Characteristics of Patients Who Complete Suicide and Suicide Attempts While Undergoing Treatment in Norway: Findings from Compensation Claims Records
Abstract
1. Introduction
2. Materials and Methods
2.1. Measures
2.2. Procedures and Participants
2.3. Interrater-Reliability Analysis
2.4. Data Analytic Procedures
3. Results
3.1. Descriptive Results
3.2. Tests of Independence
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- The World Health Organization. Suicide. Available online: https://www.who.int/data/gho/data/themes/mental-health (accessed on 9 January 2023).
- Mellesdal, L.; Mehlum, L.; Wentzel-Larsen, T.; Kroken, R.; Arild Jørgensen, H. Suicide risk and acute psychiatric readmissions: A prospective cohort study. Psychiatr. Serv. 2010, 61, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Myklebust, L.H.; Sørgaard, K.; Røtvold, K.; Wynn, R. Factors of importance to involuntary admission. Nord. J. Psychiatry 2012, 66, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Wynn, R. Involuntary admission in Norwegian adult psychiatric hospitals: A systematic review. Int. J. Ment. Health Syst. 2018, 12, 10. [Google Scholar] [CrossRef] [PubMed]
- Vermeulen, J.M.; Doedens, P.; Cullen, S.W.; van Tricht, M.J.; Hermann, R.; Frankel, M.; de Haan, L.; Marcus, S.C. Predictors of adverse events and medical errors among adult inpatients of psychiatric units of acute care general hospitals. Psychiatr. Serv. 2018, 69, 1087–1094. [Google Scholar] [CrossRef] [PubMed]
- Marcus, S.C.; Hermann, R.C.; Frankel, M.R.; Cullen, S.W. Safety of psychiatric inpatients at the Veterans Health Administration. Psychiatr. Serv. 2017, 69, 204–210. [Google Scholar] [CrossRef]
- DeJong, T.M.; Overholser, J.C.; Stockmeier, C.A. Apples to oranges?: A direct comparison between suicide attempters and suicide completers. J. Affect. Disord. 2010, 124, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Giner, L.; Blasco-Fontecilla, H.; Mercedes Perez-Rodriguez, M.; Garcia-Nieto, R.; Giner, J.; Guija, J.A.; Rico, A.; Barrero, E.; Luna, M.A.; de Leon, J.; et al. Personality disorders and health problems distinguish suicide attempters from completers in a direct comparison. J. Affect. Disord. 2013, 151, 474–483. [Google Scholar] [CrossRef]
- Marquet, R.L.; Bartelds, A.I.; Kerkhof, A.J.; Schellevis, F.G.; van der Zee, J. The epidemiology of suicide and attempted suicide in Dutch general practice 1983–2003. BMC Fam. Pract. 2005, 6, 45. [Google Scholar] [CrossRef]
- Parra Uribe, I.; Blasco-Fontecilla, H.; García-Parés, G.; Giró Batalla, M.; Llorens Capdevila, M.; Cebrià Meca, A.; de Leon-Martinez, V.; Pérez-Solà, V.; Palao Vidal, D.J. Attempted and completed suicide: Not what we expected? J. Affect. Disord. 2013, 150, 840–846. [Google Scholar] [CrossRef]
- Bostwick, J.M.; Pabbat, C.; Gieske, J.R.; Mckean, A.J. Suicide attempts as a risk factor for completed suicide: Even more lethal than we knew. Am. J. Psychiatry. 2016, 173, 1094–1100. [Google Scholar] [CrossRef]
- Younes, N.; Melchior, M.; Turbelin, C.; Blanchon, T.; Hanslik, T.; Chee, C.C. Attempted and completed suicide in primary care: Not what we expeced? J. Affect. Disord. 2015, 170, 150–174. [Google Scholar] [CrossRef] [PubMed]
- Joo, S.H.; Wang, S.M.; Kim, T.W.; Seo, H.J.; Jeong, J.H.; Han, J.H.; Hong, S.C. Factors associated with suicide completion: A comparison between suicide attempters and completers. Asia-Pac. Psychiatry 2016, 8, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Lim, M.; Lee, S.U.; Park, J.I. Difference in suicide methods used between suicide attempters and suicide completers. Int. J. Ment. Health Syst. 2014, 8, 54. [Google Scholar] [CrossRef] [PubMed]
- Turecki, G.; Brent, D.A. Suicide and suicidal behaviour. Lancet 2016, 387, 1227–1239. [Google Scholar] [CrossRef] [PubMed]
- Beatrais, A.L. Suicides and serious suicide attempts: Two populations or one? Psychol. Med. 2001, 31, 837–845. [Google Scholar] [CrossRef]
- Holmstrand, C.; Niméus, A.; Träskman-Bendz, L. Risk factors of future suicide in suicide attempters--a comparison between suicides and matched survivors. Nord. J. Psychiatry 2006, 60, 162–167. [Google Scholar] [CrossRef]
- Tidemalm, D.; Waern, M.; Stefansson, C.G.; Elofsson, S.; Runeson, B. Excess mortality in persons with severe mental disorder in Sweden: A cohort study of 12 103 individuals with and without contact with psychiatric services. Clin. Pract. Epidemiol. Ment. Health 2008, 4, 23. [Google Scholar]
- Tidemalm, D.; Elofsson, S.; Stefansson, C.G.; Waern, M.; Runeson, B. Predictors of suicide in a community-based cohort of individuals with severe mental disorder. Social. Psychiatry Psychiatr. Epidemiol. 2005, 40, 595–600. [Google Scholar] [CrossRef]
- Mortensen, P.; Agerbo, E.; Erikson, T.; Qin, P.; Westergaard-Nielsen, N. Psychiatric illness and risk factors for suicide in Denmark. Lancet 2000, 355, 9–12. [Google Scholar] [CrossRef]
- Reutfors, J.; Brandt, L.; Ekbom, A.; Isacsson, G.; Sparén, P.; Osby, U. Suicide and hospitalization for mental disorders in Sweden: A population-based case-control study. J. Psychiatry Res. 2010, 44, 741–747. [Google Scholar] [CrossRef]
- Madsen, T.; Nordentoft, M. Changes in inpatient and postdischarge suicide rates in a nationwide cohort of Danish psychiatric inpatients, 1998–2005. J. Clin. Psychiatry 2013, 74, e1190–e1194. [Google Scholar] [CrossRef]
- The Norwegian Directorate of Health. Selvmord og Selvmordsforsøk under Innleggelse/Suicide and Suicide Attempts during Admission. Læringsnotat fra Meldeordningen IS-2675; The Norwegian Directorate of Health: Oslo, Norway, 2017. [Google Scholar]
- Krvavac, S.; Jansson, B.; Bukholm, I.R.K.; Wynn, R.; Bystad, M. Patients who die by suicide: A study of treatment patterns and patient safety incidents in Norway. Int. J. Environ. Res. Public Health 2022, 19, 10686. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Norsk Pasientskade Erstatning/The Norwegian System of Patient Injury Compensation (NPE) (2023). Available online: www.npe.no (accessed on 9 January 2023).
- Gunel, E.; Dickey, J. Bayes factors for Independence in contingency tables. Biometrika 1974, 61, 545–557. [Google Scholar] [CrossRef]
- Jamil, T.; Ly, A.; Morey, R.D.; Love, J.; Marsman, M.; Wagenmakers, E.-J. Default “Gunel and Dickey” Bayes factors for contingency tables. Behav. Res. Methods 2016, 49, 638–652. [Google Scholar] [CrossRef] [PubMed]
- Dienes, Z. How Bayes factors change scientific practice. J. Math. Psychol. 2016, 72, 78–89. [Google Scholar] [CrossRef]
- Schönbrodt, F.D.; Wagenmakers, E.J. Bayes factor design analysis: Planning for compelling evidence. Psychonomic. Bull. Rev. 2018, 25, 128–142. [Google Scholar] [CrossRef] [PubMed]
- JASP (Software). Available online: https://jasp-stats.org (accessed on 9 January 2023).
- Busch, K.A.; Fawcett, J.; Jacobs, D.G. Clinical correlates of inpatient suicide. J. Clin. Psychiatry 2003, 64, 14–19. [Google Scholar] [CrossRef]
- Zouk, H.; Tousingnant, M.; Seguin, M.; Lesage, A.; Turecki, G. Characterization of impulisivity in suicide completers: Clinical, behavioural and psychosocial dimensions. J. Affect. Dis. 2006, 92, 195–204. [Google Scholar] [CrossRef]
- Christensen, K.; Chu, C.; Silverman, A.L.; Peckham, A.D.; Björgvinsson, T.; Beard, C. Prevalence and correlates of past-month suicidal thoughts, suicide attempts, and non-suicidal self-injury among adults in a partial hospital program. J. Psychiatry Res. 2021, 144, 397–404. [Google Scholar] [CrossRef]
- Franklin, J.C.; Ribeiro, J.D.; Fox, K.R.; Bentley, K.H.; Kleiman, E.M.; Huang, X.; Musacchio, K.M.; Jaroszewski, A.C.; Chang, B.P.; Nock, M.K. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol. Bull. 2017, 143, 187–232. [Google Scholar] [CrossRef]
- Goldstein, R.B.; Black, D.W.; Nasrallah, A.; Winokur, G. The prediction of suicide. Sensitivity, specificity, and predictive value of a multivariate model applied to suicide among 1906 patients with affective disorders. Arch. Gen. Psychiatry 1991, 48, 418–422. [Google Scholar] [CrossRef] [PubMed]
- Bongar, B.; Sullivan, G. The Suicidal Patient: Clinical and Legal Standards of Care, 3rd ed.; American Psychological Association: Washington, DC, USA, 2013. [Google Scholar]
- Simões, R.M.P.; Dos Santos, J.C.P.; Martinho, M.J.C.M. Adolescents with suicidal behaviours: A qualitative study about the assessment of inpatient service and transition to community. J. Psychiatry Ment. Health Nurs. 2021, 28, 622–631. [Google Scholar] [CrossRef] [PubMed]
- Harden, R.M. What is a spiral curriculum? Med. Teach. 1999, 21, 141–143. [Google Scholar] [CrossRef] [PubMed]
| Sample Characteristics | Suicide Attempters | Suicide Completers | |||
|---|---|---|---|---|---|
| N | % | N | % | Statistics | |
| Age groups | χ2(2) = 2.08, p = 0.353 BF10 = 0.07 | ||||
| 0–29 | 29 | 37.2 | 90 | 32.5 | (Reference) |
| Adj. res. = 0.8 | Adj.res. = −0.8 | ||||
| 30–59 | 42 | 53.8 | 146 | 52.7 | OR = 1.12 (0.65–1.92) |
| Adj. res. = 0.2 | Adj. res. = −0.2 | ||||
| 60– | 7 | 9.0 | 41 | 14.8 | OR = 1.89 (0.76–4.66) |
| Adj. res. = −1.3 | Adj. res. = 1.3 | ||||
| Gender | χ2(1) = 2.08, p = 0.149 BF10 = 0.46 | ||||
| Male | 38 | 48.7 | 161 | 57.9 | (Reference) |
| Adj. res. = −1.4 | Adj. res. = 1.4 | ||||
| Female | 40 | 51.3 | 117 | 42.1 | OR = 0.69 (0.42–1.14) |
| Adj. res. = 1.4 | Adj. res. = −1.4 | ||||
| Suicide Attempters (Reference) | Suicide Completers | ||||
|---|---|---|---|---|---|
| N | % | N | % | Statistics | |
| Diagnosis ICD10 | χ2(1) = 0.84, p = 0.658 BF10 = 0.45 | ||||
| F20–F29 Schizophrenia/psychotic disorders | 16 | 20.5 | 45 | 16.2 | OR = 0.79 (0.37–1.66) |
| Adj. res. = −0.9 | Adj. res. = 0.9 | ||||
| F30–F39 Mood (affective) disorders | 41 | 52.6 | 158 | 56.8 | OR = 1.08 (0.60–1.95) |
| Adj. res. = −0.7 | Adj. res. = 0.7 | ||||
| Other diagnosis | 21 | 26.9 | 75 | 27 | (Reference) |
| Adj. res. = 0 | Adj. res. = 0 | ||||
| Suicide Attempters (Reference) | Suicide Completers | ||||
|---|---|---|---|---|---|
| N | % | N | % | Statistics | |
| Patient’s status | χ2(1) = 3.65, p = 0.056 BF10 = 0.96 | ||||
| Inpatient | 52 | 66.7 | 152 | 54.7 | (Reference) |
| Adj. res. = 1.9 | Adj. res. = −1.9 | ||||
| Outpatient | 26 | 33.3 | 126 | 45.3 | OR = 1.66 (0.98–2.81) |
| Adj. res. = −1.9 | Adj. res. = 1.9 | ||||
| Type of health care | χ2(1) = 0.03, p = 0.865 BF10 = 0.14 | ||||
| Psychiatric institutions | 58 | 75.3 | 212 | 76.3 | (Reference) |
| Adj. res. = −0.2 | Adj. res. = 0.2 | ||||
| Other institutions | 19 | 24.7 | 66 | 23.7 | OR = 0.95 (0.53–1.71) |
| Adj. res. = 0.2 | Adj. res. = −0.2 | ||||
| Type of treatment | χ2(1) = 6.48, p = 0.039 BF10 = 0.75 | ||||
| Medication only | 38 | 64.4 | 107 | 48.4 | (Reference) |
| Adj. res. = 2.2, p = 0.01 | Adj. res. = −2.2, p = 0.01 | ||||
| Medication and psychotherapy | 14 | 23.7 | 91 | 41.2 | OR = 2.31 (1.18–4.53) |
| Adj. res. = −2.5, p = 0.006 | Adj. res. = 2.5, p = 0.006 | ||||
| ECT, medication, and psychotherapy | 7 | 11.9 | 23 | 10.4 | OR = 1.17 (0.46–2.94) |
| Adj. res. = 0.3 | Adj. res. = −0.3 | ||||
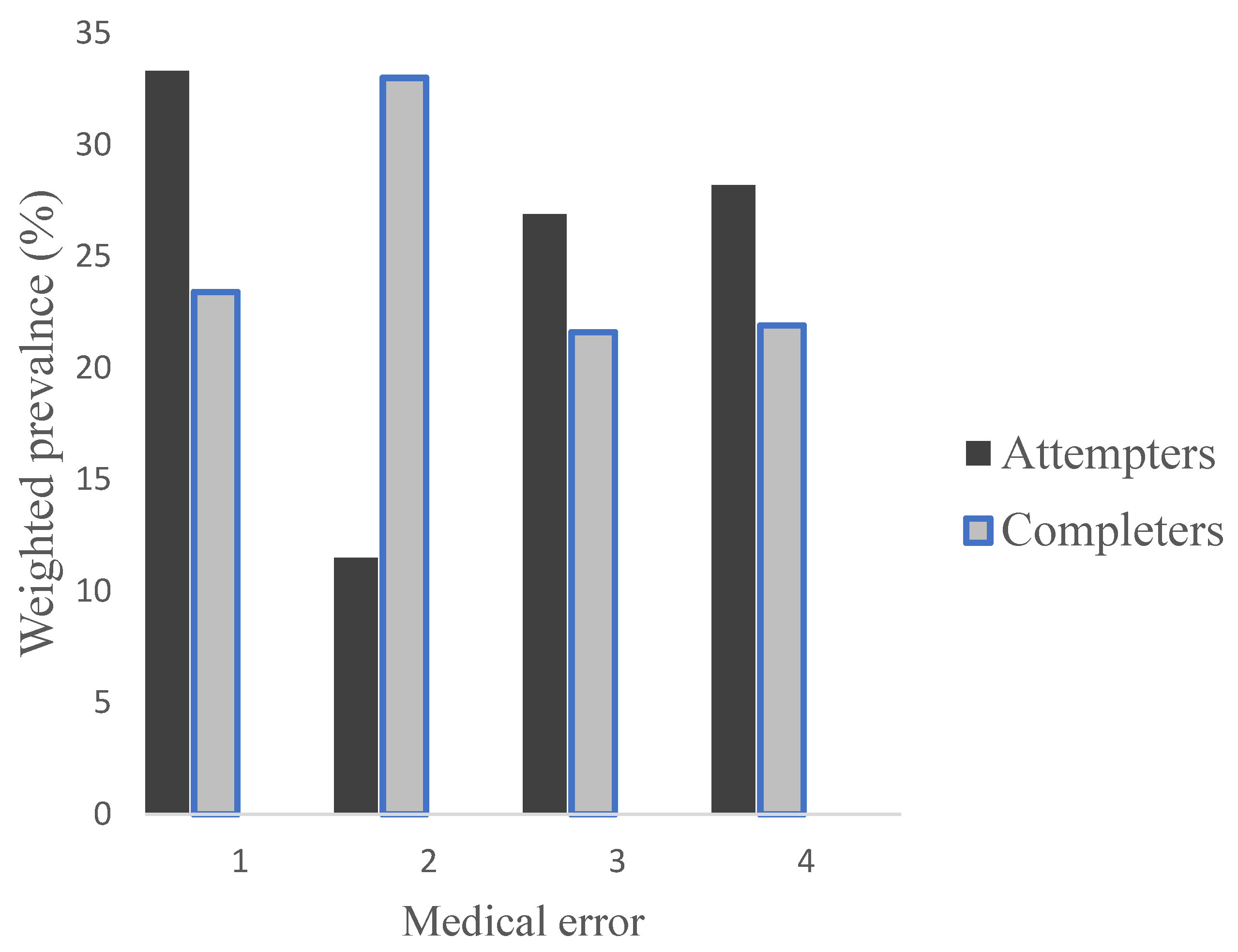
| Type of medical error | χ2(3) =16.06, p = 0.001 BF10 = 21.76 | ||||
| Insufficient level of observation and lack of safety measures | 26 | 33.3 | 65 | 23.4 | (Reference) |
| Adj. res. = 1.8, p = 0.03 | Adj. res. = −1.8, p = 0.03 | ||||
| Inadequate suicide risk assessment | 9 | 11.5 | 92 | 33.1 | OR = 4.09 (1.80–9.30) |
| Adj. res.= −3.7, p = 0.0001 | Adj. res. = 3.7, p = 0.0001 | ||||
| Inadequate/Delayed clinical/diagnostic/assessment | 21 | 26.9 | 60 | 21.6 | OR = 1.14 (0.58–2.24) |
| Adj. res. = 1 | Adj. res. = −1 | ||||
| Inadequate treatment | 22 | 28.2 | 61 | 21.9 | OR = 1.11 (0.57–2.16) |
| Adj. res. = 1.2 | Adj. res. = −1.2 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krvavac, S.; Bystad, M.; Wynn, R.; Bukholm, I.R.K.; Jansson, B. Characteristics of Patients Who Complete Suicide and Suicide Attempts While Undergoing Treatment in Norway: Findings from Compensation Claims Records. Int. J. Environ. Res. Public Health 2023, 20, 4083. https://doi.org/10.3390/ijerph20054083
Krvavac S, Bystad M, Wynn R, Bukholm IRK, Jansson B. Characteristics of Patients Who Complete Suicide and Suicide Attempts While Undergoing Treatment in Norway: Findings from Compensation Claims Records. International Journal of Environmental Research and Public Health. 2023; 20(5):4083. https://doi.org/10.3390/ijerph20054083
Chicago/Turabian StyleKrvavac, Sanja, Martin Bystad, Rolf Wynn, Ida Rashida Khan Bukholm, and Billy Jansson. 2023. "Characteristics of Patients Who Complete Suicide and Suicide Attempts While Undergoing Treatment in Norway: Findings from Compensation Claims Records" International Journal of Environmental Research and Public Health 20, no. 5: 4083. https://doi.org/10.3390/ijerph20054083
APA StyleKrvavac, S., Bystad, M., Wynn, R., Bukholm, I. R. K., & Jansson, B. (2023). Characteristics of Patients Who Complete Suicide and Suicide Attempts While Undergoing Treatment in Norway: Findings from Compensation Claims Records. International Journal of Environmental Research and Public Health, 20(5), 4083. https://doi.org/10.3390/ijerph20054083






