The Influence of Everyday Acoustic Environments on the Challenging Behavior in Dementia: A Participatory Observation Study in Nursing Homes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Context of the Study
2.2. Research Design
2.3. Sampling
2.4. Data Collection
- Field notes to include as much information as possible. Field notes are always recorded on site to ensure everything is captured (we made sure to finish the notes right after observation and before leaving the site. We were also writing notes throughout the observation). Including as much information as possible in the field notes were necessary;
- Dates, times, and space identification;
- Sensory of the space: light, sounds, smells, taste and texture of the material,
- Any conversation or phrases used during the observation or phrases in any language or any insider conversation;
- Any questions the observer may have concerning the site for further investigation;
- Personal response to the facts that were observed,
- All pages are numbered to keep the record in order,
- For clarity, always keep four sections separated: notes, description of notes, analysis, and reflection of the observation.
2.5. Data Analysis
2.6. Quality Insurance
3. Results
3.1. Naïve Understanding
3.2. Structural Analysis
3.2.1. Theme 1: Acoustic Can Prevent the Onset of CB
“Seven residents are sitting around the table in the kitchen. The doorbell rings: it sounds throughout the building. Resident 7 gets up and walks towards the corridor.”
“Resident 7 is seated with another resident, whom he considers his wife. Another resident comes along, talking and humming; a caregiver walks by with rattling keys. The footsteps of the caregiver are audible. A TV and music can be heard in the distance. Resident 7 murmurs calmly to the resident with whom he is holding hands.”
3.2.2. Theme 2: The Absence of Acoustic Triggers Causes Anxiousness and Mistrust. Wandering, Talking or Manipulating Objects Can Create a Feeling of Safety
“The hallway is empty and quiet. The night shift cart is being driven around; the wheels run on the floor tiles. The caregivers whisper and enter the room as quietly as possible. Resident 5 sits on his chair in his room, talking to himself.”
“It’s night, all the residents are in bed, and the ward is quiet. The radio is off. Resident 7 is standing in the kitchen, turning the knobs on the radio. He keeps doing this for 20 min.”
“The television is on in the dining room. The TV is very loud. Resident 1 comes out of the silent corridor through the door and walks halfway in the room while watching the TV; she stays halfway through the room and continues watching the TV from a distance.”
3.2.3. Theme 3: Complex Sound Environments Cause an Uncomfortable or Angry Feeling, Which Can Be Solved by the Resident’s Behavior That Set Outs to Avoid or Reduce the Noise
“Resident 2 is in the dining room, back-to-back with resident 1. Resident 1 talks a lot, loud and well audible; she looks angry over her shoulder several times when resident 1 talks. In the meantime, classical music playing non-dominant.”
“Resident 14 sits at the table in the dining room. The food is served. There is the clatter of cutlery. Staff and volunteers walk around; people talk at the tables. Resident 14 gets up and walks out of the dining area.”
“After dinner, resident 8 sits at the table in his wheelchair, fixated with a belt around the waist. There is much talking and singing. Resident 8 constantly tries to stand up straight from his wheelchair, despite the fixation. Resident 14 is taken out of the bath and dressed; the caretaker starts blow-drying. Resident 14 sits on a chair and allows this but puts the fingers in the ears, holding the head down.”
3.2.4. Theme 4: PwD Can Misinterpret Sounds and Therefore Do Not React in a Way That Is Expected
“Resident 7 sits in the seats in the hallway with his eyes closed. Ward is quiet. A laptop makes noise. Resident 7 looks up in the direction of the laptop, then looks back in front of him and closes his eyes.”
“Resident 10 gets up from the toilet. The caregiver flushes without announcing it. Resident 10 reacts by saying: “Oh God, who was that?”
“All seven residents sit around the table in the kitchen. The doorbell rings (sound is audible throughout the building). Resident 7 stands up and walks towards the corridor.”
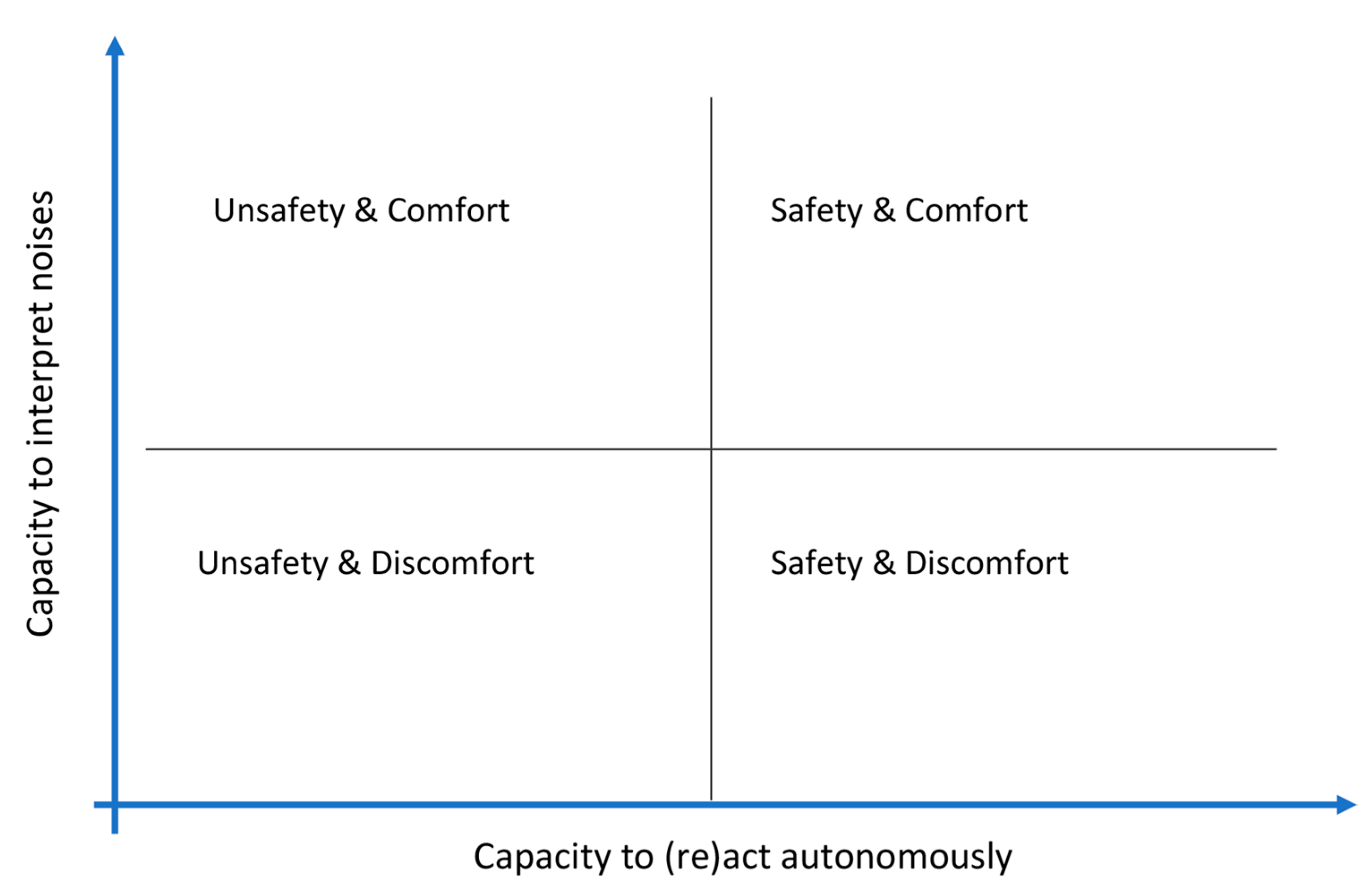
3.3. Comprehensive Understanding
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Integrated Care for Older People: Realigning Primary Health Care to Respond to Population Ageing; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Finkel, S. Introduction to behavioural and psychological symptoms of dementia (BPSD). Int. J. Geriatr. Psychiatry 2000, 15, S2–S4. [Google Scholar] [CrossRef]
- Azerma, M. Dealing with behavioral and psychological symptoms of dementia: A general overview. Psychol. Res. Behav. Manag. 2015, 2015, 181–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krishnamoorthy, A.; Anderson, D. Managing challenging behaviour in older adults with dementia. Prog. Neurol. Psychiatry 2011, 15, 20–26. [Google Scholar] [CrossRef]
- Benoit, M.; Arbus, C.; Blanchard, F.; Camus, V. Professional consensus on the treatment of agitation, aggressive behaviour, oppositional behaviour and psychotic disturbances in dementia. J. Nutr. Health Aging 2006, 10, 410–415. [Google Scholar] [PubMed]
- Oliveira, A.M.D.; Radanovic, M.; Mello, P.C.H.D.; Buchain, P.C.; Vizzotto, A.D.B.; Celestino, D.L.; Stella, F.; Piersol, C.V.; Forlenza, O.V. Nonpharmacological Interventions to Reduce Behavioral and Psychological Symptoms of Dementia: A Systematic Review. Biomed. Res. Int. 2015, 2015, 218980. [Google Scholar] [CrossRef] [Green Version]
- Liperoti, R.; Pedone, C.; Corsonello, A. Antipsychotics for the Treatment of Behavioral and Psychological Symptoms of Dementia (BPSD). Curr. Neuropharmacol. 2008, 6, 117–124. [Google Scholar] [CrossRef] [Green Version]
- Ricci, G. Social Aspects of Dementia Prevention from a Worldwide to National Perspective: A Review on the International Situation and the Example of Italy. Behav. Neurol. 2019, 2019, 8720904. [Google Scholar] [CrossRef] [Green Version]
- Agüero-Torres, H. Institutionalization in the elderly The role of chronic diseases and dementia. Cross-sectional and longitudinal data from a population-based study. J. Clin. Epidemiol. 2001, 54, 795–801. [Google Scholar] [CrossRef]
- Fauth, E.B.; Gibbons, A. Which behavioral and psychological symptoms of dementia are the most problematic? Variability by prevalence, intensity, distress ratings, and associations with caregiver depressive symptoms. Int. J. Geriatr. Psychiatry 2014, 29, 263–271. [Google Scholar] [CrossRef]
- Hurt, C.; Bhattacharyya, S.; Burns, A.; Camus, V.; Liperoti, R.; Marriott, A.; Nobili, F.; Robert, P.; Tsolaki, M.; Vellas, B.; et al. Patient and Caregiver Perspectives of Quality of Life in Dementia. Dement. Geriatr. Cogn. Disord. 2008, 26, 138–146. [Google Scholar] [CrossRef]
- Samus, Q.M.; Rosenblatt, A.; Steele, C.; Baker, A.; Harper, M.; Brandt, J.; Mayer, L.; Rabins, P.V.; Lyketsos, C.G. The Association of Neuropsychiatric Symptoms and Environment with Quality of Life in Assisted Living Residents With Dementia. Gerontologist 2005, 45, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Feast, A.; Moniz-Cook, E.; Stoner, C.; Charlesworth, G.; Orrell, M. A systematic review of the relationship between behavioral and psychological symptoms (BPSD) and caregiver well-being. Int. Psychogeriatr. 2016, 28, 1761–1774. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cook, E.D.M.; Swift, K.; James, I.; Malouf, R.; de Vugt, M.; Verhey, F. Functional analysis-based interventions for challenging behaviour in dementia. Cochrane Database Syst. Rev. 2012. [Google Scholar] [CrossRef] [Green Version]
- O’Neil, M.; Freeman, M.; Christensen, V.; Telerant, R.; Addleman, A.; Kansagara, D. A Systematic Evidence Review of Non-pharmacological Interventions for Behavioral Symptoms of Dementia; Health Services Research & Development Service: Washington, DC, USA, 2011. [Google Scholar]
- Abraha, I.; Rimland, J.M.; Trotta, F.M.; Dell’Aquila, G.; Cruz-Jentoft, A.; Petrovic, M.; Gudmundsson, A.; Soiza, R.; O’Mahony, D.; Guaita, A.; et al. Systematic review of systematic reviews of non-pharmacological interventions to treat behavioural disturbances in older patients with dementia. The SENATOR-OnTop series. BMJ Open 2017, 7, e012759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dyer, S.M.; Harrison, S.L.; Laver, K.; Whitehead, C.; Crotty, M. An overview of systematic reviews of pharmacological and non-pharmacological interventions for the treatment of behavioral and psychological symptoms of dementia. Int. Psychogeriatr. 2018, 30, 295–309. [Google Scholar] [CrossRef] [Green Version]
- Bourdon, E.; Havreng-Théry, C.; Lafuente, C.; Belmin, J. Effect of the Physical Environment on Health and Well-Being of Nursing Homes Residents: A Scoping Review. J. Am. Med. Dir. Assoc. 2022, 23, E1826.E1–E1826.E20. [Google Scholar] [CrossRef] [PubMed]
- Connolly, D.; Dockrell, J.; Shield, B.; Conetta, R.; Mydlarz, C.; Cox, T. The effects of classroom noise on the reading comprehension of adolescents. J. Acoust. Soc. Am. 2019, 145, 372–381. [Google Scholar] [CrossRef]
- Wilson, J.D.; McGinnis, N.; Latkova, P.; Tierney, P.; Yoshino, A. Urban Park Soundscapes: Association of Noise and Danger with Perceived Restoration. J. Park Recreat. Adm. 2016, 34. [Google Scholar] [CrossRef]
- Brown, B.; Rutherford, P.; Crawford, P. The role of noise in clinical environments with particular reference to mental health care: A narrative review. Int. J. Nurs. Stud. 2015, 52, 1514–1524. [Google Scholar] [CrossRef] [Green Version]
- Andringa, T.; Lanser, J. How Pleasant Sounds Promote and Annoying Sounds Impede Health: A Cognitive Approach. Int. J. Env. Res. Public Health 2013, 10, 1439–1461. [Google Scholar] [CrossRef] [Green Version]
- Truax, B. Acoustic Communication; Ablex Publishing Corp.: New York, NY, USA, 1984. [Google Scholar]
- ISO12913-1; Acoustics-Soundscape-Part 1: Definition and Conceptual Framework. Acoustique-Paysage Sonore-Partie 1: Définition et Cadre Conceptuel. ISO: Geneva, Switzerland, 2014. Available online: www.iso.org (accessed on 14 May 2019).
- Axelsson, Ö.; Nilsson, M.E.; Berglund, B. A principal components model of soundscape perception. J. Acoust. Soc. Am. 2010, 128, 2836–2846. [Google Scholar] [CrossRef] [PubMed]
- Aletta, F.; Botteldooren, D.; Thomas, P.; Vander Mynsbrugge, T.; De Vriendt, P.; Van de Velde, D.; Devos, P. Monitoring sound levels and soundscape quality in the living rooms of nursing homes: A case study in Flanders (Belgium). Appl. Sci. 2017, 7, 874. [Google Scholar] [CrossRef] [Green Version]
- Van den Bosch, K.A.M.; Welch, D.; Andringa, T.C. The evolution of soundscape appraisal through enactive cognition. Front. Psychol. 2018, 9, 1129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, P.; Aletta, F.; Filipan, K.; Vander Mynsbrugge, T.; De Geetere, L.; Dijckmans, A.; Botteldooren, D.; Petrovic, M.; Van de Velde, D.; De Vriendt, P.; et al. Noise environments in nursing homes: An overview of the literature and a case study in Flanders with quantitative and qualitative methods. Appl. Acoust. 2020, 159, 107103. [Google Scholar] [CrossRef]
- Devos, P.; Thomas, P.; Aletta, F.; Vander Mynsbrugge, T.; De Vriendt, P.; Van de Velde, D.; Botteldooren, D. Towards Understanding Healthy and Supportive Acoustic Environments: The case of a nursing home. In Proceedings of the International Congress on Acoustics, Aachen, Germany, 9–13 September 2019. [Google Scholar]
- van den Bosch, K.A.; Andringa, T.C.; Post, W.J.; Ruijssenaars, W.A.J.J.M.; Vlaskamp, C. The relationship between soundscapes and challenging behavior: A small-scale intervention study in a healthcare organization for individuals with severe or profound intellectual disabilities. Build. Acoust. 2018, 25, 123–135. [Google Scholar] [CrossRef]
- De Pessemier, T.; Vanhecke, K.; Thomas, P.; Vander Mynsbrugge, T.; Vercoutere, S.; Van de Velde, D.; De Vriendt, P.; Joseph, W.; Martens, L.; Botteldooren, D.; et al. Personalising augmented soundscapes for supporting persons with dementia. Multimed. Tools Appl. 2022. [Google Scholar] [CrossRef]
- Kosters, J.; Janus, S.I.M.; van den Bosch, K.A.; Zuidema, S.; Luijendijk, H.J.; Andringa, T.C. Soundscape Optimization in Nursing Homes Through Raising Awareness in Nursing Staff WITH MoSART+. Front. Psychol. 2022, 13, 871647. [Google Scholar] [CrossRef] [PubMed]
- Devos, P.; Aletta, F.; Vander Mynsbrugge, T.; Thomas, P.; Filipan, K.; Petrovic, M.; De Vriendt, P.; Van de Velde, D.; Botteldooren, D. Soundscape design for management of behavioral disorders: A pilot study among nursing home residents with dementia. In INTER-NOISE and NOISE-CON Congress and Conference Proceedings; Institute of Noise Control Engineering: Reston, VA, USA, 2018. [Google Scholar]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 3rd ed.; Prentice Hall: Hoboken, NJ, USA, 2007. [Google Scholar]
- Agentschap Zorg en Gezondheid. Besluit van de Vlaamse Regering tot Wijziging van Bijlage XII Bij het Besluit van de Vlaamse Regering van 24 Juli 2009 Betreffende de Programmatie, de Erkenningsvoorwaarden en de Subsidieregeling Voor Woonvoorzieningen en Verenigingen van Gebruikers en Mantelzorgers, wat de Voorwaarden Infrastructuur Betreft. 2017. Available online: https://codex.vlaanderen.be/PrintDocument.ashx?id=1032439&datum=&geannoteerd=false&print=false (accessed on 14 December 2022).
- Patton, M.Q. Qualitative Research & Evaluation Methods: Integrating Theory and Practice; Sage Publications: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. Mini-mental state. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Kok, R.; Verhey, F. Dutch translation of the Mini Mental State Examination; Altrecht GGZ: Utrecht, The Netherlands, 2002; pp. 1–2. [Google Scholar]
- Katz, S. Studies of Illness in the Aged. JAMA 1963, 185, 914. [Google Scholar] [CrossRef]
- Kaufer, D.I.; Cummings, J.L.; Ketchel, P.; Smith, V.; MacMillan, A.; Shelley, T.; Lopez, O.L.; DeKosky, S.T. Validation of the NPI-Q, a Brief Clinical Form of the Neuropsychiatric Inventory. J. Neuropsychiatry Clin. Neurosci. 2000, 12, 233–239. [Google Scholar] [CrossRef]
- Dahlke, S.; Hall, W.; Phinney, A. Maximizing theoretical contributions of participant observation while managing challenges. Qual. Health Res. 2015, 25, 1117–1122. [Google Scholar] [CrossRef]
- Taylor, R.R. Kielhofner’s Research in Occupational Therapy: Methods of Inquiry for Enhancing Practice, 2nd ed.; Davis Company: Philadelphia, PA, USA, 2017. [Google Scholar]
- Lindseth, A.; Norberg, A. A phenomenological hermeneutical method for researching lived experience. Scand. J. Caring Sci. 2004, 18, 145–153. [Google Scholar] [CrossRef]
- Volicer, L.; Hurley, A.C. Review Article: Management of Behavioral Symptoms in Progressive Degenerative Dementias. J. Gerontol. A Biol. Sci. Med. Sci. 2003, 58, M837–M845. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zuidema, S.U.; Johansson, A.; Selbaek, G.; Murray, M.; Burns, A.; Ballard, C.; Koopmans, R.T. A consensus guideline for antipsychotic drug use for dementia in care homes. Bridging the gap between scientific evidence and clinical practice. Int. Psychogeriatr. 2015, 27, 1849–1859. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerritsen, D.L.; Smalbrugge, M.; Veldwijk-Rouwenhorst, A.E.; Wetzels, R.; Zuidema, S.U.; Koopmans, R.T.C.M. The Difficulty with Studying Challenging Behavior. J. Am. Med. Dir. Assoc. 2019, 20, 879–881. [Google Scholar] [CrossRef]
- Tible, O.P.; Riese, F.; Savaskan, E.; von Gunten, A. Best practice in the management of behavioural and psychological symptoms of dementia. Adv. Neurol. Disord. 2017, 10, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Albayrak, A.; van der Cammen, T.J.M. A systematic review of non-pharmacological interventions for BPSD in nursing home residents with dementia: From a perspective of ergonomics. Int. Psychogeriatr. 2019, 31, 1137–1149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaudhury, H.; Hung, L.; Badger, M. The Role of Physical Environment in Supporting Person-centered Dining in Long-Term Care. Am. J. Alzheimer’s Dis. Other Dement. 2013, 28, 491–500. [Google Scholar] [CrossRef] [PubMed]
- van den Bosch, K.A.; Andringa, T.C.; Başkent, D.; Vlaskamp, C. The Role of Sound in Residential Facilities for People with Profound Intellectual and Multiple Disabilities. J. Policy Pr. Intellect. Disabil. 2016, 13, 61–68. [Google Scholar] [CrossRef]
- Aletta, F.; Vander Mynsbrugge, T.; Van de Velde, D.; De Vriendt, P.; Thomas, P.; Filipan, K.; Botteldooren, D.; Devos, P. Awareness of ‘sound’ in nursing homes: A large-scale soundscape survey in Flanders (Belgium). Build. Acoust. 2018, 25, 43–59. [Google Scholar] [CrossRef]
- Koch, J.; Amos, J.G.; Beattie, E.; Lautenschlager, N.T.; Doyle, C.; Anstey, K.J.; Mortby, M.E. Non-pharmacological interventions for neuropsychiatric symptoms of dementia in residential aged care settings: An umbrella review. Int. J. Nurs. Stud. 2022, 128, 104187. [Google Scholar] [CrossRef]
- Lawton, M.P. An Ecological Theory of Aging Applied to Elderly Housing. J. Archit. Educ. 1977, 31, 8–10. [Google Scholar] [CrossRef]
- Law, M.; Cooper, B.; Strong, S.; Stewart, D.; Rigby, P.; Letts, L. The Person-Environment-Occupation Model: A Transactive Approach to Occupational Performance. Can. J. Occup. Ther. 1996, 63, 9–23. [Google Scholar] [CrossRef]
- Turpin, M.; Iwama, M. Using Occupational Therapy Models in Practice, 1st ed.; Elsevier: Amsterdam, The Netherlands, 2010. [Google Scholar]
- Lawton, M.P. The Elderly in Context. Env. Behav. 1985, 17, 501–519. [Google Scholar] [CrossRef]
- Zhao, Q.F.; Tan, L.; Wang, H.F.; Jiang, T.; Tan, M.S.; Tan, L.; Xu, W.; Li, J.Q.; Wang, J.; Lai, T.J.; et al. The prevalence of neuropsychiatric symptoms in Alzheimer’s disease: Systematic review and meta-analysis. J. Affect. Disord. 2016, 190, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Drever, J.L.; Hugill, A. Aural Diversity; Routledge: New York, NY, USA, 2022. [Google Scholar] [CrossRef]
- Wiratha, M.S.; Tsaih, L. Acoustic comfort in long-term care facilities based on listening impressions from normal hearing individuals. Proc. Meet. Acoust. 2015, 25, 015003. [Google Scholar] [CrossRef] [Green Version]
- Erfanian, M.; Mitchell, A.J.; Kang, J.; Aletta, F. The Psychophysiological Implications of Soundscape: A Systematic Review of Empirical Literature and a Research Agenda. Int. J. Env. Res. Public Health 2019, 16, 3533. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Wave 1 | |||||
|---|---|---|---|---|---|
| Resident | Nursing Home | Sex | Katz-Scale Score | MMSE | NPI-Q |
| 1 | 1 | Female | D | / (1) | 16/36 |
| 2 | 1 | Female | CD | 2/30 | 8/36 |
| 3 | 1 | Female | CD | 2/30 | 13/36 |
| 4 | 1 | Female | D | 8/30 | 10/36 |
| 5 | 1 | Male | D | / (2) | 20/36 |
| 6 | 2 | Female | D | 7/30 | 6/36 |
| 7 | 2 | Male | D | 6/30 | 8/36 |
| 8 | 2 | Male | CD | / (1) | 5/36 |
| 9 | 2 | Female | D | / (1) | 5/36 |
| 10 | 2 | Female | D | 5/30 | 8/36 |
| 11 | 3 | Male | D | 14/30 | 15/36 |
| 12 | 3 | Female | CD | 10/30 | 10/36 |
| 13 | 3 | Female | CD | 13/30 | 11/36 |
| 14 | 3 | Female | CD | 2/30 | 12/36 |
| 15 | 3 | Female | D | / (2) | 9/36 |
| 16 | 4 | Female | D | 11/30 | 8/36 |
| 17 | 4 | Male | CD | 4/30 | 10/36 |
| 18 | 4 | Female | CD | / (1) | |
| 19 | 4 | Female | CD | 8/30 | 10/36 |
| 20 | 4 | Female | D | / (2) | 20/36 |
| Wave 2 | |||||
| Resident | Nursing Home | Sex | Katz-Scale Score | MMSE | GDS Score |
| 1 | 1 | Female | CD | 8/30 | 7 |
| 2 | 1 | Male | CD | / | 6 |
| 3 | 1 | Female | D | / | 6 |
| 4 | 2 | Female | CD | / | 6 |
| 5 | 2 | Male | CD | / | 6 |
| 6 | 2 | Male | CD | / | 5 |
| 7 | 3 | Female | CD | / | 7 |
| 8 | 3 | Female | CD | 16/30 | 5 |
| 9 | 3 | Male | CD | 12/30 | 6 |
| 10 | 4 | Female | CD | / | 7 |
| 11 | 4 | Female | CD | / | 6 |
| 12 | 4 | Female | B | / | 4 |
| 13 | 5 | Female | B | 15/30 | 5 |
| 14 | 5 | Female | B | 1/30 | 5 |
| 15 | 5 | Male | B | 6/30 | 6 |
| Meaning Unit | Condensation | Subtheme | Theme | ||
|---|---|---|---|---|---|
| Antecedent | Behaviour | Consequence | |||
| The caregiver goes to the wardrobe (which is against the outside wall of the bathroom). She opens the wardrobe door with a key (it makes a lot of noise). The doors are closed again, making a loud slamming noise. The room was completely silent, making the sound very noticeable | Resident 1 yells, while standing in the bathroom: boo boo! | The caregiver yells back at her: “It’s okay, I am just messing around in the wardrobe.” | Yelling in response to a striking sound that is very noticeable in a completely silent space | Vocal reaction to sound that is not understood | Not understanding the sound |
| Resident 14 sits at the table in the dining room. The food is scooped out. There is the clatter of cutlery. People (staff and volunteers) walk around the room and provide everyone with a plate of food. There is talk at the tables | Resident 14 gets up and walks out of the dining area towards the hallway | The caregiver asks her: “Wouldn’t it be better to stay seated? Your food will be served in a minute.” | Getting up, leaving the dining room, which is very crowded with voices and the cutlery | Moving away from a noisy and crowded space | Too many stimuli |
| Resident 17 sits in the dining/living room at a table. Twelve other residents are in the room, four aid workers and a family member. The family member talks to a resident at the table next to resident 17. The care workers stand behind him, talking. Sometimes the cat meows. You can hear spoons sounding against porcelain. | Resident 17 eats soup and looks over his shoulder at where the care workers are talking | He starts talking to the residents at his table. He talks to himself but directs it to others at the table | Looking over the shoulder in the direction of the voice and then talking to oneself and people at the table in a room with a lot of ambient noise. | Looking in the direction of the sound. After determining he is safe, resume activity. | Identifying the sound |
| In the living room, the TV and radio are on simultaneously. The robocat is making a purring sound on the table | Resident 16 talks in the cat’s ear and says, “So sweet; you’re so sweet.” | / | Calm and sweet talking to the robocat. | Calmly talking | No CB |
| The hallway is quiet. The sound of the dining area is occasionally audible in the distance. In some parts of the corridor, it is not audible at all. | She begins to walk down the corridor (these are endless, arranged in a square). She talks to herself and walks down the corridor. | She keeps walking around and talking to herself. | Wandering around in a very quiet hallway and talking to oneself. | Wandering around because of under-stimulation | Not enough stimuli |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Talebzadeh, A.; Decoutere, I.; Vander Mynsbrugge, T.; Botteldooren, D.; Devos, P.; Aletta, F.; Van de Velde, D.; De Vriendt, P. The Influence of Everyday Acoustic Environments on the Challenging Behavior in Dementia: A Participatory Observation Study in Nursing Homes. Int. J. Environ. Res. Public Health 2023, 20, 4191. https://doi.org/10.3390/ijerph20054191
Talebzadeh A, Decoutere I, Vander Mynsbrugge T, Botteldooren D, Devos P, Aletta F, Van de Velde D, De Vriendt P. The Influence of Everyday Acoustic Environments on the Challenging Behavior in Dementia: A Participatory Observation Study in Nursing Homes. International Journal of Environmental Research and Public Health. 2023; 20(5):4191. https://doi.org/10.3390/ijerph20054191
Chicago/Turabian StyleTalebzadeh, Arezoo, Ine Decoutere, Tara Vander Mynsbrugge, Dick Botteldooren, Paul Devos, Francesco Aletta, Dominique Van de Velde, and Patricia De Vriendt. 2023. "The Influence of Everyday Acoustic Environments on the Challenging Behavior in Dementia: A Participatory Observation Study in Nursing Homes" International Journal of Environmental Research and Public Health 20, no. 5: 4191. https://doi.org/10.3390/ijerph20054191







