hispanics: 61 years, other race/ethnicity: 60 years), and more likely to be women. Of our cohort, 11,649 patients (40%) had initiated the newer ADD (i.e., SGLT2i or GLP1a). NHW and patients of other races/ethnicities were more likely to have initiated a newer ADD versus another second-line ADD compared to NHB (NHW and other race/ethnicity: both 44%, NHB: 38%, Hispanics: 35%, p < 0.01)

Table 2.
Patient Characteristics, by race/ethnicity.
3.2. Selection of Contextual-Level SDoH
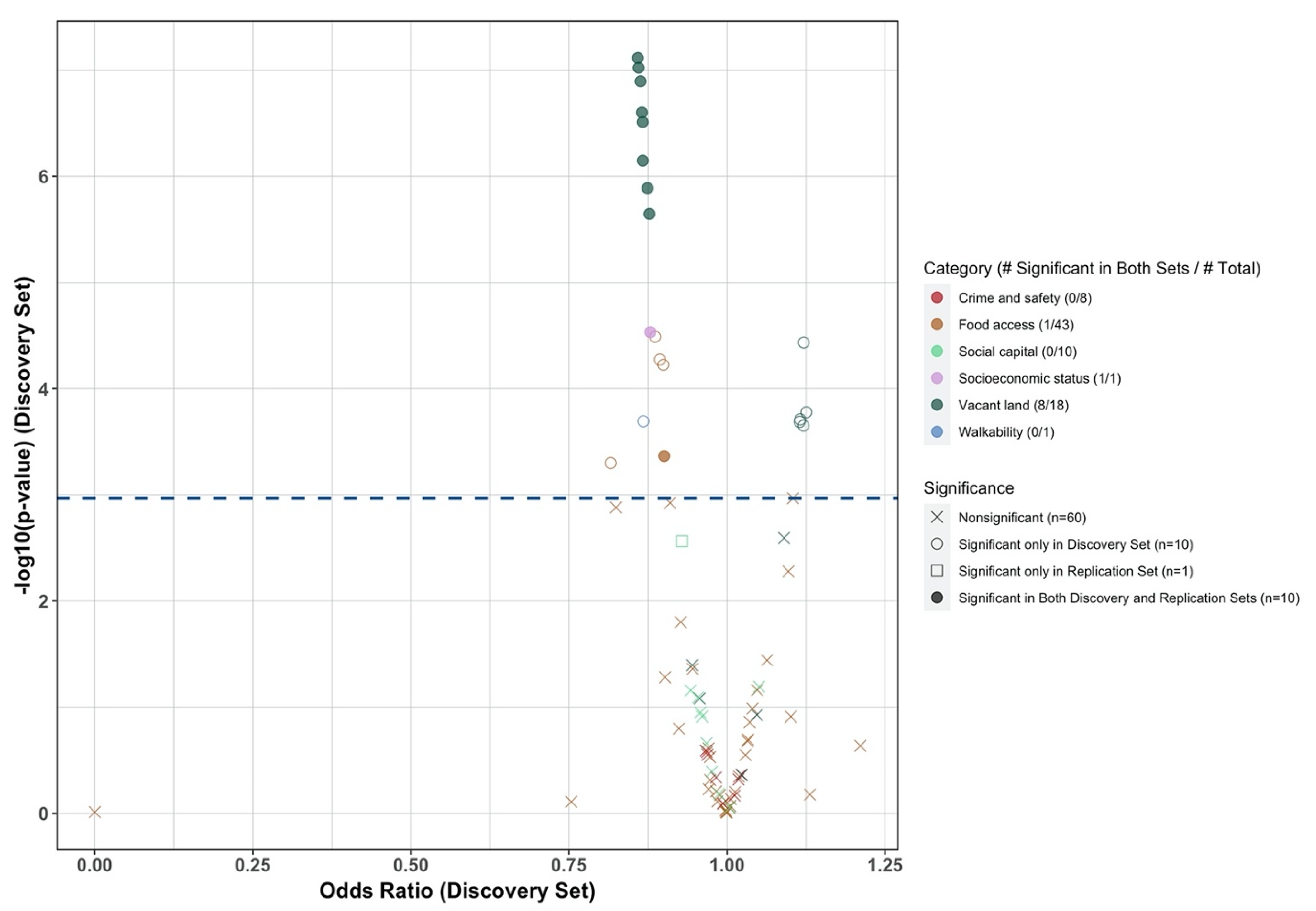
Figure 1 is a volcano plot summarizing the results from Phase 1. After accounting for multiple comparisons using the Benjamin Hochberg procedure, a total of 20 and 11 variables were significantly associated with novel ADD use in the discovery and replication sets, respectively. Among them, ten variables from three categories were significant in both the discovery and replication sets, including the NDI, percentage of low food access (percentage without vehicle access living a half-mile from supply, a food access measure variable), and eight variables documenting the vacant housing in the neighborhood. All ten variables were associated with a lower likelihood of initiating newer ADD (with OR < 1, Figure 1). We observed high correlations among the eight variables documenting vacant land measures (all pairwise correlation coefficients > 0.6, Appendix A, Figure A1). Therefore, we kept only one variable, the percent of vacant addresses in the Phase 2 analysis, as this variable is a more comprehensive measure than the others in the category.
Figure 1.
Volcano plot of the results from phase 1 of the two-phase approach.
In Phase 2 analysis, the NDI, percentage without vehicle access living a half mile from supply, and percent of vacant addresses, were simultaneously included in a multivariable logistic regression model after adjusting for baseline demographic and clinical information. Two variables—NDI and percent of vacant addresses—remained statistically significant in the multivariable model. Therefore, our two-phase approach identified two contextual-level SDoH that were significantly associated with a lower likelihood of newer ADD initiation, which are neighborhoods with a higher degree of deprivation and neighborhoods with more vacant housing (Table 3).

Table 3.
Significant social determinants of health variables associated with the use newer antidiabetic drugs identified by the two-phase approach.
3.3. Association of Contextual-Level SDoH and New ADD Initiation across Racial and Ethnic Groups
Table 4 shows the results from multivariable logistic regression of binary key contextual-level SDoH variables in association with the novel ADD initiation in the overall cohort and in each racial-ethnic subgroup. In the overall cohort, NHB were significantly less likely to use newer ADD than NHW (aOR 0.82, 95% CI: 0.76–0.88, p < 0.01) after adjusting for all the covariates listed above. Patients living in a more deprived neighborhood were associated with a significantly lower likelihood of initiating a newer ADD than the remaining patients (aOR 0.87, 95% CI: 0.81–0.94, p < 0.01). Patients living in a neighborhood with more occupancy were less likely to initiate a newer ADD (aOR: 0.91, 95% CI: 0.87–0.95, p < 0.01) than their counterparts. We observed similar trends in racial and ethnic subgroups, and no significant interaction of race/ethnicity and contextual-level SDoH was detected.

Table 4.
Results from multivariate logistic regressions (with binary contextual-level social determinants of health).
4. Discussion
SDoH are not only experienced by individuals but also exert influence at the community level. Community-level information about the neighborhoods in which individuals live, learn, work, and play is recognized as the community’s vital signs [18], conveying contextual-level social deprivation and impacting health risks. Our study is unique in linking a set of contextual-level factors documenting social and built environments to extensive collections of EHR data via individuals’ residential histories in a cohort of real-world patients with T2D. Using a data-driven approach, we determined the key contextual-level SDoH factors associated with evidence-based treatment for T2D. After accounting for multiple testing and high correlations among the exposures, two contextual-level SDoH variables characterizing the neighborhood deprivation and vacant housing were identified as being significantly associated with individuals’ limited initiation of newer ADD known to improve cardiorenal outcomes of T2D. These results provide evidence supporting a spatially explicit data-driven approach in developing interventions to address disparities in initiation of T2D treatment.
Increasing evidence has demonstrated an association between neighborhood factors and diabetes outcomes. For example, a more disadvantaged socioeconomic status, poorer food access and built environment (e.g., walkability, recreational facilities), and less social cohesion are associated with the risk of T2D [34,35,36,37]. Additionally, lower neighborhood socioeconomic status was significantly associated with worsening physical and mental health status and poor glycemic control among patients with diabetes [38,39]. However, very few studies have examined whether contextual-level SDoH may influence healthcare quality, such as the initiation of evidence-based treatment. A study conducted using claims data found that contextual-level SDoH, such as poor food access, weak social support, and lack of a healthy built environment, were significantly associated with non-adherence to antihypertensive medication [40]. A randomized trial that enrolled 749 Mexican–American patients at a university-affiliated clinic showed that patients who lived in neighborhoods with greater deprivation were much less likely to adhere to their ADD protocols than those living in neighborhoods in the next higher quartile on the deprivation index [41]. In a US-based study examining the association between neighborhood social environment factors and adherence to oral antidiabetic medications, residents living in neighborhoods with high sociability were more likely to adhere to ADD regimens than their counterparts in less sociable surroundings [42].
The current study found that the NDI, an index documenting neighborhood deprivation, was significantly associated with newer ADD initiation. NDI is a composite indicator of contextual-level socioeconomic disadvantages in four areas beyond the strictly specified healthcare setting: income, housing quality, employment, and education. Previous studies have documented the association between neighborhood deprivation, attributed to income, employment, and education, and the quality of diabetes care, reporting that patients living in more deprived neighborhoods were significantly less likely to obtain high-quality diabetes care [7,8,10]. At an individual level, a lack of income and unemployment can create barriers to accessing high-quality diabetes care, while a lack of education has been linked to poor health literacy [43]. At the contextual level, the role of political context could also shape socioeconomic factors, and this interplay could result in unequal resource distribution and structural inequalities in the neighborhoods that perpetuate health disparities [44]. Therefore, individuals with a low socioeconomic profile at the contextual level may face barriers to the use of novel ADD treatment.
The consequences of vacant housing can extend far beyond just an empty space. Vacant land usually is an indicator of population out-migration and disinvestment. In addition to the increased risk of violence and crime [45], vacant housing often leads to a reduction in business and employment, therefore resulting in a lack of community resources, as well as access to essential facilities such as food, medical and social support services [46,47], further exacerbating health disparities in these communities. This lack of resources can have far-reaching consequences on the health and well-being of individuals residing in these areas. Previous studies have shown that empty lots are associated with higher levels of chronic stress and fewer social interactions, and thus resulting in unfavorable health outcomes [25]. In our study, individuals living in a neighborhood with more vacant addresses had lower access to the newer ADD, which could be explained by the lack of access to high-quality diabetes care. It is essential to address the issue of vacant housing and provide necessary resources and support to such disadvantaged communities. Developing innovative strategies, such as mobile medical clinics, have been effective in serving the requirements of medically vulnerable populations, such as the urban poor [48] and populations without stable housing [49], for whom accessibility to fixed healthcare is limited due to the lack of facilities and meager financial resources. MMCs could improve access to care by overcoming geographic and social restrictions, such as neighborhoods with many vacant addresses, which traditional, permanent healthcare facilities must avoid, thus addressing health inequities and mitigating social obstacles to healthcare.
Despite having a disproportionately higher risk of cardiovascular disease, patients from racial and ethnic minority groups have a lower probability of initiating guideline-based therapies that improve their outcomes, including the uptake of new ADD [9,50]. It is suggested that differences might be driven by the disadvantages in insurance coverage and poor socioeconomic status among these racial and ethnic subgroups, and it has been acknowledged in several studies that Medicare Advantage enrollees are less likely to initiate newer ADD than commercial insured patients [7,8,9]. However, in our study, the racial and ethnic disparities in new ADD use persisted after adjusting not only for insurance, but also for NDI, a proxy to socioeconomic status. This represents that such disparity was not driven solely by insurance factors and socioeconomic status. However, we did not identify a significant interaction between race/ethnicity and key contextual-level SDoH in association with initiating newer ADD. While it is possible that the interaction lies elsewhere and was not captured using the two-phase method presented in this study, our findings highlight the structural–environmental factors that drive inequities in the use of evidence-based treatment, independent of race and ethnicity.
Our study has several limitations. First, our study does not exclude patients with gestational diabetes, and there is a possibility of misclassification for individuals with pregnancy and gestational diabetes but not diagnosed by physicians. Second, the two-phase approach we used did not consider non-linear associations and potential interactions. Generalize additive model could be considered in future work to account for the non-linear relationships among key contextual-level SDoH in association with the study outcome. Additionally, Bayesian kernel machine regression and Bayesian multiple index models can capture the complex interrelations among contextual-level SDoH. Third, although many contextual-level SDoH have been included to characterize the social and built environment, this list is not exhaustive. Continuing efforts are needed to improve the measurement of the contextual-level SDoH further. Fourth, our study cohort was constructed using EHR data, and we cannot completely preclude the prevalence of users of second-line ADD. However, we extended our baseline to three years and restricted individuals who had at least two encounters per year to capture prescription and medical information, which largely eliminated the cases of prevalent users. In addition, regarding the association between individual-level factors and newer ADD initiation, our results were consistent with prior studies using claims data [50], suggesting the validity of the current study’s findings. Finally, participants included in this study were limited to those who received care at one or more sites included in the OneFlorida+ Clinical Research Network. Thus, our results may not be generalizable to those who did not receive healthcare at one of these facilities.
5. Conclusions
In a cohort of T2D patients from a statewide network of EHR, we identified two key contextual-level SDoH factors associated with limited use of new ADD: individuals living in neighborhoods with a higher deprivation index and more vacant addresses were less likely to initiate newer ADD compared with those living in less deprived and more fully occupied neighborhoods. Although the specific mechanisms underlying these associations require further investigation, our findings have contributed to the growing body of evidence of the neighborhood-level factors, their interplay with race across various spatial contexts, and their circumstances on evidence-based healthcare. It is crucial to gain a comprehensive understanding of these complex factors to develop effective strategies for addressing health equities and promoting evidence-based treatment in T2D care.
Author Contributions
Conceptualization, J.G.; methodology, H.H.; formal analysis, Y.L. and Y.Z.; resources, W.T.D.; writing—initial draft, Y.L.; writing—review and editing, Y.G., J.X., N.L., W.-H.C. and E.A.S.; supervision: J.B. All authors have read and agreed to the published version of the manuscript.
Funding
It is funded by NIH NIDDK R01DK133465.
Institutional Review Board Statement
The study was approved by the Institutional Review Board at the University of Florida (IRB202100024).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
Figure A1.
Correlation heatmap of significant SDoH variables from Phase 1 of the two-phase approach.
Figure A1.
Correlation heatmap of significant SDoH variables from Phase 1 of the two-phase approach.
References
- Murphy, S.L.; Kochanek, K.D.; Xu, J.; Arias, E. Mortality in the United States, 2020; NCHS Data Briefs; National Center for Health Statistics: Hyattsville, MD, USA, 2021. [Google Scholar]
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2020 Update: A Report From the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef] [PubMed]
- Palmer, S.C.; Tendal, B.; Mustafa, R.A.; Vandvik, P.O.; Li, S.; Hao, Q.; Tunnicliffe, D.; Ruospo, M.; Natale, P.; Saglimbene, V.; et al. Sodium-glucose cotransporter protein-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes: Systematic review and network meta-analysis of randomised controlled trials. BMJ 2021, 372, m4573. [Google Scholar] [CrossRef]
- American Diabetes Association. 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021, 44, S111–S124. [Google Scholar] [CrossRef]
- Writing Committee; Das, S.R.; Everett, B.M.; Birtcher, K.K.; Brown, J.M.; Januzzi, J.L.; Kalyani, R.R.; Kosiborod, M.; Magwire, M.; Morris, P.B.; et al. 2020 Expert Consensus Decision Pathway on Novel Therapies for Cardiovascular Risk Reduction in Patients with Type 2 Diabetes a Report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 2020, 76, 1117–1145. [Google Scholar] [CrossRef]
- Mahtta, D.; Ramsey, D.J.; Lee, M.T.; Chen, L.; Al Rifai, M.; Akeroyd, J.M.; Vaughan, E.M.; Matheny, M.E.; Santo, K.R.D.E.; Navaneethan, S.D.; et al. Utilization Rates of SGLT2 Inhibitors and GLP-1 Receptor Agonists and Their Facility-Level Variation Among Patients with Atherosclerotic Cardiovascular Disease and Type 2 Diabetes: Insights from the Department of Veterans Affairs. Diabetes Care 2022, 45, 372–380. [Google Scholar] [CrossRef]
- Eberly, L.A.; Yang, L.; Eneanya, N.D.; Essien, U.; Julien, H.; Nathan, A.S.; Khatana, S.A.M.; Dayoub, E.J.; Fanaroff, A.C.; Giri, J.; et al. Association of Race/Ethnicity, Gender, and Socioeconomic Status With Sodium-Glucose Cotransporter 2 Inhibitor Use Among Patients With Diabetes in the US. JAMA Netw. Open 2021, 4, e216139. [Google Scholar] [CrossRef] [PubMed]
- McCoy, R.G.; Dykhoff, H.J.; Sangaralingham, L.; Ross, J.S.; Karaca-Mandic, P.; Montori, V.M.; Shah, N.D. Adoption of New Glucose-Lowering Medications in the U.S.—The Case of SGLT2 Inhibitors: Nationwide Cohort Study. Diabetes Technol. Ther. 2019, 21, 702–712. [Google Scholar] [CrossRef] [PubMed]
- Eberly, L.A.; Yang, L.; Essien, U.R.; Eneanya, N.D.; Julien, H.M.; Luo, J.; Nathan, A.S.; Khatana, S.A.M.; Dayoub, E.J.; Fanaroff, A.C.; et al. Racial, Ethnic, and Socioeconomic Inequities in Glucagon-Like Peptide-1 Receptor Agonist Use Among Patients With Diabetes in the US. JAMA Health Forum 2021, 2, e214182. [Google Scholar] [CrossRef]
- Elhussein, A.; Anderson, A.; Bancks, M.P.; Coday, M.; Knowler, W.C.; Peters, A.; Vaughan, E.M.; Maruthur, N.M.; Clark, J.M.; Pilla, S.; et al. Racial/ethnic and socioeconomic disparities in the use of newer diabetes medications in the Look AHEAD study. Lancet Reg. Health. Am. 2022, 6, 100111. [Google Scholar] [CrossRef]
- Davis, J.; Fischl, A.H.; Beck, J.; Browning, L.; Carter, A.; Condon, J.E.; Dennison, M.; Francis, T.; Hughes, P.J.; Jaime, S.; et al. 2022 National Standards for Diabetes Self-Management Education and Support. Diabetes Spectr. 2022, 35, 137–149. [Google Scholar] [CrossRef]
- Walker, R.J.; Smalls, B.L.; Campbell, J.A.; Strom Williams, J.L.; Egede, L.E. Impact of social determinants of health on outcomes for type 2 diabetes: A systematic review. Endocrine 2014, 47, 29–48. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Social Determinants of Health—Healthy People 2030. Available online: https://health.gov/healthypeople/priority-areas/social-determinants-health/ (accessed on 14 February 2023).
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.E.; Woerle, H.J.; et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N. Engl. J. Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef] [PubMed]
- Inzucchi, S.E.; Zinman, B.; Fitchett, D.; Wanner, C.; Ferrannini, E.; Schumacher, M.; Schmoor, C.; Ohneberg, K.; Johansen, O.E.; George, J.T.; et al. How Does Empagliflozin Reduce Cardiovascular Mortality? Insights From a Mediation Analysis of the EMPA-REG OUTCOME Trial. Diabetes Care 2017, 41, 356–363. [Google Scholar] [CrossRef]
- Kauhl, B.; Schweikart, J.; Krafft, T.; Keste, A.; Moskwyn, M. Do the risk factors for type 2 diabetes mellitus vary by location? A spatial analysis of health insurance claims in Northeastern Germany using kernel density estimation and geographically weighted regression. Int. J. Health Geogr. 2016, 15, 38. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, A.; Janssen, F.; Bakker, M.D.; Bos, J.; Lub, R.; Wissen, L.J.G.V.; Hak, E. Using Spatial Analysis to Predict Health Care Use at the Local Level: A Case Study of Type 2 Diabetes Medication Use and Its Association with Demographic Change and Socioeconomic Status. PLoS ONE 2013, 8, e72730. [Google Scholar] [CrossRef]
- Bazemore, A.W.; Cottrell, E.K.; Gold, R.; Hughes, L.S.; Phillips, R.L.; Angier, H.; Burdick, T.E.; Carrozza, M.A.; DeVoe, J.E. “Community vital signs”: Incorporating geocoded social determinants into electronic records to promote patient and population health. J. Am. Med. Inform. Assoc. 2016, 23, 407–412. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Naik, A.D.; Dodson, J.A. Moving From Disease-Centered to Patient Goals–Directed Care for Patients with Multiple Chronic Conditions: Patient Value-Based Care. JAMA Cardiol. 2016, 1, 9. [Google Scholar] [CrossRef]
- OneFlorida+ Clinical Research Network. Data Summary—OneFlorida. Available online: https://onefloridaconsortium.org/data/ (accessed on 5 May 2022).
- Wiese, A.D.; Roumie, C.L.; Buse, J.B.; Guzman, H.; Bradford, R.; Zalimeni, E.; Knoepp, P.; Morris, H.L.; Donahoo, W.T.; Fanous, N.; et al. Performance of a computable phenotype for identification of patients with diabetes within PCORnet: The Patient-Centered Clinical Research Network. Pharmacoepidemiol. Drug Saf. 2019, 28, 632–639. [Google Scholar] [CrossRef]
- Shivade, C.; Raghavan, P.; Fosler-Lussier, E.; Embi, P.J.; Elhadad, N.; Johnson, S.B.; Lai, A.M. A review of approaches to identifying patient phenotype cohorts using electronic health records. J. Am. Med. Inform. Assoc. 2014, 21, 221–230. [Google Scholar] [CrossRef]
- U.S. Department of Agriculture Economic Research Service. USDA ERS—Food Access Research Atlas. Available online: https://www.ers.usda.gov/data-products/food-access-research-atlas/ (accessed on 2 December 2022).
- Thomas, J.; Zeller, L. National Walkability Index User Guide and Methodology; Prot. Agency: Washington, DC, USA, 2017. [Google Scholar]
- Garvin, E.; Branas, C.; Keddem, S.; Sellman, J.; Cannuscio, C. More Than Just An Eyesore: Local Insights and Solutions on Vacant Land and Urban Health. J. Urban Health 2013, 90, 412–426. [Google Scholar] [CrossRef]
- Messer, L.C.; Laraia, B.A.; Kaufman, J.S.; Eyster, J.; Holzman, C.; Culhane, J.; Elo, I.; Burke, J.G.; O’Campo, P. The development of a standardized neighborhood deprivation index. J. Urban Health 2006, 83, 1041–1062. [Google Scholar] [CrossRef] [PubMed]
- Rupasingha, A.; Goetz, S.J.; Freshwater, D. The production of social capital in US counties. J. Socio-Econ. 2006, 35, 83–101. [Google Scholar] [CrossRef]
- Barnett-Ryan, C. Introduction to the uniform crime reporting program. In Understanding Crime Statistics: Revisiting the Divergence of the NCVS and the UCR; Cambridge University Press: Cambridge, UK, 2007; pp. 55–89. [Google Scholar]
- Peterson, R.A. Finding Optimal Normalizing Transformations via best Normalize. R J. 2021, 13, 310–329. [Google Scholar] [CrossRef]
- Hu, H.; Zhao, J.; Savitz, D.A.; Prosperi, M.; Zheng, Y.; Pearson, T.A. An external exposome-wide association study of hypertensive disorders of pregnancy. Environ. Int. 2020, 141, 105797. [Google Scholar] [CrossRef]
- Agier, L.; Portengen, L.; Chadeau-Hyam, M.; Basagaña, X.; Giorgis-Allemand, L.; Siroux, V.; Robinson, O.; Vlaanderen, J.; González Juan, R.; Nieuwenhuijsen Mark, J.; et al. A Systematic Comparison of Linear Regression–Based Statistical Methods to Assess Exposome-Health Associations. Environ. Health Perspect. 2016, 124, 1848–1856. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B (Methodol.) 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Vatcheva, K.P.; Lee, M.; McCormick, J.B.; Rahbar, M.H. Multicollinearity in Regression Analyses Conducted in Epidemiologic Studies. Epidemiology 2016, 6, 227. [Google Scholar] [CrossRef] [PubMed]
- Christine, P.J.; Auchincloss, A.H.; Bertoni, A.G.; Carnethon, M.R.; Sánchez, B.N.; Moore, K.; Adar, S.D.; Horwich, T.B.; Watson, K.E.; Diez Roux, A.V. Longitudinal Associations Between Neighborhood Physical and Social Environments and Incident Type 2 Diabetes Mellitus. JAMA Intern. Med. 2015, 175, 1311. [Google Scholar] [CrossRef]
- Kanchi, R.; Lopez, P.; Rummo, P.E.; Lee, D.C.; Adhikari, S.; Schwartz, M.D.; Avramovic, S.; Siegel, K.R.; Rolka, D.B.; Imperatore, G.; et al. Longitudinal Analysis of Neighborhood Food Environment and Diabetes Risk in the Veterans Administration Diabetes Risk Cohort. JAMA Netw. Open 2021, 4, e2130789. [Google Scholar] [CrossRef]
- Mcdoom, M.M.; Cooper, L.A.; Hsu, Y.-J.; Singh, A.; Perin, J.; Thornton, R.L.J. Neighborhood Environment Characteristics and Control of Hypertension and Diabetes in a Primary Care Patient Sample. J. Gen. Intern. Med. 2020, 35, 1189–1198. [Google Scholar] [CrossRef]
- Gebreab, S.Y.; Hickson, D.A.; Sims, M.; Wyatt, S.B.; Davis, S.K.; Correa, A.; Diez-Roux, A.V. Neighborhood social and physical environments and type 2 diabetes mellitus in African Americans: The Jackson Heart Study. Health Place 2017, 43, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Tabaei, B.P.; Rundle, A.G.; Wu, W.Y.; Horowitz, C.R.; Mayer, V.; Sheehan, D.M.; Chamany, S. Associations of Residential Socioeconomic, Food, and Built Environments with Glycemic Control in Persons with Diabetes in New York City From 2007–2013. Am. J. Epidemiol. 2018, 187, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Gary-Webb, T.L.; Baptiste-Roberts, K.; Pham, L.; Wesche-Thobaben, J.; Patricio, J.; Pi-Sunyer, F.X.; Brown, A.F.; Jones-Corneille, L.; Brancati, F.L. Neighborhood Socioeconomic Status, Depression, and Health Status in the Look AHEAD (Action for Health in Diabetes) Study. BMC Public Health 2011, 11, 349. [Google Scholar] [CrossRef]
- Donneyong, M.M.; Chang, T.-J.; Jackson, J.W.; Langston, M.A.; Juarez, P.D.; Sealy-Jefferson, S.; Lu, B.; Im, W.; Valdez, R.B.; Way, B.M.; et al. Structural and Social Determinants of Health Factors Associated with County-Level Variation in Non-Adherence to Antihypertensive Medication Treatment. Int. J. Environ. Res. Public Health 2020, 17, 6684. [Google Scholar] [CrossRef] [PubMed]
- Billimek, J.; August, K.J. Costs and beliefs: Understanding individual- and neighborhood-level correlates of medication nonadherence among Mexican Americans with type 2 diabetes. Health Psychol. 2014, 33, 1602–1605. [Google Scholar] [CrossRef]
- McClintock, H.F.d.V.; Wiebe, D.J.; O’Donnell, A.J.; Morales, K.H.; Small, D.S.; Bogner, H.R. Neighborhood Social Environment and Patterns of Adherence to Oral Hypoglycemic Agents Among Patients With Type 2 Diabetes Mellitus. Fam. Community Health 2015, 38, 169–179. [Google Scholar] [CrossRef]
- Schillinger, D.; Grumbach, K.; Piette, J.; Wang, F.; Osmond, D.; Daher, C.; Palacios, J.; Sullivan, G.D.; Bindman, A.B. Association of health literacy with diabetes outcomes. JAMA 2002, 288, 475–482. [Google Scholar] [CrossRef]
- Diez Roux, A.V.; Mair, C. Neighborhoods and health. Ann. N. Y. Acad. Sci. 2010, 1186, 125–145. [Google Scholar] [CrossRef]
- Hohl, B.C.; Kondo, M.C.; Kajeepeta, S.; MacDonald, J.M.; Theall, K.P.; Zimmerman, M.A.; Branas, C.C. Creating Safe and Healthy Neighborhoods with Place-Based Violence Interventions. Health Aff. 2019, 38, 1687–1694. [Google Scholar] [CrossRef]
- Cole, M.B.; Nguyen, K.H. Unmet social needs among low-income adults in the United States: Associations with health care access and quality. Health Serv. Res. 2020, 55, 873–882. [Google Scholar] [CrossRef]
- Titus, S.K.; Kataoka-Yahiro, M. A Systematic Review of Barriers to Access-to-Care in Hispanics With Type 2 Diabetes. J. Transcult. Nurs. 2019, 30, 280–290. [Google Scholar] [CrossRef] [PubMed]
- Daiski, I. The Health Bus: Healthcare for Marginalized Populations. Policy Politics Nurs. Pract. 2005, 6, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Whelan, C.; Chambers, C.; Chan, M.; Thomas, S.; Ramos, G.; Hwang, S.W. Why Do Homeless People Use a Mobile Health Unit in a Country With Universal Health Care? J. Prim. Care Community Health 2010, 1, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Gabriel, N.; Korytkowski, M.; Hernandez, I.; Gellad, W.F. Association of formulary restrictions and initiation of an SGLT2i or GLP1-RA among Medicare beneficiaries with type 2 diabetes. Diabetes Res. Clin. Pract. 2022, 187, 109855. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).